Abstract
Background
Scoring systems that weigh the degree of abnormality of bedside observations might be able to identify patients at risk of catastrophic deterioration.
Objectives
To establish a frequency distribution for typical physiological scoring systems and to establish the potential benefit of adding these to an existing triage system in accident and emergency departments.
Methods
Physiological data were collected from 53 unselected emergency department admissions, from 50 patients admitted from the emergency department to intensive care, and from 50 patients admitted from emergency department to general wards and then to intensive care. Three different physiological scores were calculated from the data. Identification of sick patients by the scores was compared with triage information from the Manchester Triage System (MTS).
Results
Most patients admitted to the emergency department would not be identified as critically ill with the aid of physiological scoring systems. This was true even for patients who were admitted to intensive care. Only in 0–8% of unselected patients did the scores indicate increased risk. In 100 patients admitted to the intensive care, adding of medical emergency team call‐out criteria, Modified Early Warning Score or Assessment Score for Sick patient Identification and Step‐up in Treatment would identify none, seven or one patient in addition to those triaged as orange and red by the MTS.
Conclusions
Introduction of a physiological scoring system would have identified only a small number of additional patients as critically ill and added little to the triage system currently in use.
Delayed recognition of critically ill patients increases the risk of cardiopulmonary arrests1 and death in the intensive care unit (ICU).2 Usage of algorithms based on bedside observations might improve recognition and outcome of patients on hospital wards.3
The overall prognosis of patients admitted to ICU directly from emergency departments is better than the prognosis for those admitted to the ICU from general wards.4 Most emergency departments use triage systems to identify those patients requiring the most urgent attention. The Manchester Triage system (MTS) is one of the most commonly used triage systems in the UK and triages patients across a large variety of medical and surgical specialties. The MTS uses protocols based on the presenting complaint and questions about potentially aggravating factors. It is designed as a tool for prioritising the urgency of being seen, but its ability to assess the severity of the disease has been questioned.5
It is not known whether a system based on physiological parameters would be able to identify patients at risk of intensive care admissions better than the MTS or provide additional information about the severity of the condition of a patient in the setting of an emergency department. A pilot study conducted in the Wrexham Maelor Hospital, Wrexham, UK, has examined Modified Early Warning Scores (MEWS) in patients admitted to the emergency department and classified as orange according to the MTS. The study suggested that patients with high scores had a higher likelihood of being admitted to hospital than those with low MEWS.6 Medical and elderly patients had higher MEWS than younger and surgical patients. In the setting of the emergency department, a serial evaluation of physiological scores might be better for detecting critical illness than a single assessment.7
Accuracy of triage by using the Manchester Triage System has not been compared with the accuracy of a severity classification based on physiological parameters.
It is not known whether a physiologically based triage system could potentially shorten the time of transfer from the emergency department admission to ICU and avoid inappropriate admissions of critically ill patients from the emergency department to the general wards.
Methods
Design
A retrospective cohort study was conducted. Formal application for ethics approval was waived by the local research ethics committee because of the observational nature of the study.
Setting
The study was conducted in a district general hospital (Wrexham Maelor Hospital, Wrexham, UK) serving a population of 300 000 in North Wales. The hospital covers all major surgical and medical specialties, including vascular surgery and renal dialysis. In 2004, the emergency department saw 62 692 patients, of whom 8535 were classified as orange, 18 727 as yellow and 33 060 as green using the MTS. The ICU comprises five beds with four additional high‐dependency beds.
Physiological triage systems
Physiological scores were calculated from the first set of physiological parameters collected by nursing staff on admission to the emergency department.
Modified Early Warning Score
MEWS is a linear summary score of five parameters with seven bands each. It classifies systolic blood pressure, pulse rate, respiratory rate, temperature and level of consciousness (AVPU score for Alert, reacting to Voice, reacting to Pain, Unresponsiveness), according to their deviation from normality. Scores range from 0 to 15. A score of ⩾5 is associated with increased risk of death, admission to intensive care or high‐dependency unit in acute medical admissions.8 The nursing staff scores every set of observations and activates the call‐out of senior staff if a score of ⩾3 is reached. MEWS on admission to the emergency department was calculated for all patients included in the study.
Assessment Score for Sick patient Identification and Step‐up in Treatment
The Assessment Score for Sick patient Identification and Step‐up in Treatment (ASSIST) is a non‐linear summary score of five parameters with seven bands each.9 It classifies systolic blood pressure, pulse rate, respiratory rate and level of consciousness (ACDN score for Alert and orientated, Confused, Drowsy, Not responsive or only to nail pressure) according to their deviation from normality. Additionally, patients aged >70 years are scored with an extra point. Scores range from 0 to 21. A score of ⩾4 is associated with increased risk of death and admission to the intensive care or high‐dependency unit in acute medical admissions.
Medical emergency team
Criteria for the call‐out of a medical emergency team (MET) have been developed following principles of the Airway, Breathing, Circulation and Disability assessment. Nursing staff are asked to call out senior staff if bedside observations are below or above defined thresholds for blood pressure, heart rate, respiratory rate and level of consciousness, or if they are worried about a patient.10
Patient population
Three patient groups were reviewed. Physiological data for group 1 were collected prospectively on admission to the emergency department. All other data was retrieved from emergency department and hospital records. Physiological data were used to calculate MEWS, ASSIST and MET scores. Information about ICU admission, including Acute Physiology And Chronic Health Evaluation (APACHE) II scores, was collected from the ICU database (database for the Intensive Care National Audit and Research Centre). The number of times of admission to the emergency department and to the ICU were recorded.
Group 1: 53 unselected patients presenting at the emergency department in two samples of consecutive patients on 30 and 31 October 2003. For these patients, information regarding triage category, age, blood pressure, pulse rate, respiratory rate, temperature, saturations, fraction of inspired oxygen and admission status for hospital and ICU admission was collected.
Group 2: 50 direct admissions from the emergency department to the ICU admitted between 1 April and 31 October 2003. Emergency department and inpatient records of these patients were reviewed.
Group 3: 50 patients admitted to the emergency department, who were transferred to a general medical or surgical ward and then admitted to intensive care between 1 April and 31 October 2003.
Statistics
Means and standard deviations (SD) were calculated for all physiological variables. Groups were compared using the Student's t test for independent samples for parametric parameters and Mann–Whitney U test for non‐parametric parameters. Spearman's correlation was used to evaluate the relationship between different systems. Critically ill patients in the emergency department were defined as those with MEWS >2, ASSIST >3 and MET criteria applicable, with MTS categories orange or red.
Results
Epidemiological data in the accident and emergency department
Tables 1 and 2 summarise the epidemiological parameters and diagnostic groups for the three groups. After exclusion of datasets with insufficient physiological data, 49 cases were analysed in group 2 and 49 in group 3.
Table 1 Data on admission to the accident and emergency department.
| Group 1*, n = 53 | Group 2†, n = 49 | Group 3‡, n = 49 | Total, n = 151 | |
|---|---|---|---|---|
| Female (%) | 27 (51) | 17 (35) | 18 (37) | 62 (41) |
| Age (years) | 48 (24) | 43 (20) | 57 (18) | 49 (21) |
| Systolic blood pressure (mm Hg) | 137 (21) | 122 (36) | 135 (25) | 132 (28) |
| Diastolic blood pressure (mm Hg) | 81 (15) | 68 (25) | 77 (20) | 75 (20) |
| Pulse rate (bpm) | 81 (18) | 104 (24) | 97 (25) | 93 (24) |
| Respiratory rate (/min) | 17 (4) | 22 (6) | 24 (8) | 21 (7) |
| Temperature (°C) | 36.3 (0.8) | 35.7 (1.1) | 36.4 (1.6) | 36.2 (1.2) |
| Oxygen saturations (%) | 97 (2.3) | 92 (11) | 93 (6) | 94 (7) |
| Median GCS (range) | NA | 9 (3–15) | 15 (12–15) | 11 (3–15) |
A&E, accident and emergency; GCS, Glasgow Coma Scale; ICU, intensive care unit. NA, not applicable.
Values are mean (SD) unless specified.
*Unselected patients.
†Direct admissions from A&E to ICU.
‡Admissions from A&E to general wards and then ICU.
Table 2 Diagnostic categories on admission to the accident and emergency department.
| Group 1* | Group 2† | Group 3‡ | |
|---|---|---|---|
| Trauma | 24 | 14 | 9 |
| Gastrointestinal bleeding | 2 | 1 | 3 |
| Overdose | 1 | 5 | 2 |
| Neurological catastrophe (ie, cerebrovascular accident and epilepsy) | 2 | 9 | 5 |
| Cardiac (acute coronary syndrome, myocardial infarction and left ventricular failure) | 5 | 3 | 1 |
| Chest (COPD, asthma and pneumonia) | 5 | 5 | 16 |
| Sepsis of other origin | 1 | 3 | 4 |
| Aortic aneurysm | 1 | 1 | 1 |
| Others | 12 | 8 | 8 |
| Total | 53 | 49 | 49 |
COPD, chronic obstructive pulmonary disease.
*Unselected patients.
†Direct admissions from accident and emergency (A&E) department to intensive care unit (ICU).
‡Admissions from A&E to general wards and then ICU.
Comparison between groups
Compared with group 1, group 2 had on admission a lower systolic blood pressure (p<0.01), lower diastolic blood pressure (p<0.01), higher pulse rate (p<0.001), higher respiratory rate (p<0.001), lower temperature (p<0.01) and lower saturations (p<0.002).
Compared with group 1, group 3 had on admission only a lower pulse rate, higher respiratory rate and lower saturations (all p<0.001).
Admission to ICU
Table 3 shows the sensitivities of scores.
Table 3 Sensitivity of scoring systems for admission to intensive care.
| MTS in % (orange or red) | MEWS in % (>2) | ASSIST in % (>3) | MET in % ( = 1) | |
|---|---|---|---|---|
| Group 2 | 46 (96) | 34 (77) | 11 (22) | 1 (2) |
| Group 3 | 32 (65) | 24 (55) | 8 (16) | 3 (7) |
ASSIST, Assessment Score for Sick patient Identification and Step‐up in Treatment; MET, medical emergency team; MEWS, Modified Early Warning Score; MTS, Manchester Triage System.
Proportion of patients with calculated scores above a predefined threshold indicate risk of catastrophic deterioration.
The mean (SD) APACHE II scores11 on admissions to ICU were 12 (8.4) in group 2 and 16 (SD 6.9) in group 3 (difference not significant, p<0.058 for Student's t test for independent samples). The biggest groups of patients admitted to intensive care had trauma (23%), respiratory tract infections with acute respiratory failure (21%) and neurological catastrophes (10.6%). The case mix in groups 2 and 3 was comparable, but there were 16 respiratory cases in group 3 as opposed to 5 in group 2. Respiratory rate on admission was higher in group 3, but not significantly so (p<0.38 for Student's t test for independent samples). ASSIST and MEWS did correlate with APACHE II on admission (MEWS correlation coefficient 0.29, p<0.017; ASSIST correlation coefficient 0.25, p<0.03).
Scoring
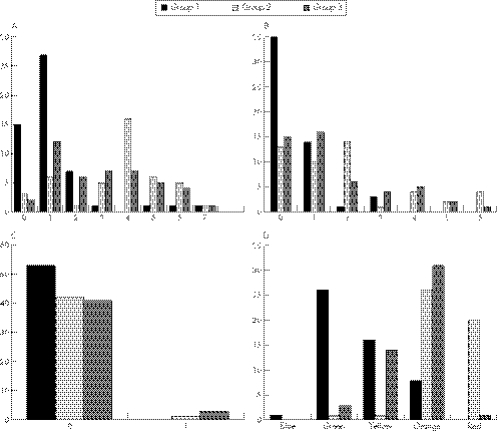
Data collected on admission to the emergency department were used to calculate the scores. Scores were put in relation to categories from the MTS. Figure 1 shows the frequency distribution of the derived scores on admission.
Figure 1 Distribution of scores and MTS on admission to the accident and emergency (A&E) department in unselected admissions to A&E (group 1), direct admissions from A&E to ICU (group 2) and admission from A&E admitted to ICU after transfer to a general ward (group 3)*. (A) MEWS, (B) ASSIST, (C) MET and (D) MTS. ASSIST, Assessment Score for Sick patient Identification and Step‐up in Treatment; ICU, intensive care unit; MET, medical emergency team; MEWS, Modified Early Warning Score; MTS, Manchester Triage System.
In group 1, MTS identified 8 (15%, category orange or red) sick patients, MEWS would have identified 4 (8% of scores >2) patients, two of these in addition to the MTS. ASSIST and MET would have classified no patients as at risk. Median for ASSIST and MEWS was 0 (interquartile range (IQR) 0–1).
Two patients triggered MET in group 2 and three in group 3. The median score for MEWS was 4 in group 2 (IQR 3–5) and 3 in group 3 (IQR 1–4). Median scores for ASSIST were 2 in group 2 (IQR 0–6) and 1 in group 3 (IQR 0–3).
Comparison between groups of patients admitted to intensive care
Patients in groups 2 and 3 were comparable with regard to age, MEWS and ASSIST on admission. Group 2 had a lower age (p<0.001, Student's t test) and lower Glasgow Coma Scale (p<0.001, Mann–Whitney U test) when compared with Group 3. Furthermore, they scored red and orange less often on the MTS (p<0.001 for Mann–Whitney U test).
Mean difference of delay to intensive care was 3.7 days in group 3 (p<0.001, 95% confidence interval (CI) −5.7 to –1.6). Patients admitted first to the wards stayed longer in ICU (3.8 (SD 7.3) days v 6.8 (7.9) days, mean difference 3 days, p<0.052, 95% CI–6.1 to 0.3) and longer in hospital (11.4 (18.6) days v 20.2 (18.2), mean difference 8.8 days, 95% CI –16.3 to –1.4, p<0.021). These differences are not adjusted for age or APACHE II scores.
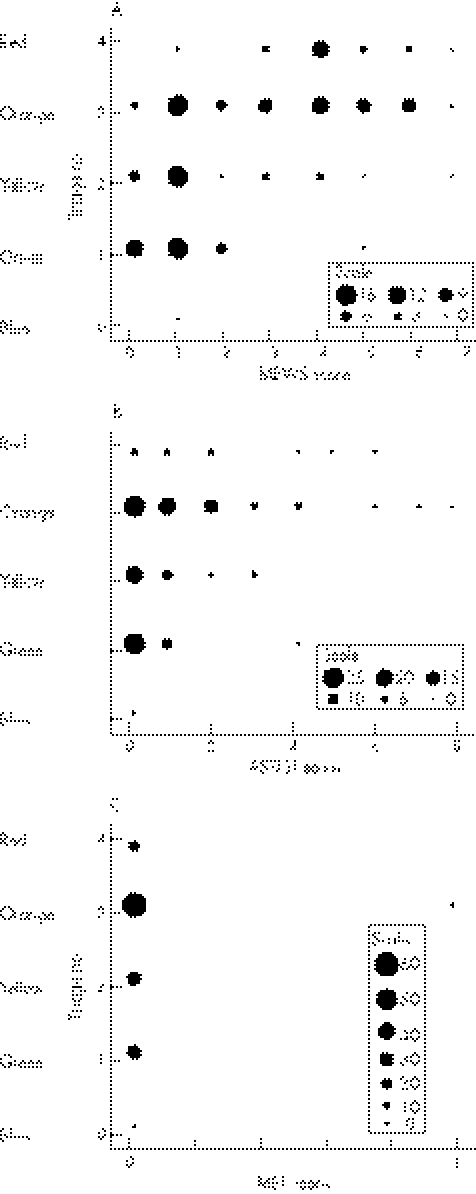
The number of patients with categories indicating risk of catastrophic deterioration was largest if assessed by the MTS and MEWS, respectively (table 3). Only a small number of patients admitted with categories of “blue”, “green” or “yellow” would have triggered any of the three scoring systems (available online at http://www.emjonline.com/supplemental). In some patients none of the four systems applied would have indicated increased risk. The number of patients triggering a simulated MET score was very low, taking into account that the criterion of “worrying” could not be applied to the dataset.
In group 2, MTS identified 42 sick patients; MEWS, ASSIST and MET would not have identified any additional sick patients.
In group 3, MTS identified 28 sick patients; MEWS would have identified an additional 7 patients; ASSIST and MET would not have identified additional sick patients.
Discussion
Our study of a sample of unselected patients in the emergency department (group 1) did not show gross physiological abnormalities. This resulted in normal scores for MEWS, ASSIST and MET criteria.
Patients who were admitted to ICU either directly from emergency departments or from emergency departments via general wards had physiological abnormalities more often. Despite this, a major proportion would not have triggered on any of the scoring systems tested. Addition of a physiological scoring system would have identified only a few patients missed by MTS. Patients who were admitted to intensive care via general wards were likely to be older, to suffer from respiratory conditions and had a worse APACHE II score on admission to intensive care. They stayed longer in hospital.
However, this is a small‐scale, non‐randomised study; the scoring systems used were developed for use on general wards and their properties are therefore expected to be different in a different patient population.
We did not assess or score pain. Pain could be a powerful confounding variable that influences the value of physiological parameters, and pain relief would alter subsequent measurements.
Other scores such as the Emergency Severity Index have been developed and validated for usage in emergency departments. They might perform better compared with the MTS with regard to identification of potential ICU admissions12 and correlation with APACHE II.13 Modifications of MEWS to fit the different setting are currently being developed.14
Serial measurements of MEWS or ASSIST might help identify early deterioration of patients in the emergency department and could potentially offer benefit in being able to track patients' progress or deterioration over time. Patients with certain disease categories (eg, asthma, chronic obstructive pulmonary disease and sepsis) in which pathways could be identified on the basis of evidence‐based guidelines would be the group most likely to benefit from scoring. The effect of these properties on patient outcomes would need to be examined in a further study.
Measurement of scores might alert clinicians to some patients not captured as “patients that need intervention sooner” by the MTS. It remains important that in cases of doubt the clinical impression or acumen of a senior and experienced medical or nursing staff should always remain the default position and should overrule triage categories or scoring systems.
Conclusion
In summary, the data from our study provide a frequency distribution of commonly used scoring models in unselected and critically ill the emergency department patients. The number of patients identified as “at risk of catastrophic deterioration” in addition to the MTS appears to be small. Early identification of critically ill patients in the emergency department is of central importance for these patients, but only a small number of emergency department patients are likely to be identified earlier, with the usage of scores rather than with MTS. How useful the identification of these additional patients is will depend on resources and priorities of practising clinicians.
Figure 2 Scatter graph of categories for MTS and score for physiological triage systems across all three patient groups. The size of the dots represents the number of cases in each category. (A) MTS versus MEWS. (B) MTS versus ASSIST. (C) MTS versus MET. ASSIST, Assessment Score for Sick patient Identification and Step‐up in Treatment; MET, medical emergency team; MEWS, Modified Early Warning Score; MTS, Manchester Triage System.
Supplementary Material
Acknowledgements
We thank Kate Gallagher and Lucy Marshall, students from Cardiff University, for collecting the accident and emergency data as part of their attachment. We also thank Carol Davies for providing data from the Intensive Care National Audit and Research Centre database and the department of medical records for assistance with retrieving patient files.
Abbreviations
APACHE - Acute Physiology And Chronic Health Evaluation
ASSIST - Assessment Score for Sick patient Identification and Step‐up in Treatment
ICU - intensive care unit, IQR, interquartile range
MET - medical emergency team
MEWS - Modified Early Warning Score
MTS - Manchester Triage System
Footnotes
Competing interests: CPS and LG have published on Early Warning Scores and received local research and development grants for this work. CPS is currently part of a group that has received a grant to examine the effect of outreach in England (NHS Service Delivery and Organisation Research and Development Programme, outline proposal to evaluate outreach services in critical care (SDO/74/2004)).
References
- 1.Schein R M H, Hazday N, Pena M.et al Clinical antecedents to in‐hospital cardiopulmonary arrest. Chest 1990981388–1392. [DOI] [PubMed] [Google Scholar]
- 2.McQuillan P, Pilkington S, Allan A.et al Confidential inquiry into quality of care before admission to intensive care. BMJ 19983161853–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Priestley G, Watson W, Rashidian A.et al Introducing critical care outreach: a ward‐randomised trial of phased introduction in a general hospital. Intensive Care Med 2004301398–1404. [DOI] [PubMed] [Google Scholar]
- 4.Goldhill D R, Sumner A. Outcomes of intensive care patients in a group of British intensive care units. Crit Care Med 1998261337–1345. [DOI] [PubMed] [Google Scholar]
- 5.Cooke M W, Jinks S. Does the Manchester triage system detect the critically ill? J Accid Emerg Med 199916179–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byng S, Sen A, Subbe S.et al Modified early warning score: one for all and A&E? Br J Anaesth 200492611P–2P. [Google Scholar]
- 7.Rees J E, Mann C. Use of the patient at risk scores in the emergency department: a preliminary study. Emerg Med J 200421698–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subbe C P, Kruger M, Rutherford P.et al Patients at risk: validation of a modified Early Warning Score in medical admissions. QJM 200194521–526. [DOI] [PubMed] [Google Scholar]
- 9.Subbe C P, Hibbs R, Williams E.et al ASSIST: a screening tool for critically ill patients on general medical wards. Intensive Care Med 200228(Suppl)S21 [Google Scholar]
- 10.Lee A, Bishop G, Hilman K.et al The medical emergency team. Anaesth Intensive Care 199523183–186. [DOI] [PubMed] [Google Scholar]
- 11.Knaus W A, Draper E A, Wagner D P.et al APACHE II: a severity of disease classification system. Crit Care Med 198513818–829. [PubMed] [Google Scholar]
- 12.Tanabe P, Gimbel R, Yarnold P R.et al Reliability and validity of scores on the emergency severity index version 3. Acad Emerg Med 20041159–65. [DOI] [PubMed] [Google Scholar]
- 13.Olsson T, Lind L. Comparison of the rapid emergency medicine score and APACHE II in nonsurgical emergency department patients. Acad Emerg Med 2003101040–1048. [DOI] [PubMed] [Google Scholar]
- 14.Gottschalk S B, Wood D, DeVries S.et al The care triage score: a new triage system South Africa. Proposal from the care triage group. Emerg Med J 200623149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.