Abstract
Aim: The last decade the external approach has gained enormous popularity in rhinoplastic surgery and it is a relatively new technique in Greece for the correction of functional and aesthetic problems of the nose. We introduce our experience in open rhinoplasty, we describe the operative technique, its advantages.
Material-methods: In a period of two years (2003-2005), 98 patients underwent open rhinoplasty in our department. In 42 of them, breathing problems were existed in combination with nasal deformities. Eighty seven patients underwent septo/rhinoplasty under general anesthesia and the other 11 under local anesthesia.
Results: The postoperative course was uneventful, painless and without postoperative bleeding in all patients. Postoperative photo documentation was performed in all of them after 1, 3, 6, and 12 months. Only two patients needed to undergo revision surgery (the first patient due to "polly beak" deformity and the second one due to postoperative nasal valve stenosis). The scar of broken columella incision was invisible in all patents some weeks postoperatively.
Conclusion: In open approach in Rhinoplasty, as provides a full exposure of the osseocartilaginous vault, it is much more easier to perform all the modern rhinoplasty techniques with sutures, biological and non biological materials, to modify the nasal tip deformities and asymmetries and to gain an aesthetic result balanced with the other facial components. Its disadvantages are minimal, that’s why it becomes every day more popular all over the world.
Keywords: rhinoplasty, open approach
The last decade the external approach has gained enormous popularity in rhinoplastic surgery1.
The various indications of open approach are: asymmetry of the alar cartilages or upper lateral cartilages, nasal tip with lack of support, rotation or projection, overprojected nose, nasal tip asymmetry or deformities, crooked nose, saddle nose, cleft lip nose or other congenital anomalies, septal perforations and revision rhinoplasty2.
We describe the basic steps of the open approach, it’s advantages and disadvantages and some cases of patients who underwent open rhinoplasty in our department.
Material-methods
In a period of two years (2003-2005), 98 patients underwent open rhinoplasty in our department. In 42 of them, nasal breathing problems were combined with nasal deformities (septal deviation, internal or external valve collapse, hypertrophic inferior turbinates). A full preoperative evaluation (medical history, clinical evaluation, photo documentation and filling of the special preoperative work sheet) was performed in each case. Eighty seven patients underwent septo rhinoplasty under general anesthesia and the other 11 under local anesthesia.
Open rhinoplasty technique
When performing an external approach, the broken transcolumella incision is most commonly used3. This incision situated anterior to the medial crus footplates with the narrowest distance (halfway along the columella) between the nostrils. The marginals incisions bilaterally are marked. The vertical columella part of the marginal incisions should be placed 1,5-2 mm inside the vestibulum.
The skin incision is done with No15 blade perpendicular to the skin with special care not to damage the underlying media crura4. Then, with sharp, pointed curved scissors, a pocket is created underneath the skin and a skin flap is performed. With spreading movements using the Converse scissors, the broken columella incision is connected with the marginal incisions. To obtain adequate exposure of the nasal skeleton, the marginal incisions should be extended at least halfway along the vestibulum. Care should be taken not to disturb the "soft triangle of Converse" to prevent alar retraction and visible scars postoperatively. In cases with short columella in relation to the intended tip projection, a -V- incision at the base of columella is done (V-Y procedure).
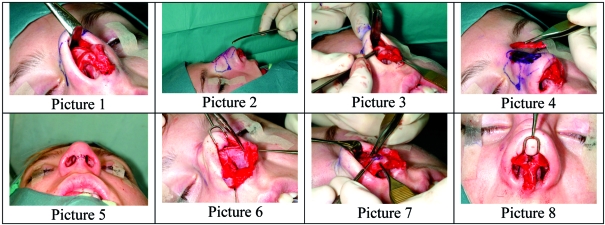
Dissection in the direct subperichondrial plane is obligatory in order to prevent intraoperative bleeding and enhance the healing process (Picture 1). Dissection should be conducted in a lateral direction up to the hinge scroll area, with further extension in a cephalic direction to the scroll area. To free the cartilaginous vault, the surgeon should start dissection in the midline, between or just cephalic to the domes.
Figure 1. Picture 1. Exposure of the cartilaginous part of the dorsum (upper lateral cartilages and dorsal part of the septum) Picture 2. Use of the Joseph’s elevation for the periosteum of the nasal bones before removing the bony hump Picture 3-4. Removal of the osseocartilaginous hump. Picture 5. Closure of broken columella incision with non-absorbable suture (ethilon 6/0) Picture 6. Exposure of the quandrangular cartilage of the septum Picture 7. Incomplete strip (cephalic trimming of LLC) Picture 8. Columellar strut and transdomal-interdomal sutures.
It can be helpful to incise the perichondrium at the caudal end of the cartilaginous vault vertically in the midline, after which subperichondrial dissection from medial to lateral and in a cephalic direction should be carried out. In some cases, a too thick supratip soft tissue envelope can be thinned but very conservatively not to compromise the blood supply to the overlying skin.
Dissection of the soft tissue ovelying the bony pyramid in a subperiosteal plane should start 2-3 mm parallel to and above the caudal end of the nasal bones. The periosteum is first incised and elevated with Joseph elevator (Picture 2). The elevation should not be very far laterally but only to the area of the hump to be resected. Then, dissection of the periosteum attached to the sutura intranasalis is performed with Kilner’s scissors.
With an "Aufricht" retractor in place, the cartilaginous vault is incised by through-and-through incision (No15 blade) from cephalic to caudal at the planned resection line. Using as a guide the cartilaginous cutting face, the hump osteotome (10 or 14 mm width) is introduced to loosen the bony part of the hump, followed by the removal of the osseocartilaginous hump "en bloc" (Picture 3-4). The broken columella incision is closed with interrupted non- resorbable sutures (ethilon 6/0) under no tension (Picture 5). In most of the cases there is no need for subcutaneous sutures except if there is much tension.
The first suture is always placed in the midline, continuing with angled off-midline sutures. This helps to recruit skin medially and prevents lateral notching of columellar incision. It’s also important to be mentioned that the edges of the wound should be everted for better healing and for preventing a visible scar postoperatively.
Intranasal packing, when performed, provides some compression to the septal flaps and prevents hematoma formation, synecchia, and decreases the risk of postoperative bleeding. It can be generally removed after 24 hours.
Taping of the nose will help to reduce the dead space, edema and the formation of hematoma, will protect the nasal structures from external trauma and prevent displacement of the newly aligned nasal structures.
Before applying the external dressing, operative edema is reduced by massage of the nasal covering. Then a piece of geal foam is applied (which prevents extraction of the skin from the underlying nasal skeleton ehile removing external nose dressing). Ovelapping strips of papertape are applied across the bridge of the nose including the supratip area.
At the end, a nasal splint is applied. The splint only covers the bridge of the nose. Lateral and frontal extensions prevent the possibility of distortion due to movements of the facial musculature. A splint applied too tightly may result in ischemia of the skin.
From the 42 patients with nasal breathing problems, 27 had septal deviation and they underwent septoplasty via the broken columella incision at the same time (Picture 6). In 7 of them, total septal reconstruction with PDS foil was performed (PDS is a material used to stabilize the septum in its new position, absorbed after 12–14 weeks of its implantation). In 10 patients with internal valve collapse and narrow middle vault, unilateral or bilateral spreader grafts were used. In the last 5 patients with collapse of the lateral nasal wall during inspiration, alar batten grafts from autogenous cartilage (septum or concha) were used.
In hump noses, after hump resection, osteotomies (medial oblique and lateral) with guarded microosteotome 2.5 mm were performed (endonasally or externally)5, without elevation and disturbance of the periosteum. Closure of the bony pyramid was achieved and in some cases of crooked nose, lateral osteotomies in different levels were performed to straighten the bony dorsum6.
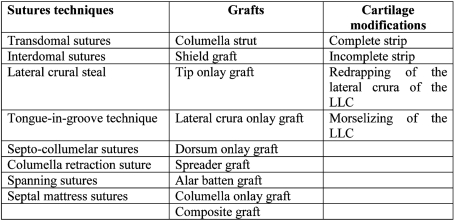
Autogenous grafts (septal cartilage, ear cartilage, rib) were used in order to achieve an aesthetic balance to nasal contour and to correct functional (breathing) problems (Table 1)7.
Table 1.
For the nasal tip reshaping and contouring, all the modern sutures techniques were used8. Modifications of the alar cartilages were performed (complete strip, incomplete strip) in order to achieve a more natural tip schema with the appropriate projection and rotation in relation with the other facial components9 (Table 1, Picture 7, 8).
Results
The most common nasal deformities in these 98 patients were: hump nose (53%), deviated nose (23%), tension nose (12%) and saddle nose (7%). All patients had nasal tip problems (schema, volume, symmetry, projection, rotation).
In all patients the postoperative course was uneventful, painless and without postoperative bleeding. The mean time of internal packing removal was after 6.3 hours and the mean time of hospitalization was 19.3 hours. The use of microosteotomes for performing the osteotomies without disturbing the periosteum, reduced the postoperative perioccular ecchymosis (the mean time of ecchymosis was 5,9 days). Postoperative photo documentation was performed in all patients after 1, 3, 6, and 12 months. Only two patients needed to undergo revision surgery (the first patient due to "polly beak" deformity and the second one due to postoperative nasal valve stenosis). The scar of broken columella incision was invisible in all patents some weeks postoperatively.
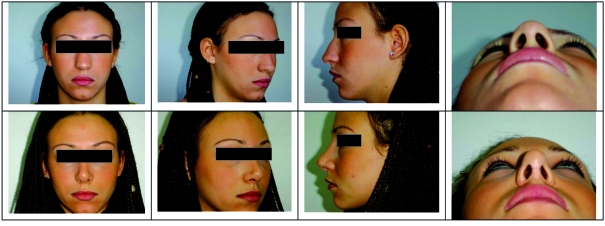
In Picture 9, we introduce a case who underwent open rhinoplasty in our department with preoperative and postoperative pictures 1 year later.
Figure 2. Picture 9. A 22-years old lady admitted in our department with severe nasal obstruction, wide dorsum, bulbous, underprojected and underotated tip, slight hump. She underwent open rhinoplasty: 1) Hump removal and medial oblique and lateral osteotomies with guarded microosteotome 2,5 mm 2) Septoplasty via the columellar incision 3)Dorsal onlay autologous graft (septal cartilage) 4) removal of a strip from the caudal septum and a part of the anterior nasal spine 5) Columella strut 6) transdomal and interdomal sutures 7) columella onlay graft. Preoperative and postoperative pictures 1 year later.
Discussion
Open rhinoplasty gives the possibility to assess anatomical deformities, asymmetries and structural alterations by direct inspection of the nasal framework. The much easier bimanual sculpturing under direct vision, have added a further dimension to rhinoplasty10. The structures of the nose can be manipulated in a more precise manner and sutures and grafts placed and fixed adequately.
In revision cases and when the aesthetic problem concerns only minor tip asymmetries it is much more easier via the open approach to achieve the desired result. It is also easier to imply with all the modern sutures techniques and grafts in order to contour the face balance.
Open approach in rhinoplasty is a more traumatic technique in comparison with the closed rhinoplasty, with more supratip edema postoperatively11. The scar of the skin incision is invisible in the majority of cases if the precise technique is performed12.
In conclusion open approach in Rhinoplasty provides a full exposure of the osseocartilaginous vault is much and for that reason easier to perform all the modern rhinoplasty techniques with sutures, biological and non biological materials, to modify the nasal tip deformities and asymmetries and to gain an aesthetic result balanced with the other facial components. Its disadvantages are minimal, and for this reason it has become popular all over the world.
References
- 1.Constantian MB. The two essential elements for planning tip surgery in primary and secondary rhinoplasty: observations based on review of 100 consecutive patients. Plast Reconstr Surg. 2004;114:1571–158. doi: 10.1097/01.prs.0000138755.00167.f5. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker EG, Johnson Cm., Jr The evolution of open structure rhinoplasty. Arch Facial Plast Surg. 2003;5:291–300. doi: 10.1001/archfaci.5.4.291. [DOI] [PubMed] [Google Scholar]
- 3.Rohrich RJ, Hollier LH, Jr, Janis JE, Kim J. Rinoplsty with advancing age. Plast Reconstr Surg. 2004;114:1936–1944. doi: 10.1097/01.prs.0000143308.48146.0a. [DOI] [PubMed] [Google Scholar]
- 4.Ganis JE, Kim J. The aging nose: characteristics and correction. Otolarygol Clinic North Am. 1992:172–179. [Google Scholar]
- 5.Ahn MS, Maas CS. Nasal osteotomies and clinical comparison of the perforaties methohs versus the continuous thechnique. Plast Reconstr Surg. 2003;3:127–132. [Google Scholar]
- 6.Mondin V, Rinaldo A, Ferlito A. Management of nasal bone fractures. Am J Otolaryngol. 2005;26:181–185. doi: 10.1016/j.amjoto.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Adamson PA, Galli SK. Rhinoplasty approaches: current state of the art. Arch Facial Plast Surg. 2005;7:32–37. doi: 10.1001/archfaci.7.1.32. [DOI] [PubMed] [Google Scholar]
- 8.Acarturk S, Gencel E. The spreader-splay graft combination: a treatment approach for the osseocartilaginous vault deformities following rhinoplasty. Aesthetic Plast Surg. 2003;27:275–280. doi: 10.1007/s00266-003-3030-1. [DOI] [PubMed] [Google Scholar]
- 9.Hafezi F, Naghibzadeh B. Prevention of hanging columella in open rhinoplasty. Ann Otol Rhinol Laryngol. 2004;113:839–842. doi: 10.1177/000348940411301012. [DOI] [PubMed] [Google Scholar]
- 10.Foda HM. External rhinoplasty: a critical analysis of 500 cases. J Laryngol Otol. 2003;117:473–477. doi: 10.1258/002221503321892325. [DOI] [PubMed] [Google Scholar]
- 11.Sporri S, Simmen D, Briner HR, Jones N. Objective assessment of tip projection and the nasolabial angle in rhinoplasty. Arch Facial Plast Surg. 2004;6:295–298. doi: 10.1001/archfaci.6.5.295. [DOI] [PubMed] [Google Scholar]
- 12.Constantian MB. Nasal tip surtures part II. Plast Reconstr Surg. 2002;4:444–451. [Google Scholar]