Abstract
Background: At the current stage, the criteria for making the diagnosis of SLE (ARA, 1982) include only two neuropsychiatric manifestations: seizures and psychoses. In view of the need for early detection of the lesions of the nervous system, we set ourselves to the task of developing an approach for making the diagnosis of NPSLE (neuropsychiatric SLE) on the basis of criteria with high sensitivity and specificity.
Methods: In view of determining the type and incidence of the lesions of the nervous system (NS), clinical, laboratory, and instrumental examinations were performed within the period from 1998 to 2006 in 225 patients with SLE. Depending on the specific features of the clinical course, these patients were divided into three groups: with clinically manifested lesions of NS; without clinically manifested lesions of NS; and with incomplete SLE.
Results and conclusions: The results from the performed examinations showed a high percentage (64.44%) of neuropsychiatric lesions in the patients with SLE. According our results, NPSLE diagnosis should be made in the presence of at least one indicator from the first group of criteria (seizures, psychosis, cerebrovascular event, lesion of cranial nerves, motor disturbances, quantitative alterations of consciousness) and at least two indicators from the second group of criteria (cognitive dysfunction, headache due to lupus, peripheral neuropathy, MRI changes, EEG changes, ENMG changes, positive aRPA, positive aPL) after ruling out other causes (except for SLE) for their occurrence.
Keywords: neuropsychiatric systemic lupus erythematosus, classification criteria
Systemic lupus erythematosus is an autoimmune, immune-complex, multi-system, chronic inflammatory disease of the connective tissue where immune disorders develop on the background and with the involvement of genetic, hormonal and environmental factors.
Neuropsychiatric manifestations have been described in the very first communications on the disease1. Recent studies show that lesions of this kind are present in more than two thirds of patients with SLE2. The lesions of the nervous system are characterized by a broad spectrum of clinical manifestations3–7. At this stage, widely accepted is the nomenclature system proposed by American College of Rheumatology (ACR, 1999) and providing a definition of 19 such manifestations8. The neuropsychiatric manifestations that have found their place in the classification criteria for SLE9 as well as in the revised version suggested by M. Hochberg et al (1997)10 are only two: seizures and psychoses.
The great medical and social significance of the neuropsychiatric lesions in patients with SLE are determined by their high incidence (up to 79%) mainly in women in childbearing and active creative age (20-40 yrs) as well as by the fact that these lesions are one of the most difficult to diagnose and treat in cases of SLE, and also because their presence is one of the most serious indicators for severe course and poor prognosis in patients with SLE.
The requirement for an early diagnosis of the lesions of the nervous system in patients with SLE and their timely and adequate treatment grounded our examinations.
The aim of the presented study was to examine the nature of the lesions of the nervous system in patients with SLE and to define criteria for classification of the disease as neuropsychiatric systemic lupus erythematosus.
Materials and methods
Within the period from 1998 to 2006, 384 subjects (329 female and 55 male) aged from 18 to 57 (mean age 33.22±8.15) were examined in the Clinic of Rheumatology of the Medical University of Sofia. The study protocol was approved by the local committee and the informed consent was obtained from all patients before inclusion in the study. Depending on the clinical course, the patients (pts) with SLE (225) were divided into three groups: Group I: Patients with SLE and clinically manifested lesions of the nervous system (104 pts); Group II: Patients with SLE without clinically manifested lesions of the nervous system (63 pts) - these patients were active but had lesions of other organs and systems (nephritis, pulmonitis, serositis); Group III: Patients with incomplete (subclinical) SLE (58 pts). In view of the more precise differentiation of the cognitive disturbances in patients with SLE, two control groups (IV и V) were used as well. Group IV: Patients with rheumatoid arthritis (96 pts) having received corticosteroid treatment for a period of at least 3 years - the constitution of this control group aimed at excluding the probability for existence of a relation of the ascertained structural and functional changes in the central nervous system of patients with SLE with the administered corticosteroid and immunosuppressive treatment; Group V: Healthy volunteers (63 subjects). All subjects from these groups have undergone integral clinical examinations with tests for assessment of their cognitive functions.
We assumed that the examined patients with SLE have primary neuropsychiatric manifestations, after ruling out the probability for presence of secondary lesions of the nervous system related to infections, electrolyte disturbances, drug intake (neuroleptics, L-Dopa), concurrent syndromes, like chronic renal failure, or diseases like hyperthyroidism. Subjects with data of overlapping of SLE with other systemic diseases of the connective tissue, illiteracy, chronic alcoholism, drug abuse, were not included in the study.
The diagnosis of SLE was made on the basis of the presence of at least 4 of the 11 revised criteria of ARA (American Rheumatism Association, 1982)9. In case that less than 4 of the criteria of ARA for diagnosing SLE were present, we assumed the presence of an incomplete (subclinical) lupus erythematosus11. The diagnosis of rheumatoid arthritis (RA) was made in case that at least 4 of the seven ARA (American Rheumatism Association, 1987) criteria were present12. SLEDAI (SLE Disease Activity Index) score system of ACR (1992) was used to determine the activity of SLE13. The systemic nature of the lesion in SLE was estimated according to SLICC score system (Systemic Lupus International Collaborating Clinics/ACR Damage Index for SLE)14. The nomenclature of ACR was used to define major neuropsychiatric manifestations8. To assure a high level of intrinsic quality and comparability of this approach we used the EULAR standard operating procedures15.
The following standard laboratory examinations were performed: blood count, ESR, biochemical examinations ( creatinine, creatinine clearance, ASAT, ALAT, γGTP, alkaline phosphatase, blood sugar, serum albumin, total cholesterol, high density lipoproteins, low density lipoproteins, very low density lipoproteins, triglycerides, uric acid, urea ), electrolytes, examination of the urine.
The immunological examinations included determination of: antiribosomal P-antibodies (ELISA immunoenzymatic method, standardized and approbated in the Faculty of Biology at the Sofia University "St. Kliment Ohridski", Department of Biochemistry, Bulgaria); antiphospholipid antibodies (aPL); Lupus anticoagulant (LAC); anticardiolipin antibodies (kit: ORG 5155 Anticardiolipin Screen, Orgentec); antibodies against β2-Gp1 (ELISA method, Orgentec); antinuclear antibodies (ELISA - kit Varelise, Farmacia); antibodies against native double-stranded DNA (ELISA immunoenzymatic method); antibodies against Smith antigen (ELISA immunoemzymatic method, Orgentec); anti-neutrophil cytoplasmic antibodies (standard indirect immunofluorescence upon human neutrophil); a-SS-A (ELISA qualitative immunoenzyme screening) and a-SS-B (ELISA qualitative immunoenzyme screening) antibodies; aRNP antibodies (ELISA); C3 and C4 components of the complement system (radial immunodiffusion and monospecific anti-C3 and anti-C4 Immunotest sera); aC1q antibodies16; Circulating Immune Complexes; Immunoglobulins M, A, G (radial immunodiffusion G. Manchini et al.)17; cryoglobulins (qualitative and spectrophotometric reading at 280 nm, immunoelectrophoresis and immunodiffusion of the cryoprecipitate); LE cells. Other laboratory examinations were also performed, for example: Matrix Metalloproteinase 9 (ELISA, Diabor, Oslu, Finland); Antithrombin III (radial immunodiffusion), examination of cerebrospinal liquid in patients with written approved consent for this investigation and under suspicion for central nervous system (CNS) infections or cerebral bleeding.
Instrumental methods of examination: Magnetic Resonance Tomography (MRT) - MRI (Magnetic Resonance Imaging), using FLAIR (Fluid Attenuated Inversion Recovery) and TIRM (Turbo Inversion Recovery Measurement) techniques; electroencephalography (EEG); electroneuromyography (ENMG); direct ophthalmoscopy. In some patients additional instrumental examination was performed, such as: conventional roentgenography of the cervical section of the spine; Doppler-ultrasonographic examination of the carotid and vertebral arteries; fluorescein angiography of the retinal vessels; and computed tomography of the brain in view of ruling out other vascular and mechanical etiology provoking secondary neuropsychiatric manifestations. Instrumental examinations like conventional roentgenography of the lungs, HRCT (High Resolution Computed Tomography), Doppler- utrasonographic examination of peripheral veins and arteries, capillaroscopy, perfusion scintigraphy of the lungs, echography of visceral organs, echocardiography, puncture renal biopsy, were used for determining the lesions of the other organs and systems. Single photon emission computed tomography (SPECT) and position emission tomography (PET) were made in limited number of patients (which are included in the study after 2004 year) due to limited availability and excessive cost.
Other methods - determination of the level of intellectual development (IQ - Intelligence Quotient); tests for cognitive disturbances at onset of SLE . With the participation of clinical psychologists, the following disturbances were determined: memory disturbances - by means of R. A. Luria's tests ("learning 10 words" and "pictogram"); attention distractions - used the test of Pieron-Ruther; disturbances of thought - the test for comparing notions; classification of the psychiatric syndromes according to DSM-IV (Diagnostic and Statistic Manual of Mental Disorders)18 - the examination was performed by a psychiatrist.
The data were entered and processed by means of the statistical package SPSS 13.0.1.
The following statistical methods were applied: parametric Student's t-test and Fisher's exact test for nominal variables, correlation analysis (daily dose/type of syndromes; age/development of steroid-induced psychiatric syndromes and others), single-sample test of Kolmogorov-Smirnov to determine if two datasets differ significantly; variation analysis to determine the independent factors related with psychiatric syndromes. When 3 populations were compared, ANOVA (Analysis Of Variances) was used with Fisher's least significant difference test to assess differences between individual groups, analysis of criteria for validation of screening tests; descriptive analysis cross-tabulation, graphic analysis, nonparametric test of Kruskal-Wallis for testing equality of population medians among groups, non-parametric test of Mann-Whitney, χ2 test to compare differences in the other considered items. Continuous data are presented as mean (SD) and categorical data as number (percentage). For all analyses p values less than or equal to 0.05 considered statistically significant.
In view of assessing the validity of the criteria we suggested for diagnosing NPSLE, the following parameters were examined: Sensitivity (Se) - the capability of the test to detect diseased individuals; Specificity (Sp) - it characterizes the capability of the test to detect healthy individuals; Positive predictive value (VPP) - it is measured by the probability for presence of a disease in the individuals with a positive test; Negative predictive value (VPN)- it is measured by the probability for absence of neuropsychiatric manifestations in the patients with SLE and a positive test.
The computations were performed in the Department of Social Medicine and Health Management at the Medical University, Sofia, Bulgaria.
Results
On the ground of the performed examinations, we found that:
Neuropsychiatric lesions are ascertained at a high rate (64.44%) in patients with SLE.
The most common neuropsychiatric manifestations in SLE are: cognitive deficit (49.33 %), lupus headache (23.11 %, in 57.69% of these patients - tension-type), psychoses (12.00 %), seizures (10.67 %), and cerebrovascular events (9.78 %).
The most common cognitive deficit in patients with SLE is memory disturbance (74.77%).
Typical CNS changes for NPSLE during MRI examination are the multiple lacunar infarctions with temporal localization as well as a parenchymatous cerebral atrophy.
MRI changes are ascertained more frequently in patients with SLE and positive aCL (p < 0.001, r: 0.79), aPL (p < 0.002, r: 0.86), and aRPA (p < 0.05, r: 0.65). SPECT perfusion defects correlates with cumulative damage (SLICC) (r: 0.97).
Cognitive disturbances and cerebrovascular events (CVE) are detected reliably more often in patients with SLE and positive aCL (p < 0.001, r1: 0,81, r2: 0.94), but not all patients with positive aCL suffer from CVE.
Detection of antiribosomal P-antibodies in SLE requires a predetermined search for psychoses (p < 0.001, r: 0.83) in such patients while detection of aSm antibodies (p < 0.001, r: 0.79) and MMP 9 (p < 0.001, r: 0.64) requires a search for epileptic disposition.
Skin vasculitis, serositis and pulmonary involvement are the most common extracerebral manifestations in patients with SLE and data for neuropsychiatric lesions (seizures, psychoses, cerebrovascular events) being signs of general vascular pathology disease activity.
EEG changes in NPSLE are non-specific and take the form of paroxysmal disposition in the frontotemporal and parietal areas, also in patients with SLE but without clinically evident neuropsychiatric manifestations.
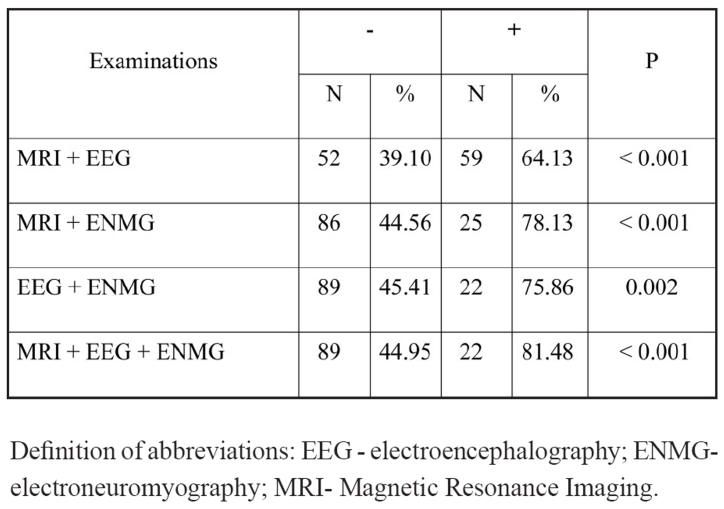
The combinative application of the instrumental methods for examination significantly increases the rate of diagnostics of neuro-psychological manifestations and this being particularly well expressed in patients with cognitive disturbances (Table 1).
SLE activity is greater in patients with neuropsychiatric manifestations; aPL positive patients; a-dsDNA positive patients; patients with positive aRPA.
Table 1. The significance of the instrumental methods for examination in patients with cognitive disturbances.
Definition of abbreviations: EEG - electroencephalography; ENMG-electroneuromyography; MRI- Magnetic Resonance Imaging.
Discussion
No single clinical, laboratory, neuropsychological and imaging test can be used to differentiate NPSLE from non-NPSLE patients with similar neuropsychiatric manifestations. A combination of the aforementioned tests may provide useful information in assessment of selected SLE patients presenting with neuropsychiatric symptoms.
On the ground of the performed examinations, the following conclusions were made:
The tests for cognitive disturbances can be used as a screening for detection of neuropsychiatric manifestations in patients with SLE.
The basic methods for early detection of lesions of the nervous system in SLE are tests for cognitive disturbances and an MRI examination. Current imaging techniques do not adequately discriminate between immune mediated demyelination as a result of immune-mediated injury to myelin, and demyelination as a result of ischemic injury within the central nervous system (CNS). Neither CT nor MRI can easily distinguish small vessel vasculitis from multiple small vessel thrombosis. PET scan appears to be sensitive in detecting metabolism and perfusion abnormalities in virtually all patients with overt or subclinical CNS involvement, and has been claimed to correlate with disease course, but evidence comes from small number of patients (n=17).
Immunological examinations (aRPA, aPL, aCL, etc.) as well as the MMP 9 examination are auxiliary methods for determining the nature of the neuropsychiatric lesions in SLE.
In order to make a final diagnosis of NPSLE, two successive stages should be passed:
First stage. Answers to two basic questions are required:
Are there data for exacerbation of SLE?
Are there causes (besides SLE) for the neurological and/or psychiatric symptoms, i.e. it should be specified whether in every particular case the neuropsychiatric symptoms are primary or secondary?
In case of a positive answer to the first question and absence of other causes for neuropsychiatric manifestations, the diagnosis of probable NPSLE should be made.
Second stage. The type of the lesion of the nervous system should be specified - central and/or peripheral, diffuse and/or focal - by means of clinical (tests for cognitive disturbances), instrumental (MRI, EEG, ENMG, etc.), and laboratory (aPL, aRPA, with/without CSF examination, etc.) methods of examination.
In case of a negative results from thus performed examinations, high-sensitivity and expensive (at this stage) instrumental methods of examination like SPECT, PET, and MRS should be considered.
A positive result from the performed examination grounds the differentiation of a specific NPSLE syndrome (ACR, 1999)8.
Third stage. Application of the suggested criteria for making a final diagnosis of NPSLE - these criteria are divided into two groups:
First group - seizure, psychosis, cerebrovascular event, lesion of cranial nerves, quantitative alterations of consciousness.
Second group - cognitive dysfunction, lupus headache, peripheral neuropathy, MRI changes, EEG changes, ENMG changes, positive aRPA, positive aPL.
The presence of at least one criterion from the first group and at least two criteria from the second groups is a sufficient condition for making a final diagnosis of NPSLE.
The application of tests for validation of the results from the presented study showed that the suggested criteria for making a diagnosis of neurolupus possess a very high capability to detect individuals with lesions of the nervous system in SLE (Se = 90,38%, Sp = 67,77%) at relatively high values of the positive predictive value (VPP = 70,68%) and negative predictive value (VPN = 89,13%).
The approach we developed for making the diagnosis of NPSLE is essential for early detection of individuals with NPSLE, for prevention of neuropsychiatric manifestations, and for optimization of the treatment schedule for SLE. The patients with NPSLE were treated with different combination of immunomodulating drugs. In patients with antiphospholipid antibodies low dose aspirin or anticoagulants were included if there was no contraindication, but this was no the object of our study.
Nervous system involvement in systemic lupus erythematosus can present with diverse neurologic or psychiatric symptomatology. Estimates of the prevalence of clinical neuropsychiatric SLE vary from 14% to 75%, reflecting variable diagnostic methodologies and criteria2,19. To standardize clinical diagnosis, a system for classification of neuropsychiatric symptomatology in SLE, based on modification and extension of previous clinical classifications, has been proposed8, but in the classification criteria for SLE neuropsychiatric manifestations are only two: seizures and psychosis9–10. In addition to these clinical syndromes, however, patients with SLE complain of many neurologic and psychiatric problems. These complaints, although difficult to evaluate by virtue of their subjective nature, are nonetheless endorsed by many SLE patients, including those who have never experienced seizures and psychosis. The possibility that at least some of these subjective experiences may reflect nervous system involvement and/or herald future neuropsychiatric events cannot be discounted.
Our preliminary data show that the classification criteria for neuropsychiatric systemic lupus erythematosus need a discussion. Large multicenter studies are necessary to determine if other neuropsychiatric manifestations can be included in criteria for SLE.
References
- 1.Kaposi MK. Neue Beitrage zur Kenntnis des Lupus erythematosus. Arch Dermatol Syph. 1982;4:36–78. [Google Scholar]
- 2.Brey RL, Hollyday SL, Saklad AR, et al. Neuropsychiatric syndromes in lupus: prevalence using standardized definitions. Neurology. 2002;58:1214–1220. doi: 10.1212/wnl.58.8.1214. [DOI] [PubMed] [Google Scholar]
- 3.Bertsias GK, Ioannidis JPA, Boletis J, et al. EULAR recommendations for the management of Systemic Lupus Erytematosus (SLE). Report of a Task Force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). ARD online. 2007 available: http://journals.bmj.com/cgi/reprint form. [Google Scholar]
- 4.Jennekens FGI, Kater L. The central nervous system in systemic lupus erythematosus. Part I. Clinical syndromes: a literature investigation. Rheumatology. 2002;41:605–618. doi: 10.1093/rheumatology/41.6.605. [DOI] [PubMed] [Google Scholar]
- 5.Karassa FB, Afeltra A, Ambrozic A, et al. Accuracy of anti-ribosomal P protein antibody testing for the diagnosis of neuropsychiatric systemic lupus erythematosus: an international meta-analysis. Arthritis Rheum. 2006;54:312–324. doi: 10.1002/art.21539. [DOI] [PubMed] [Google Scholar]
- 6.Mitsikostas DD, Sfikakis PP, Goadsby PJ. A meta-analysis for headache in systemic lupus erythematosus: the evidence and the myth. Brain. 2004;127:1200–1209. doi: 10.1093/brain/awh146. [DOI] [PubMed] [Google Scholar]
- 7.Sanna G, Piga M, Terryberry JW, et al. Central nervous system involvement in systemic lupus erythematosus & cerebral imaging and serologic profile in patients with and without overt neuropsychiatric manifestations. Lupus. 2000;9:573–583. doi: 10.1191/096120300678828695. [DOI] [PubMed] [Google Scholar]
- 8.ACR Ad Hoc Committee of Neuropsychiatric Lupus Nomenclature. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999;42:599–608. doi: 10.1002/1529-0131(199904)42:4<599::AID-ANR2>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 9.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 10.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725–1734. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 11.Swaak AJ, van de Brink H, Smeenk R, et al. Incomplete lupus erythematosus: results of a multicentre study under the supervision of the EULAR Standing Committee on International Clinical Studies Including Therapeutic Trails. Rheumatology. 2001;40:89–94. doi: 10.1093/rheumatology/40.1.89. [DOI] [PubMed] [Google Scholar]
- 12.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Assotiation 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 13.Bombardier C, Gladman DD, Chang CH, Urovitz MB. The Committee of Prognosis Study in SLE & Development of the SLE disease activity index: the SlEDAI. Arthritis Rheum. 1992;35:630–640. doi: 10.1002/art.1780350606. [DOI] [PubMed] [Google Scholar]
- 14.Denburg SD, Carbotte RM, Ginsberg JS, Denburg JA. The relationship of antiphospholipid antibodies to cognitive function in patients with systemic lupus erythematosus. J Int Neuropsychol Soc. 1997;3:377–386. [PubMed] [Google Scholar]
- 15.Dougados M, Betteridge N, Burmester GR, et al. EULAR standardized operating procedures for the elaboration, evaluation, dissemination, and implementation of recommendations endorsed by the EULAR standing committees. Ann Rheum Dis. 2004;63:1172–1176. doi: 10.1136/ard.2004.023697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tenner AJ, Lesavre PH, Cooper NR. Purification and radio-labelling of human C1q. J Immunol. 1981;3:648–653. [PubMed] [Google Scholar]
- 17.Mancini G, Carbonara AO, Heremans JF. Immunochemical quantitation of antigens by single radial immunodiffusion. Immunochemistry. 1965;2:235–254. doi: 10.1016/0019-2791(65)90004-2. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): American Psychiatric Association; 1994. pp. 45–67. [Google Scholar]
- 19.McCune WJ, Golbus J. Neuropsychiatric lupus. Rheum Dis Clin North Am. 1988;14:149–167. [PubMed] [Google Scholar]