Abstract
Introduction
A high number of emergency (999) calls are made for older people who fall, with many patients not subsequently conveyed to hospital. Ambulance crews do not generally have protocols or training to leave people at home, and systems for referral are rare. The quality and safety of current practice is explored in this study, in which for the first time, the short‐term outcomes of older people left at home by emergency ambulance crews after a fall are described. Results will inform the development of care for this population.
Methods
Emergency ambulance data in London were analysed for patterns of attendance and call outcomes in 2003–4. All older people who were attended by emergency ambulance staff after a fall in September and October 2003, within three London areas, were identified. Those who were not conveyed to hospital were followed up; healthcare contacts and deaths within the following 2 weeks were identified.
Results
During 2003–4, 8% of all 999 calls in London were for older people who had fallen (n = 60 064), with 40% not then conveyed to hospital. Of 2151 emergency calls attended in the study areas during September and October 2003, 534 were for people aged ⩾65 who had fallen. Of these, 194 (36.3%) were left at home. 86 (49%) people made healthcare contacts within the 2‐week follow‐up period, with 83 (47%) people calling 999 again at least once. There was an increased risk of death (standard mortality ratio 5.4) and of hospital admission (4.7) compared with the general population of the same age in London.
Comment
The rate of subsequent emergency healthcare contacts and increased risk of death and hospitalisation for older people who fall and who are left at home after a 999 call are alarming. Further research is needed to explore appropriate models for delivery of care for this vulnerable group.
Falls in older people occur as a result of a dynamic interaction between intrinsic and extrinsic factors. The health‐related costs of a fall are high. Reduction in quality of life and physical activity often lead to social isolation and functional deterioration, with a high risk of resultant dependency, institutionalisation and death.1,2 It has been estimated that the cost of falls accounts for 3% of the total National Health Service expenditure.3
Although most people who fall do not seek any medical advice,4,5 older people account for 12–21% of emergency department visits, and those who are taken to the emergency department after a fall are likely to fall again in the following year, with a 30% chance of sustaining a fracture or dislocation.6 Although prevention strategies have been shown to be effective,7 reduction of falls, injuries and associated morbidity are dependent on early identification of people at high risk and intervention delivered across traditional service boundaries.8 This is now reflected in current national and international guidelines.9,10,11
Ambulance services across the UK respond to about 300 000–400 000 emergency (999) calls for falls in older people per year.12 Previous studies have shown that up to half of these patients are attended by an emergency ambulance crew but are not taken to hospital.12,13 Ambulance staff do not generally have specific protocols or training to assess older people; nor do they have access to other services to support the patient at home. Non‐conveyance of emergency callers is recognised internationally as a safety and litigation risk.14 However, recent policy changes in the UK have encouraged the development of alternative models of care for delivery by the ambulance service, including enhanced training for paramedics and new community‐based referral pathways for patients who do not need to be taken to the emergency department.15,16
Although the high rate of emergency calls for falls in older people has been highlighted in the UK and internationally,14,17,18 outcomes for those left at home have not been reported previously. Uniquely, this study assessed the quality and safety of current practice by investigating the short‐term outcomes of older patients left at home by the ambulance service after a 999 call for a fall.
Methods
Routine data analysis
London Ambulance Service (LAS) data for emergency attendance and call outcomes (conveyance to hospital or non‐conveyance) were analysed for a 1‐year period, 2003–4, for all calls and for calls made for people aged ⩾65 whose incident was coded by the call‐taker as a “fall”. Descriptive statistics were produced for each primary care trust (PCT).
Outcome follow‐up
People aged ⩾65 years who were left at home after an emergency ambulance call, with an incident code of fall, and within the catchment areas of three London hospitals in September and October 2003, were identified from the same LAS data source. The routine ambulance records—patient report forms—completed by their attending crews were retrieved. Patients were contacted by post and offered the opportunity to opt out of the study. For those patients who did not opt out, healthcare contacts and deaths within 2 weeks of the index emergency ambulance call were identified as follows:
ambulance service reattendance from routine electronic records;
local emergency department attendance by searching for the patient's details on electronic databases; and
general practitioner attendance by contacting the patient's own general practitioner where details were available.
Deaths within 2 weeks were identified from coroners' records, which were also searched for patients' details. If the patient's details were not found in any of these data sources, it was assumed that he or she had not attended.
Ethical approval for the study was obtained from the Metropolitan Multi‐centre Research Ethics Committee and local research ethics committees.
Results
During 2003–4, the LAS attended 60 064 calls for people aged ⩾65 who had fallen, which was 8% of the total emergency workload. Of these 40% were not conveyed to hospital, varying widely between PCT areas, from 29.1% (Tower Hamlets: 275/944) to 52.0% (Hillingdon: 1137/2187).
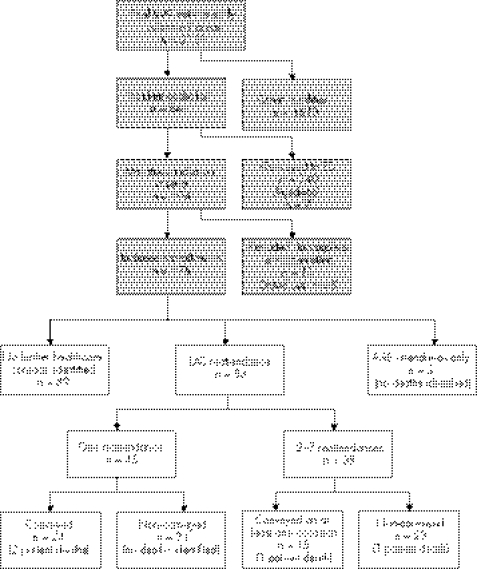
Of the 2151 emergency calls for people aged ⩾65 who were attended in the catchment areas of the three study hospitals during September and October 2003, a quarter (n = 534) were for people who had fallen. More than one third of these (n = 194) were left at home by their attending crew (fig 1).
Figure 1 999 calls received during the study period: number meeting inclusion criteria and outcomes. A&E, accident and emergency; ED, emergency department; LAS, London Ambulance Service.
Eleven patients were excluded from the follow‐up data search owing to incomplete details on the patient report forms (name and address), and a further eight patients opted out of the study. The remaining 175 patients included in the study had an average age of 83 years (range 65–99) and 111 (63.4%) were women. Just under half of all cases were attended to “out‐of‐hours”—between 18:00 and 08:00 (n = 82, 43.3%). Most patients (78.3%, n = 137) were classified as having “no injury or illness”; and 13 (7.4%) as having “minor cuts and bruising”. Three quarters of the patients (n = 126) were recorded as “assisted and treated but not conveyed”; 15% (n = 27) as “declined aid against advice”; 4% (n = 7) as “general practitioner to call and left in care”; and 4% (n = 7) as other.
In all, 86 of the 175 study participants (49.1%, 95% CI 41.5 to 56.8) made subsequent unplanned healthcare contacts within the 2‐week follow‐up period.
Eighty three of the 175 (47.4%, 95% CI 39.8 to 55.1) patients called an emergency ambulance again; 39 made more than one call (two calls: 21 patients; three calls: 8; four calls: 6; five calls: 1; six calls: 2; seven calls: 1).
Forty two (24%, 95% CI 17.9 to 31.0) patients attended the emergency department, 39 by emergency ambulance. Of the 27 people who attended study hospitals, 11 were admitted, with an increased risk of emergency hospital admission of 4.7 (95% CI 2.3 to 7.9) compared with the general population of the same age in London.
Four patients (2.3%) died, with an increased risk of mortality (standard mortality ratio) of 5.4 (95% CI 1.4 to 11.9) compared with the general population of the same age in London. The 2‐week case fatality rate of 2.3% among the study group compared with 0.43% in the corresponding general population in London.
Missing general practitioner details prevented the follow‐up of 68 cases and a further 20 general practitioners did not respond. Of the remaining 87 patients, 22 (25.3%) made contact with their general practitioner. For the other 65, general practitioners reported no contact within this period.
Discussion
In older people, falls are a common cause of emergency ambulance attendance, with a high rate of non‐conveyance. Those not taken to hospital have an alarmingly high rate of further emergency healthcare contact within 2 weeks. Previous studies in the UK and USA have found similar patterns of high non‐conveyance of this group,13,17,18 although outcomes have not previously been reported.
With a fivefold increased risk of emergency admission to hospital and a fivefold increased risk of death, this study has highlighted an easily identifiable high‐risk population that is not being adequately cared for within the existing healthcare system. Although we have not assessed the appropriateness of the decision to leave the patient at home, the finding that such a high proportion has made a further emergency care contact within such a short space of time adds weight to the conclusion that the emergency care currently provided by the ambulance service is doing little to meet the overall needs of the person who has fallen, and leaves the patient at high risk of falling again. Good evidence exists to support a multifactorial intervention for those who attend the emergency department after a fall, to prevent further falls and so improve health outcomes. No such evidence exists for the population that was attended by emergency ambulance, although, as they are known to be older and frailer,12,18 alternative care may not have the same positive effects on outcomes in this group as in the population that attends the emergency department. These findings suggest that there may be an opportunity to introduce a new model of care that could bring benefits for the individual, as well as more efficient use of the health and social care system, although a rigorous evaluation of any alternative model will need to be undertaken.
Despite the lack of evidence about effectiveness, the National service framework for older people recommends that those using the emergency ambulance service as a result of a fall should be referred to a falls service.19 The recent White paper Our health, our care, our say focuses on “improving patient experience and significantly reducing unnecessary admissions to hospital”,20 with paramedics and emergency care practitioners (ECPs) playing a role in providing care at the scene. This study was carried out with standard paramedic and emergency medical technician‐staffed vehicles. It cannot be assumed that the newly defined and nationally promoted ECPs, with their focus on assessment skills and links into an integrated urgent care system, will make the same decisions about whether to convey patients, or that their decisions will result in the same high rate of reattendance. With the ECP model only recently introduced, however, new information about current practice and outcomes, such as we have reported, must be fed into the development of the role, educational materials and evaluation of the model.
The findings of this study, alongside the policy and practice developments, make this subject both a service development and research priority. A randomised controlled trial is urgently needed to assess the effectiveness of alternative models of care. Without improvements in the quality of care provided, older people who fall will continue to be at risk of suffering poor health outcomes, as well as using disproportionately high levels of health services.
Abbreviations
ECP - emergency care practitioner
LAS - London Ambulance Service
PCT - primary care trust
Footnotes
Competing interests: None declared.
References
- 1.Keene G S, Parker M J, Pryor G A. Mortality and morbidity after hip fractures. BMJ 19933071248–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Day L, Fildes B, Gordon I.et al Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002325128–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scuffam P, Chaplin S.The incidence and costs of accidental falls in the UK. York: Health Economics Consortium, The University of York, 2002
- 4.Aminzadeh F, Dalziel W B. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes and effectiveness of interventions. Ann Emerg Med 200239238–247. [DOI] [PubMed] [Google Scholar]
- 5.Graham H J, Firth J. Home accidents in older people: role of primary health care team. BMJ 199230530–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Close J, Ellis M, Hooper R.et al Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 199935393–97. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie L D, Gillespie W J, Robertson M C.et alInterventions for preventing falls in elderly people (Cochrane Review). Cochrane Library. Chichester: John Wiley and Sons, 2003 [DOI] [PubMed]
- 8.Close J C T. Interdisciplinary practice in the prevention of falls – a review of working models of care. Age Ageing 200130(S4)S8–12. [DOI] [PubMed] [Google Scholar]
- 9.Aoyagi K, Ross P D, David J W.et al Falls among community‐dwelling elderly in Japan. J Bone Miner Res 1998131468–1474. [DOI] [PubMed] [Google Scholar]
- 10.American Geriatrics Society BGSaAAoOS: guidelines for the prevention of falls in older persons. J Am Geriatr Soc 200149664–672. [PubMed] [Google Scholar]
- 11.NICE Clinical guideline 21. Falls: the assessment and prevention of falls in older people. London: National Institute for Clinical Excellence, 2004
- 12.Close J C, Halter M, Elrick A.et al Falls in the older population: a pilot study to assess those attended by the London Ambulance Service but not taken to A&E. Age Ageing 200231488–489. [DOI] [PubMed] [Google Scholar]
- 13.Marks P J, Daniel T D, Afolabi O.et al Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: an epidemiological study. Emerg Med J 200219449–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg R J, Zautcke J L, Koenigsberg M D.et al A review of prehospital care litigation in a larger metropolitan EMS system. Ann Emerg Med 199019557–561. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health Taking healthcare to the patient. Transforming NHS ambulance services. London: Department of Health, 2005, www.dh.gov.uk/publications (accessed 7 Sep 2006)
- 16.Cooper S, Barrett B, Black S.et al The emerging role of the emergency care practitioner. Emerg Med J 200421614–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss S J, Chong R, Ong M.et al Emergency medical services screening of elderly falls in the home. Prehosp Emerg Care 2003779–84. [DOI] [PubMed] [Google Scholar]
- 18.Snooks H, Close J, Gaze S.et al Older fallers attended by the ambulance service and left at home: risks and opportunities. Final Report to the Wales Office of R&D (WORD). Centre for Health Improvement and Evaluation, Swansea University, SA2 8PP 2003
- 19.Department of Health National service framework for older people. London: Department of Health, 2001
- 20.Department of Health Our health, our care, our say. London: Department of Health, 2006 (White Paper),