Abstract
Objective: Certain disorders may be falsely diagnosed as stroke. We examined the efficacy of the diagnostic protocol that is followed in our stroke unit and was designed in order to early differentiate more efficiently between stroke and conditions that mimic it.
Methods - Patients: Three hundred sixty-two elderly patients (196 male, 166 female with average age 74.56 years), who were hospitalized at our stroke center between January of 2005 and June of 2007 and diagnosed at admission as stroke patients, were retrospectively studied in order to investigate if the final diagnosis agreed with the initial diagnosis of stroke on admission.
Our diagnostic protocol included medical history of the patient, assessment of state of consciousness, blood pressure, electrocardiogram, complete blood cell count (hematocrit/hemoglobin, leukocytes, platelets), clotting mechanism (prothrombin time, activated partial thromboplastin time), glucose, electrolytes (Na, K, Ca), renal (blood urea nitrogen, creatinine) and liver function (SGOT, SGPT), as well as imaging methods like chest X-Ray and brain CT scan.
Results: In 95% of patients, the final diagnosis agreed with the initial diagnosis of stroke at admission. According to final diagnosis, 344 (95%) of them had stroke -either hemorrhagic or ischemic-, while from the rest 18 (5%), 12 (66.7%) were found to have metastatic neoplasm of brain, 3 (18.7%) had primal tumour of brain, whereas 3 (18.7%) suffered from other diseases (respiratory infection, meningoencephalitis, thyrotoxicosis). The principal symptoms of the conditions that mimicked a stroke were: aphasic disturbances (27.3%), dizziness/fainting (27.3%), headache/diplopia (11.1%), dysarthria (11.1%), hiccup and/or swallow disturbances (5.6%).
Conclusion: Our diagnostic protocol seems to ensure a high degree of differential diagnosis between stroke and conditions that mimic it.
Keywords: stroke, conditions that mimic stroke, brain cancer
Cerebrovascular strokes are acute events that should be diagnosed as soon as possible, since immediate medical treatment leads to significant reduction of morbidity and mortality. An early and accurate diagnosis is based on physical examination, laboratory examination as well as imaging methods, like computed tomography of the brain.
However, certain disorders may be falsely diagnosed as stroke, leading to delayed diagnosis of their real nature as well as inappropriate initial treatment with all its possible hazards.
Gliomas, meningiomas and hypophyseal adenomas are among the commonest primary tumors that may mimic a stroke. Metastatic lesions of the brain may have a similar presentation. Primary tumours which most frequently metastasize in the brain include lungs, breast, alimentary canal, kidneys and skin melanomas1. The rest of the cases include tumour lesions from biliary system, liver, thyroid, testis, uterus, ovaries, pancreas.
Certain infectious diseases may also be wrongly diagnosed as stroke. Such conditions include those which affect directly the brain like meningoencephalitis, as well as other infections that may present with symptoms from central nervous system due to inadequate blood supply of the brain, especially at elderly patients2.
Finally, toxic/metabolic conditions that may mimic stroke include diabetes mellitus, hypocalcaemia, hyponatremia, hypoglycemia, uremia, hepatic encephalopathy, hypothyroidism and thyroid crisis.
Patients - Methods
Three hundred sixty-two cases of patients, who were hospitalized at our stroke unit between January of 2005 and June of 2007 and diagnosed at admission as stroke patients, were retrospectively studied in order to investigate if the final diagnosis agreed with the initial diagnosis of stroke on admission. One hundred ninety-six were male and 166 were female, whereas the average age of the patients was 74.56 years. All patients followed the diagnostic protocol of our stroke unit, which is presented at Tables 1 and 2.
Table 1. Standard clinical examination and laboratory investigations of stroke patients according to our protocol.
Table 2. Neurological examination of stroke patients according to our diagnostic protocol.
On admission, patients were examined successively by an internist, a neurologist and a cardiologist. The initial diagnosis was based on physical examination, medical history, vital signs, complete blood cell count (hematocrit/ hemoglobin, leukocytes, platelets), clotting mechanism (prothrombin time, activated partial thromboplastin time), glucose, electrolytes (Na, K, Ca), renal (blood urea nitrogen, creatinine) and liver function (SGOT, SGPT), electrocardiogram (ECG) and chest X-Ray (CXR). A CT scan of the brain (without use of contrast material) was immediately performed. Five days after admission, patients underwent a second brain CT scan (using contrast material, unless contraindicated) and then, a thorough neurological examination was again performed in order to establish the final diagnosis. All the aforementioned clinical and laboratory examinations and their correlation to the initial and final diagnosis were statistically analyzed with the x2 test.
Results
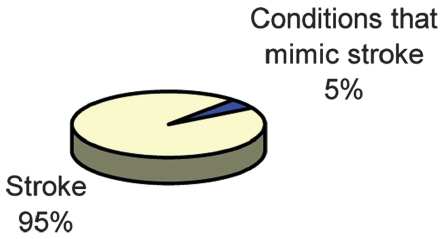
The patients were divided into two groups according to the final diagnosis: the first group concerned patients with a final diagnosis of stroke (either ischemic or hemorrhagic) and comprised 344 patients (of a total of 362 patients), that means 95% of the total admissions. The second group concerned patients with a final diagnosis other than stroke, who were initially falsely diagnosed as stroke patients. This group contained 18 patients, which means 5% of all admissions (Figure 1). Summarizing, in 95% of patients the final diagnosis of stroke agreed with the initial diagnosis of stroke on admission.
Figure 1. Final diagnosis of patients with stroke-like presentation.
Twelve out of the 18 patients of the second group (66.7%) were diagnosed having metastatic tumour of the brain, three (16.7%) were diagnosed suffering from primary brain cancers, one (5.6%) from thyroid crisis, one (5.6%) from meningoencephalitis and one (5.6%) from infection of the respiratory tract (Figure 2).
Figure 2. Conditions that mimicked stroke.
Twelve patients were diagnosed to have metastatic tumour of the brain of unknown primary lesion. Our investigation revealed that the primary lesion was at the lung (3 patients, 25%), colon (2 patients, 16.7%), prostate (2 patients, 16.7%), urinary bladder (2 patients, 16.7%), kidney (1 patient, 8.3%), breast (1 patient, 8.3%), whereas at one patient (8.3%) the final diagnosis of skin melanoma was histologically reached although the primary lesion was not possible to be identified (Figure 3).
Figure 3. Primary lesions with metastatic disease of the brain which mimicked stroke.
Among the three patients with primary brain cancer, two (66.7%) suffered from glioblastoma, whereas one (33.3%) suffered from meningioma. The main clinical presentations of the patients of the second group, as it can be seen at table 3, were: aphasic disorder (27.3%), dizziness/ collapse (27.3%), headache and/or diplopia (11.1%), confusion (11.1%), dysarthria (11.1%), epileptic seizures (5.6%), hiccup/dysphagia (5.6%).
Discussion
Various conditions may mimic stroke. It is important to reach the correct diagnosis early so as to offer an early medical treatment and better prognosis, especially at the elderly. In order to achieve that, a protocol of examinations is followed for every patient with a stroke-like presentation referring at the emergency unit of our clinic (Tables 1 and 2). Firstly, an internist performs a physical examination followed by a neurologist and a cardiologist. Important aspects to be taken into account are medical history of the patient, state of consciousness, blood pressure and other vital signs, ECG, blood tests (blood cell count, clotting mechanism, glucose, electrolytes, renal and liver function), as well as imaging methods like chest X-Ray and brain CT scan (even before the patient enters clinical and laboratory examinations are able to exclude metabolic or toxic conditions with symptoms from the central nervous system like diabetes mellitus, hypocalcemia, hypercalcemia, hyponatremia, hypoglycemia, uremia, hepatic encephalopathy as well as certain infectious diseases2. Moreover, it is possible to differentiate between ischemic and hemorrhagic stroke, as well as primary and metastatic tumors of the brain.
A study performed in the U.S.A. in 1995 revealed that 77 out of 388 (19%) patients presented with symptoms that mimicked stroke leading to false initial diagnosis of stroke at admission3. The significant difference of false diagnosis at admission compared to our study (19% vs. 5% in our study) seems to be due to a predefined clinical/ laboratory diagnostic protocol, which is followed at the emergency unit of our clinic and was presented above. The distribution of the conditions that mimicked stroke is similar to our study. It should be mentioned that in our study, epileptic seizures were considered as a clinical symptom rather than a nosologic entity. This is the reason why it is not included within the conditions that mimicked stroke.
In case an ischemic stroke is revealed at a brain CT scan during the acute phase of the event (66-98% of cases), it presents as a hypodense area without surrounding oedema4. Radiological signs like presence of oedema, localization of the lesion at the cerebral cortex, well-demarcated margins of the lesions and lack of association of the area of the lesion with a specific brain artery point toward brain tumour4. The presence of more than one lesion with the aforementioned characteristics supports the diagnosis of metastatic disease of the brain. On the contrary, intracranial bleeding presents at the brain CT scan as a hyperdense area4. In this case, the presence of surrounding oedema supports the diagnosis of hemorrhage from a brain tumour. Another radiological sign to support this diagnosis is the presence of hypodense areas within a hemorrhagic lesion. The presence of multiple lesions suggests metastatic cancer, if firstly we exclude bleeding diathesis and amyloid encephalopathy of the elderly5. Intracranial bleeding could complicate virtually any brain tumor, whereas in 33% to 50% of cases it constitutes the presenting manifestation5. A study on transient ischemic attacks which was conducted in U.K. (U.K. TIA study group) revealed that 0.4% of patients (10 out of 2449) who were initially diagnosed as stroke patients turned out finally to suffer from primary brain tumors6. Half of them suffered from glioma, whereas the other half suffered from meningioma. In our study, 15 out of 352 patients who were initially diagnosed as stroke patients turned out finally to suffer from brain tumor. Three of them (0.85%) had primary brain tumor (2 with glioma, one with meningioma). The findings of our study are similar with the findings of the U.K. TIA study: a) the frequency of primary brain tumors was similar, b) the type of brain tumor was similar, c) none of the patients with primary brain tumor presented with intracranial hemorrhage. Primary brain tumors rarely bleed (less than 1%)7. Among gliomas, the risk of bleeding correlates with the degree of malignancy and glioblastoma multiforme and astrocytoma have the highest rates of hemorrhage. However, there are exceptions like oligodendroglioma and polycystic astrocytoma, which although benign lesions have high rate of bleeding7,8, and meningioma which bleeds very rarely, and almost never intracerebrally7.
Concerning the patients of our study with metastatic disease of the brain, 27.3% of them had primary lung cancer. Various studies reveal similar results (20-40%). Brain metastases usually create lacunar infarcts and present with ataxia or motor hemiplegia9. Brain metastasis of bronchogenic carcinoma bleed relatively rarely, but its high frequency makes it the most common cause of intracranial bleeding due to metastasis10. Metastatic tumors of the brain bleed more often (10-14%) than primary ones5. Melanoma and choriocarcinoma are uncommon causes of brain metastasis but have high rates of intracranial bleeding (40-60%). The distribution of the primary lesion at the patients with brain metastatic disease of our study is similar to the frequency described in various studies. Specifically, one patient (8.3%) of our study had brain metastasis due to melanoma, a rate similar to 3-6%, which is described in other studies1. Similarly, two patients (16.7%) of our study had brain metastasis from colonic cancer, a rate similar to 10-20%, described in other studies1.
Our study also reveals that in a significant number (33%) of patients with brain metastasis the primary lesion was in the urinary tract (prostate, bladder), which is considered to be uncommon site of brain metastasis. Therefore, we believe that the investigation of the primary site in a patient with brain metastasis should include the urinary tract through ultrasonography and PSA.
It is also interesting that sometimes the primary lesion may remain unknown, depriving us of the possibility to treat. This was the case in one patient of our study, where the final diagnosis of skin melanoma was made with the help of histology.
The main symptoms, that patients not suffering of stroke in our study complained of, in the emergency room, are shown in Table 3. All these symptoms may be present in more than one clinical condition. Diziness/ fainting may accompany stroke but may also be present in encephalitis, toxic/metabolic disturbances, circulatory instability. Moreover, serious infections of the pulmonary system may disturb the normal alveolar gas exchange and lead to symptoms from the central nervous system2. Especially in elderly patients where the blood supply to the brain may be inadequate due to concomitant atherosclerosis, infections may present with disturbed level of consciousness, delirium and even coma while the clinical signs of the infection may not be obvious yet due to decreased immune response. The symptoms from the central nervous system arise from either increased metabolism that leads to further decrease of oxygen supply to the brain, or direct effect of the toxin to the brain, especially in bacterial infections. In meningoencephalitis, the patient may be irritable at the beginning, while later on may get drowsy or even comatose11. Signs of focal neurological deficit, although rare, may be present in meningoencephalitis due to pneumococcus or hemophilus influenza11. Convulsions may also be present, especially in younger patients, due to meningeal irritation11. In case of cerebral oedema or formation of abscess, symptoms are similar to any other intracranial mass-occupying lesion. In thyroid crisis, the oxygen needs are increased due to increased metabolism, whereas the direct effect of thyroid hormones to the myocardium may cause tachyarrhythmia, which may aggravate the function of the heart as a pump. As a result, blood and oxygen supply to the brain may be compromised, especially in elderly, arteriosclerotic patients. Frequently, patients in thyroid crisis present with apathy, severe muscle weakness and coma.
Table 3. The main clinical presentations of the patients who did not suffered a stroke.
We believe that physicians at the emergency room should be aware of the conditions that may mimic stroke. Our diagnostic protocol seems to ensure a high degree of differential diagnosis between these conditions and stroke. Still, we believe that additional investigations like thyroid hormones when hyper- or hypothyroidism is suspected, cerebrospinal fluid aspiration when meningoencephalitis is suspected, arterial gas examination and rectal thermometry in case sepsis is suspected may be of additional help.
References
- 1.Mintz A, Perry J, Spithoff K, Chambers A, Laperriere N. Management of single brain metastasis: a practice guideline. Curr Oncol. 2007;14:131–143. doi: 10.3747/co.2007.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demaerschalk BM. Diagnosis and management of stroke (brain attack) Semin Neurol. 2003;23:241–252. doi: 10.1055/s-2003-814740. [DOI] [PubMed] [Google Scholar]
- 3.Libman RB, Wirkowski E, Alvir J, Rao TH. Conditions that mimic stroke in the emergency department. Implications for acute stroke trials. Arch Neurol. 1995;52:1119–1122. doi: 10.1001/archneur.1995.00540350113023. [DOI] [PubMed] [Google Scholar]
- 4.Bradac GB, Oberson R. CT and angiography in cases with occlusive disease of supratentorial cerebral vessels. Neuroradiology. 1980;19:193–200. doi: 10.1007/BF00376707. [DOI] [PubMed] [Google Scholar]
- 5.Mandybur TI. Intracranial hemorrhage caused by metastatic tumorse. Neurology. 1977;27:650–655. doi: 10.1212/wnl.27.7.650. [DOI] [PubMed] [Google Scholar]
- 6.The UK TIA Study Group. Intracranial tumours that mimic transient cerebral ischaemia: lessons from a large multicentre trial. J Neurol Neurosurg Psychiatry. 1993;56:563–566. doi: 10.1136/jnnp.56.5.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kondziolka D, Bernstein M, Resch L, et al. Significance of hemorrhage into brain tumors: clinicopathological study. J Neurosurg. 1987;67:852–857. doi: 10.3171/jns.1987.67.6.0852. [DOI] [PubMed] [Google Scholar]
- 8.Bitoh S, Hasegawa H, Ohtsuki H, Obashi J, Fujiwara M, Sakurai M. Cerebral neoplasms initially presenting with massive intracerebral hemorrhage. Surg Neurol. 1984;22:57–62. doi: 10.1016/0090-3019(84)90230-1. [DOI] [PubMed] [Google Scholar]
- 9.Chen WH, Yin HL, Chang YY, Liu JS. Metastatic brain tumor manifesting as lacunar syndrome in adults. Gaoxiong Yi Xue Ke Xue Za Zhi. 1993;9:317–321. [PubMed] [Google Scholar]
- 10.Gildersleeve N, Jr, Koo AH, McDonald CJ. Metastic tumor presenting as intracerebral hemorrhage. Report of 6 cases examined by computed tomography. Radiology. 1977;124:109–112. doi: 10.1148/124.1.109. [DOI] [PubMed] [Google Scholar]
- 11.Van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351:1849–1859. doi: 10.1056/NEJMoa040845. [DOI] [PubMed] [Google Scholar]