Abstract
Breast cancer remains to be one of the most malignant diseases in the female population. It affects an essential part of female self-consciousness, and therefore causes a wide range of psychological traumas. The incidence in Europe and North America varies between 70 up to 100 new cases in 100.000 inhabitants per year. According to contemporary literature, mastectomy remains one of the most effective methods in the laborious effort to treat and overcome cancer. In this report the history of breast reconstruction is presented. The established methods which are taken into consideration after mastectomy and their clinical outcome are portrayed. The authors propose the free TRAM and DIEP flap as the methods of first choice after mastectomy, which offer most reliable transfer and low morbidity. In the recent past, increasing interest is observed for the SIEA flap. The free S-GAP flap is proposed for patients who are not candidates for a TRAM, DIEP or SIEA flap. Moreover, the pedicled Latissimus Dorsi flap remains still as a reliable, versatile alternative, particularly in case of contraindications for the above mentioned free flaps or when complications occurred.
Keywords: breast cancer, mastectomy, breast reconstruction, Latissimus Dorsi flap, TRAM flap, DIEP flap, SIEA flap
Introduction
Breast cancer remains to be one of the most malignant diseases in the female population. In contrast to other tumors, it affects an essential part of female self-consciousness, and therefore causes a wide range of psychological traumas. The incidence in Europe and North America varies between 70 up to 100 new cases in 100.000 inhabitants per year. According to statistics, one out of nine women will suffer from breast cancer in their lives1–3.
In the past, the diagnosis of breast cancer was associated with a radical mastectomy. In 1894 Halsted introduced this method as a standard treatment of mammary carcinoma4. In the course of time, a spread of highly mutilating operations was ascertained which cancer victims had to undergo. Over the years, other breast conserving methods were added. Today, in 75- 85% of all cases conservative surgery is preferred, especially because most tumors could be reduced in size by primary chemotherapy1. Breast-cancer-patients treated with conservative surgery followed by postoperative radiotherapy have nearly a similar prognosis to those treated with mastectomy only, with a crude rate of local recurrences of 23% vs. 24%5. The rate of local recurrences in breast cancer after post-mastectomy irradiation was only 4%. Therefore, many patients still receive mastectomy.
The first methods to reconstruct breasts after amputation reach back to the early 19th century. In 1897 Iginio Tansini was the first who transferred the Latissimus Dorsi muscle to cover chest wall defects that resulted from breast amputation6. Eight decades later Olivari rediscovered this method and covered radiation traumas as well as ulcers by transfers of a Latissimus Dorsi Myocutaneous Flap (LDMF)7.
Silicone implants for medical purpose were introduced in 1953. In 1971, Cronin and Gerow carried out the first attempts to reconstruct the shape of the female breast after mastectomy by the application of implants8, 9, which were partly replaced when in 1982 the tissue-expander-method began to achieve more successful results10.
Breast implants have aesthetic limitations, for example the way the reconstructed breast drapes on the chest or the possible loss of the inframammary fold by disruption of the inframammary crease ligament11. Temporary tissue expanders, introduced by Radovan, enable to form a breast mound with a more natural appearance by expansion of the remaining chest wall skin10. The expander is placed almost subpectorally, or in rare cases subcutaneously, and pumped up in 7-days intervals with normal saline. When a volume larger than that of the permanent prosthesis is achieved, it is replaced by a permanent implant in a second operation. Breast reconstruction with tissue expanders allows creating larger breasts and helps to avoid breast reduction on the healthy side. The appearance of capsule formations is rare, if the expander achieves a sufficient volume. The two-staged operation requires a longer hospitalization and recovery time. At least the surrounding of the implants always consists of silicone, which leads to implant-related complications like implant perforation, implant contracture, hematomas, infections, geometrical asymmetry, sensory changes and development of peri-implant capsules12, 13.
Increasing awareness of complications of silicone breast implants generated high interest in reconstruction based on autologous tissue. The choice of a particular method and donor site depends on the final breast volume, shape and softness, surgeon’s experience and preference, as well as the patient’s considerations.
Breast reconstruction with autologous tissue
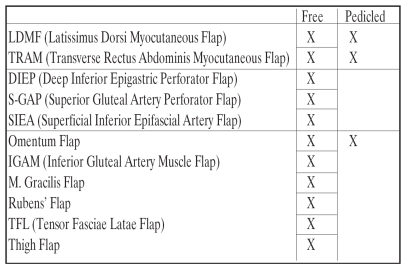
Herein, we intend to present solutions for breast reconstruction based on autologous tissue, mentioning advantages and disadvantages of each (Table 1).
Table 1. Well known flaps for breast reconstruction with autologous tissue.
The LDMF developed by Iginio Tansini in 18976and used by Olivari in 1976 to cover irradiation ulceras7was introduced by Mühlbauer and Olbrisch for breast reconstruction in 197714. Since augmentation with the LDMF creates smaller breasts, it is required to set supplementary breast implants in some cases. In 1979, Holmström reconstructed breasts using the free TRAM flap, thus receiving more volume and sufficient blood supply in the donor region15. His method asserted in breast reconstructive surgery.
Among the possibilities for breast reconstruction there is the transfer of tissue from adjacent regions to the breast, keeping up the original blood supply (pedicled flaps). Possible donor regions are the LDMF (from the back) or the myocutaneous Rectus Abdominis flap (from the abdominal wall), which has surpassed the LDMF in the preferred adjustment due to the versatility and large quantity of available tissue16, e.g. in thin patients17.
Tissue transfer in breast reconstructive surgery can also be performed in form of free flaps, in which blood supply has to be reestablished by vascular microanastomosis at the recipient site. The most popular and reliable free flaps are the free Transverse Rectus Abdominis Myocutaneous flap (free TRAM) and the free Deep Inferior Epigastric Perforator flap (DIEP)18. Other free flaps are taken from the gluteal region as the S-GAP flap, from the thigh or the omentum16. Recent methods, as the Superficial Inferior Epigastric Artery flap (SIEA), provide sufficient blood-supply and minimize donor site morbidity, since no fascia incision has to be performed19.
Latissimus Dorsi Myocutaneous Flap (LDMF)
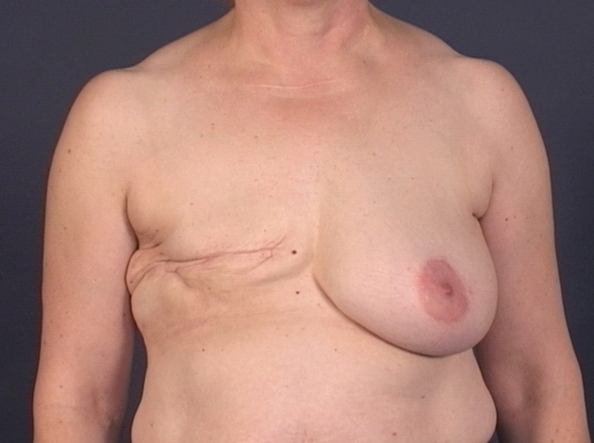
The LDMF bases on the triangular-shaped Latissimus Dorsi muscle20 and includes the skin and its fat tissue. Two vascular systems supply the LDMF. The muscle itself is supplied by the thoracodorsal vessels which branch from the subscapular vessels distal to the circumflex scapular vessels. The subscapular vessels come from the axillar vessels. The flap’s blood supply also arises from myocutaneous perforators which are branches of the intercostal and lumbar vessels. For breast reconstruction the LDMF is described either as a pedicled or a free flap, however, mostly used as a pedicled flap (Figure 1a and b).
Figure 1a and b. a) Appearance of the breast after radical mastectomy on the left side. b) Final result after breast reconstruction on the left side using an LDMF and reconstruction of the nipple-areola complex. Contralateral side was adapted to the reconstructed one by reduction mammaplasty.
After an incision posterior to the lateral border of the Latissimus Dorsi muscle in posterioinferior direction16, the muscle is elevated, and the space between it and the underlying serratus anterior muscle is enlarged by blunt dissection. At the upper lateral edge of the muscle the thoracodorsal vessels can be found. The branches from the thoracodorsal muscle to the serratus anterior muscle must be ligated. The circumflex scapular artery must be carefully preserved. After ligating all branches from the intercostals arteries, the whole muscle is harvested off the back and pleated under the axilla, passed through a tunnel between the two wound areas and brought to the place of the mastectomy. Then the flap is brought into position and the recipient area is sutured (Figure 1a and b).
The LDMF is a very reliable and versatile method, and thus, the workhorse for breast reconstruction. Often it is performed on patients with previous abdominal operations or contraindications for other free or pedicled flaps. Possible complications are seroma and flap necrosis21. The loss of the Latissimus Dorsi muscle in the back, however, leads to deficits in extension and adduction3. Mostly athletes, patients who use crutches or wheelchair bounded are affected in terms of a faster rate of fatigue during activities16. The LDMF is shown disadvantageous due to the need of implants in cases when greater breasts are desired, accompanied by the risk of the development of all the above mentioned implant-related complications12. An extended latissimus dorsi myocutaneous (ELD-MC) flap with some amount of surrounding subcutaneous fat from the lumbar area can sometimes avoid the use of any implant. Additional fat tissue can also be harvested subcutaneously at right angle in continuity with the usual LDMF, imitating the pattern of a lily flower, in French called "fleur de lis"22, a technically simple method which permits improved volume and projection in the inferior pole of the breast.
Transverse Myocutaneous Rectus Abdominis Flap (TRAM):
The skin island for the TRAM flap is taken out between the umbilicus, pubic region and from the front of the iliac bone16. Skin and fat tissue are supplied by perforators through the rectus abdominis muscle. The muscle has a dual blood supply, i.e. the deep, superior and inferior epigastric vessels. The TRAM flap can be performed as well in a free microvascular as in a pedicled form. In the pedicled form, the caudal muscle part is detached. Still left connected to the rest of the muscle, the flap is then placed upwards to the mastectomy site.
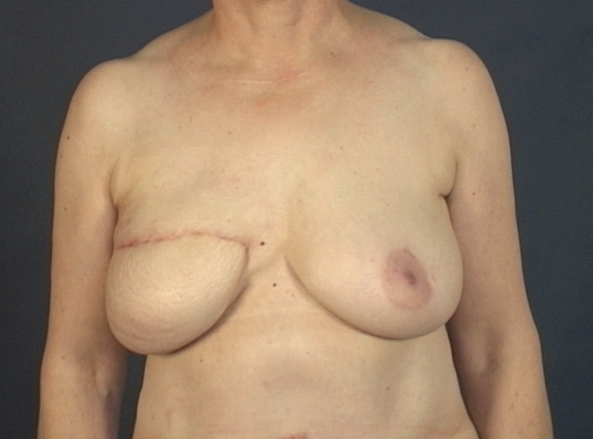
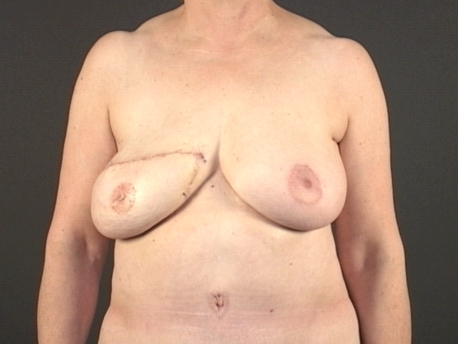
As a free microvascular flap the TRAM flap is harvested with a small cuff of the rectus abdominis muscle and brought to the mastectomy site. The blood supply is reestablished by microsurgical anastomosis between the pedicle of the deep inferior epigastric vessels and the vessels from the breast area. Normally, the thoracodorsal or internal thoracic vessels are chosen as recipients. Although just a small part of the muscle is taken out with the perforators of the inferior epigastric vessels, an optimal vascularity of the tissue is guaranteed23The abdominal fault is reconstructed by fascial duplication of the rectus abdominis muscle sheath, as well as by epifascial decrease at the abdominal wall cranial of the umbilicus, in accordance with an abdominoplasty19 (Figure 2, 3, 4a and b).
Figure 2. Example of postmastectomy appearance of the breast.
Figure 3. Same patient as in figure 2 after breast reconstruction with a free TRAM flap.
Figure 4a. a) Postoperative appearance after unilateral reconstruction with free TRAM flap and reconstruction of the nipple areola complex.
Figure 4b. b) Postoperative appearance of donor region.
Breast reconstruction with free or pedicled TRAM flaps has shown excellent results and has become the method of choice in breast reconstruction with autologous tissue. Compared to the pedicled TRAM flap, reconstruction of breasts with the free TRAM flap offers a lower complication rate at the mastectomy site, and a low donor site morbidity rate24.Pedicled and free TRAM flaps allow a more reliable transfer of large tissue, and thus, reconstruction of larger breasts than with LDMF flaps (Figure 2, 3, 4a and b), and simultaneous bilateral reconstruction (Figure 5a and b). The pedicled and free TRAM flap is similar to the natural breast in softness and in the way the tissue drapes on the chest25 (Figure 3, 4a,5b). The major disadvantages of breast reconstructions with TRAM flaps in general are a relatively long operative time and thus the need of blood transfusions. Thus, the operation itself can unmask a cardiopulmonal disease, which will even be more important in obese patients26. In the past, there were concerns that abdominal liposuction could destroy the musculocutaneous perforator vessels and thus make them inapplicable for a TRAM flap. Though, several studies show successfully performed breast reconstructions with TRAM flaps in patients with history of abdominal liposuction27, 28, if the perforators are not disrupted. Similarly, the DIEP flap is also taken into consideration after cosmetic procedures of the abdomen29. The TRAM flap is not proper for patients who consider to birth children because of the diminished compliance of the abdominal wall. The lack of abdominal tissue in very thin patients is another contraindication for the TRAM flap19.
Figure 5a. a) Preoperative views after bilateral mastectomy. [Reproduced with the permission of Annals of Plastic Surgery: Kovacs L, et al: Clinical Outcome and Patients_ Satisfaction after Simultaneous bilateral Breast Reconstruction with free Transverse Rectus Abdominis Muscle (TRAM) flap. Ann Plast Surg 2004; 53(3):199-204].
Figure 5b. b) The appearance of the breast after bilateral reconstruction with free TRAM flaps and reconstruction of the nipple areola complex. [Reproduced with the permission of Annals of Plastic Surgery: Kovacs L, et al: Clinical Outcome and Patients_ Satisfaction after Simultaneous bilateral Breast Reconstruction with free Transverse Rectus Abdominis Muscle (TRAM) flap. Ann Plast Surg 2004; 53(3):199-204].
After breast reconstruction with a TRAM flap, the development of herniation as well as of defects in the harvested region has to be taken into consideration. The incidence of epigastric fullness, upper bulge, lower bulge, and hernia is higher in women who had a pedicled TRAM flap in comparison to those who got a free TRAM operation30, 31. On the other hand, postoperative abdominal strength, as measured by the ability do situps, is influenced significantly by the type of TRAM flap (pedicled or free TRAM flap) and the number of muscle pedicles harvested32. Patients reconstructed with a free TRAM are more likely to be able to do sit-ups (58.3%) than were those with a pedicled TRAM (38.2%). Patients, who had only one muscle pedicle used, are more likely to be able to do sit-ups (61.7%) than were those, who had more pedicles used (35.6%). The risk of subsequent hernia formation can be minimised, if the anterior rectus sheath is repaired by a patch after harvesting33.
A method to reduce donor site morbidity is the muscle-sparing free TRAM (MS-2)18,23. Taken out with just a small plug of muscle, it maintains the vascularity, innervation and continuity of the rectus abdominis muscle and offers minimal function loss23, 34.
Deep Inferior Epigastric Perforator Flap (DIEP)
In 1994, Allen and Treece proposed the free DIEP flap for autologous tissue reconstruction35. Perforator flaps base on abdominal fat and skin, and on one to three musculocutaneous perforators, which supply the soft tissue of the skin paddle through the muscle, in case of the DIEP flap through the rectus abdominis muscle. The DIEP flap requires at least one large perforator or two substantial perforators in the lateral row to survive36. Its perforators originate from the deep inferior epigastric vessels. The muscle is dissected to gain access to the main vascular pedicle, but not sacrificed by harvesting the flap. This affords a long vascular pedicle, which directly enters the skin paddle. As a versatile alternative to the traditional free TRAM flap and LDMF, the DIEP flap offers the preservation of the rectus abdominis muscle and its anterior rectus sheath, thus reducing abdominal morbidity such as hernia, weakness and bulge (0.7%)37. Hamdi et al. have shown a complete return of lower rectus function with the free DIEP flap after only 3 months38. Additionally, the DIEP flap offers a reconstructive method applicable to bilateral reconstructions. Finally, recovery is quicker and hospital stay is reduced in comparison to TRAM flaps39.
As to TRAM flap, the DIEP flap is only a relative contraindication for patients with a lack of abdominal tissue and patients with a prior liposuction of the abdomen or other previous abdominal surgery28, 29. Disadvantages of the flap are a longer operative time due to a more meticulous dissection than in free TRAM flap operations18. The fact that the DIEP flap bases on only up to three perforators might be disadvantageous for the flap’s blood supply in comparison to the TRAM40. Diffuse venous insufficiency appears more often in DIEP than in TRAM flaps and requires a microvascular anastomosis to drain the superficial inferior epigastric vein. Consequently, preoperative planning remains of high importance.
Superior Gluteal Artery Perforator Flap (S-GAP)
In 1975, Fujino first described the superior gluteal myocutaneous free flap for breast reconstruction41. The flap extends from the trochanter major of the femur to the posterior superior iliac spine. The skin island is taken out with the superior gluteal vessels which emerge in the upper third. These vessels are dissected through the retracted gluteus maximus muscle. Most superior gluteal flaps are performed on patients with contraindications for a TRAM or DIEP flap, i.e. prior abdominal liposuction or other previous abdominal surgery that has damaged or interrupted the blood supply to the TRAM or DIEP flap28, obesity42, and patients with a lack of tissue in the lower abdominal area19. The S-GAP causes minimal donor muscle morbidity. The scar is inconspicious and the donor site can be primarily closed43, and there is no violation of the abdominal wall, eliminating the possibility of postoperative bulges or hernias. Thus, it is performed on patients who consider getting pregnant44. A transfer of bilateral S-GAP flaps can be offered to patients who desire a one-stage bilateral breast reconstruction with highly esthetic results and acceptable overall morbidity45. In case of a short pedicle, the use of thoracodorsal vessels as recipient vessels leads to either excess lateral fullness or inadequate medial fullness46.These problems may be avoided using the internal mammary vessels instead. A sufficient pedicle length can be obtained by resecting the third costal cartilage. Although the scar can be positioned in the bikini line, often a contour deformity results, which can be disfiguring. Also, asymmetry remains a possible complication that should require subsequent refinements when one-side reconstruction is performed.
Superficial Inferior Epigastric Artery Flap (SIEA-flap)
The procedure is similar to the DIEP flap, but with different arterial supply and venous drainage47. The SIEA flap relies on superficial inferior epigastric vessels just below the skin surface. Thus, unlike the DIEP flap, the harvest of the SIEA flap does not injure the anterior rectus abdominis fascia or the muscle36, providing a minimization of donor site morbidity such as bulge and hernia formation. Nonetheless, the SIEA carries the same volume, texture and colour of tissue as the free TRAM or DIEP flap48.
On that account, the SIEA flap is of increasing importance in many centers. Disadvantages are the smaller pedicle diameter and shorter pedicle length than in TRAM and DIEP flap. Unlike the internal mammary vessels, the pedicle length and size may be insufficient when the subscapular vascular axis is selected as the recipient, making the use of vein grafts mandatory48, 49.A lot of patients are not candidates for SIEA flaps because of the inconsistent vascular pedicle anatomy, small pedicle diameter and the short pedicle length (about 7cm)36,resulting in an inadequacy of the arterial pedicle. About 70% of the patients have suitable superficial blood vessels for this operation47. Preoperatively, an exact examination of the abdominal vessels is obligatory to determine, if the patient complies the requirements for an SIEA flap or not. However, if unsuitable perforators are noticed no more than during the operation, the SIEA can be converted into a TRAM or DIEP flap.
Omentum flap
The omentum flap is available as a pedicle or a free flap and is mostly of historical relevance. The omentum can be transferred to a subcutaneous position where an omental skin flap can be prefabricated. Free tissue transfer is performed by using the gastroepiploic vessels for microanastomosis50.
Other flaps
For the sake of completeness one should name the Inferior Gluteal Artery Muscle flap (IGAM)51, the M. gracilis-52, the Rubens-53, the Tensor fasciae latae (TFL) and the Thigh flap54, 55, which are being used under special circumstances or are of historical relevance.
Refinements in breast reconstruction
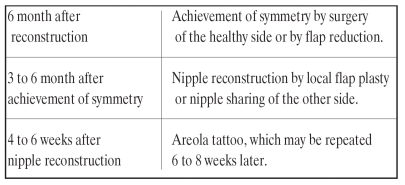
In most cases secondary procedures in breast reconstructive surgery are needed, aiming to an as close as possible natural appearance. In our department following algorithm for refinements after breast reconstruction is used56 (Table 2).
Table 2. Algorithmn for refinements after breast reconstruction.
The reconstruction of greater breasts requires a more demanding approach due to the difficulty to form a breast with the same mass as the healthy one. In most cases the reduction of the healthy breast side is performed to achieve symmetry. Because breasts get their final form approximately 3 to 6 months after surgery, it is mostly convenient to perform these procedures afterwards.
Rarely, the flap has to be reduced or the shape of the reconstructed breast has to be corrected. It is of prime importance to control and keep up the blood supply of the flap. Therefore it is recommendable to carry out such correcting operations not earlier than 3 months - or better 6 months after the previous operation.
After symmetry is achieved, the nipple has to be reconstructed. Several methods are applicable, e.g. the tristar-flap, providing just small defects in the donor region56, or sharing a part of a large controlateral nipple with the reconstructed breast. That yields good results, since shared nipples do not tend to shrink, contrary to local flap plasty.
At last, the reconstruction of the areola is performed after 4 to 6 weeks. Earlier, grafts were used from the groin or the pudendal lips, causing painful donor site defects and the impossibility to influence the final color. Today it is possible to shape position, form and color of areola by tattoo (Fig. 4a & 5b).
Refinements are of great importance for achieving a satisfactory aesthetic result and the completeness of breast reconstruction. The highest subjective satisfaction scores were described to be given to the natural appearance i.e. the color, shape and mobility of the reconstructed breast, the lowest to sensibility and the scar at the donor site24. Secondary interventions, however, give a result more compatible with the natural female appearance, and thus help to increase the patients' satisfaction.
Discussion
The main aim in breast reconstruction is to create a breast, which offers softness, symmetry, sensibility, aesthetically acceptable scars, as well as texture and color similar to the healthy side. The optimal method should offer a result that makes the patient feel as natural as possible. It should be safe, reliable, and accompanied by little donor-site morbidity. By achieving an acceptable appearance, reconstruction of the breast should improve the patients’ quality of life and offer no subsequent health risk24, 25. Because of the patients' different ideas as to their own physical appearance, a suitable reconstruction method with the possibility for individual adjustment is required. Increasing awareness of implant-related complications generated high interest in breast reconstruction with autologous tissue12, 57–61.
Before performing breast reconstruction, some important factors have to be considered, which require clarification for avoidance of postoperative complications. These are smoking62, obesity63, postoperative irradiation64, the stage and the location of cancer, the patients' age and her expectations. Breast reconstruction with free flaps as the free TRAM flap in smokers is not associated with a significant increase of the rates of vessel thrombosis, flap loss or fat necrosis compared with nonsmokers62. However, smokers are at significantly higher risk for mastectomy skin flap necrosis, abdominal flap necrosis, and hernia. Smoking-related complications can be reduced when patients stop smoking at least 4 weeks before reconstruction. The majority of overweight patients who undertake breast reconstruction with free TRAM flaps complete the reconstruction successfully63. Nevertheless, obese patients have a significantly higher rate of flap complications (i.e. flap loss, seroma, necrosis etc.) and donor-site complications (i.e. infection, seroma, hernia etc.). Postmastectomy irradiation does not significantly affect the rate of partial or total free-flap loss65. The over-all complication rate in the reconstructed breast is higher in irradiated patients than in non-irradiated (39% vs. 25%) and the aesthetic outcome is also slightly poorer. Thus, irradiated patients should consider a delayed reconstruction.
In the past, several studies tried to evaluate the quality of operations, the patients' satisfaction and quality of life after reconstruction24, 25, 66, 67. The fact that surgical results are difficult to be recognized on the base of quantitative figures led to several studies trying to evaluate the patients’ quality of life by using questionnaires or patients'long-term observations. Long-term outcomes of the most applied reconstructive methods - free TRAM flap and expander/implant - did not show any significant differences in the quality of life between patients, who had received breast reconstruction, and healthy women25. However, women with TRAM-based reconstructed breasts achieved an improvement of their quality of life. Naturally, the evaluation regarding the quality of life and the potential improvement after a mastectomy depends on women’s expectation24, 25. Patients’ unrealistic expectations like keeping in mind the breast they had before and disregarding the limitations of surgery may influence their satisfaction.
Another parameter to evaluate the success of reconstructive procedures is the screening of symmetry of the breasts. Sometimes symmetry is obtained by a single procedure. In contrast to implant-based reconstructions, secondary procedures as reduction mammaplasty, mastopexy etc. are often required in reconstructions using autologous tissue68. The role of three-dimensional photography is getting increasingly important for discerning accurate symmetry68–70.
The priority in each breast reconstruction must be the preservation of the patients’ health and quality of life. All the procedures should consider the needs and expectations of the individual patient and their effects on the patient’s lifestyle. The LDMF is one of the most reliable and versatile reconstructive methods and still the method of first choice when free flaps are contraindicated or when complications occured17 (Figure 1a and b). However, the LDMF is hitting its bounds of possibilities in reconstructing larger breasts and has to be combined with implants to achieve enough volume. This increases the risk of above mentioned implant-related complications and makes the breast feel different from the healthy side. The use of any implant can eventually be avoided by an ELD-MC flap12, 71 or the harvest of adjacent subcutaneous fat by an LDMF with fleur-de-lis-pattern22.
TRAM and DIEP flaps are good alternatives for patients who are unsuitable for implants or who have failed such an operation72, 73Even in case of reconstructing a large breast, the TRAM or the DIEP flap can create a ptotic, soft and symmetrical breast mound with a more naturally looking inframammay fold (Figure 3, 4a4a,5b) in comparison to a breast reconstructed with an implant18, 25. The reconstructed breast drapes similarly to the natural one on the chest and the flap shows a satisfactory long term result16, 25, 64. Besides, the abdominal fault is corrected in accordance with an abdominoplasty within a TRAM or DIEP procedure (Figure 4b). Intraoperatively, patients need not to be turned around in TRAM or DIEP reconstructions, as in LDMF or S-GAP flap operations, thus making bilateral reconstructions easier without loosing precious time 24.
The TRAM flap can be performed as a pedicled or a free flap. Compared to the pedicled TRAM flap, reconstruction of breasts with the free TRAM flap offers a lower complication rate24. However, the free TRAM flap provides a better blood supply and survival rate of the reconstructed breast than the free DIEP flap18, 74which bases on only up to 3 perforators35. In contrast, the free TRAM flap is harvested with a small cuff of the rectus abdominis muscle16, which includes almost all the perforators and offers excellent vascularity. This results in a secure flap transfer, and therefore, in higher patient’s satisfaction25. Both methods require high microsurgical experience and standards, and thus longer operative times than LDMF flap operations. The DIEP flap requires a more meticulous technique and longer operative time in comparison to the TRAM flap. A higher incidence of fat necrosis and venous congestion than in TRAM flaps, which can lead to total flap loss, threatens the DIEP flap’s survival40, 74. The benefits of DIEP flaps regard the abdominal wall, because no muscle is taken out when the flap is harvested. Of course the muscle is dissected to gain access to the perforators and the pedicle, but both, the muscle and the anterior rectus sheath are completely preserved35, 74. Thus, the abdominal morbidity such as hernia, weakness or bulge is reduced, compared to the TRAM flap, and a complete return of the lower rectus function after only 3 months can be achieved37–39. Consequently, the DIEP flap is highly indicated for bilateral reconstruction.
Our investigations led to the result that reconstructions with free TRAM and DIEP flap are the methods of choice. The selection of the free TRAM or DIEP flap should be made on the basis of the patient’s weight, amount of abdominal fat, required breast volume, the patient’s vascular anatomy, i.e. the number, diameter and location of the perforating vessels, and the surgeon’s experience74. These methods require high microsurgical skills and standards, and thus, long operative times.
In case the free TRAM or the DIEP flap is not applicable, the S-GAP flap can be recommended. Most S-GAP flaps are performed on patients who have relative contraindications for a TRAM flap, i.e. a prior liposuction of the abdomen, or other procedures which could have damaged or interrupted the blood supply to the free TRAM or DIEP flap28. Therefore, the evaluation of the abdominal perforator status (pre-operative duplex scan examination) is very important in the planning of TRAM or DIEP flap. Other contraindications are scars in the abdominal area, obesity that may unmask cardiopulmonal diseases due to the long operative times19, 42, and little tissue in the lower abdominal area41. Due to the diminished compliance of the abdominal wall after a TRAM or DIEP operation, the patient’s wish to birth more children might be a further contraindication44.
A method of recent interest is the SIEA flap that is harvested with minimal donor site morbidity and offers similar aesthetic results as TRAM and DIEP flap. Its harvest does not injure the anterior rectus abdominis fascia and the underlying rectus abdominis muscle36, because it relies on the superficial inferior epigastric vessels just below the skin. That is why the SIEA flap provides sufficient blood-supply as well as minimization of donor site morbidity, such as bulge and hernia formation47. Regrettably, many patients have inadequate arterial pedicles36. In case of unsuitable perforators however, the SIEA can be converted into a TRAM or DIEP flap intraoperatively.
The remaining methods mentioned are being used under special circumstances or are of historical significance only (Omentum-flap)16, 50–55.
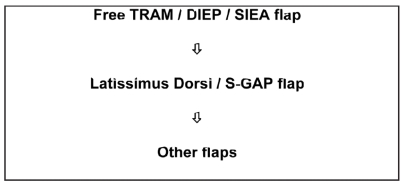
We propose the free TRAM, DIEP- and SIEA flap as the methods of first choice after mastectomy, which offer most reliable transfer and low morbidity, depending on surgeon’s microsurgical experience and patients’ conditions. The free S-GAP flap is proposed for patients who are not candidates for a free TRAM, DIEP and SIEA flap or failed the TRAM, DIEP or SIEA operation. Moreover, the LDMF remains still as a reliable and versatile method, particularly in case of contraindications of the above mentioned free flaps or when complications occurred (Table 3).
Table 3. Algorithm for the usage of autologous tissue in breast reconstruction.
Within the bounds of breast reconstruction all the above mentioned interventions are very important for the affected women’s satisfaction24, 25. Regardless of the method preferred, surgeons and patients have to consider refinements after the operation, if complications or non-satisfying results occur. Three to six months after the operation, the reconstructed breast can be adapted to the other side with the help of secondary interventions and thus induce patients to appreciate their own appearance and become more self-confident56. In that way a result more compatible with the natural female appearance can be achieved. This helps to take away women’s feeling of mutilation after mastectomy, and thus, to rebuild their self-confidence and make them live without feeling a loss of their femininity.
References
- 1.Veronesi U, Boyle P, Goldhirsch A, Orecchia R, Viale G. Breast cancer. Lancet. 2005;365:1727–1741. doi: 10.1016/S0140-6736(05)66546-4. [DOI] [PubMed] [Google Scholar]
- 2.Laffer U, Harder F, Almendral AC, et al. Breast preserving therapy of breast carcinoma: analysis of over 1,300 patients treated in the Basel region. Zentralbl Chir. 1997;122:79–85. [PubMed] [Google Scholar]
- 3.Scott S, Morrow M. Breast cancer. Making the diagnosis. Surg Clin North Am. 1999;79:991–1005. doi: 10.1016/s0039-6109(05)70057-8. [DOI] [PubMed] [Google Scholar]
- 4.Halsted W. The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907;46:1–19. doi: 10.1097/00000658-190707000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fodor J, Mozsa E, Zaka Z, Polgar C, Major T. Local relapse in young (</=40 years) women with breast cancer after mastectomy or breast conserving surgery: 15-year results. Magy Onkol. 2005;49:203–208. [PubMed] [Google Scholar]
- 6.Maxwell GP. Iginio Tansini and the origin of the latissimus dorsi musculocutaneous flap. Plast Reconstr Surg. 1980;65:686–692. doi: 10.1097/00006534-198005000-00027. [DOI] [PubMed] [Google Scholar]
- 7.Olivari N. The latissimus flap. Br J Plast Surg. 1976;29:126–128. doi: 10.1016/0007-1226(76)90036-9. [DOI] [PubMed] [Google Scholar]
- 8.Cronin TD, Brauer RO. Augmentation mammaplasty. Surg Clin North Am. 1971;51:441–452. doi: 10.1016/s0039-6109(16)39388-4. [DOI] [PubMed] [Google Scholar]
- 9.Gerow FJ, Spira M, Hardy SB. Plastic surgery applications of synthetic implants. Med Instrum. 1973;7:96–99. [PubMed] [Google Scholar]
- 10.Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982;69:195–208. doi: 10.1097/00006534-198202000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Bayati S, Seckel BR. Inframammary crease ligament. Plast Reconstr Surg. 1995;95:501–508. doi: 10.1097/00006534-199503000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Sakai S, Ando K, Natori M. Cosmetic reconstruction after resection of breast cancer: use of the ELD-MC flap and EVRAM flap. Int J Clin Oncol. 2005;10:298–303. doi: 10.1007/s10147-005-0523-8. [DOI] [PubMed] [Google Scholar]
- 13.Biemer E. Breast reconstruction only by implant of a silicone gel prosthesis, possibly following tissue stretching by an expander. Chirurg. 1989;60:611–613. [PubMed] [Google Scholar]
- 14.Muhlbauer W, Olbrisch R. The latissimus dorsi myocutaneous flap for breast reconstruction. Chir Plastica. 1977;4:27. [Google Scholar]
- 15.Holmstrom H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13:423–427. doi: 10.3109/02844317909013092. [DOI] [PubMed] [Google Scholar]
- 16.Graf K, Gröner P, Brunner C, Müller D, Hönke C, Biemer E. Breast reconstruction with autologous tissue after mastectomy. Münch med Wschr. 1998;140:260–264. [Google Scholar]
- 17.Kronowitz SJ, Robb GL, Youssef A, et al. Optimizing autologous breast reconstruction in thin patients. Plast Reconstr Surg. 2003;112:1768–1778. doi: 10.1097/01.PRS.0000090541.54788.AD. [DOI] [PubMed] [Google Scholar]
- 18.Tachi M, Yamada A. Choice of flaps for breast reconstruction. Int J Clin Oncol. 2005;10:289–297. doi: 10.1007/s10147-005-0527-4. [DOI] [PubMed] [Google Scholar]
- 19.Allen RJ, Heitland AS. Autogenous augmentation mammaplasty with microsurgical tissue transfer. Plast Reconstr Surg. 2003;112:91–100. doi: 10.1097/01.PRS.0000066006.07602.86. [DOI] [PubMed] [Google Scholar]
- 20.Bostwick J, 3rd, Nahai F, Wallace JG, Vasconez LO. Sixty latissimus dorsi flaps. Plast Reconstr Surg. 1979;63:31–41. doi: 10.1097/00006534-197901000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Moore TS, Farrell LD. Latissimus dorsi myocutaneous flap for breast reconstruction: long-term results. Plast Reconstr Surg. 1992;89:666–672. discussion 673-664. [PubMed] [Google Scholar]
- 22.Aitken ME, Mustoe TA. Why change a good thing? Revisiting the fleur-de-lis reconstruction of the breast. Plast Reconstr Surg. 2002;109:525–533. doi: 10.1097/00006534-200202000-00018. discussion 534-528. [DOI] [PubMed] [Google Scholar]
- 23.Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg. 2005;115:436–444. doi: 10.1097/01.prs.0000149404.57087.8e. discussion 445-436. [DOI] [PubMed] [Google Scholar]
- 24.Kovacs L, Papadopulos NA, Ammar SA, et al. Clinical outcome and patients' satisfaction after simultaneous bilateral breast reconstruction with free transverse rectus abdominis muscle (TRAM) flap. Ann Plast Surg. 2004;53:199–204. doi: 10.1097/01.sap.0000120525.86997.52. [DOI] [PubMed] [Google Scholar]
- 25.Papadopulos NA, Kovacs L, Baumann A, et al. Quality of life and patient satisfaction after breast reconstruction. Chirurg. 2006;77:610–615. doi: 10.1007/s00104-005-1147-2. [DOI] [PubMed] [Google Scholar]
- 26.Baldwin BJ, Schusterman MA, Miller MJ, Kroll SS, Wang BG. Bilateral breast reconstruction: conventional versus free TRAM. Plast Reconstr Surg. 1994;93:1410–1416. discussion 1417. [PubMed] [Google Scholar]
- 27.Ribuffo D, Marcellino M, Barnett GR, Houseman ND, Scuderi N. Breast reconstruction with abdominal flaps after abdominoplasties. Plast Reconstr Surg. 2001;108:1604–1608. doi: 10.1097/00006534-200111000-00026. [DOI] [PubMed] [Google Scholar]
- 28.Hess CL, Gartside RL, Ganz JC. TRAM flap breast reconstruction after abdominal liposuction. Ann Plast Surg. 2004;53:166–169. doi: 10.1097/01.sap.0000112289.88210.32. [DOI] [PubMed] [Google Scholar]
- 29.Fabre G, Vranckx J, Massage P, Vandevoort M. Deep inferior epigastric perforator flap for breast reconstruction after cosmetic procedures of the abdomen. Personal Communication at the III Congress of the World Society for Reconstructive Microsurgery; October 23-26, 2005; Buenos Aires, Argentina. 2005. [Google Scholar]
- 30.Nahabedian MY, Dooley W, Singh N, Manson PN. Contour abnormalities of the abdomen after breast reconstruction with abdominal flaps: the role of muscle preservation. Plast Reconstr Surg. 2002;109:91–101. doi: 10.1097/00006534-200201000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Feller AM, Horl HW, Biemer E. The transverse rectus abdominis musculocutaneous free flap: a reliable alternative for delayed autologous tissue breast reconstruction. Ann Plast Surg. 1990;25:425–434. doi: 10.1097/00000637-199012000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Kroll SS, Schusterman MA, Reece GP, Miller MJ, Robb G, Evans G. Abdominal wall strength, bulging, and hernia after TRAM flap breast reconstruction. Plast Reconstr Surg. 1995;96:616–619. doi: 10.1097/00006534-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Pennington DG, Lam T. Gore-Tex patch repair of the anterior rectus sheath in free rectus abdominis muscle and myocutaneous flaps. Plast Reconstr Surg. 1996;97:1436–1440. doi: 10.1097/00006534-199606000-00019. discussion 1441-1432. [DOI] [PubMed] [Google Scholar]
- 34.Plogmeier K, Schneider W, Jost S, Feistner H, von Rohden L, Fessel L. Myosonographic and electromyographic (EMC) evaluation of donor-site morbidity after microsurgical TRAM flap. Handchir Mikrochir Plast Chir. 2003;35:43–50. doi: 10.1055/s-2003-39556. [DOI] [PubMed] [Google Scholar]
- 35.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. doi: 10.1097/00000637-199401000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Chevray PM. Breast reconstruction with superficial inferior epigastric artery flaps: a prospective comparison with TRAM and DIEP flaps. Plast Reconstr Surg. 2004;114:1077–1083. doi: 10.1097/01.prs.0000135328.88101.53. discussion 1084-1075. [DOI] [PubMed] [Google Scholar]
- 37.Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004;113:1153–1160. doi: 10.1097/01.prs.0000110328.47206.50. [DOI] [PubMed] [Google Scholar]
- 38.Hamdi M, Weiler-Mithoff EM, Webster MH. Deep inferior epigastric perforator flap in breast reconstruction: experience with the first 50 flaps. Plast Reconstr Surg. 1999;103:86–95. doi: 10.1097/00006534-199901000-00015. [DOI] [PubMed] [Google Scholar]
- 39.Blondeel PN. One hundred free DIEP flap breast reconstructions: a personal experience. Br J Plast Surg. 1999;52:104–111. doi: 10.1054/bjps.1998.3033. [DOI] [PubMed] [Google Scholar]
- 40.Blondeel PN, Arnstein M, Verstraete K, et al. Venous congestion and blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:1295–1299. doi: 10.1097/00006534-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Fujino T, Harasina T, Aoyagi F. Reconstruction for aplasia of the breast and pectoral region by microvascular transfer of a free flap from the buttock. Plast Reconstr Surg. 1975;56:178–181. doi: 10.1097/00006534-197508000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Moran SL, Serletti JM. Outcome comparison between free and pedicled TRAM flap breast reconstruction in the obese patient. Plast Reconstr Surg. 2001;108:1954–1960. doi: 10.1097/00006534-200112000-00017. discussion 1961-1952. [DOI] [PubMed] [Google Scholar]
- 43.Biemer E, Steinau HU. Brustrekonstruktion mit freiem oberen myokutanen Gluteallappen mit mikrovaskulärer Anastomose. [Breast reconstruction using a free upper myocutaneous gluteal flap with microvascular anastomoses]. Chirurg. 1989;60:625–626. (Ger). [PubMed] [Google Scholar]
- 44.Shaw WW. Superior gluteal free flap breast reconstruction. Clin Plast Surg. 1998;25:267–274. [PubMed] [Google Scholar]
- 45.Guerra AB, Soueid N, Metzinger SE, et al. Simultaneous bilateral breast reconstruction with superior gluteal artery perforator (SGAP) flaps. Ann Plast Surg. 2004;53:305–310. doi: 10.1097/01.sap.0000128619.83670.e1. [DOI] [PubMed] [Google Scholar]
- 46.Allen RJ. The superior gluteal artery perforator flap. Clin Plast Surg. 1998;25:293–302. [PubMed] [Google Scholar]
- 47.Allen R, Heitland A. Superficial inferior epigastric artery flap for breast reconstruction. Seminars in plastic surgery. 2002;16:35–43. [Google Scholar]
- 48.Arnez ZM, Khan U, Pogorelec D, Planinsek F. Breast reconstruction using the free superficial inferior epigastric artery (SIEA) flap. Br J Plast Surg. 1999;52:276–279. doi: 10.1054/bjps.1999.3100. [DOI] [PubMed] [Google Scholar]
- 49.Volpe AG, Rothkopf DM, Walton RL. The versatile superficial inferior epigastric flap for breast reconstruction. Ann Plast Surg. 1994;32:113–117. doi: 10.1097/00000637-199402000-00001. [DOI] [PubMed] [Google Scholar]
- 50.Jimenez AG, St Germain P, Sirois M, Hatheway M, Lethbridge R. Free omental flap for skin-sparing breast reconstruction harvested laparoscopically. Plast Reconstr Surg. 2002;110:545–551. doi: 10.1097/00006534-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 51.Paletta CE, Bostwick J, 3rd, Nahai F. The inferior gluteal free flap in breast reconstruction. Plast Reconstr Surg. 1989;84:875–883. discussion 884-875. [PubMed] [Google Scholar]
- 52.Peek A, Muller M, Exner K. Der freie Grazilis-Perforator-Lappen zur autologen Brustrekonstruktion [The free gracilis perforator flap for autologous breast reconstruction] Handchir Mikrochir Plast Chir. 2002;34:245–250. doi: 10.1055/s-2002-36292. [DOI] [PubMed] [Google Scholar]
- 53.Elliott LF, Hartrampf CR., Jr The Rubens flap. The deep circumflex iliac artery flap. Clin Plast Surg. 1998;25:283–291. [PubMed] [Google Scholar]
- 54.Elliott LF, Beegle PH, Hartrampf CR., Jr The lateral transverse thigh free flap: an alternative for autogenous-tissue breast reconstruction. Plast Reconstr Surg. 1990;85:169–178. discussion 179-181. [PubMed] [Google Scholar]
- 55.Kaplan JL, Allen RJ, Guerra A, Sullivan SK. Anterolateral thigh flap for breast reconstruction: review of the literature and case reports. J Reconstr Microsurg. 2003;19:63–68. doi: 10.1055/s-2003-37807. [DOI] [PubMed] [Google Scholar]
- 56.Brunner C, Gröner P, Graf K, Biemer E. Refinements in breast reconstruction. Münch med Wschr. 1998;140:265–266. [Google Scholar]
- 57.Goldman JA, Greenblatt J, Joines R, White L, Aylward B, Lamm SH. Breast implants, rheumatoid arthritis, and connective tissue diseases in a clinical practice. J Clin Epidemiol. 1995;48:571–582. doi: 10.1016/0895-4356(94)00215-c. [DOI] [PubMed] [Google Scholar]
- 58.Sanchez-Guerrero J, Colditz GA, Karlson EW, Hunter DJ, Speizer FE, Liang MH. Silicone breast implants and the risk of connective-tissue diseases and symptoms. N Engl J Med. 1995;332:1666–1670. doi: 10.1056/NEJM199506223322502. [DOI] [PubMed] [Google Scholar]
- 59.Strom BL, Reidenberg MM, Freundlich B, Schinnar R. Breast silicone implants and risk of systemic lupus erythematosus. J Clin Epidemiol. 1994;47:1211–1214. doi: 10.1016/0895-4356(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 60.Schusterman MA, Kroll SS, Reece GP, et al. Incidence of autoimmune disease in patients after breast reconstruction with silicone gel implants versus autogenous tissue: a preliminary report. Ann Plast Surg. 1993;31:1–6. [PubMed] [Google Scholar]
- 61.Brunner C, Gröner P, Graf K, Kuhberger E, Biemer E. How risky are silicone gel-filled breast implants? Current standpoints and alternatives. Münch med Wschr. 1998;140:257–259. [Google Scholar]
- 62.Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg. 2000;105:2374–2380. doi: 10.1097/00006534-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 63.Chang DW, Wang B, Robb GL, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg. 2000;105:1640–1648. doi: 10.1097/00006534-200004050-00007. [DOI] [PubMed] [Google Scholar]
- 64.Temple CL, Strom EA, Youssef A, Langstein HN. Choice of recipient vessels in delayed TRAM flap breast reconstruction after radiotherapy. Plast Reconstr Surg. 2005;115:105–113. [PubMed] [Google Scholar]
- 65.Kroll SS, Robb GL, Reece GP, et al. Does prior irradiation increase the risk of total or partial free-flap loss? J Reconstr Microsurg. 1998;14:263–268. doi: 10.1055/s-2007-1000179. [DOI] [PubMed] [Google Scholar]
- 66.Cordeiro PG, Pusic AL, Disa JJ, McCormick B, VanZee K. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113:877–881. doi: 10.1097/01.prs.0000105689.84930.e5. [DOI] [PubMed] [Google Scholar]
- 67.Metcalfe KA, Semple JL, Narod SA. Satisfaction with breast reconstruction in women with bilateral prophylactic mastectomy: a descriptive study. Plast Reconstr Surg. 2004;114:360–366. doi: 10.1097/01.prs.0000131877.52740.0e. [DOI] [PubMed] [Google Scholar]
- 68.Nahabedian MY. Symmetrical breast reconstruction: analysis of secondary procedures after reconstruction with implants and autologous tissue. Plast Reconstr Surg. 2005;115:257–260. [PubMed] [Google Scholar]
- 69.Hudson DA. Factors determining shape and symmetry in immediate breast reconstruction. Ann Plast Surg. 2004;52:15–21. doi: 10.1097/01.sap.0000099962.79156.16. [DOI] [PubMed] [Google Scholar]
- 70.Kovacs L, Zimmermann A, Papadopulos NA, Biemer E. Re: factors determining shape and symmetry in immediate breast reconstruction. Ann Plast Surg. 2004;53:192–194. doi: 10.1097/01.sap.0000132572.72432.74. [DOI] [PubMed] [Google Scholar]
- 71.Sakai S, Ando K, Natori M, Sakai S. Cosmetic reconstruction after resection of breast cancer: use of the ELD-MC flap and EVRAM flap. Int J Clin Oncol. 2005;10:298–303. doi: 10.1007/s10147-005-0523-8. [DOI] [PubMed] [Google Scholar]
- 72.Spiro SA, Marshall D. Bilateral TRAM flaps for the reconstruction of the post implantectomy/capsulectomy breast deformity. Aesthetic Plast Surg. 1996;20:315–318. doi: 10.1007/BF00228462. [DOI] [PubMed] [Google Scholar]
- 73.Spear SL, Wolfe AJ. The coincidence of TRAM flaps and prostheses in the setting of breast reconstruction. Plast Reconstr Surg. 2002;110:478–486. doi: 10.1097/00006534-200208000-00017. [DOI] [PubMed] [Google Scholar]
- 74.Nahabedian MY, Momen B, Galdino G, Manson PN. Breast Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg. 2002;110:466–475. doi: 10.1097/00006534-200208000-00015. discussion 476-467. [DOI] [PubMed] [Google Scholar]