Abstract
Objective
To appraise the evidence on the diagnostic accuracy of CT pulmonary angiography and the prognostic value of a negative CT pulmonary angiogram in the diagnosis of pulmonary embolism.
Methods
Medline, EMBASE, and grey literature were systematically searched by two researchers. Any study which compared CT pulmonary angiography to an acceptable reference standard or prospectively followed up a cohort of patients with a normal CT pulmonary angiogram was included. Study methods were appraised independently by two researchers, and data were extracted independently by three researchers.
Results
Thirteen diagnostic and 11 follow up studies were identified. Studies varied in prevalence of pulmonary embolism (19–79%), patient groups, and method quality. Few studies recruited unselected emergency department patients. There was heterogeneity in the analysis of sensitivity (53 to 100%), specificity (79 to 100%), and false negative rate (1.0 to 10.7%). The pooled false negative rate of combined negative CT pulmonary angiography and negative deep vein thrombosis testing was 1.5% (95% CI 1.0 to 1.9%).
Conclusion
Diagnostic studies give conflicting results for the diagnostic accuracy of CT pulmonary angiography. Follow up studies show that CT pulmonary angiography can be used in combination with investigation for deep vein thrombosis to exclude pulmonary embolism.
Keywords: pulmonary embolism, CT scan, diagnosis
The diagnosis of pulmonary embolism is challenging as symptoms of pulmonary embolism are varied and range from mild, non‐specific lethargy or breathlessness, to collapse and cardiac arrest.1,2,3 Recurrent pulmonary embolism is associated with a case mortality of 26%.4 Early diagnosis is essential as even patients with minor symptoms are at risk of recurrent pulmonary emboli.
The combination of a normal D‐dimer concentration and low clinical probability score5,6,7 provides a robust screening method, facilitating exclusion of pulmonary embolism without diagnostic imaging. The PIOPED study8 proposed combining ventilation‐perfusion scanning with clinical probability for the safe exclusion and diagnosis in a subset of patients. This strategy does not exclude or diagnose pulmonary embolism in all suspected cases. The gold standard investigation—pulmonary angiography—is invasive and carries a recognised morbidity and mortality.9 Furthermore, a normal angiogram is associated with a 1.6% incidence of venous thromboembolism in the following year.10
Computed tomographic pulmonary angiography (CT pulmonary angiography) is increasingly used in the diagnosis of pulmonary embolism. CT has the advantage of imaging the entire thorax, facilitating the diagnosis of conditions mistaken for pulmonary embolism, such as pneumonia, aortic dissection, and malignancy.11 UK and US guidelines have planted CT among the basic investigations for pulmonary embolism.12,13 Attempts to evaluate the clinical utility of CT pulmonary angiography have been complicated by rapid advances in CT scanning technology, acceptance that angiography may not be the most appropriate reference standard, and heterogeneous study populations.
The aim of this study was to appraise the diagnostic accuracy of CT pulmonary angiography in the emergency department diagnosis of pulmonary embolism and the prognostic value of a negative CT pulmonary angiogram.
Method
Search strategy
Searches were conducted on Medline (Ovid interface 1966–July week 2, 2005) and EMBASE (1980–week 29, 2005) using the following search strategy: [Exp Tomography, X‐ray Computed, OR CT.mp OR Computed tomograph$.mp] AND [exp pulmonary embolism OR pulmonary embol$.mp. OR PE.mp. OR exp thromboembolism OR pulmonary infarct$.mp] LIMIT to human. The ACP Journal Club, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, MEDION‐database, SIGLE database of grey literature, and the international published guidelines for diagnosis of pulmonary embolism were searched for any further references. All database searches were conducted independently by two researchers who reviewed the titles and abstracts of database search results. All potentially relevant papers were sourced in full. Studies published in languages other than English were translated. The reference sections of all publications were cross referenced. Lastly, experts in the field from the UK, USA, France, and Switzerland were contacted to identify further unpublished data.
Inclusion criteria
Studies were analysed if they were either a diagnostic study assessing the accuracy of CT pulmonary angiography in diagnosing pulmonary embolism or a follow up study that recruited a cohort of patients with negative CT pulmonary angiograms and followed them clinically. Studies of chronic pulmonary emboli and those using electron beam CT scanners were excluded.
To be included, diagnostic studies had to apply an adequate reference standard to all patients or a subgroup of patients. A high probability ventilation‐perfusion scan in a patient with high clinical probability of pulmonary embolism, a positive investigation for deep vein thrombosis, or positive pulmonary angiography were considered adequate to confirm pulmonary embolism. A normal or near normal ventilation‐perfusion scan was adequate to exclude pulmonary embolism as was a low probability ventilation‐perfusion scan combined with either low clinical probability or an uneventful three month follow up. The CT scan result had to form no part of the reference standard diagnosis of pulmonary embolism. Data had to be presented as true positive, false positive, true negative, and false negatives.
Only prospective follow up studies with a greater than 85% follow up rate involving patient contact were included. In addition it had to be possible to calculate the number of patients who developed deep vein thrombosis or pulmonary embolism during the follow up period.
Two clinical researchers examined all potential papers. In the event of a discrepancy, a third was asked to review the study.
Quality appraisal
Each included study was appraised for quality using predetermined guidelines (appendices 1 and 2). In particular, diagnostic papers were appraised to establish whether the reference standard investigation was blinded to the CT pulmonary angiogram result and vice versa. Follow up studies were appraised to establish whether the outcomes included both pulmonary embolism and deep vein thrombosis, that a uniform assessment was applied to all patients following the negative CT, and details of further diagnostic tests were given. The length of follow up, whether personal contact had been employed in all cases and whether all deaths were examined by postmortem or an adjudication panel, was also assessed.
All studies were evaluated for evidence of a consecutive cohort, details of the recruitment process, number of centres involved, and prevalence of pulmonary embolism among the study population. Details of inclusion criteria, inpatient/outpatient mix, comorbidity, and a record of all previous diagnostic tests were sought as were exclusion criteria and the demographics of those excluded.
Details of the process of CT pulmonary angiography were appraised checking whether the scans were interpreted blinded to the reference standard investigation, the CT scanner type, technique, and diagnostic criteria, and the number of radiologists interpreting each CT scan.
This appraisal was performed independently by two researchers. In the case of a discrepancy, a third was asked to appraise the study.
Data extraction
For each diagnostic study the numbers of true positive, false positive, true negative, and false negative patients were extracted independently by three researchers. Two studies compared the results from experienced and junior radiologists interpreting CT scans. In this case only the results for the experienced radiologists were used.
For each follow up study the number of false negative CT scans was calculated independently by three researchers. Any positive venous ultrasounds, high probability ventilation‐perfusion scans, positive pulmonary angiograms, or deaths caused by pulmonary embolism were considered to represent false negative CT scans.
Statistical methods
Sensitivity and specificity were calculated for CT pulmonary angiography. The false negative rates were calculated for CT pulmonary angiography alone and CT pulmonary angiography combined with a deep vein thrombosis investigation. These results were recorded in Excel (Microsoft Excel, USA) and Forest plots with Mantel‐Haenszel weighting were constructed using StatsDirect (StatsDirect Ltd, Cheshire, UK). The presence of a cut off point effect was assessed by calculating the Spearman correlation coefficient between sensitivity and specificity.14 The random effects model was employed to pool data using Stata version 7.0 (Stata Corp LP, Texas, USA).
Results
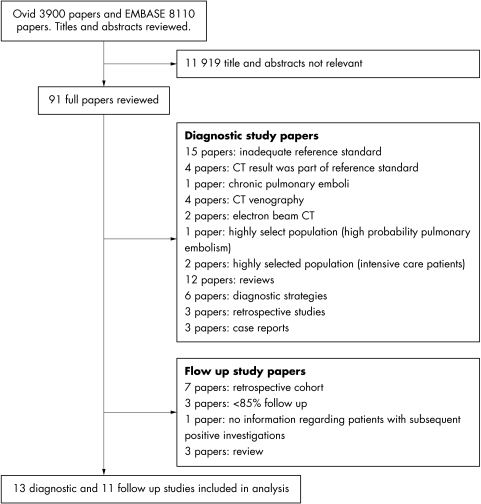
The OVID search found 3900 papers and EMBASE 8110 papers. The results of the systematic search are shown in figure 1. Twenty four studies meeting the inclusion criteria were included. One study recruiting patients suspected of massive pulmonary embolism (n = 10) and two studies recruiting intensive care patients (a different population to the emergency department, n = 59) were excluded.
Figure 1 Systematic review results.
Diagnostic studies
Thirteen were diagnostic studies (summarised in table 1).15,16,17,18,19,20,21,22,23,24,25,26,27 Twelve used pulmonary angiography alone as a gold standard, with one19 using a diagnostic algorithm. The patient groups ranged from emergency department patients suspected of pulmonary embolic disease15 to highly selected groups.22,27 The prevalence of pulmonary embolism ranged from 19% to 79%. Only one was a multicentre study.15 All but three studies used a single detector CT scanner and 12 studies employed two or more radiologists to interpret the CT scan. One study did not stipulate the number of radiologists.27 Appraisal scores varied widely.
Table 1 Diagnostic studies for analysis.
| Author | Country and year | Inclusion criteria | Outpatients (%) | Prevalence of PE | Sensitivity | Specificity | Study appraisal scores: 0 = no criteria fulfilled, 1 = only some criteria fulfilled, 2 = all criteria fulfilled | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference standard | Study cohort | Included patients | Excluded patients | CTPA protocol | |||||||
| Nilsson et al15 | Sweden 2002 | Emergency department patients suspected of PE | 100% | 37% | 30/33 | 55/57 | 2 | 1 | 1 | 1 | 2 |
| Qanadli et al16 | France 2000 | Patients referred for radiological investigation of PE | 87% | 39% | 56/59 | 89/92 | 2 | 1 | 1 | 2 | 2 |
| Remy‐Jardin et al17 | France 1992 | 32 patients suspected of PE and 10 with abnormal chest x rays | Unknown | 54% | 18/18 | 23/24 | 2 | 1 | 1 | 0 | 2 |
| von Steiner et al18 | Germany 1994 | Patients suspected of PE | Unknown | 79% | 30/30 | 8/8 | 0 | 1 | 1 | 0 | 1 |
| Sostman et al19 | USA 1996 | Patients suspected of PE | Unknown | 38% | 9/13 | 14/15 | 2 | 1 | 1 | 1 | 1 |
| Stone et al20 | Australia 2003 | Patients with non‐diagnostic VQ scans | Unknown | 28% | 4/7 | 17/18 | 0 | 1 | 1 | 1 | 1 |
| Garg et al21 | USA 1998 | Patients with non‐diagnostic VQ scan, some had normal lower limb ultrasound | Unknown | 20% | 4/6 | 18/18 | 2 | 1 | 1 | 1 | 2 |
| Goodman et al22 | USA 1995 | Patients with non‐diagnostic VQs and normal ultrasound | Unknown | 55% | 7/11 | 8/9 | 2 | 1 | 1 | 1 | 2 |
| Remy‐Jardin et al23 | France 1996 | Patients referred for pulmonary angiography | Unknown | 62% | 39/40 | 25/25 | 2 | 1 | 1 | 1 | 2 |
| Drucker et al24 | USA 1998 | Patients referred for pulmonary angiography | Unknown | 32% | 8/15 | 31/32 | 0 | 1 | 1 | 1 | 1 |
| Ruiz et al25 | Spain 2003 | Patients referred for pulmonary angiography | Unknown | 38% | 22/25 | 30/35 | 2 | 1 | 1 | 1 | 2 |
| Winer‐Muram et al26 | USA 2004 | Patients referred for pulmonary angiography | Unknown | 19% | 18/18 | 67/75 | 2 | 1 | 1 | 1 | 2 |
| Christiansen et al27 | Sweden 1997 | Patients with high clinical suspicion of PE | Unknown | 31% | 19/22 | 40/44 | 2 | 1 | 0 | 0 | 1 |
CTPA, computer tomography pulmonary angiogram; PE, pulmonary embolism; VQ, ventilation‐perfusion scan.
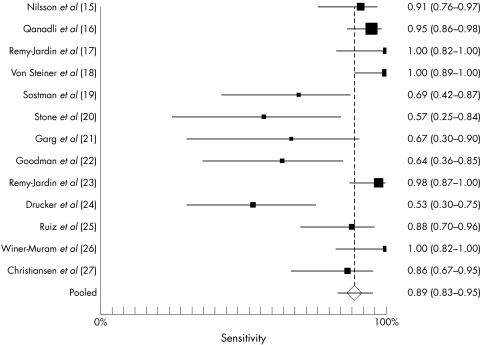
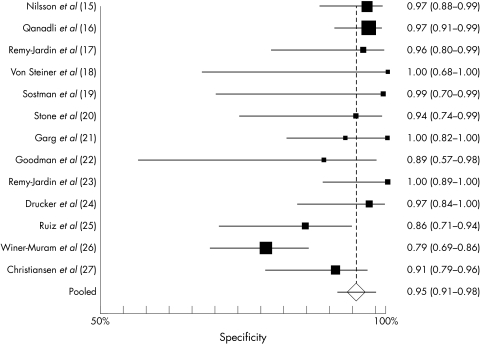
Figure 2 shows the weighted sensitivities for the diagnostic studies. Figure 3 shows the weighted specificities for the diagnostic studies. Sensitivity varied markedly between studies (Breslow‐Day test for heterogeneity p = 0.001). Although there was less variation in specificity, the studies were heterogeneous (Breslow‐Day test p = 0.004). The random effects pooled result for sensitivity was 88.9% (95% CI 82.0 to 95.0%) and specificity 94.6% (95% CI 91.3 to 98.0%). Subgroups were analysed (emergency department patients, patients with ventilation‐perfusion scans, patients with ultrasound scans, patients referred for pulmonary angiography, or studies with high appraisal scores). Two studies recruited mainly outpatients,15,16 both giving high sensitivity and specificity. No other subgroup analysis improved heterogeneity. Sensitivity and specificity were poorly correlated (Spearman p = 0.017).
Figure 2 Forest plot for sensitivity.
Figure 3 Forest plot for specificity.
Follow up studies
Eleven prospective follow up studies were identified (table 2).28,29,30,31,32,33,34,35,36,37,38 These ranged from unselected patients suspected of pulmonary embolic disease28,29,30 to patients with high clinical probability of pulmonary embolic disease and a non‐diagnostic ventilation‐perfusion scan.34 Four were multicentre studies.28,30,31,32 Only four studies28,30,31,32 insured that all patients underwent a uniform investigative process after the negative CT pulmonary angiogram. One study37 followed up patients for pulmonary embolism only, excluding data on deep venous thrombosis. Follow up ranged from examinations at six weeks and three months30 to one telephone call at six months.34 Seven studies achieved follow up rates of 95% or above. Two studies followed up 93% of patients29,37 and one study followed only 87%.36 Mortality during follow up was as high as 32%34 and 14%.29 Neither of these studies employed postmortem examination or an independent adjudication committee to ascertain cause of death. Four studies used an adjudication committee to review study deaths.28,30,31,32
Table 2 Follow up studies for analysis.
| Author | Country and year | Inclusion criteria | Outpatients (%) | Prevalence of PE | False negatives (%) | Study appraisal scores: 0 = no criteria fulfilled, 1 = only some criteria fulfilled, 2 = all criteria fulfilled. | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Follow up | Study cohort | Included patients | Excluded patients | CTPA protocol | ||||||
| Musset et al28 | France 2002 | All patients suspected of pulmonary embolism | 77% | 35% | 68/638 | 2 | 1 | 1 | 1 | 2 |
| Tillie‐Leblond et al29 | France 2002 | All patients suspected of pulmonary embolism | 85% | 30% | 19/201 | 1 | 1 | 2 | 1 | 2 |
| van Strijen et al30 | Holland 2003 | All patients suspected of pulmonary embolism | 54% | 24% | 5/378 | 2 | 1 | 1 | 1 | 2 |
| Perrier et al31 | Switzerland, France 2004 | Elevated D‐dimer and normal ultrasound | 100% | 23% | 9/413 | 2 | 1 | 2 | 2 | 2 |
| Perrier et al32 | Switzerland, France 2005 | Elevated D‐dimer or high clinical probability of pulmonary embolism | 100% | 26% | 8/324 | 2 | 1 | 2 | 1 | 2 |
| Ferretti et al33 | France 1997 | Normal ultrasound and intermedate VQ scan | 35% | 24% | 7/112 | 1 | 1 | 1 | 1 | 2 |
| Ost et al34 | USA 2001 | Patients with high clinical probability of PE and non‐diagnostic VQ scan | Unknown | 27% | 3/71 | 1 | 1 | 1 | 1 | 2 |
| Remy‐Jardin et al35 | France 2002 | Patients referred for CT pulmonary angiogram | 17% | 18% | 11/173 | 1 | 1 | 1 | 1 | 2 |
| Friera et al36 | Spain 2004 | Patients referred for CT pulmonary angiogram | Unknown | 25% | 1/115 | 1 | 1 | 1 | 0 | 2 |
| Revel et al37 | France 2005 | Patients referred for CT pulmonary angiogram | 44% | 24% | 7/140 | 1 | 1 | 1 | 0 | 2 |
| Prologo et al38 | USA 2005 | Patients referred for CT pulmonary angiography | Unknown | 10% | 2/198 | 1 | 1 | 1 | 1 | 2 |
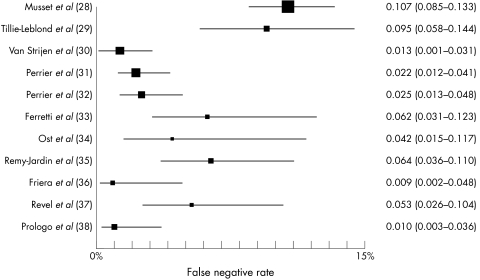
Figure 4 shows the weighted false negative rates for the follow up studies. The results are heterogeneous (Breslow‐Day test p = 0.000). A sensitivity analysis removing studies with poor appraisal scores did not reduce the heterogeneity, nor did patient subgroup analysis (emergency department patients, patients with ventilation‐perfusion scans, patients with ultrasound scans, or patients referred for pulmonary angiography).
Figure 4 Forest plot for false negative rate of CT pulmonary angiography.
The false negative rates were calculated for patients with both a negative investigation for deep vein thrombosis and negative CT angiography on presentation. The results are displayed in figure 5. The data are homogeneous (Breslow‐Day test p = 0.382). The random effects pooled false negative rate was 1.5% (95% CI 1.0 to 1.9%).
Figure 5 Forest plot for false negative rate of combined CT pulmonary angiography and DVT investigation. (Study 29 all had CT but only 84% cohort had an ultrasound scan. Study 37 all had CT but only 90% cohort had CT venography.)
Discussion
There are very few high quality studies assessing the diagnostic utility of CT pulmonary angiography in pulmonary embolism. Few study cohorts represent the emergency department population. There are conflicting results for the sensitivity and specificity of CT pulmonary angiography. The false negative rate for CT pulmonary angiography varies between studies. The pooled false negative rate for combining negative CT pulmonary angiography with a negative investigation for deep vein thrombosis was 1.5% (95% CI 1.0 to 1.9%).
Sensitivity of CT pulmonary angiography is heterogeneous ranging from 53% to 100%. The pooled result for sensitivity was 88.9% (95% CI 82.0 to 95.0%), however given the heterogeneous study methods and populations (as noted by Eng et al39) this figure may not accurately represent the true value for sensitivity. It is possible that radiologists in different studies interpret CT pulmonary angiograms using different thresholds for the cut off point between a positive and negative scan. However variation cannot be explained by a cut off point effect since sensitivity and specificity are poorly correlated. Most studies calculated sensitivity with very small cohorts and large confidence intervals. Two of the largest studies15,16 recruited outpatients (emergency department patients) finding sensitivities of 91% (95% CI 76 to 97%) and 95% (95% CI 86 to 98%). They had a similar prevalence of disease (37% and 39% respectively) and may be most representative of the emergency department population. Both studies used single slice scanners and scored reasonable appraisal scores.
Specificity varied less. The pooled specificity result was 94.6% (95% CI 91.3 to 98.0%). All results were over 90% with the notable exception of two studies.25,26 The study by Ruiz et al used a single slice scanner and recruited patients referred for pulmonary angiography. No demographics were provided about the patient cohort, and it is hard to establish why this study differed from the others. Winer‐Muram et al were the only diagnostic study researchers to use a four channel multidetector row CT scanner. Notably, this did not appear to improve the ability to correctly exclude smaller peripheral emboli and gave the poorest specificity result of 79% (95% CI 69 to 86%).
Almost all diagnostic studies used pulmonary angiography as the reference standard investigation. Pulmonary angiography can diagnose pulmonary emboli in the small, peripheral pulmonary vasculature. Single slice CT scanning may be less accurate in identifying these emboli. However clinicians are uncertain of the clinical significance of such small emboli which may not require anticoagulant therapy. Follow up studies provide practical evidence on the clinical safety of withholding anticoagulant therapy from patients who have thromboembolism excluded on CT scan. This is a more relevant question for the emergency physician.
The reported false negative rates varied between studies from 0.9% to 10.7%. In this analysis we considered deep vein thrombosis to be a marker for pulmonary embolism as deep vein thrombosis is a manifestation of the same disease. Our false negative results may be an overestimation as not every patient with a deep vein thrombosis will have a pulmonary embolism. In fact patients with a recent diagnosis of venous thrombosis may become concerned about relatively benign chest symptoms and be recruited onto a study.
The pooled false negative rate for combined negative CT angiography and negative deep vein thrombosis testing was 1.5% (95% CI 1.0 to 1.9%). Despite the varied results on sensitivity and specificity, CT pulmonary angiography in combination with ultrasonography or CT venography appears to be a safe approach to the exclusion of pulmonary embolism. Our results concord with an older review40 which showed that studies combining a negative CT pulmonary angiogram with a negative ultrasound gave a smaller estimated negative likelihood ratio for pulmonary embolism than other conventional diagnostic tests. The PIOPED study10 demonstrated that a normal pulmonary angiogram has a false negative rate of 1.6%. This is similar to CT combined with deep vein thrombosis testing. CT avoids cardiac catheterisation, can be performed more readily in more hospitals and facilitates the diagnosis of other emergency conditions commonly mistaken for pulmonary embolism.
Most studies in this review used a single slice CT scanner. Today, many hospitals have multislice CT scanners which produce images with less movement artefact, better arterial contrast filling, and more detail. Although our results may not be applicable to multislice CT scanners we might see an increase in CT accuracy with the new technology, rather than a reduction.
We chose not to categorise results by the site of the pulmonary embolism. Although this may be seen as a criticism of the review, in the practicing world physicians request a CT pulmonary angiogram without specifying the levels to which images should be analysed. Likewise we chose not to look at interobserver variation in CT reporting. A meta‐analysis will not establish accuracy of reporting in a given institution. Instead we focussed on three simple outcomes: sensitivity, specificity, and false negative rate.
Follow up studies give vital evidence on the safety of withholding treatment after a normal CT pulmonary angiogram and for that reason were included. Two other reviews41,42 have pooled information from follow up studies. However the authors included retrospective studies and quoted the authors' non‐standardised false negative rates. We chose to exclude retrospective studies to ensure a higher standard of follow up data and independently recalculated the sensitivity, specificity, and false negative rates.
Before the true sensitivity and specificity of CT pulmonary angiography can be estimated, more multicentre studies of high quality are required. Most UK hospitals use multislice scanners (with up to 64 channels). As yet, there is little evidence on the diagnostic utility of multislice CT pulmonary angiograms. With rapidly progressing technology and accumulative CT interpretation experience, we may find results with compatible accuracy to pulmonary angiography.
Supplementary Material
Acknowledgements
The authors would like to acknowledge the help provided by Michelle Jenkins and Katherine Wylie in sourcing the journal papers.
Contributors‘ statement
KH designed the study. KH, GB, JW, BF, and KMJ participated in the systematic review, data extraction and study appraisal. JD provided statistical expertise. KH, BF, SC, and KMJ drafted the paper.
Footnotes
Financial support: none.
Competing interests: none declared
References
- 1.Stein P D, Willis P W, DeMets D L. History and physical examination in acute pulmonary embolism in patients without pre‐existing cardiac or pulmonary disease. Am J Cardiol 198147218–223. [DOI] [PubMed] [Google Scholar]
- 2.Stein P D, Henry J W. Clinical characteristics of patients with acute pulmonary embolism stratified according to their presenting syndromes. Chest 1997112974–979. [DOI] [PubMed] [Google Scholar]
- 3.Susec O, Boudrow D, Kline J A. The clinical features of acute pulmonary embolus in ambulatory patients. Acad Emerg Med 199749891–897. [DOI] [PubMed] [Google Scholar]
- 4.Douketis J D, Kearon C, Bates S.et al Risk of fatal pulmonary embolism in patients with treated venous thromboembolism. JAMA 1998279458–462. [DOI] [PubMed] [Google Scholar]
- 5.Wells P S, Anderson D R, Rodger M.et al Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d‐dimer. Ann Intern Med 200113598–107. [DOI] [PubMed] [Google Scholar]
- 6.Ginsberg J S, Wells P S, Kearon C.et al Sensitivity and specificity of a rapid whole‐blood assay for D‐dimer in the diagnosis of pulmonary embolism. Ann Intern Med 19981291006–1011. [DOI] [PubMed] [Google Scholar]
- 7.Kruip M J, Slob M J, Schijen J H.et al Use of a clinical decision rule in combination with D‐dimer concentration in diagnostic workup of patients with suspected pulmonary embolism: a prospective management study. Arch Intern Med 20021621631–1635. [DOI] [PubMed] [Google Scholar]
- 8.The Pioped Investigators Value of the ventilation/perfusion scan in acute pulmonary embolism. Results of the prospective investigation of pulmonary embolism diagnosis (PIOPED). JAMA 19902632753–2759. [DOI] [PubMed] [Google Scholar]
- 9.Stein P D, Athanasoulis C, Alavi A.et al Complications and validity of pulmonary angiography in acute pulmonary embolism. Circulation 199285462–468. [DOI] [PubMed] [Google Scholar]
- 10.Henry J W, Relyea B, Stein P D. Continuing risk of thromboemboli among patients with normal pulmonary angiograms. Chest 19951071375–1378. [DOI] [PubMed] [Google Scholar]
- 11.Richman P, Courtney D, Friese J.et al Chest CT angiography (CTA) to rule‐out pulmonary embolism (PE) frequently reveals clinically significant ancillary findings: a multicentre study of 1025 emergency department patients. Acad Emerg Med 200310564–565. [Google Scholar]
- 12.American College of Emergency Physicians Clinical Policies Committee, Clinical Policies Committee Subcommittee on Suspected Pulmonary Embolism Clinical policy: critical issues in the evaluation and management of adult patients presenting with suspected pulmonary embolism. Ann Emerg Med 200341257–270. [DOI] [PubMed] [Google Scholar]
- 13.Campbell I A, Fennerty A, Miller A C.et al British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax 200358470–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deville W L, Buntinx F, Bouter L M.et al Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 200229–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nilsson T, Soderberg M, Lundqvist G.et al A comparison of spiral computed tomography and latex agglutination D‐dimer assay in acute pulmonary embolism using pulmonary arteriography as gold standard. Scand Cardiovasc J 200236373–377. [DOI] [PubMed] [Google Scholar]
- 16.Qanadli S D, Hajjam M E, Mesurolle B.et al Pulmonary embolism detection: prospective evaluation of dual‐section helical CT versus selective pulmonary arteriography in 157 patients. Radiology 2000217447–455. [DOI] [PubMed] [Google Scholar]
- 17.Remy‐Jardin M, Remy J, Wattinne L.et al Central pulmonary thromboembolism: diagnosis with spiral volumetric CT with the single‐breath‐hold technique—comparison with pulmonary angiography. Radiology 1992185381–387. [DOI] [PubMed] [Google Scholar]
- 18.Steiner P, Phillips F, Wesner D.et al Primary diagnosis and follow‐up of acute pulmonary emboli: Comparison between digital subtraction angiography and spiral CT. Fortschr Rontgenstr 1994161285–291. [DOI] [PubMed] [Google Scholar]
- 19.Sostman H D, Layish D T, Tapson V F.et al Prospective comparison of helical CT and MR imaging in clinically suspected acute pulmonary embolism. J Magn Reson Imaging 19966275–281. [DOI] [PubMed] [Google Scholar]
- 20.Stone E, Roach P, Bernard E.et al Use of computed tomography pulmonary angiography in the diagnosis of pulmonary embolism in patients with an intermediate probability ventilation/perfusion scan. Intern Med J 20033374–78. [DOI] [PubMed] [Google Scholar]
- 21.Garg K, Welsh C H, Feyerabend A J.et al Pulmonary embolism: diagnosis with spiral CT and ventilation‐perfusion scanning‐correlation with pulmonary angiographic results or clinical outcome. Radiology 1998208201–208. [DOI] [PubMed] [Google Scholar]
- 22.Goodman L R, Curtin J J, Mewissen M W.et al Detection of pulmonary embolism in patients with unresolved clinical and scintigraphic diagnosis: helical CT versus angiography. Am J Roentgenol 19951641369–1374. [DOI] [PubMed] [Google Scholar]
- 23.Remy‐Jardin M, Remy J, Deschildre F.et al Diagnosis of pulmonary embolism with spiral CT: comparison with pulmonary angiography and scintigraphy. Radiology 1996200699–706. [DOI] [PubMed] [Google Scholar]
- 24.Drucker E A, Rivitz S M, Shepard J A.et al Acute pulmonary embolism: assessment of helical CT for diagnosis. Radiology 1998209235–241. [DOI] [PubMed] [Google Scholar]
- 25.Ruiz Y, Caballero P, Caniego J L.et al Prospective comparison of helical CT with angiography in pulmonary embolism: global and selective vascular territory analysis. Interobserver agreement. Eur Radiol 200313823–829. [DOI] [PubMed] [Google Scholar]
- 26.Winer‐Muram H T, Rydberg J, Johnson M S.et al Suspected acute pulmonary embolism: evaluation with multi‐detector row CT versus digital subtraction pulmonary arteriography. Radiology 2004233(3)806–815. [DOI] [PubMed] [Google Scholar]
- 27.Christiansen F. Diagnostic imaging of acute pulmonary embolism. Acta Radiol Suppl 19974101–33. [PubMed] [Google Scholar]
- 28.Musset D, Parent F, Meyer G.et al Diagnostic strategy for patients with suspected pulmonary embolism: a prospective multicentre outcome study. Lancet 20023601914–1920. [DOI] [PubMed] [Google Scholar]
- 29.Tillie‐Leblond I, Mastora I, Radenne F.et al Risk of pulmonary embolism after a negative spiral CT angiogram in patients with pulmonary disease: 1‐year clinical follow‐up study. Radiology 2002223461–467. [DOI] [PubMed] [Google Scholar]
- 30.van Strijen M J, de Monye W, Schiereck J.et al Single‐detector helical computed tomography as the primary diagnostic test in suspected pulmonary embolism: a multicenter clinical management study of 510 patients. Ann Intern Med 2003138307–314. [DOI] [PubMed] [Google Scholar]
- 31.Perrier A, Roy P M, Aujesky D.et al Diagnosing pulmonary embolism in outpatients with clinical assessment, D‐dimer measurement, venous ultrasound, and helical computed tomography: a multicenter management study. Am J Med 2004116291–299. [DOI] [PubMed] [Google Scholar]
- 32.Perrier A, Roy P M, Sanchez O.et al Multidetector‐row computed tomography in suspected pulmonary embolism. N Eng J Med 20053521760–1768. [DOI] [PubMed] [Google Scholar]
- 33.Ferretti G R, Bosson J L, Buffaz P D.et al Acute pulmonary embolism: role of helical CT in 164 patients with intermediate probability at ventilation‐perfusion scintigraphy and normal results at duplex US of the legs. Radiology 1997205453–458. [DOI] [PubMed] [Google Scholar]
- 34.Ost D, Rozenshtein A, Saffran L.et al The negative predictive value of spiral computed tomography for the diagnosis of pulmonary embolism in patients with nondiagnostic ventilation‐perfusion scans. Am J Med 200111016–21. [DOI] [PubMed] [Google Scholar]
- 35.Remy‐Jardin M, Tillie‐Leblond I, Szapiro D.et al CT angiography of pulmonary embolism in patients with underlying respiratory disease: impact of multislice CT on image quality and negative predictive value. Eur Radiol 2002121971–1978. [DOI] [PubMed] [Google Scholar]
- 36.Friera A, Olivera M J, Suarez C.et al Clinical validity of negative helical computed tomography for clinical suspicion of pulmonary embolism. Respiration 20047130–36. [DOI] [PubMed] [Google Scholar]
- 37.Revel M P, Petrover D, Hernigou A.et al Diagnosing pulmonary embolism with four‐detector row helical CT: prospective evaluation of 216 outpatients and inpatients. Radiology 2005234265–273. [DOI] [PubMed] [Google Scholar]
- 38.Prologo J D, Gilkeson R C, Diaz M.et al The effect of single detector CT versus MDCT on clinical outcomes in patients with suspected acute pulmonary embolism and negative results on CT pulmonary angiography. Am J Roentgen 20051841231–1234. [DOI] [PubMed] [Google Scholar]
- 39.Eng J, Krishnan J A, Segal J B.et al Accuracy of CT in the diagnosis of pulmonary embolism: a systematic literature review. Am J Roentgen1831819–1827. [DOI] [PubMed] [Google Scholar]
- 40.Roy P, Colombet I, Durieux P.et al Systematic review and meta‐analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ 2005331259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moores L K, Jackson W L, Shorr A F.et al Meta‐analysis: outcomes in patients with suspected pulmonary embolism managed with computed tomographic pulmonary angiography. Ann Int Med 2004141866–874. [DOI] [PubMed] [Google Scholar]
- 42.Quiroz B, Kucher N, Zou K H.et al Clinical validity of a negative computed tomography scan in patients with suspected pulmonary embilsm. A systematic review. JAMA 20052932012–2017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.