Abstract
Objective
To assess whether patients' perceptions of a hypothetical medical error are influenced by staff responsiveness, disclosure of error, and health consequences of the error.
Design
Hypothetical scenario describing a medication error submitted by mail. Three factors were manipulated at random: rapid v slow staff responsiveness to error; disclosure v non‐disclosure of the error; and occurrence of serious v minor health consequences.
Participants
Patients discharged from hospital.
Measures
Assessment of care described in the scenario as bad or very bad, rating of care as unsafe, and intent to not recommend the hospital.
Results
Of 1274 participants who evaluated the scenario, 71.4% rated health care as bad or very bad, 60.2% rated healthcare conditions as unsafe, and 25.5% stated that they would not recommend the hospital. Rating health care as bad or very bad was associated with slow reaction to error (odds ratio (OR) 2.8, 95% CI 2.1 to 3.6), non‐disclosure of error (OR 2.0, 95% CI 1.5 to 2.6), and serious health consequences (OR 3.4, 95% CI 2.6 to 4.5). Similar associations were observed for rating healthcare conditions as unsafe and the intent to not recommend the hospital. Younger patients were more sensitive to non‐disclosure than older patients.
Conclusions
Former patients view medical errors less favorably when hospital staff react slowly, when the error is not disclosed to the patient, and when the patient suffers serious health consequences.
Keywords: patient perceptions, medical error, patient safety
The prevention and effective management of medical errors have become a priority for most healthcare systems.1,2,3,4,5,6 An appropriate response to medical errors must take into account patients' expectations. For instance, hospitals should respect most patients' wish that errors be openly disclosed.7,8,9,10,11,12
Several studies have explored people's opinions through experimentally manipulated hypothetical scenarios that describe a medical mishap. These studies have established that perceptions of the public are more negative when an error has severe health consequences,13,14,15 and when the error is not disclosed to the patient.14,15,16
Both adverse health outcome and non‐disclosure of the error concern the patient directly, so the importance of these variables for people's perceptions is not surprising. However, we do not know whether patients are sensitive to the responsiveness of healthcare staff once an error has occurred, in particular the prompt recognition and management of the error. This is an important issue since error management is under the control of the healthcare provider and can be improved.
In this study we used a hypothetical scenario of a medical error to test the effects of health consequences, disclosure of the error, and staff responsiveness to the error on the assessment of the incident by recently hospitalised patients.
Methods
Study design and sample
A cross sectional patient survey was conducted at Geneva University Hospitals, a public hospital system in Geneva, Switzerland. Participants were all adult Swiss residents discharged from the hospital between 15 September and 15 October 2002, identified through the administrative database. The survey package was sent to 2275 individuals 4–8 weeks after discharge. It included a cover letter, the self‐administered questionnaire, and a business reply envelope. Non‐respondents were sent a reminder postcard and two survey packages at 2–4 week intervals. During data collection we excluded patients who had moved away, died, were too sick to fill in the questionnaire, or did not speak French.
Questionnaire
The core of the questionnaire was the Picker patient experience survey17 which includes an item for the respondent's overall opinion of the care received at the hospital. We added items to explore the patient's feeling of security during the hospital stay (one item) and the occurrence of various undesirable events18 including two related to the use of medicines (allergic reaction to drug or wrong drug administered). Patients were also asked to record demographic parameters (age, sex, nationality, level of education) and their current health (two items from the SF‐36 questionnaire: general health, and feeling downhearted and blue during the last 4 weeks).19
The questionnaire also explored patients' opinions about identification wrist bands20 and included a scenario about a hypothetical medical error. There were 83 items in total.
Medical error scenario
The survey included a hypothetical scenario describing a medication overdose (table 1). This type of incident was chosen because drug administration errors are a leading cause of adverse events in inpatients.21,22 Three experimental factors were studied:
Table 1 Scenario.
| Best case scenario | Worst case scenario |
|---|---|
| Mr C is admitted to the hospital to receive an intravenous treatment. He receives the treatment in his room. Unfortunately Mr C does not tolerate the treatment well: he starts sweating and feels nauseous.He calls the nurse who arrives quickly. Noting the state of the patient, the nurse stops the intravenous line immediately and quickly informs the doctor who realises that Mr C received an overdose of the drug by mistake. The patient is immediately transferred to the intensive care unit (ICU) to be watched closely and to receive treatment to remove the drug.The doctor takes time to explain the situation to Mr C. He admits that an error was made and apologises to the patient. He also tells him that the hospital will take all necessary measures to ensure that such an incident does not occur again.Mr C's stay in the ICU is uneventful. He leaves the ICU after 2 days, resumes his initial treatment as planned, and leaves the hospital without further health problems. | Mr C is admitted to the hospital to receive an intravenous treatment. He receives the treatment in his room. Unfortunately Mr C does not tolerate the treatment well: he starts sweating and feels nauseous.He calls the nurse but nobody answers. He has to call several times before a nurse arrives.The nurse who comes is filling in for a colleague and does not know the treatment in progress. She spends time searching through the patient's file. The patient insists and she rings the doctor on call who also arrives late. Noting the state of the patient, the doctor then realises that Mr C received an overdose of the drug by mistake. Only several hours after his initial faintness is Mr C transferred to the ICU to be watched closely and to receive a treatment to remove the drug.Neither the doctor nor the nurse mention the error made to Mr C. The implication is that this was an unforeseeable complication.However, Mr C's kidneys were seriously damaged in spite of the treatment given in the ICU. Furthermore, he now cannot be treated as initially planned. He will have to be treated with a less effective drug. |
staff responsiveness to error (ineffective and slow v effective and fast);
disclosure of the error (non‐disclosure v full disclosure and apology); and
consequences for the patient (serious v minor).
Eight versions of the scenario were produced using a factorial design. Each participant received one randomly selected version of the scenario. Respondents were asked the following questions:
How would you rate the health care received by Mr C? (Very bad/Bad/Fair/Good/Very good).
Do you think that Mr C was treated in safe conditions? (Yes, completely/Yes, to some extent/No).
Imagine you were in this patient's place. Would you recommend this hospital to people close to you? (Yes, definitely/Yes, probably/No).
Initial versions of these questions and of the scenarios were pre‐tested with 42 volunteer inpatients in order to ensure that they were easily understood.
Analysis of data
Dependent variables were the proportions of respondents who rated the care received by the patient in the scenario as Bad or Very bad (versus Fair, Good, or Very good), who thought that the patient had not been treated in safe conditions (No or Yes, to some extent versus Yes, completely), and who would not recommend the hospital where the error occurred (No or Yes, probably versus Yes, definitely).
We examined associations between each of the three experimental factors and the three dependent variables using cross‐tabulations and χ2 tests. Logistic regression was used to model the mutually adjusted effects of the experimental factors on each outcome variable. For dichotomous outcome y1 and experimental factors x1, x2 and x3, the equation was:
 |
The results were expressed as odds ratios (OR = eb). We then tested first order interactions between experimental factors for each outcome variable. In this analysis we examined whether the effect on one experimental factor was the same across levels of another experimental factor. The logistic regression equation for testing an interaction between x1 and x2 was:
 |
The coefficient b4 corresponds to the interaction between the two experimental factors. Finally, we repeated the analysis of main effects across strata of previously defined respondent characteristics (table 2). Here too we tested whether the effect of an experimental factor was stable across respondent characteristics by means of interaction terms. For instance, to see if the effect of experimental factor x1 was related to age (grouped in three age groups coded as age3 = 0, 1, 2), we tested the following model:
Table 2 Personal and hospital stay characteristics of 1274 former patients of Geneva University Hospitals.
| Characteristics of respondents | N (%) |
|---|---|
| Sex | |
| Male | 565 (44.3) |
| Female | 709 (55.7) |
| Age (years) | |
| 18–44 | 478 (37.5) |
| 45–64 | 354 (27.8) |
| 65+ | 442 (34.7) |
| Nationality | |
| Swiss | 853 (67.0) |
| Others countries | 421 (33.0) |
| Level of education | |
| Higher (university) | 369 (29.7) |
| Medium and basic | 873 (70.3) |
| Current health status | |
| Excellent/Very good | 352 (28.6) |
| Good/Fair/Poor | 880 (71.1) |
| Felt downhearted and blue in past 4 weeks | |
| All of the time/Most of the time/Some of the time | 653 (52.2) |
| A little of the time/None of the time | 597 (47.8) |
| Length of stay (days) | |
| 2–10 | 905 (71.0) |
| >10 | 369 (29.0) |
| Personal experience of adverse events related to medication | |
| Yes | 94 (7.4) |
| No | 1028 (80.7) |
| Missing | 152 (11.9) |
| Rating of quality of care based on own hospital stay experience | |
| Excellent/Very good | 770 (61.5) |
| Good/Fair/Poor | 482 (38.5) |
| Rating of care as safe based on own experience | |
| Yes, completely | 1003 (80.2) |
| Yes, partially/No | 248 (19.8) |
| Intention to recommend the hospital based on own experience | |
| Yes, completely | 914 (72.9) |
| Yes, probably/No | 339 (27.1) |
The regression coefficient b5 corresponds to a linear trend across age groups for the effect of experimental factor x1 on outcome y1. The significance level was p<0.05 for all analyses.
Results
Sample characteristics
Of the 2275 patients to whom the questionnaire was sent, 262 were classified as ineligible because they had died, had an invalid address, did not understand French, or were too sick to answer. Of 2013 eligible patients, 1411 (70.1%) returned the completed survey.
Among the 1411 respondents, 1274 (90.2%, and 63.3% of initial sample) answered at least one of the questions about the scenario. The 137 non‐respondents were older than the 1274 respondents (mean age 66 v 54 years, p<0.001) and had longer hospital stays (mean 18 v 11 days, p<0.001). Respondents had been discharged from the departments of medicine (n = 274), surgery (n = 393), neurosciences (n = 200), gynaecology‐obstetrics (n = 255), geriatrics (n = 75), and psychiatry (n = 71); six patients had missing information on this variable) and most were discharged to their home (n = 1203, 94.4%). Other characteristics are shown in table 2.
There were no differences between the eight groups of patients allocated to the different versions of the scenario in terms of sex, age, nationality, level of education, hospital department, or hospital length of stay (data not shown, available upon request).
Perceptions of the hypothetical medical error
Overall, 71.4% (n = 880 of 1232 patients) of the respondents considered that the care received by the hypothetical patient was bad or very bad, 60.2% (n = 749 of 1244) considered that the patient was treated in unsafe conditions, and 25.5% (n = 315 of 1235) would not recommend the hospital based on the scenario. The assessments of care varied considerably according to the version of the scenario (table 3). Only 34.0% of respondents assigned to the best case scenario considered that Mr C received bad or very bad care compared with 89.5% of those assigned to the worst case scenario.
Table 3 Proportion of respondents who gave negative assessments of the hypothetical scenario across the eight versions of the scenario.
| Version of questionnaire | Staff responsiveness to error | Disclosure of error | Consequences of error | N | Respondents' assessments of hypothetical scenario | ||
|---|---|---|---|---|---|---|---|
| Care was bad or very bad (%) | Patient was treated in unsafe conditions (%) | Would not recommend the hospital (%) | |||||
| 1 | Rapid | Yes | Minor | 151 | 34.0 | 27.9 | 13.1 |
| 2 | Rapid | No | Minor | 166 | 55.7 | 43.5 | 17.4 |
| 3 | Slow | Yes | Minor | 165 | 70.4 | 55.9 | 17.9 |
| 4 | Slow | No | Minor | 148 | 79.2 | 71.0 | 30.8 |
| 5 | Rapid | Yes | Serious | 162 | 71.8 | 58.8 | 18.6 |
| 6 | Rapid | No | Serious | 166 | 85.8 | 69.6 | 35.8 |
| 7 | Slow | Yes | Serious | 160 | 82.7 | 72.3 | 28.4 |
| 8 | Slow | No | Serious | 156 | 89.5 | 82.5 | 42.1 |
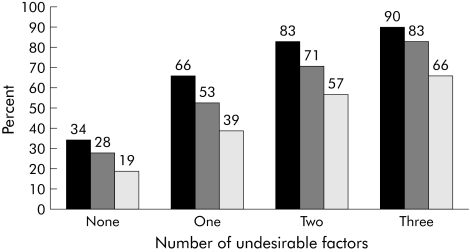
The effects of the three experimental factors (staff responsiveness to error, disclosure of error and consequences) on the assessments of the scenario were cumulative (fig 1). The more non‐desirable experimental factors were present, the more likely was a negative assessment of the scenario. Linear trends were statistically significant (p<0.001) for all three assessments.
Figure 1 Negative assessments of care described in a hypothetical scenario of a medical error. According to the number of undesirable factors included in the scenario (slow responsiveness to error, non‐disclosure of error, serious consequences). Percentage of respondents who rated the care as bad or very bad (black bars), who thought that the patient was treated in unsafe conditions (grey bars), and who would not recommend the hospital (white bars).
Each non‐desirable experimental factor doubled or tripled the odds that the respondents would consider the care received by the hypothetical patient as bad or very bad, that the patient was treated in unsafe conditions, and that they would not recommend the hospital if such an incident happened to them (table 4).
Table 4 Associations between experimental factors and former patients' assessments of hypothetical scenario.
| Experimental factors | Patient assessments of hypothetical scenario | ||
|---|---|---|---|
| Care was bad or very bad | Patient was treated in unsafe conditions | Would not recommend the hospital | |
| Slow responsiveness to error | 2.8 (2.1 to 3.6) | 2.5 (2.0 to 3.2) | 1.6 (1.2 to 2.1) |
| Non‐disclosure of error | 2.0 (1.5 to 2.6) | 1.8 (1.4 to 2.3) | 1.9 (1.5 to 2.5) |
| Serious consequences | 3.4 (2.6 to 4.5) | 2.6 (2.1 to 3.4) | 1.9 (1.4 to 2.5) |
Data are shown as odds ratios (95% confidence intervals).
Interactions
We tested all interaction terms between the experimental factors (staff responsiveness, disclosure, and health consequences) in relation to the three outcome variables. Of the nine interaction terms tested, two were statistically significant. The odds ratio for rating care as bad or very bad if staff were unresponsive was 3.8 (95% CI 2.7 to 5.4) when health consequences were minor compared with 1.7 (95% CI 1.1 to 2.6) when health consequences were serious (p for difference = 0.004). Likewise, the odds ratio for describing care as unsafe if staff were unresponsive was 3.2 (95% CI 2.3 to 4.5) when health consequences were minor but 1.9 (95% CI 1.4 to 2.7) when health consequences were serious (p for difference = 0.04).
Subgroup analysis
The effects of the experimental factors were similar among most subgroups of respondents. Odds ratios for rating the care received by the hypothetical patient as bad or very bad are shown in table 5. Results for the two other outcome variables were similar (not shown, available upon request). There were eight significant differences among 90 interaction tests. Only one difference was present consistently for all of the three outcome variables—the effect of non‐disclosure of the error was stronger among younger respondents than among older respondents. The odds ratio for rating care as bad or very bad associated with non‐disclosure was 3.7 for respondents aged 18–44 years, 2.1 for those aged 45–64 years, and 1.3 for those aged 65 years and older (table 5, p value for linear trend = 0.004). The odds ratios of perceiving care as unsafe associated with non‐disclosure were 2.8 (95% CI 1.8 to 4.4), 2.1 (95% CI 1.3 to 3.3), and 1.2 (95% CI 0.8 to 1.9) respectively in these age groups (p value for linear trend = 0.008). Similarly, the odds ratios of not recommending the hospital associated with non‐disclosure were 2.7 (95% CI 1.8 to 4.1), 2.5 (95% CI 1.5 to 4.3), and 1.1 (95% CI 0.7 to 1.9) in the younger, middle aged, and oldest patients (p value for linear trend = 0.02). The other five significant differences between subgroups were inconsistent across outcome variables (data not shown, available on request).
Table 5 Effects of experimental factors among subgroups on respondents' perception of care as bad or very bad.
| Subgroups of respondents | Odds ratio (95% CI) | |||
|---|---|---|---|---|
| Slow responsiveness to error | Non‐disclosure | Serious consequences | ||
| Sex | ||||
| Female | 2.6 (1.7 to 3.8) | 2.2 (1.5 to 3.3) | 3.6 (2.4 to 5.4) | |
| Male | 2.9 (2.0 to 4.4) | 1.9 (1.3 to 2.8) | 3.3 (2.3 to 4.9) | |
| Age (years) | ||||
| 18–44 | 3.8 (2.3 to 6.2) | 3.7 (2.2 to 6.1) | 4.5 (2.7 to 7.6) | |
| 45–64 | 1.9 (1.2 to 3.3) | 2.1 (1.3 to 3.5) | 2.8 (1.7 to 4.7) | |
| 65+ | 2.7 (1.8 to 4.3) | 1.3 (0.9 to 2.1) | 3.5 (2.2 to 5.3) | |
| Nationality | ||||
| Swiss | 3.3 (2.3 to 4.6) | 1.9 (1.4 to 2.7) | 4.2 (3.0 to 6.0) | |
| Not Swiss | 2.1 (1.3 to 3.2) | 2.2 (1.4 to 3.4) | 2.4 (1.6 to 3.8) | |
| Felt downhearted and blue | ||||
| All/Most/Some of the time | 2.9 (1.9 to 4.3) | 2.4 (1.6 to 3.6) | 3.6 (2.4 to 5.4) | |
| A little/None of the time | 2.7 (1.9 to 4.0) | 1.7 (1.2 to 2.4) | 3.4 (2.3 to 5.0) | |
| Level of education | ||||
| Higher (University) | 2.5 (1.9 to 3.5) | 1.9 (1.4 to 2.6) | 3.0 (2.2 to 4.1) | |
| Medium and basic | 4.0 (2.3 to 7.1) | 2.8 (1.6 to 4.8) | 5.8 (3.2 to 10.6) | |
| Current health status | ||||
| Excellent/Very good | 3.3 (1.9 to 5.6) | 3.4 (2.0 to 6.0) | 4.3 (2.5 to 7.3) | |
| Good/Fair/Poor | 2.8 (2.0 to 3.8) | 1.7 (1.2 to 2.4) | 3.3 (2.4 to 4.6) | |
| Rating of quality of care based on own hospital stay experience | ||||
| Excellent/Very good | 2.5 (1.6 to 3.9) | 1.9 (1.2 to 2.9) | 2.8 (1.8 to 4.3) | |
| Good/Fair/Poor | 3.2 (2.3 to 4.6) | 2.1 (1.5 to 2.9) | 3.9 (2.8 to 5.7) | |
| Rating of care as safe based on own experience | ||||
| Yes, completely | 2.9 (2.2 to 4.0) | 2.0 (1.5 to 2.8) | 3.7 (2.7 to 5.0) | |
| Yes, partially/No | 2.7 (1.4 to 5.1) | 1.8 (0.9 to 3.2) | 2.3 (1.3 to 4.4) | |
| Intention to recommend the hospital based on own experience | ||||
| Yes, definitely | 2.9 (2.2 to 4.1) | 1.9 (1.4 to 2.6) | 3.3 (2.4 to 4.6) | |
| Yes, probably/No | 2.5 (1.5 to 4.4) | 2.2 (1.3 to 3.8) | 3.8 (2.1 to 6.8) | |
| Personal experience of drug related adverse events | ||||
| Yes | 1.4 (0.5 to 3.8) | 4.5 (1.6 to 13.1) | 3.5 (1.3 to 9.6) | |
| No | 2.9 (2.2 to 3.9) | 1.9 (1.4 to 2.5) | 3.4 (2.5 to 4.5) | |
Discussion
Using an experimentally manipulated hypothetical scenario of a medication error, we found that inadequate staff responsiveness in the face of the error, non‐disclosure of the error to the patient, and serious health consequences for the patient have a negative influence on respondents' evaluation of the incident. Accumulation of these factors increased respondents' tendency to evaluate negatively the care received, to rate healthcare conditions as unsafe, and to not recommend the hospital to others. Stratified analyses showed that the reactions to the medical error were similar across subgroups of respondents, with the exception of the effect of non‐disclosure of the error which was stronger for younger than for older respondents.
Disclosure of errors
Like others, we found that patients perceive negatively the non‐disclosure of errors.7,8,9,10,11,12,14,15,16 That patients should wish healthcare providers to admit to errors and apologise for them reflects basic human decency. However, in the real world and unlike in our scenario, a patient to whom the error was not disclosed may never know that it occurred and may therefore keep a favourable opinion of the healthcare provider.
While open disclosure of errors to patients is the currently recommended standard,23,24 only limited empirical evidence exists about the impact of such a policy on malpractice litigation and relationships between doctors and patients. One study has suggested that a policy of open disclosure does not increase malpractice claims,25 and another revealed that lack of openness may be in itself a motivation for lawsuits.26 A survey of hospital managers in the United States shows that disclosure of errors to patients is increasing, but also that fear of malpractice remains the main barrier to disclosure.27 Errors that lead to the most serious injuries are most likely to be disclosed to patients.28
In our scenario we grouped the disclosure of the error with a commitment for improvement on the part of the hospital. We cannot therefore disentangle the impact of these two messages on patient perceptions. Future studies should model and analyse these components separately.
Health outcome
We also replicated previous findings that health outcomes influence people's perceptions. Pairs of scenarios describing the same error were rated differently, depending on the seriousness of the health outcome. While this result has been reported by others,13,14,15,16 it is debatable whether it reflects fair judgement on the part of the patients. After all, the healthcare provider behaved identically in both situations. This observation can be considered as an example of hindsight bias due to the human tendency to overestimate causality:1,29 if the outcome is bad, the error must be bad too. Previous research indicates that doctors30 and court experts31 are also prone to this bias.
Handling of errors
A novel finding was that slow and ineffective handling of the error by healthcare staff resulted in a more negative perception by patients. This was true whether the error was disclosed or not, and whether health consequences were minor or severe. Patients' assessments are therefore sensitive to the process of error management and not only to the consequences of the incident for themselves. This suggests that hospitals may improve or maintain trust by informing the public about their policies and procedures for dealing with errors—both the immediate reactions to an error that aim to minimise patient harm and the organisational learning processes that aim to make the system of care safer. The latter recommendation is somewhat speculative as our scenario tested only the immediate reaction to error.
Subgroups and interactions
Generally, the experimental factors we tested had similar effects on the judgements of various subgroups of patients. In particular, these effects were not stronger among patients who reported a personal experience of a problem related to the administration of a drug, which was the mishap described in the scenario. This suggests that the set of values used for judgements of medical errors is shared by most patients and is not very sensitive to recent personal experience. There was one exception: the effect of non‐disclosure of the error was stronger among younger people than among older respondents for all three outcome variables. Older patients may be used to a more secretive and paternalistic practice of medicine, and may be less disturbed by non‐disclosure than younger generations. Other research suggests that younger patients want more involvement in medical decisions.32
While all three experimental factors had strong independent and cumulative effects on patient evaluations of care, we found a statistical interaction between staff responsiveness and health consequences: the negative impact of slow responsiveness was more pronounced when health consequences were described as minor than when they were serious. This suggests that a “ceiling effect” may affect respondents' unfavourable assessments of care—the first undesirable event affects patient perceptions the most negatively, the second a little less, etc. It should be noted that the interpretation of statistical interactions depends on the type of risk model applied to the data.33 We used a multiplicative model which assumes that, when two risk factors are present, their odds ratios will multiply each other. This model assumption may or may not be reasonable when applied to real life data.
Methodological issues
The main limitation of the study is that respondents did not react to a real life situation but rated a hypothetical scenario. Whether they would have responded similarly if the medical error had happened to them personally is uncertain. While vignettes have been used successfully in health and social research, they may yield unreliable results when they neglect important social or environmental cues that occur in real life, or when they describe experiences that are unfamiliar.34 But even if scenarios do not reflect exactly the real world, they help clarify the judgement principles employed in the real world.31 Furthermore, the psychological distance vignettes afford between the situation being described and the rater may be an advantage when threatening or emotionally stressful situations are explored.10,34 In such cases, direct questioning of protagonists may be either difficult or unethical.10 Medical errors may fall in this category.
We surveyed recently hospitalised patients while previous studies have surveyed the general public,13 health insurance plan members,14 outpatients,16 or an internet panel.15 Recently hospitalised people can probably easily imagine being in the situation portrayed in the scenario, and results obtained through hypothetical vignettes are more credible if the vignette describes a familiar situation.34
Another limitation is that we tested only one type of medical error. It is possible that patients would react differently to other types of error. However, studies that used hypothetical scenarios based on different types of medical errors did not show meaningful differences.14,15
The response rate of the survey was acceptable, and an analysis of a similar patient survey at our hospital has shown that selection bias was modest, at least with regard to the Picker patient opinion survey.35 We therefore believe that the results reported here are internally valid. However, as with any local study, our results may not be applicable to other contexts.
In conclusion, all three experimental variables—handling of the error by hospital staff, disclosure of the error to the patient, and severity of health consequences—influenced patients' perceptions of the healthcare incident.
Footnotes
Funded by the Quality of Care Program of University Hospitals of Geneva. There was no external funding.
Competing interests: none.
Part of this paper was presented at the 25th Annual Meeting of the Society for Medical Decision Making, Chicago, USA, October 2003.
AC and AV contributed equally to this article.
Ethics review: As a quality improvement project that entailed minimal risk to participants, the Hospital Research Ethics Committee exempted the survey from full formal review.
References
- 1.Leape L L. Error in medicine. JAMA 19942721851–1857. [PubMed] [Google Scholar]
- 2.Cole T. Medical errors vs medical injuries: physicians seek to prevent both. JAMA 20002842175–2177. [PubMed] [Google Scholar]
- 3.Wolff A M, Bourke J. Reducing medical errors: a practical guide. Med J Aust 2000173247–251. [DOI] [PubMed] [Google Scholar]
- 4.Bates D W, Gawande A A. Error in medicine: what have we learned? Ann Intern Med 2000132763–767. [DOI] [PubMed] [Google Scholar]
- 5.Robinson A R, Hohmann K B, Rifkin J I.et al Physician and public opinions on quality of health care and the problem of medical errors. Arch Intern Med 20021622186–2190. [DOI] [PubMed] [Google Scholar]
- 6.Blendon R J, Schoen C, Donelan K.et al Physicians' views on quality of care: a five‐country comparison. Health Aff (Millwood) 200120233–243. [DOI] [PubMed] [Google Scholar]
- 7.Vincent C, Young M, Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet 19943431609–1613. [DOI] [PubMed] [Google Scholar]
- 8.Hingorani M, Wong T, Vafidis G. Patients' and doctors' attitudes to amount of information given after unintended injury during treatment: cross sectional, questionnaire survey. BMJ 1999318640–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallagher T H, Waterman A D, Ebers A G.et al Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA 20032891001–1007. [DOI] [PubMed] [Google Scholar]
- 10.Mazor K M, Simon S R, Gurwitz J H. Communicating with patients about medical errors: a review of the literature. Arch Intern Med 20041641690–1697. [DOI] [PubMed] [Google Scholar]
- 11.Wu A W. Handling hospital errors: is disclosure the best defense? Ann Intern Med 1999131970–972. [DOI] [PubMed] [Google Scholar]
- 12.Cantor M D. Telling patients the truth: a systems approach to disclosing adverse events. Qual Saf Health Care 2002117–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blendon R J, DesRoches C M, Brodie M.et al Views of practicing physicians and the public on medical errors. N Engl J Med 20023471933–1940. [DOI] [PubMed] [Google Scholar]
- 14.Mazor K M, Simon S R, Yood R A.et al Health plan members' views about disclosure of medical errors. Ann Intern Med 2004140409–418. [DOI] [PubMed] [Google Scholar]
- 15.Schwappach D L, Koeck C M. What makes an error unacceptable? A factorial survey on the disclosure of medical errors. Int J Qual Health Care 200416317–326. [DOI] [PubMed] [Google Scholar]
- 16.Witman A B, Park D M, Hardin S B. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med 19961562565–2569. [PubMed] [Google Scholar]
- 17.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in‐patient surveys in five countries. Int J Qual Health Care 200214353–358. [DOI] [PubMed] [Google Scholar]
- 18.Agoritsas T, Bovier P, Perneger T V. Patient reports of undesirable events during hospitalization. J Gen Intern Med 200520922–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jenkinson C, Stewart‐Brown S, Petersen S.et al Assessment of the SF‐36 version 2 in the United Kingdom. J Epidemiol Community Health 19995346–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cleopas A, Kolly V, Bovier P A.et al Acceptability of identification bracelets for hospital inpatients. Qual Saf Health Care 200413344–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bates D W, Cullen D J, Laird N.et al Incidence of adverse drug events and potential adverse drug events. JAMA 199527429–34. [PubMed] [Google Scholar]
- 22.Runciman W B, Roughhead E E, Semple S J.et al Adverse drug events and medication errors in Australia. Int J Qual Health Care 200315(Suppl 1)i49–i59. [DOI] [PubMed] [Google Scholar]
- 23.Liang B A. A system of medical error disclosure. Qual Saf Health Care 20021164–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallagher T H, Levinson W. Disclosing harmful medical errors ro patients. A time for professional action. Arch Intern Med 20051651819–1824. [DOI] [PubMed] [Google Scholar]
- 25.Kraman S S, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999131963–967. [DOI] [PubMed] [Google Scholar]
- 26.Vincent C, Young M, Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet 19943431609–1613. [DOI] [PubMed] [Google Scholar]
- 27.Lamb R M, Studdert D M, Bohmer R M J.et al Hospital disclosure practices: results of a national survey. Health Aff 20032273–83. [DOI] [PubMed] [Google Scholar]
- 28.Weissman J S, Annas C L, Epstein A M.et al Error reporting and disclosure systems. Views from hospital leaders. JAMA 20052931359–1366. [DOI] [PubMed] [Google Scholar]
- 29.Tversky A, Kahneman D. Causal schemas in judgments under uncertainty. In: Kahneman D, Slovic P, Tversky A, eds. Judgment under uncertainty: heuristics and biases. Cambridge and New York: Cambridge University Press, 1982117–128.
- 30.Caplan R A, Posner K L, Cheney F W. Effect of outcome on physician judgments of appropriateness of care. JAMA 19912651957–1960. [PubMed] [Google Scholar]
- 31.Hugh T B, Tracy G D. Hindsight bias in medicolegal expert reports. Med J Aust 2002176277–278. [DOI] [PubMed] [Google Scholar]
- 32.Benbassat J, Pilpel D, Tidhar, M Patient's preferences for participation in clinical decision making: a review of published surveys. Behav Med 19982481–88. [DOI] [PubMed] [Google Scholar]
- 33.Perneger T V. Sex, smoking and cancer: a reappraisal. J Natl Cancer Inst 2001931600–1602. [DOI] [PubMed] [Google Scholar]
- 34.Hughes R. Considering the vignette technique and its application to a study of drug injecting and HIV risk and safer behavior. Sociol Health Illn 199820381–400. [Google Scholar]
- 35.Perneger T V, Chamot A, Bovier P A. Non‐response bias in a survey of patient perceptions of hospital care. Med Care 200543374–380. [DOI] [PubMed] [Google Scholar]