Abstract
Objectives
Reconfiguration of emergency services could lead to patients with life‐threatening conditions travelling longer distances to hospital. Concerns have been raised that this could increase the risk of death. We aimed to determine whether distance to hospital was associated with mortality in patients with life‐threatening emergencies.
Methods
We undertook an observational cohort study of 10 315 cases transported with a potentially life‐threatening condition (excluding cardiac arrests) by four English ambulance services to associated acute hospitals, to determine whether distance to hospital was associated with mortality, after adjustment for age, sex, clinical category and illness severity.
Results
Straight‐line ambulance journey distances ranged from 0 to 58 km with a median of 5 km, and 644 patients died (6.2%). Increased distance was associated with increased risk of death (odds ratio 1.02 per kilometre; 95% CI 1.01 to 1.03; p<0.001). This association was not changed by adjustment for confounding by age, sex, clinical category or illness severity. Patients with respiratory emergencies showed the greatest association between distance and mortality.
Conclusion
Increased journey distance to hospital appears to be associated with increased risk of mortality. Our data suggest that a 10‐km increase in straight‐line distance is associated with around a 1% absolute increase in mortality.
Keywords: emergency services, health service research, mortality
It has recently been suggested that reconfiguration of emergency care to concentrate services in a limited number of specialist centres could save thousands of lives each year in the UK, and that opposing the closure of local services could counterintuitively cost lives.1 In opposition to this view, concerns have been raised that reconfiguration could lead to acutely ill patients having to be transported greater distances to hospital with an associated risk of increased mortality. Few published studies have addressed this issue, so there is a risk that policy‐making may be driven by anecdote or supposition.
We have recently completed a study to assess the effect on mortality among patients with life‐threatening emergencies of implementing response time standards in four ambulance services.2 We have used these data to determine whether longer journey distances to hospital were associated with an increased risk of mortality.
Methods
Call identification
Ambulance services use emergency medical dispatch (EMD) systems to prioritise 999 calls. Two systems were used during this study: the Advanced Medical Priority Dispatch System (AMPDS) and the Criteria Based Dispatch (CBD) system. Each provides structured protocols that allow trained emergency medical dispatchers to categorise 999 calls depending on urgency, and assigns each call a priority code based on condition and urgency. The Department of Health (DH) has identified a set of EMD codes for each system that correspond to conditions that are potentially life‐threatening and to which the highest priority (category A) ambulance response should be made. We selected for inclusion in the study a subgroup of category A calls identified using the DH codes, in which the patient was reported as unconscious or not breathing or with acute chest pain. We termed these A* calls. Exclusion criteria were A* calls where patients were found dead at the scene, or were discharged at the scene and not conveyed to hospital, or were treated in hospitals other than those in our study areas; calls where no vehicle attended the scene; and out‐of‐hospital cardiac arrests (the last category was excluded because survival from out‐of‐hospital cardiac arrest has clearly been shown to depend upon the time from call to treatment that can be provided by ambulance staff, rather than time or distance from scene to hospital).3
Data collection
Consecutive, life‐threatening category A ambulance calls were sampled annually from 1997 to 2001 from four ambulance services: the Royal Berkshire, Derbyshire, Essex and West Midlands. These services were representative of the types of environment typically encountered in England and included urban, mixed urban and rural, and very rural areas. In 1999, the Derbyshire, Nottinghamshire and Leicestershire ambulance services merged to become East Midlands Ambulance Service NHS Trust. Two services used CBD, one used AMPDS, and one used CBD at the beginning of the study and changed to AMPDS halfway through.
From all category A calls, we sampled approximately 1000 consecutive A* calls from each service in each year, using the same sampling period for each service for all years. The ambulance service dispatch system provided patient information (name, sex, age), grid reference for the incident, and dispatch category codes. This information was then used to identify the paper ambulance patient report forms (PRFs). From the PRFs, further information was obtained about the patient (name, date of birth and address), incident description, the patient condition on arrival of the crew (including vital signs), details of treatment given, disposal of the patient (left at the scene or transported to hospital) and outcome at this point (alive or deceased).
From the grid references of the incident and hospital, we calculated the straight‐line ambulance journey distance from scene to hospital. These straight‐line distances were preferred to journey times to hospital because journey times depend on the accuracy and consistency with which times of leaving the scene and arrival at hospital are recorded, and they can also be affected by ”reverse causation”. This occurs when the patient condition is a cause of the journey time rather than vice versa, such as when ambulances drive as fast as possible to hospital for critically ill patients but more slowly and with less risk for patients not critically ill.
If the patient was taken to hospital, the emergency department (ED) notes were identified and information recorded on time of arrival and discharge from the ED, patient condition including vital signs, cardiac rhythm (for cardiac patients), preliminary diagnosis, condition on leaving the ED and disposal. If admitted, details of the length of stay, final diagnosis and disposition were recorded. For any patient who died, details were recorded of the date, time, place and cause of death. If the patient died before reaching hospital and was taken directly to the mortuary, the cause of death was obtained by accessing death certificates from the coroner or the National Health Service (NHS) Central Registry.
Details of patients taken to hospital, for whom no records could be found, were also sent to the NHS Central Registry. For those identified as dead, the date, place and cause of death were obtained and used to identify those who had died as a result of the incident for which the call was made and those who had survived.
Ethics approval was obtained, covering 27 hospitals that patients could be taken to within the geographical boundary of each of the ambulance services.
Analysis
We planned to test for an association between journey distance to hospital and mortality. Such an association could be confounded by illness severity. Patients living further from hospital may have a higher threshold for calling for help and may therefore be more ill and at higher risk of death. There is currently no widely validated system for risk‐adjusting emergency medical cases, but the Rapid Emergency Medicine Score (REMS) has been validated in a local setting4 and shown to predict mortality in our cohort.5 This score uses six variables (age, Glasgow Coma Score (GCS), oxygen saturation, pulse, blood pressure and respiratory rate) to give each patient a score between 0 (lowest predicted mortality) and 20 (highest). We therefore planned to examine whether patients with a longer journey distance had higher REMS scores and determine whether any association between distance and mortality was confounded by illness severity by testing the association in a multivariate analysis, with REMS score included as a covariate. Because full REMS scores were only available for a small number of patients, we also tried adjusting for partial scores based only on age and GCS, which were available for 80.8% of patients. We also tried adjusting for sex, categorical age, and clinical category coded as chest pain (any cause), respiratory disease or symptoms, and injury, poisoning, asphyxiation or haemorrhage, or other and unknown. By including ”other and unknown” as a category all cases were included in this analysis. All analyses were undertaken using SPSS V.11.0 (SPSS Inc, Chicago, Illinois, USA).
Results
Numbers
During the 5‐year period, A* calls resulted in ambulance attendance for 11 794 patients who met the study inclusion criteria and who were followed up to discharge or traced through the NHS Central Register. Of these, we excluded 1479 from this analysis because distance to hospital could not be calculated. This resulted in a study sample of 10 315 (58.3% male, with a median age of 61 years).
Analyses
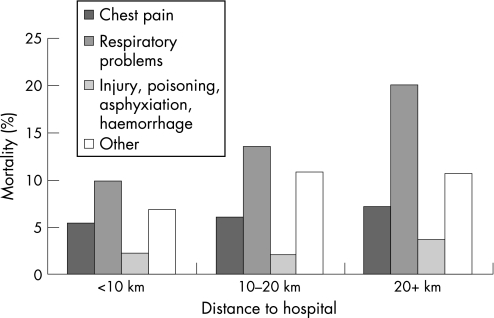
Ambulance journey distances ranged from 0 to 58 km, with a median of 5 km. Overall, 644 patients died (6.2%). Table 1 shows how mortality varied with straight‐line distances, categorised as short (<10 km), medium (10–20 km) or long (>20 km). Longer distances were associated with higher mortality (p<0.002, χ2 test for trend). Logistic regression showed that mortality increased with each additional kilometre of distance travelled, with an odds ratio (OR) of 1.02 per kilometre (95% CI 1.01 to 1.03; p<0.001). Some association was observed in all four clinical categories, but it was particularly striking for patients with respiratory problems (fig 1).
Table 1 Relationship between ambulance journey distance and survival to discharge.
| Distance category (km) | Outcome | Total | |
|---|---|---|---|
| Survived (%) | Died (%) | ||
| 0–10 | 7725 (94.2) | 475 (5.8) | 8200 |
| 11–20 | 1479 (92.3) | 124 (7.7) | 1603 |
| 21+ | 467 (91.2) | 45 (8.8) | 512 |
| Total | 9671 (93.8) | 644 (6.2) | 10315 |
Figure 1 Variation in mortality with distance to hospital, by clinical category.
A full REMS score could be calculated for 3882 patients (37.6%). The mean REMS score was 6.79 (95% CI 6.67 to 6.91) for those with a short journey distance, 7.22 (6.92 to 7.51) for those with a medium journey distance and 7.33 (6.78 to 7.88) for those with a long journey distance. The association between journey distance and mortality remained significant after inclusion of REMS score in the logistic regression to adjust for potential confounding by disease severity (OR = 1.03; 95% CI 1.01 to 1.05; p = 0.006).
Missing oxygen saturation information was the main reason why a full REMS score could not be calculated, so we repeated the analysis using only the age and GCS components of REMS. We have previously shown that age, GCS and oxygen saturation are the only components of the REMS score that are independent predictors of mortality in our cohort.5 We were able to include 8335 (80.8%) cases and found that the association between journey distance and mortality remained significant (OR = 1.018; 95% CI 1.005 to 1.03; p = 0.005).
Adjusting for age, sex, and clinical category, and including all 10 315 patients in the analysis, strengthened the evidence for the observed association (OR = 1.02; 95% CI 1.01 to 1.03; p<0.001).
Discussion
Increased journey distance to hospital seems to be associated with increased risk of mortality, even after potential confounding by illness severity is taken into account. Our data suggest that each additional kilometre is associated with a 2% relative increase in mortality. This equates to an approximate 1% absolute increase in mortality associated with each 10‐km increase in straight‐line distance. Our results show a sharp increase in mortality in patients with respiratory problems, but less change in patients with chest pain. This is clinically plausible. This means that, other things being equal, closing local EDs could result in an increase in mortality for a small number of patients with life‐threatening emergencies, who have to travel further as a result.
Other evidence
Our results concur with a number of studies from around the world that have shown increased mortality in rural compared with urban trauma. However, much of this can be explained by the increased severity of road traffic crashes and increased ambulance response times in rural areas. Furthermore, results may not be generalisable from trauma to other emergency medical conditions nor from one emergency system to another. Only a few studies have examined hospital accessibility and outcomes in the UK. Studies of road traffic crashes in Norfolk,6 all serious trauma in Scotland,7 and ruptured abdominal aortic aneurysms in West Sussex8 all failed to find any relationship between time to hospital and mortality. However, in line with our findings, two studies of the relationship between accessibility and mortality in asthma patients have found a 10% increase in the relative risk of death for each 10‐km increase in distance,9 and a 7% increase for each 10‐minute increase in journey time.10
Limitations
A number of potential limitations of our study should be considered when interpreting these results. First, this is an observational study, and inferring causality from our observed associations is fraught with difficulties, most notably by confounding. Although we attempted to adjust for confounding by illness severity and case mix, it is possible that at least some of the observed association may be explained by residual confounding. Second, we deliberately selected ambulance service calls that suggested patients might have life‐threatening conditions and a high risk of mortality. Our findings should not be applied to the vast majority of patients transported to hospital by ambulance, who have a much lower risk of death. Third, our results reflect associations between distance and outcome within the emergency care system as it performed between 1997 and 2001. Changes in performance in recent years or new policies that have changed to both increase distances and either improve care at the more distant facilities or improve the effectiveness of prehospital care could attenuate the potential effect of increased journey distance upon mortality.
The emergency medical system and future research
There is good evidence for some groups of emergency patients that care provided in specialist centres improves outcomes.1 Examples include primary angioplasty for acute myocardial infarction,11 and care for major trauma patients with multiple injuries.12 In these cases we can be reasonably confident that with appropriate pre‐hospital care and at distances typical in the UK, the benefits of specialist care, which is only available in certain centres, would outweigh any detriments resulting from the increased travel distances to the centres. However, there are also some groups of critically ill patients who need urgent but not specialist care. For example, patients in anaphylactic shock, choking, drowning, or having acute asthma attacks need urgent care that would be the same wherever it is provided. For these patients, there may be a detriment in having to travel increased distances. Of course, if care for these types of patients, although the same wherever it is provided, were to be of higher quality in high‐volume centres, there might be other arguments for concentrating emergency care in some centres by closing local EDs. However, although the evidence for improved outcomes at higher volumes is reasonably robust for a few conditions,13 it is almost non‐existent for ED care.14
The debate between local emergency care and more distant, high‐volume or specialist centre care has also confused the issue of hospital bypass with the issue of ED closure. The evidence that some critically ill patients have the capacity to benefit from specialist care is an argument for bypass, not an argument for closure or restriction of hours of non‐specialist centres. Patients with specialist needs such as burns and serious head trauma are already taken directly or indirectly to specialist centres. The current debate should be about extending the list of patient conditions that should bypass local hospitals and be taken to specialist centres, rather than about the closure of locally accessible 24‐hour EDs. Closure enforces bypass for those patients who would benefit but at a cost for any patients who will not benefit.
Nevertheless, the optimum configuration of local and specialist emergency care centres for an effective and efficient emergency care system is unclear. Research is needed to investigate the benefits of different system configurations rather than the effectiveness of different services. One potentially fruitful avenue for future research aimed at resolving these issues would be to model the emergency medical system, populating the model based on the epidemiology of emergencies in the UK, and using the available evidence on risks and benefits by distance or time and setting.
Conclusion
Decisions regarding reconfiguration of acute services are complex, and require consideration of many conflicting factors. Our data suggest that any changes that increase journey distances to hospital for all emergency patients may lead to an increase in mortality for a small number of patients with life‐threatening medical emergencies, unless care is improved as a result of the reorganisation. However, even then it is not certain that it would be acceptable to trade an increased risk for some groups of patients, such as those with severe respiratory compromise, for a reduced risk in other groups such as those with myocardial infarction.
Abbreviations
AMPDS - Advanced Medical Priority Dispatch System
CBD - Criteria Based Dispatch
DH - Department of Health
ED - emergency department
EMD - emergency medical dispatch
GCS - Glasgow Coma Score
NHS - National Health Service
PRF - patient report form
REMS - Rapid Emergency Medicine Score
Footnotes
Funding: The original ambulance response times study was undertaken by the Medical Care Research Unit, which is core funded by the UK Department of Health. The views expressed here are those of the authors and not necessarily those of the Department.
Competing interests: None.
References
- 1.Farrington‐Douglas J, Brooks R.The future hospital: The progressive case for change. London: Institute for Public Policy Research, 2007, http://www.ippr.org.uk/members/download.asp?f = %2Fecomm%2Ffiles%2Ffuture%5Fhospital%2Epdf Accessed 13 July 2007
- 2.Turner J, O'Keefe C, Dixon S.et alThe costs and benefits of changing ambulance service response time standards. Sheffield: Medical Care Research Unit, University of Sheffield, 2005
- 3.Larsen M P, Eisenberg M S, Cummins R O.et al Predicting survival from out‐of‐hospital cardiac arrest: A graphic model. Ann Emerg Med 2003221652–1658. [DOI] [PubMed] [Google Scholar]
- 4.Olsson T, Terent A, Lind L. Rapid Emergency Medicine Score: a new prognostic tool for in‐hospital mortality in nonsurgical emergency department patients. J Intern Med 2004255579–587. [DOI] [PubMed] [Google Scholar]
- 5.Goodacre S, Turner J, Nicholl J P. Prediction of mortality among emergency medical admissions. Emerg Med J 200523372–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones A P, Bentham G. Emergency medical service accessibility and outcomes from road traffic accidents. Public Health 1995109169–177. [DOI] [PubMed] [Google Scholar]
- 7.McGuffie A C, Graham C A, Beard D.et al Scottish urban versus rural trauma outcome study. J Trauma 200559632–638. [PubMed] [Google Scholar]
- 8.Souza V C, Strachan D P. Relationship between travel time to the nearest hospital and survival from ruptured aortic aneurysm: record linkage study. J Public Health 200527165–170. [DOI] [PubMed] [Google Scholar]
- 9.Jones A P, Bentham G. Health service accessibility and deaths from asthma in 401 local authority districts in England and Wales, 1988–92. Thorax 199752218–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones A P, Bentham G, Horwell C. Health service accessibility and deaths from asthma. Int J Epidemiol 199928101–105. [DOI] [PubMed] [Google Scholar]
- 11.Keeley E C, Boura J A, Grines C L. Primary angioplasty versus intravenous thrombolytic therapy of acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 200336113–20. [DOI] [PubMed] [Google Scholar]
- 12.Freeman J, Nicholl J, Turner J. Does size matter? The relationship between volume and outcome in the care of major trauma. J Health Serv Res Policy 200611101–105. [DOI] [PubMed] [Google Scholar]
- 13.Halm E A, Lee C, Chassin M R. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 2002137511–520. [DOI] [PubMed] [Google Scholar]
- 14.Chase M, Hollander J E. Volume and outcome: the more patients the better? Ann Emerg Med 200648657–659. [DOI] [PubMed] [Google Scholar]