ABSTRACT
Intracranial enterogenous cysts are rare. There have been only two cases reported of such cysts that extended into both the infratentorial and supratentorial compartments. We add a third case and review the literature to assess their pathogenesis, clinical features, and management.
Keywords: Enterogenous cyst, neurenteric cyst, infratentorial, supratentorial
CASE REPORT
A 20-year-old woman was admitted to our department with an 8-month history of gradual onset progressive headache, left hemiparesis, left deafness, unsteadiness, and blurred vision. A clinical examination revealed sensorineural deafness on the left, left trigeminal and left hypoglossal palsies, and left hemiparesis (MRC grade 4). We also observed bilateral papilledema.
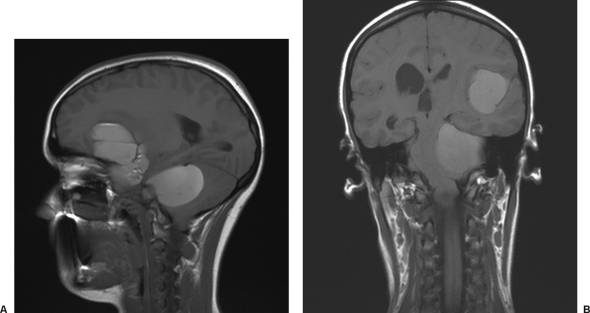
A magnetic resonance imaging (MRI) brain scan showed a very large cystic lesion involving the left temporal, peri-insular region and the left cerebellopontine region, with gross midline shift and compression of the left lateral ventricle (Fig. 1).
Figure 1.
(A) Sagittal T1 magnetic resonance image indicates a narrow extension of the cyst (not shown) connected the supratentorial and infratentorial extension of the enterogenous cyst. (B) Coronal T1 magnetic resonance image.
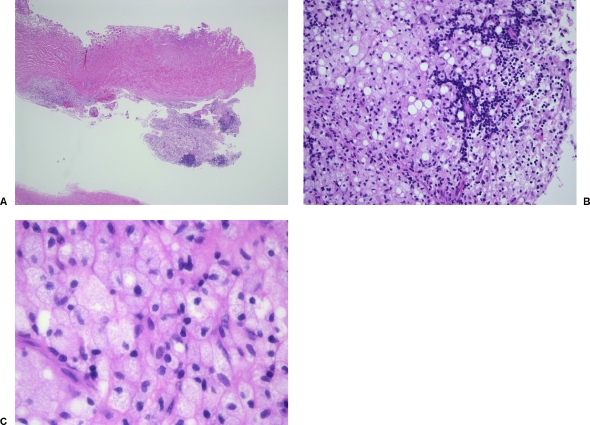
An evacuation of the cyst was performed through a double craniotomy; a left subtemporal craniotomy, and a left suboccipital retrosigmoid craniotomy. A very turbid and thick fluid was aspirated and a large lump of inspissated proteinaceous material was removed. The cyst was followed into the tentorial hiatus and because it was impossible to evacuate completely from the supratentorial route, a suboccipital craniotomy was performed and the rest of the cyst was evacuated. The whole cystic cavity was washed with Hartmann's solution. The histopathological findings of the cyst and its contents were in keeping with the diagnosis of enterogenous cyst (Fig. 2). The patient achieved good postoperative recovery with improvement of the hearing deficit and left hemiparesis and returned to work.
Figure 2.
(A) Lower magnification (4×) photomicrograph of the cyst wall and its contents: cuboidal epithelium (two-layered in most areas) with evidence of keratinization and considerable sclerosis. (B) (20×) Photomicrograph of the cyst wall: there are cholesterol clefting and foamy macrophages associated with the cyst. (C) (60×) Photomicrograph with high magnification: note the glandular structures containing proteinaceous material.
DISCUSSION
Enterogenous cysts (ECs) are thought to originate from persistence of endodermal remnants of the notochord during the first 3 weeks of gestation. It is assumed by most authors1,2 that an incomplete separation of the primitive foregut (endoderm) and of the primitive notocord may trap a small part of endodermal germ cells inside the spinal canal and disturb the development of the mesoderm. This theory on the embryogenesis of ECs fails to explain this intracranial location, in the cerebral hemispheres or in the sellar or parasellar regions.2 In fact, during embryogenesis, the endoderm does not extend cranially farther than the clivus. Graziani et al,3 having considered the immunohistochemistry and the histology of ECs, colloid cyst, and Rathke cleft cyst, suggested that all three of these entities originate from Seessel's pouch, a diverticulum of the primitive foregut that in humans usually regresses and disappears. The name of the cyst will thus depend on the anatomical location of the remnants of Seessel's pouch. Further evidence in support of the previous theory is that intracranial ECs have not been associated with additional developmental malformations commonly observed with spinal ECs4 (vertebral anomalies, fistulae, or fibrous tract connecting to thoracic or abdominal structures derived from the primitive gut). A topographical classification of intracranial ECs does not exist.4 These lesions are classified according to histological characterization of their wall instead and the presence or absence of components specific to the respiratory or gastrointestinal tracts.5 Type A cysts have a simple lining (or pseudostratified) cuboidal or columnar epithelium, on a basal membrane, with or without cilia, resembling gastrointestinal or respiratory epithelium. The presence of other components usually seen along the gastrointestinal or respiratory tracts (serous or mucous glands, connective or lymphoid tissue, smooth muscle, nerve ganglion) is typical of type B cysts. Type C cysts, in addition, contain glial or ependymal elements.6 ECs have seeding potential4,7,8,9 and intraoperative confirmation of the histology is desirable, to remove the cyst completely and avoid delayed recurrences.10 The optimum treatment for ECs therefore should be total excision at a single sitting4,11 and long-term follow-up is mandatory to detect any recurrences.
REFERENCES
- Bejjani G K, Wright D C, Schessel D, Sekhar L N. Endodermal cyst of the posterior fossa: report of three cases and review of the literature. J Neurosurg. 1998;89:326–335. doi: 10.3171/jns.1998.89.2.0326. [DOI] [PubMed] [Google Scholar]
- Harris C P, Dras M S, Brockmeier D L, Townsend J J, Willis B K, Apflebaum R I. Neurenteric cyst of the posterior fossa: recognition, management and embryogenesis. Neurosurgery. 1991;29:893–897. doi: 10.1097/00006123-199112000-00015. [DOI] [PubMed] [Google Scholar]
- Graziani N, Dufour H, Figarella-Branger D, Donnet A, Bouillot P, Grisoli F. Do the suprasellar neurenteric cyst, the Rathke cleft cyst and the colloid cyst constitute a same entity? Acta Neurochir (Wien) 1995;133:174–180. doi: 10.1007/BF01420070. [DOI] [PubMed] [Google Scholar]
- Malcolm G P, Symon L, Kendall B, Pires M. Intracranial neurenteric cysts. J Neurosurg. 1991;75:115–120. doi: 10.3171/jns.1991.75.1.0115. [DOI] [PubMed] [Google Scholar]
- Wilkins R H, Odom G L. In: Vynken PJ, Bruyin GW, editor. Handbook of Clinical Neurology. Vol. 20. Amsterdam: North Holland; 1976. Spinal intradural cysts. pp. 55–102.
- Lantos P L, Louis D N, Rosenblum M K, Kleihues P. In: Graham DI, Lantos PL, editor. Greenfield's Neuropathology. 7th ed. Vol. 2. London: Arnold Publisher; 2002. Tumours of the nervous system. pp. 968–969.
- Perry A, Scheithauer B W, Zaias B W, Minassian H V. Aggressive enterogenous cyst with extensive craniospinal spread: case report. Neurosurgery. 1999;44:401–404. doi: 10.1097/00006123-199902000-00098. [DOI] [PubMed] [Google Scholar]
- Dadachanji M C, Dastur D K, Bhagwati S N, Manghani D K. Recurrent enterogenous cyst of the CP angle. Neurol India. 1994;42:160–162. [Google Scholar]
- Christov C, Chrétien F, Brugieres P, Djindjian M. Giant supratentorial enterogenous cyst: report of a case, literature review, and discussion of pathogenesis. Neurosurgery. 2004;54:759–763. doi: 10.1227/01.neu.0000109538.07853.7f. [DOI] [PubMed] [Google Scholar]
- Eynon-Lewis N J, Kitchen N, Scaravilli F, Brookes G. Neurenteric cyst of the cerebellopontine angle: case report. Neurosurgery. 1998;42:655–658. doi: 10.1097/00006123-199803000-00040. [DOI] [PubMed] [Google Scholar]
- Bavetta S, El-Shunnar K, Hamlyn P J. Neurenteric cyst of the anterior cranial fossa. Br J Neurosurg. 1996;10:225–227. doi: 10.1080/02688699650040430. [DOI] [PubMed] [Google Scholar]