Abstract
Rather than continuing to try to measure the width and depths of the quality chasm, a legitimate question is how does one actually begin to close the quality chasm? One way to think about the problem is as a design challenge rather than as a quality improvement challenge. It is time to move from reactive measurement to a more proactive use of proven design methods, and to involve a number of professions outside health care so that we can design out system failure and design in quality of care. Is it possible to actually design in quality and design out failure? A three level conceptual framework design would use the six quality aims laid out in Crossing the quality chasm. The first or core level of the framework would be designing for patient centered care, with safety as the second level. The third design attributes would be efficiency, effectiveness, timeliness, and equity. Design methods and approaches are available that can be used for the design of healthcare organizations and facilities, learning systems to train and maintain competency of health professionals, clinical systems, clinical work, and information technology systems. In order to bring about major improvements in quality and safety, these design methods can and should be used to redesign healthcare delivery systems.
Keywords: patient safety, quality improvement, design, medical error
Rather than continuing to try to measure the width and depths of the quality chasm,1 a legitimate question to be asked is how does one actually begin to close the quality chasm? One way to think about the problem is as a design challenge more from an engineering and systems approach than as a healthcare quality improvement challenge. It is time to move from reactive measurement to a more proactive use of proven design methods, and to involve a number of professions outside health care so that we can design out system failure and design in quality of care.
The current healthcare delivery system is provider centric, with the primary focus operating at the convenience of the provider rather than the patient. As noted by the Institute of Medicine (IOM): “In the current system, control over decisions, access, and information is typically in the hands of care givers and is ceded to patients only when caregivers choose to do so…. A common practice today is that control over the times and location of care and the information needed to make such decisions resides with professionals.”1 This provider centric system of health care has resulted in a fractionated loosely coupled collection of services provided by separate clinical silos both within and between components of the system, with limited to no continuity and coordination of care for the patient. As pointed out by the Institute of Medicine in Crossing the quality chasm: “Health care has safety and quality problems because it relies on outmoded systems of work. Poor designs set the workforce up to fail, regardless of how hard they try. If we want safer, higher quality care, we will need to redesign systems of care…”.1
Some might argue that the concept of redesign is inappropriate because the current healthcare system was never designed in the first place, so the focus should be on design rather than (re)design. While the concept of design is integral to a number of professions—such as architecture, engineering, the arts, and education—with focuses on specific methods and formal training in design, the concept of design is generally lacking in health care. If design is taught at all, it is for research design rather than a formal discipline for the design of the healthcare system or any of its components.
Framework for system design
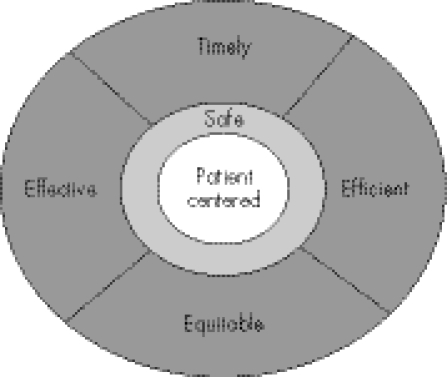
The IOM outlined the following six aims for redesigning healthcare systems in the 21st century—they should be safe, effective, patient centred, timely, efficient, and equitable.1 How can one organize an approach to achieve the design or redesign aims called for in Crossing the quality chasm?
A first step in safety and quality by design would be to take the six aims and place them in a slightly different order from that originally presented. The six aims can be divided into three levels or circles that govern or should govern the design process.
Level 1: design a patient centred healthcare system rather than the provider centric delivery approaches which currently influence health care. Placing the patient at the center serves as a fundamental design concept that shapes all other considerations in systems design. Clearly, a healthcare delivery system that is patient centric rather than provider centric might look quite different from what exists today.
Level 2: design a safe care system. “First do no harm” is the foundation of health care passed down from Hippocrates. Thus, safety becomes an immediate barrier surrounding the patient in the design of health care. The care delivery system must be resilient enough to prevent human errors or system failures to have an adverse impact on the patient. Health care cannot, like any other system, be completely error free or even be totally failure proof. However, the system can be robust enough to recover from human error and other system failures before they harm the patient. No other attribute of health care is of value if the patient is not safe at the center of the care system.
Level 3: design is a combination of the other four quality aims—effective, timely, efficient, and equitable. These four design aims constitute the third level of design and are equally important, but must be considered only after design aims 1 and 2 are fully addressed.
Figure 1 is an illustration of prioritization of the system design aims for the new health system of the 21st century. This model of quality can serve as a guide to system operation and outcome but, as Donabedian2 has taught us, the structure and process of health care ultimately influences the outcome of care.
Figure 1 Illustration of prioritization of system design aims for a new health system.
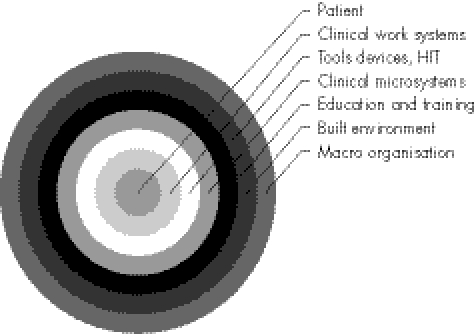
Battles and Lilford have provided a modification of the Donabedian model to serve patient safety which uses a nested approach of structure surrounding process with human behaviors at the core.3 The framework of structure and process can help determine what to design for the healthcare system.
Structure
Elements of structure that need to be considered for design include:
the organization of the healthcare macro system;
the educational system for health professions who are working or will be working in the organization; and
the physical structures within which care is delivered.
At the organization level there are both macro and micro levels that shape all other structure and process. At the macro level the nature of the organizational structure influences all other aspects of performance of the resulting system or subsystems.
Health care is one of the few industries in which the delivery of care is tightly coupled with the education of future caregivers. Thus, health professions education is an essential part of the structure which has a major impact on the quality and safety of care and therefore needs to be carefully designed.4 Fortunately, proven methods are available for the design of educational experiences or instruction.
The physical structure of the health system—referred to as the built or physical environment—interacts with both the organization and all of the processes of care that take place within the built environment.5 However, once the environment is built, our facilities have a lasting and pervasive influence on the quality and safety of the care provided to patients.
Process
Elements of process that need to be considered for design include:
the organization of clinical microsystems;
the tools and devices that shape and enhance the process of care; and
the clinical work systems involved in the process of care.
Today's health care is more often than not a loose collection of independent microsystems that have given health care a cottage industry approach.6 There has been a growing awareness that clinical microsystems are essential organizational units where clinical care is actually delivered to patients.7 Just as macro elements of the organization are a critical part of the structure, so are the ways the microsystem influence the process of care. It is therefore essential to consider the design of microsystems.
The delivery of health care has—and continues to be—dominated by human performance. The physicians, pharmacists, nurses, and other allied health professionals must be highly skilled knowledge workers. However, clinical work is increasingly being supported and shaped by technology in the form of tools, devices, and health information technology (HIT). Technology represents a range of sophistication from automated laboratory testing, pharmaceutical dispensing equipment, robotic surgery devices, to simple mistake proofing devices. There is a growing recognition that health care lags behind other major industries in the use of information technology. Major initiatives in both the US and the UK are intended to close that gap. But technology is in many ways a two‐edged sword, offering many benefits on the one hand and representing new safety and quality concerns on the other.8 The simple fact is that the tools of work are embedded in the process of care and are connected directly to the built environment. They must be designed in coordination with both the built environment and work itself. Automating broken work/clinical processes can, and often does, make matters worse rather than bringing promised improvements.
The process of care can also be thought of as a clinical work system. Clinical work is an interaction of teams of healthcare providers working in microsystems within a built environment using tools, devices, and HIT to care for the object of the system—the patient. The concept that work can be designed is not new. From pioneers like Frederick Taylor at the turn of the 20th century, the field of industrial engineering has proved that work and work systems can be designed.9 In health care there has been a reluctance to break from the mythology of the independent professional model of work to embrace the reality of interconnected clinical work systems.10 Clinical work can and should be designed for quality and safety.
Figure 2 is a graphic representation of the nested model of the critical elements of structure and process that must be designed. This model shares similar characteristics with Ferlie and Shortell's model of the healthcare system and with Moray's onion model of human factors design elements.11,12
Figure 2 Graphic representation of the nested model of the critical elements of structure and process required in a healthcare system.
Design disciplines and methods
While health care may not have a strong tradition in the area of design, other disciplines consider design as a core function. The articles in this supplement represent methods and approaches from authors from a variety of disciplines outside the traditional boundaries of the health professions. Each of these articles discusses approaches to quality and safety by design at the different levels illustrated in fig 2.
At the structure level, organizational sociology and management sciences have developed design methods and approaches that apply to healthcare organizations, particularly those striving to become high reliability organizations. At the macro organizational level, Carroll and Rudolph discuss approaches to be used for the design of high reliability organizations. Barach and Johnson explore design considerations at the microsystem level where much of health care is delivered.
The delivery of heath care and the training of health professionals are tightly coupled, with one influencing the other and vice versa.4 If one is to design in quality and eliminate safety problems by design, one must consider education and training as part of the overall design process. Henriksen and Dayton explore issues of design for training for quality and safety. Battles describes the process of instructional systems design (ISD) as a proven approach to improving the quality of education and training programs in the health professions. Galbraith and colleagues discuss the importance of assessment of health professions as a major influencing factor that can shape the quality and safety of care.
There is nothing more lasting than a physical structure that can shape the quality and safety of care than that of the built environment. Significant attention is now being paid to the built environment. Reiling describes the methods used at one institution in the Untied States to apply safety science to the design and construction of a new community hospital, and Senders discusses the complexity of design as it applies to multiple systems and system components.
The clinical work and work processes are key elements in the delivery of safe and quality care. The concept that clinical work and related processes can be designed is just beginning to be understood in health care. The authors in this section examine design methods and approaches to improve quality and safety of clinical work. Grout explores how mistake proofing can be incorporated into clinical processes to proactively prevent patient harm; Carayon and colleagues describe a method for work system design for patient safety emerging from industrial engineering; Karsh discusses human factors engineering paradigms for patient safety, exploring concepts of usability and performance support for healthcare works; and Amalberti and his colleagues review human performance and the management of violations and migrations from safe practice among healthcare professionals.
Key message
Rather than continually measuring the width and depth of the quality chasm, we need to design and build the bridge to span it.
Lowe describes methods for applying concepts of design as a vehicle for reducing harm that have been applied in the UK. Johnson deals with the issue of the proliferation of barely usable software applications which are disappointing in the results they obtain and actually cause more harm in the worst case scenarios. Finally, Runciman outlines an integrated framework for event reporting systems which can be used to monitor both design problems and successes over time.
Conclusion
The quality chasm can be crossed, but it will require more than measuring the width and depth of that chasm. We must design and build the bridge that crosses the chasm. We can and should design in quality and design out identifiable risks and hazards. Well established design methods and approaches are available from a number of disciplines that can be applied to healthcare quality and safety problems. We can be much more proactive in our responses through safety and quality by design.
Footnotes
Competing interests: none declared.
The opinions and assertions contained herein are the private views of the author and are not to be construed as official or as reflecting the views of the Agency for Healthcare Research and Quality, the United States, Department of Health and Human Services.
References
- 1.Corrigan J M, Donaldson M S, Kohn L T.et al eds. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press, 2001
- 2.Donabedian A.Explorations in quality assessment and monitoring: the definition of quality approaches to its assessment. Volume 1. Ann Arbor, MI: Health Administration Press, 1980
- 3.Battles J B, Lilford R J. Organizing patient safety research to identify risks and hazards. Qual Saf Health Care 200312(Suppl II)ii2–ii7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Battles J B, Shea C E. A system of analyzing medical errors to improve GME curricula and programs. Acad Med 200176125–139. [DOI] [PubMed] [Google Scholar]
- 5.Ulrich R, Zimring C.The role of the physical environment in the hospital of the 21st century: a once‐in‐a‐lifetime opportunity. Report to the Center for Health Design for the Designing for the 21st Century Hospital Project 20043
- 6.Reid P P, Compton D, Grossman J H.et al eds. Building a better delivery system: a new engineering/health care partnership. Washington, DC: National Academies Press, 2005 [PubMed]
- 7.Donaldson M S, Mohr J J.Improvement and innovation in health care microsystems. A Technical Report for the Institute of Medicine Committee on the Quality of Health Care in America. Princeton: Robert Wood Johnson Foundation, 2000
- 8.Battles J B, Keyes M A. Technology and patient safety: a two‐edged sword. Biomed Instrum Technol 20023684–88. [DOI] [PubMed] [Google Scholar]
- 9.Nadler G.Works systems design: the IDEALS concept. Homewood, IL: Richard D Davis, 1967
- 10.Reinersten J L. Health care past, present and future. 14th Annual Terry C Shackelford, MD Memorial Lecture. The Bulletin 19964061–70. [Google Scholar]
- 11.Ferlie E B, Shortell S M. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 200179281–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moray N. Error reduction as a system problem. In: Bogner MS, ed. Human error in medicine. Hillsdale, NJ: Lawrence Erlbaum, 199467–91.