A 72‐year‐old man presented to the emergency department with a 2‐day history of fever and difficulty in breathing. His medical history included Henoch–Schonlein purpura treated with steroids, pulmonary tuberculosis treated with antimicrobials, and lobectomy of the right lung 30 years previously.
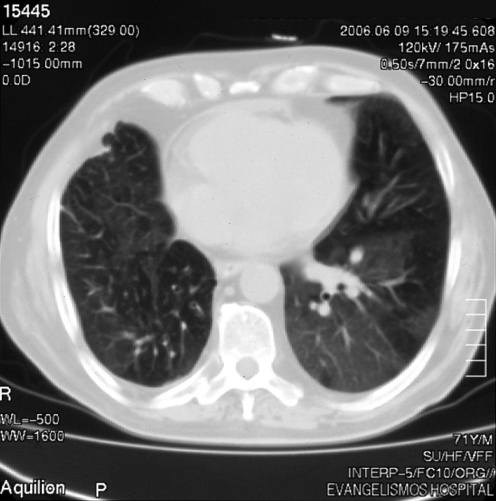
On presentation, his vital signs were as follows: blood pressure 120/80 mm Hg, heart rate 100 beats/min, oral temperature 38.2°C, respiratory rate 22/min, oxygen saturation 86% (on air). Lung auscultation showed crackles in bases bilaterally. The rest of the physical examination was unremarkable. Laboratory tests showed leucocytosis (11.69×103 U/l) and increased C reactive protein (11.1 mg/dl), without other abnormal values. Purified protein derivative test and sputum cultures for mycobacterium were negative. The patient underwent a computed tomography scan of the chest (fig 1), which showed ground‐glass opacification compatible with interstitial pneumonia. He was treated successfully with antibiotics. Pulmonary involvement in Henoch–Schonlein purpura is rare, occurring more often in adults and commonly manifesting as diffuse alveolar haemorrhage and occasionally as usual interstitial pneumonia or interstitial fibrosis.1
Figure 1 Chest computed tomography scan showing ground‐glass opacification compatible with interstitial pneumonia.
Footnotes
Competing interests: None declared.
References
- 1.Nadrous H F, Yu A C, Specks U.et al Pulmonary involvement in Henoch‐Schonlein purpura. Mayo Clin Proc 2004791151–1157. [DOI] [PubMed] [Google Scholar]