Abstract
Background
Experts call for stronger safety cultures and transparent reporting practices to increase medication safety in today's strained healthcare environments. The field of ecological restoration is concerned with the effective, efficient, and sustainable repair and recovery of ecosystems that have been degraded, damaged, or destroyed. A study was undertaken to determine whether the lessons of restoration science can be adapted to the study of medication safety issues.
Methods
Working with 26 practitioners, the principles of good restoration were used to design and pilot an innovative multifaceted medication safety intervention. The intervention included focus groups with practitioners, the construction and administration of a research based medication safety inventory, repeat digital photography of environmental safety issues, and targeted environmental modifications.
Results
Participants were most concerned about staff education and the physical environment for medication administration. Ward staff used the research to build a healthy reporting culture, introduce regular discussions of near misses, develop education strategies, redesign delivery and storage processes, and renovate the environment.
Conclusions
Members of a busy hospital ward successfully adapted methods of restoration science to study, redesign, and strengthen medication safety practices and ward safety culture within existing resources. Further research will be conducted to test the merits of restoration science for health care.
Keywords: ecological design, repeat photography, medication safety, restoration science, safety culture
Strengthening the environment for medication safety is a significant challenge for modern health systems. Similar to earlier reports in other countries,1,2,3 approximately 7.5% of patient admissions to a cross‐national sample of Canadian acute care hospitals were associated with an adverse event,4 and a considerable number of adverse events that occur in hospitals are related to medications.5 Healthcare leaders now recognize the importance of systemic approaches to patient safety that account for interrelated human and organizational factors,6,7,8,9 but our abilities to translate sound systems thinking into better care continues to lag.10 There is a call for further patient safety research that is guided by explicit theoretical frameworks,11,12,13,14,15 but we have not reached theoretical agreement on what kind of system a healthcare system is.16 Nonetheless, there is a growing consensus that today's technological healthcare environments are high risk places where practitioners, managers, and patients navigate the practical complexities of dynamic living systems that are fraught with uncertainty.17,18,19,20 As Wears and Cook observe, we are most likely to strengthen the safety of messy, real world clinical practice when we learn to use the scientific wisdom from many disciplines to discover “the sources of power that make the healthcare delivery system resilient and robust”.21 With this context for patient safety science in view, we seek to adapt the principles and techniques of another form of messy, real world healing work—that of ecological restoration—to the study and repair of today's complex strained healthcare systems.6,22,23,24 We report here on the use of restoration theory to design and pilot a multifaceted medication safety intervention for a busy medical ward at a tertiary acute care site, the Royal Alexandra Hospital.
The field of ecological restoration is concerned with the effective, efficient, and sustainable repair and recovery of ecosystems that have been degraded, damaged, or destroyed (table 1).25 In effect, restoration science and the companion endeavor of ecosystems management combine aspects of human systems thinking with ecological knowledge of living systems in order to develop best practices in continuous nested cycles of research, evaluation, and adaptive management.26,27,28,29,30 Most contemporary restoration scientists advocate a deep respect for the history of places without aiming for a return to an idealized pristine past, focusing instead on the collaborative design and implementation of practical lasting repairs that are ethically, scientifically, and culturally sound.26,27 Scientific methods in restoration research include working with local communities and stakeholders to assess the health of the environment and its inhabitants; observation of local customs and practices; repeat photography to document patterns of land use over time; and the mapping of degraded terrain.31 The knowledge generated through restoration research enables us to use our finite resources more efficiently, to identify and support critical redundant feedback mechanisms, to reduce patterns of unnecessary consumption, to mitigate the effects of pollutants and toxins, and to plan for the adaptive management of complex living systems.23,32
Table 1 Principles of ecological restoration for complex healthcare systems.
| Good restorations are ecologically effective | Effective restorations revitalize the adaptive capacities of living systems by implementing repairs that (1) increase the ecological integrity or self‐organizing capacities of the system (for example, by improving system processes that enable self‐monitoring and correction); and (2) maintain fidelity to the significant history of a place (for example, by acknowledging the impact of a merger on a hospital community) |
| Good restorations are ecologically efficient | Ecologically efficient restorations focus on setting safe margins for error and sustainable levels of production over time. Short term, cost effective repairs are balanced with longer range investments that allow us to maintain and renew (rather than maximize and deplete) critical human and material resources. For example, if we deploy more expert older practitioners into clinical mentoring roles with reduced patient loads, we might recoup any extra labor costs within a relatively short timeframe as we reduce early attrition from the workforce, decrease overtime, and increase the safety of frontline clinical supervision and decision making |
| Good restorations build ethical cultures by design | Good restorations last because they engage us in communal work that improves the way we treat each other and the places we share. The rebuilding of ecological and cultural integrity go hand in hand as we redevelop shared knowledge, ethical relations, and cultural practices that enable us to maintain safer better places in which to give and receive care |
The Royal Alexandra Hospital is a 700 bed teaching and referral hospital in the heart of the city which serves approximately 32 500 inpatients and 112 000 outpatients from the region and across northern Alberta every year. Like so many colleagues across the globe, our leaders, physicians, staff and patients have weathered a decade of health care re‐engineering, cost constraints, and change initiatives. As an interdisciplinary research team from nursing, pharmacy, medicine, and administration, we therefore recognize several compelling reasons to explore the potential benefits of restoration science for healthcare research, management, and practice. Firstly, health care and restoration are both complicated, labor intensive, healing endeavors where teams of practitioners, managers, and scientists collaborate to achieve outcomes that are ethically, scientifically, and economically sound for unpredictable, technologically complex worlds.22,33,34,35 Secondly, healthcare leaders are searching for adaptive management strategies to navigate the risks of modern healthcare environments in the face of multiple uncertainties and paradoxical constraints.20,36,37 Thirdly, in an era of ongoing cost constraints, the science of restoration offers us alternative ways to think about achieving lasting efficiencies in a sustainable way. Fourthly, the communal nature of restoration projects means that we simultaneously work together on the ecological and cultural integrity of the places we share.38 Finally, various forms of ecological thinking are gaining ground in health services and patient safety research.16,36,39,40,41 For all of these reasons, we believe that we can adapt restoration knowledge to study and strengthen vital safety structures, processes, practices, and relations in modern healthcare environments. In short, we hope to use restoration science to build safer systems by creating safer places in which to give and receive care.
Methods
Developing a medication safety intervention by ecological design
We used an exploratory research design that included photographic and quantitative survey methods to apply the principles and techniques of restoration science to the study of medication safety issues identified by practitioners and managers of an acute inpatient medical ward. With the review and approval of the health research ethics board of the University of Alberta, Edmonton, a volunteer convenience sample of 26 full and regular part time registered nurses (RNs) and licensed practical nurses (LPNs) was used to conduct our study on an acute medical ward which serves older vulnerable patients with frequent co‐morbidities. In keeping with the participatory character of restoration science (box 1), we met with clinical staff and leaders to discuss historical and daily practices, medication administration processes, and the physical and cultural environment for medication administration. After developing a list of medication safety problems with ward staff, digital photographs were taken of all the environmental safety concerns and the images were entered into a computerized digital image catalogue. In subsequent design sessions, techniques of photo elicitation42 were used with the same groups of practitioners to draw out further commentary on the original problem list as we reviewed the digital images together. At the suggestion of participating practitioners, we observed and mapped ward medication administration processes and incorporated the process map along with existing research39,43,44,45,46,47,48,49,50,51,52,53 into the collaborative design of a medication safety inventory (MSI) of agreed upon medication safety issues. After initial testing of the face and content validity of potential items with 40 practitioners and managers attending two medication safety workshops in another health region, a revised set of items were reviewed with seven clinical nurse educators in the hospital's medical program. The format and wording of the pilot inventory were then finalized.
Box 1 Using restoration science: steps in an ecological research design
Create an initial list of medication safety problems with researchers, clinical staff, and leaders through discussion of historical and daily practices, medication administration processes, and the physical and cultural environment for medication administration.
Collect baseline digital photographs of all the environmental safety concerns identified on the initial problem list and enter the photographs into a digital image catalogue (DIC).
Conduct focus groups with staff to elicit further ideas about the initial problem list while viewing the digital photographs together.
Create an expanded problem list of medication safety issues based on practitioner feedback.
Observe and map the ward medication administration process.
Review and incorporate existing medication safety research evidence into the collaborative construction of a medication safety inventory (MSI) of medication safety issues.
Distribute the MSI to all ward RNs and LPNs for anonymous voluntary completion.
Analyze the MSI responses and use thematic analysis of focus group comments to identify priority areas for safety improvement.
Share aggregate MSI findings and digital photographs with staff in order to validate the interpretation of the data and identify priority system and ward improvements.
Work with ward staff and unit manager to use the research findings to design and implement interventions to improve medication safety (table 2).
Enable ward leaders and staff to conduct ongoing monitoring and self‐correction through (1) regular re‐administration of the MSI; (2) regular collection of repeat photographs to update the DIC; and (3) regular review of updated MSIs and updated DICs in staff meetings.
Before administering the inventory, the research team completed and logged a comprehensive series of digital photographs to document all the environmental medication safety issues that had been identified during the design phase. The four‐part inventory was then distributed to all ward RNs and LPNs for anonymous voluntary completion. Part 1 provided a series of definitions related to medication safety such as “near miss”, “medication error”, and “adverse drug event”; part 2 was a series of statements about medication safety using a 5 point Likert scale for response; part 3 was a series of ranking questions where staff could prioritize areas for improvement; and part 4 provided a place for participants to comment on medication safety as desired. Nursing staff had 1 month to complete and return the inventory to research staff in a stamped self‐addressed envelope.
Analysis of data
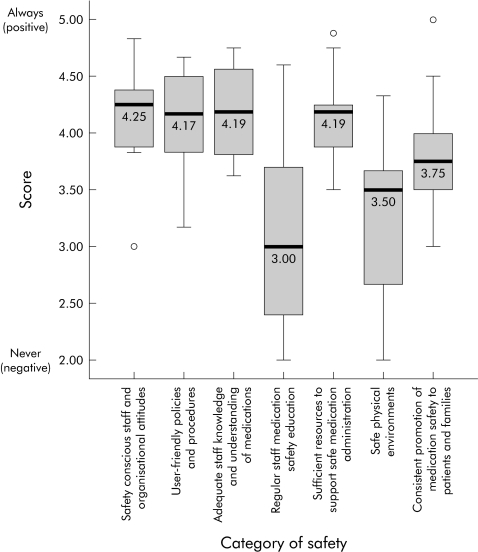
To analyze the inventory responses, we calculated descriptive statistics for all of Likert scale items. In part 3 of the inventory, where respondents were asked to rate a number of items in order of importance for strengthening medication safety on the ward, the median rank and interquartile range for each item was calculated and then reported as a summarized ranking. Based on thematic analysis of the focus group comments and the written responses to part 4 of the inventory, the medication safety attributes of the ward were grouped into seven categories: (1) safety conscious staff and organizational attitudes; (2) user friendly policies and procedures; (3) adequate staff knowledge and understanding of medications; (4) regular staff medication safety education; (5) sufficient resources to support safe medication administration; (6) safe physical environment; and (7) consistent promotion of medication safety to patients and families. The Likert scale items were then grouped and assigned to one of the seven medication safety categories and composite median and interquartile scores were calculated. The research team then shared the findings with ward staff in conjunction with a second review of the digital photographs in order to validate the interpretation of the data and elicit any additional comments.
Results
Early findings from research and restoration
As an introductory attempt to apply restoration science to patient safety research, we worked within several limitations. We depended on the participation of a self‐volunteering ward and the use of a self‐report survey, and we administered the inventory to ward nurses only rather than to all members of the patient care team. While the majority of staff (20/26) participated in focus groups with the ward manager and clinical educator, only 12 of the 26 nurses (46%) returned completed MSIs after both leaders were seconded to open a second ward for overflow medical patients. Despite these constraints, we learned a great deal about local and system medication safety issues and the use of an ecological research design. For instance, in the design phase of our research, the ward staff's review of the initial set of digital photographs in focus groups stimulated in‐depth discussion of several medication safety issues. Focus group feedback from staff centered on perceived deficits in daily practice and concerns about the physical environment. Staff also indicated that, although they felt supported to report medication incidents that occurred, they wanted better coaching to prevent errors and learn from near misses. In addition, most also wanted more consistent debriefing after actual errors and more education about a variety of older and new medications. Environmental issues such as cluttered counter space, look‐alike medications, an overcrowded narcotics cupboard, and a disorganized medication room were also identified.
When the Likert scale items on the inventory responses were analyzed, the scores for safety conscious staff and organizational attitudes, user friendly policies and procedures, adequate staff knowledge and understanding of medications, and sufficient resources to support safe medication administration were positive, all scoring above 4.00 (fig 1). Nurses felt that information about medication information and troubleshooting was easy to find most of the time, and that other health professionals were usually available for consultation as required. Median scores for consistent promotion of medication safety to patients (3.75), regular staff medication safety education (3.00), and the safety of the ward environment (3.50) were identified as key areas of concern. Responses indicated that staff usually discussed medication safety reactively rather than proactively, and did not consistently alert each other about the type of medication orders most associated with medication error. In addition, while staff reported sporadic learning from near misses, medication errors, and adverse drug events, they also indicated that they did not consistently learn about medication safety through any ongoing reliable forums. Interestingly, respondents rated their own knowledge for managing near misses or medication errors as higher than that of their co‐workers.
Figure 1 Boxplot of pilot ward medication safety inventory scores. Bold line = median score; bottom of box = first quartile (Q1); top of box = third quartile (Q3); lines = 1.5 × interquartile range (IQR) = Q3 − Q1; open circles = outliers.
When the research team presented a complete catalogue of digital photographs along with a report of the inventory findings to the staff, practitioners identified additional system factors requiring modification such as stock list revisions, delivery schedules, and other “taken for granted” practices. Several staff also suggested the need for a user friendly reporting process to encourage consistent reporting of near misses. Based on these findings, the ward has progressed with its own efforts to implement and evaluate ongoing monitoring of medication administration safety. In effect, the participatory photographic research techniques enabled practitioners to actively create and debate photo novellas or meaningful narratives of their experience and knowledge of the issues under study.54 With the support of the ward manager and clinical educator, the nurses have formed a “coaching and clean up crew” to address education concerns and redesign and strengthen the physical environment for medication administration (table 2).
Table 2 Ward improvements to date.
| Improvements to date | • Clean up of the narcotics cupboard, reducing quantities of seldom used narcotics and eliminating unused narcotics (fig 2) |
| • New charting procedures and protocols | |
| • Reorganization of hard log‐off for all narcotics | |
| • Enhanced medication administration component of nursing orientation | |
| • Decluttering and rearranging the medication room | |
| • Institution of near miss reporting and debriefing practices | |
| Improvements in progress | • Needs assessment to determine priority areas for staff medication administration education |
| • “Ecological tour” of other wards to generate ideas for further reorganization options | |
| • Adjustment of pharmacy delivery schedule and process | |
| • Working with pharmacy to transfer responsibility for stocking observation room | |
| Wish list | • Physical redesign of the medication administration area in the observation room |
| • Larger medication cups |
In ranking the items on the inventory, several opportunities were identified to address human factors that contribute to error. Specifically, the highest ranked priorities for strengthening patient safety included improving communication about new medications, policies, equipment, and developments in patients' treatment orders (8/12); improving the accuracy and completeness of transcribing medication orders (6/12); improving the storage of medications (6/12); and improving the visibility and accessibility of clear procedures for medication administration (6/12). Figure 2 shows the improvements which the pharmacist and nursing staff made to a cluttered narcotic cupboard by removing unused or seldom used narcotics and increasing the delivery schedule of frequently used medications. For example, the pre‐intervention cupboard housed three strengths of injectable demerol, two strengths of morphine, and two strengths of hydromorphone. Consistent with current recommendations from the Institute of Safe Medication Practices, the ward used the project findings to reduce the opportunity for selection error by storing a single strength of each of these medications in the narcotic cupboard.
Figure 2 Digital photographs of the narcotics cupboard (A) before the medication safety intervention and (B) following ward selected changes.
The observable power of the ward images to engage practitioners in critical re‐examination and repair of their environment is consistent with recent findings in restoration research. As Higgs notes, the collective review of environmental photographs in conjunction with significant historical and ecological data can help local citizens to first re‐imagine and subsequently “re‐story” the communities they inhabit into places that are more culturally and ecologically sound.26 In Higgs' view, this heightened “place sense” that restorationists seek to develop with local citizens is fundamental to the implementation of good lasting restorations.26,27 In essence, he argues, we can use our discussions of the images to create a narrative continuity about the places we share that encourages us to question more thoughtfully: “How is this story best continued into the future? What guidance does the past provide?” (page 146).26 For example, local citizens and research teams used the collection and study of repeat photographs in Canada's Rocky Mountains to develop historical narratives of the landscape that inform present day efforts to repair and strengthen the ecological and cultural integrity of Jasper National Park and its communities.26,31
Other outcomes of our work suggest that ecologically designed interventions may contribute to the growth of a healthy safety reporting culture. For the 6 months prior to initiating the research, 26 medication incident reports were submitted, none of which were near misses. During the period of the project nine near misses were reported, and in the 6 months following the intervention 59 medication incident reports were submitted. Nursing staff now ask for more coaching and debriefing around near misses and errors, and daily communication about medication safety issues among ward staff and leaders has increased. In addition, the healthcare team is more aware of the degree and range of unnecessary interruptions to nurses as they prepare and administer medications, and several staff members who refrained from active roles in past ward initiatives are leading the activities of the ward crew. Concurrently, we incorporated the frontline “error wisdom”6 which we generated with practitioners during this project into a revised MSI (see Appendix A available online at http://www.qshc.com/supplemental) for future use in related research.
Discussion
In this initial project we broke new ground to adapt the ethics, science and practice of ecological restoration to the conduct of patient safety research. Working as an interdisciplinary research team, we used restoration thinking and participatory photographic techniques to discover and incorporate what clinicians know about their local environments to strengthen the ward's safety culture, medication safety practices, and medication delivery systems design.54,55 In keeping with the principles of research based practice and good restoration, practitioners used methods of repeat photography, photo elicitation, and photo novella to creatively question the safety of their surroundings and implement several inexpensive or cost neutral repairs. Practitioners' increased use of self‐regulation through ward reporting mechanisms to learn about medication safety is evident, and the digital photography that supported the redesign process now forms an integral component of a viable monitoring program.
Key messages
The principles of good ecological restoration can be used to study today's complex health systems and to strengthen the safety of the places where care is provided.
Ecological research designs support the use of mixed methods and multifaceted interventions. For example, we successfully adapted several techniques from restoration science such as citizen forums (focus groups), repeat photography, and mapping the terrain (medication process mapping) to research and monitor the safety of a modern healthcare environment.
Good restoration fosters the development of safer practice communities by encouraging the interdisciplinary work of collaborative self‐monitoring healthcare teams.
As Berwick56 and others20,21 urge us to broaden our scientific curiosity about an array of theoretically grounded approaches to quality and safety research, this initial project suggests that we can learn from all forms of healing work. Across the fields of health care, ethics, ecosystems management and restoration, there is a growing call to deepen our imagination about what is scientifically valid, economically viable, and ethically sustainable in a complex technological world.24,26,27,28,29,30,35,55,57,58,59 The conduct of good restoration asks us to integrate good systems thinking with better capacity to “think like a system”16,60 in order to constructively re‐imagine and re‐story our approach to the study and management of today's healthcare systems. Based on these early findings, we will conduct further research to refine our photographic research methods and test a revised version of our multifaceted medication safety intervention in further research. Our goal is to build and sustain safer systems with the best patient safety interventions that our healthcare organizations can afford.
The revised medication safety inventory is shown in Appendix A available online at http://www.qshc.com/supplemental
Supplementary Material
Acknowledgements
The authors thank Dr Edwards' 2006 research internship class and the QSHC reviewers for their critiques of this paper.
Abbreviations
DIC - digital image catalogue
LPN - licensed practical nurse
MSI - medication safety inventory
RN - registered nurse
Footnotes
Portions of this work were supported by the Faculty of Nursing, University of Alberta; the Royal Alexandra Hospital Clinical Research Unit, Capital Health; the Canadian Nurses Foundation Nursing Care Partnership Program; Dr J Lander's Canadian Health Services Research Foundation Chair for Better Care Summer Studentship Program; the Alberta Heritage Foundation for Medical Research Summer Studentship Program; and Dr Nancy Edwards' Canadian Institutes for Health Research/Canadian Health Services Research Foundation Nursing Chair (Multiple Interventions for Community Health Nursing) at the University of Ottawa. Dr Majumdar is a Population Health Investigator of the Alberta Heritage Foundation for Medical Research and a New Investigator of the Canadian Institutes of Health Research.
The authors have no competing interests to declare.
The revised medication safety inventory is shown in Appendix A available online at http://www.qshc.com/supplemental
References
- 1.Brennan T A, Leape L L, Laird N M.et al Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991324370–376. [DOI] [PubMed] [Google Scholar]
- 2.Wilson R M, Runciman W B, Gibberd R W.et al Quality in Australian Health Care Study. Med J Aust 1996164754. [DOI] [PubMed] [Google Scholar]
- 3.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001322517–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker G R, Norton P G, Flintoft V.et al The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. Can Med Assoc J 20041701678–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forster A J, Clark H D, Menard A.et al Adverse events among medical patients after discharge from hospital. Can Med Assoc J 2004170345–349. [PMC free article] [PubMed] [Google Scholar]
- 6.Reason J. Beyond the organizational accident: the need for error wisdom on the frontline. Qual Saf Health Care 20041328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Steering Committee on Patient Safety Building a safer system: a national integrated strategy for improving patient safety in Canadian health care. Ottawa 2002
- 8.National Health Service An organization with a memory. Report of an Expert Working Group on Learning from Adverse Events in the NHS. London: Department of Health, 2000
- 9.Australian Council for S a f e t y, Quality in Health Care ( A C S Q H.Safety in practice: making health care safer. Sydney, Australia: ACSQHC, 2001
- 10.Leape L L, Berwick D M. Five years after to err is human: what have we learned? JAMA 20052932384–2390. [DOI] [PubMed] [Google Scholar]
- 11.Woolf S H. Patient safety is not enough: targeting quality improvements to optimize the health of the population. Ann Intern Med 200414033–36. [DOI] [PubMed] [Google Scholar]
- 12.White P, McGillis‐Hall L. Patient safety outcomes. In: Doran DM, ed. Nursing sensitive outcomes. Sudnumy, MA: Jones and Bartlett, 2003211–242.
- 13.Baker G R, Norton P G.Patient safety and healthcare error in the Canadian healthcare system – a systematic review and analysis of leading practices in Canada with reference to key initiatives elsewhere. Ottawa: Health Canada, 2002, Available at www.hc‐sc.gc.ca/english/care/report
- 14.Shojania K G, Duncan B W, McDonald K M.et al Safe but sound: patient safety meets evidence‐based medicine. JAMA 2002288508–513. [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality Making health care safer: a critical analysis of patient safety practices. Rockville, MD: Agency for Healthcare Research and Quality, 2001
- 16.Marck P B. Theorizing about systems: an ecological task for patient safety research. Clin Nurs Res. 2005;14: 103–8, (See also Revista Latina Americana Enfermagem 2005 for Portuguese translation). [DOI] [PubMed]
- 17.Majumdar S R, McAlister F A, Furberg C D. From knowledge to practice in chronic cardiovascular disease: a long and winding road. J Am Coll Cardiol 2004431738–1742. [DOI] [PubMed] [Google Scholar]
- 18.Bion J. F, Heffner JE. Challenges in the care of the acutely ill. Lancet 2004363970–977. [DOI] [PubMed] [Google Scholar]
- 19.Wears R L, Berg M. Computer technology and clinical work. Still waiting for Godot. JAMA 20052931261–1263. [DOI] [PubMed] [Google Scholar]
- 20.Amalberti R, Auroy Y, Berwick D.et al Five system barriers to achieving ultrasafe health care. Ann Intern Med 2005142756–765. [DOI] [PubMed] [Google Scholar]
- 21.Wears R L, Cook R I. The illusion of explanation. Acad Emerg Med 2004111064–1065. [DOI] [PubMed] [Google Scholar]
- 22.Marck P B. Ethics in hard places: the ecology of safer systems in modern health care. Health Ethics Today 2004142–5. [Google Scholar]
- 23.Marck P B. Ecological error management for ethical health care. In: Provincial Health Ethics Network Newsletter In Touch. Edmonton: Provincial Health Ethics Network, 200031–2. [Google Scholar]
- 24.Marck P B. Ethics for practitioners: an ecological framework. In: Storch J, Rodney P, Starzomski RT, eds. Toward a moral horizon: nursing ethics for leadership and practice. Toronto: Pearson Education Canada, 2004232–247.
- 25.Society for Ecological Restoration International Science and Policy Working Group The SER international primer on ecological restoration. Tucson: Society for Ecological Restoration International, 2004, Available at www.ser.org
- 26.Higgs E S.Nature by design: human agency, natural processes and ecological restoration. Boston, MA: MIT Press, 2003
- 27.Higgs E S. What is good ecological restoration? Conserv Biol 199711338–348. [Google Scholar]
- 28.Gunderson L, Holling C S.eds. Panarchy: understanding transformations in human and natural systems. Washington, DC: Island Press, 2002
- 29.Walker B, Carpenter S R, Anderies J M.et al Resilience management in social‐ecological systems: a working hypothesis for a participatory approach. Conservation Ecology 2002614 [Google Scholar]
- 30.Gunderson L H, Holling C S, Light S S.eds. Barriers and bridges to the renewal of ecosystems and institutions. New York: Columbia University Press, 1995
- 31.Higgs E.Rocky Mountain Repeat Photography Project. 2003. Available at http://bridgland.sunsite.ualberta.ca
- 32.Gilmour A, Walkerden G, Scandol J. Adaptive management of the water cycle on the urban fringe: three Australian case studies. Conservation Ecology 1999311 [Google Scholar]
- 33.Vitek W, Jackson W.Rooted in the land. Essays on community and place. New Haven, CT: Yale University Press, 1996
- 34.Mills S.Service of the wild. Restoring and reinhabiting damaged land. Boston, MA: Beacon Press, 1995
- 35.Wears R L. A different approach to safety in emergency medicine. Ann Emerg Med 200342334–336. [DOI] [PubMed] [Google Scholar]
- 36.Rasmussen J. The role of error in organizing behaviour. Ergonomcs 1990331185–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wears R L. High reliability organizations. Keep the celebrations short. Qual Saf Health Care 200514154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgs E S. A quantity of engaging work to be done: ecological restoration and morality in a technological culture. Restoration and Management Notes 1991997–103. [Google Scholar]
- 39.Reason J, Hobbs A.Managing maintenance error. Aldershot: Ashgate, 2003
- 40.Gloubeman S. Walkerton water and complex adaptive systems. Hosp Q 2001428–31. [DOI] [PubMed] [Google Scholar]
- 41.Edwards N, Mill J, Kothari A R. Multiple intervention research programs in community health. Can J Nurs Res 20043640–54. [PubMed] [Google Scholar]
- 42.Harper D. Talking about pictures: a case for photo elicitation. Visual Studies 20021713–26. [Google Scholar]
- 43.Institute for Safe Medication Practices Medication safety self‐assessment tool. Canadian version. 2003. Available at www.ismp.org
- 44.Leape L L, Bates D W, Cullen D J.et al Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA 199527435–43. [PubMed] [Google Scholar]
- 45.Pape T M. Searching for the final answer: factors contributing to medication administration errors. J Cont Educ Nurs 200132152–160. [DOI] [PubMed] [Google Scholar]
- 46.Sexton J B, Helmreich R, Pronovost P J.et alThe safety climate survey. Boston, MA: Institute for Healthcare Improvement, 2003
- 47.Zuzelo P R, Inverso T, Linkewich K M. Content validation of the Medication Error Worksheet. Clin Nurs Spec 200115253–259. [DOI] [PubMed] [Google Scholar]
- 48.Piotrowski M M, Hinshaw D B. The safety checklist program: creating a culture of safety in intensive care units. Jt Comm J Qual Improv 200228306–315. [DOI] [PubMed] [Google Scholar]
- 49.Yamagishi M, Kanda K, Takemura Y. Methods developed to elucidate nursing related adverse events in Japan. J Nurs Manag 200311168–176. [DOI] [PubMed] [Google Scholar]
- 50.Pape T M. Applying airline safety practices to medication administration. Medsurg Nurs 20031277–94. [PubMed] [Google Scholar]
- 51.Hoffman S, Powell‐Cope G, MacClellan L.et al BedSAFE: a bed safety project for frail older adults. J Gerontol Nurs 20032934–42. [DOI] [PubMed] [Google Scholar]
- 52.Senholzi C, Fricker M P. Improving the quality of care: a regional medication safety effort. Pharmacy and Therapeutics 200227341–344. [Google Scholar]
- 53.Helmreich R L, Klinect J R, Wilhelm J A.et alThe Line/LOS error checklist, Version 6.0: A checklist for human factors skills assessment, a log for off‐normal events, and a worksheet for cockpit crew error management. Technical Report 99‐01 (crew resource management for aviation safety). Austin, TX: University of Texas Team Research Project, 1999
- 54.Lockett D, Willis A, Edwards N. Through senior's eyes: An exploratory qualitative study to identify environmental facilitators and barriers to walking. Can J Nurs Res 20053748–65. [PubMed] [Google Scholar]
- 55.Mills A E, Spencer E M, Werhane P H. eds. Developing organization ethics in healthcare: a case‐based approach to policy, practice, and compliance. Hagerstown, MD: University Publishing Group, 2001
- 56.Berwick D M. Broadening the view of evidence‐based medicine. Qual Saf Health Care 200514315–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Donnelley S. Nature as reality check. Hastings Center Report 19962621–28. [PubMed] [Google Scholar]
- 58.Johnson M.Moral imagination: implications of cognitive science for ethics. Chicago: The University of Chicago Press, 1993
- 59.Plsek P E, Greenhalgh T. Complexity science. The challenge of complexity in health care. BMJ 2001323625–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gunderson L, Folke C, Lee M.et al In memory of mavericks. Conservation Ecology 2002619 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.