Abstract
Background
Multicomponent Check-It-Out project interventions were found to be effective at increasing thorough skin self-examinations (TSSE). Application of this research will benefit from determining the most important interventions for promoting TSSE.
Objective
Identification of the most important Check-It-Out intervention components for promoting TSSE.
Methods
This study analyzed the responses of the 567 participants who were randomized into the skin examination intervention group and who did not report performing TSSE at their baseline interview.
Results
Watching the video, using the hand mirror, shower card, American Cancer Society brochure, sample photos, and finding the health educator helpful was associated with performing TSSE at 2 months, 12 months, or both.
Limitations
Use of the materials within the skin group was not randomly assigned. All data was based on participant self-report.
Conclusions
As future interventions to increase TSSE are developed, the identified useful components will be important to include.
Introduction
Melanoma remains a serious public health problem with an estimated 59,940 cases and 8110 melanoma deaths in 2007.1 Melanomas most frequently occur on visible skin surfaces including the trunk, head, and neck in men and the trunk and legs in women. Early detection may be instrumental in reducing melanoma mortality and is widely recommended for that purpose. Strategies to increase early detection include professional skin examinations as well as monthly thorough skin self-examination (TSSE).2
Those who receive physician advice, have a wall mirror, and an available partner are more likely to perform TSSE.3 A successful intervention was conducted (The Check-It-Out Project), which included instructional materials, cues and aids, health educator counseling, and follow up letters, to effectively increase the performance of TSSE.4 This report explores the use of the various components of the Check-It-Out intervention and their associations with subsequently performing successful TSSE in patients who were not previously performing TSSE.
Methods
Recruitment and Sample
Data analyzed were collected during the Check-It-Out Project, a randomized trial of an intervention developed to increase TSSE performance. The study participants were recruited from primary care practices in Rhode Island and Southeastern Massachusetts between May 2000 and December 2001. Participants were randomly assigned to one of two experimental groups: one that encouraged increasing TSSE performances and one that encouraged improvement of diet. Details of recruitment, study procedures, and patient population have been previously described.4, 5 The analyses for this paper were restricted to those 567 participants who were randomized into the skin examination group and who did not report performing TSSE at their baseline interview. Appropriate approvals from relevant institutional review boards and signed informed consents from participants were obtained.
Interventions
Participants in the skin examination group received an intervention directed at increasing TSSE performance for early detection of malignant melanoma. The intervention materials included educational materials, cues, aids, and a brief counseling session by a health educator. Their physicians did not participate in the intervention and were blinded to the group to which the participant was randomized. The content of the interventions were created or adapted by the project team and were guided by the transtheoretical model stages-of-adoption perspective as previously described.4
Educational Materials
The educational materials included the video, “Check It Out: Why and How to do Skin Self-Exam,”6 the American Cancer Society (ACS) brochure “Why You Should Know About Melanoma,”7 and sample photos of skin cancers. These materials advocated monthly TSSE with physician consultation for any new or changing skin lesions. The video contained motivational messages as well as specific “how-to” instructions and demonstrations for how to perform a skin self-exam. The sample photos included pictures of actual skin cancers with descriptions of common appearances of basal cell carcinoma, squamous cell carcinoma, and malignant melanoma cancers.
Environmental Cues
Environmental cues to action included a refrigerator magnet and a shower card. The refrigerator magnet was in the shape of a hand mirror and included the study logo. The shower card included directions for performing a TSSE on one side and warning signs for melanoma on the other side.
Aids
Aids to help perform self-examinations included a hand mirror and a body diagram for noting locations of individual lesions.
Health Educator Counseling Session
The brief counseling session for participants consisted of one-on-one sessions with the health educator, and included assessment of current practice, motivating factors for performance of thorough skin self-examination, barriers to improvement, and agreement between the participant and health educator on an action plan. The action plan was created based on the principles of social cognitive theory, which emphasizes the need to provide a clear plan for behavior change. The health educator made a follow-up call 3 weeks later to discuss the participant’s progress.
Feedback letters
After the 2 and 6 month interviews, each participant also received a feedback letter individually tailored to their TSSE performance, perceived risk of skin cancer, intention to perform TSSE, and availability of a partner to help with TSSE.
Measures
Follow-up telephone interviews were scheduled with all participants at 2, 6, and 12 months after randomization. TSSE was defined as those who responded “once” or more times to questions regarding whether or not they carefully examined each of seven areas of the body (the front of you from the waist up, the front of your thighs and legs, the bottoms of your feet, your calves, the back of your thighs, your buttocks and lower parts of your back, and your upper back).
At two months, participants were asked to the respond to the question “How much of the video that the health educator gave you did you watch?” on a 1 to 4 scale from “all” to “none”. At 12 months respondents reported whether or not they had used the following items that the health educator gave them: hand mirror, shower card, refrigerator magnet, ACS brochure, and sample photos. They also reported how helpful they thought the item was in helping them to perform a thorough skin exam on a scale of 1 to 3 from “very helpful” to “not helpful.” Participants were also asked to rate how helpful it was to meet with the health educator on a scale of 1 to 4 from “very helpful” to “not helpful at all” and to indicate yes or no if they thought the materials would have worked the same if they were received without a meeting with the health educator. They also indicated whether or not they received and read the follow up letters, and rated the helpfulness of the follow up letters on a 1 to 4 scale from “very helpful to “not helpful at all.”
Use of the intervention materials by demographic characteristics, perceived and estimated skin cancer risk, and the previously identified baseline TSSE predictors (receiving physician advice, having a wall mirror, and having an available partner) were assessed. The demographic characteristics, perceived and estimated skin cancer risk, and baseline TSSE predictors are previously described.3 For the univariate analyses, responses to questions regarding amount of video watched and whether or not participants found the health educator helpful were recoded into dichotomous variables. Amount of video watched response choices ‘all’, ‘some’, and ‘a little’ were recoded into “Yes,” and ‘none’ was recoded into “No.” Responses to helpfulness of the health educator were recoded “No” for ‘not very helpful’ or ‘not helpful,’ and “Yes” for ‘very helpful’ or ‘helpful.’ All responses originally entered as “doesn’t remember,” “don’t know,” or “refused” were recoded as missing for the univariate analyses.
Statistical Analysis
Comparison of groups on categorical variables were assessed using chi-squared analyses and age was analyzed as a continuous variable using Pearson product-moment correlations. Associations of use of materials and helpfulness of materials with performance of TSSE were assessed using logistic regression. Statistical analyses were performed using STATA 8.0.
Results
Participants
The Check-It-Out project enrolled 1356 participants who were recruited from 11 practices; 688 were randomized to the skin group. The study population is described in more detail in a previous report.5
The analysis reported here are restricted to 567 participants in the skin group who were not performing TSSE at baseline (82% of those randomized to the skin group). By 2, 6, and 12 months after randomization, 47%, 50%, and 49%, respectively of those not reporting TSSE at baseline were performing TSSE.
Overall Use of Materials
At 2 months, 50% of the participants watched all the video and an additional 16% reported watching some of the video (Table 1). At 12 months most participants reported using the hand mirror, ACS brochure, and sample photos; and approximately one-third reported using the shower card and the refrigerator magnet. Except for the refrigerator magnet, most of the participants reported that each of the components of the intervention was very helpful in performing a thorough skin self-examination (Table 2).
Table 1.
Use of video
| How much of the video that the health educator gave you did you watch? | |||||
|---|---|---|---|---|---|
| (%) of respondents | |||||
| All | Some | A Little | None | Don't Know/Refused | |
| N | (%) | (%) | (%) | (%) | (%) |
| 325 | 50% | 8 | 8 | 32 | 1 |
Table 2.
Use and helpfulness of materials
| Have you used the items that the health educator gave you at the beginning of the project? | How helpful was the item in helping you to do a thorough skin examination? Would you say…. | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Yes | No | Don't know/Refused | N | Very Helpful | Somewhat Helpful | Not helpful | Don't know/Refused | |
| (%) | (%) | (%) | (%) | (%) | (%) | (%) | |||
| Hand Mirror | 382 | 86 | 14 | 0 | 327 | 69 | 30 | 1 | 0 |
| Shower card | 382 | 29 | 68 | 4 | 110 | 57 | 37 | 5 | 0 |
| Refrigerator magnet | 382 | 33 | 65 | 2 | 127 | 37 | 46 | 16 | 1 |
| ACS Brochure | 382 | 63 | 35 | 2 | 240 | 59 | 37 | 3 | 1 |
| Sample Photos | 382 | 73 | 25 | 2 | 278 | 68 | 31 | 1 | 0 |
About half of the participants found the meeting with the health educator helpful. One-third found it very helpful and most felt that this meeting affected how they used the materials. Two-thirds of the participants reported reading the follow up letters and about half of those found those somewhat helpful (Figure 1).
Figure 1. Helpfulness of health educator and letters.
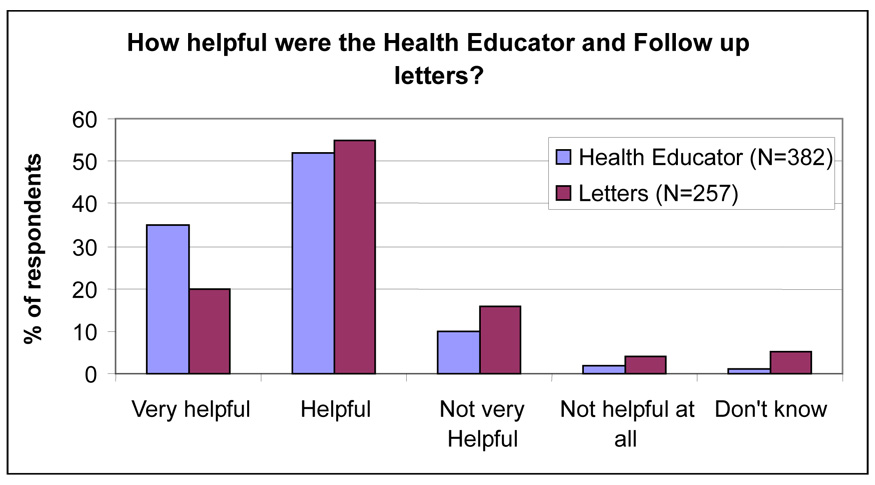
Notes: Fifty-eight percent of respondents felt the materials would not have worked the same if they were received without a health educator meeting. Sixty-seven percent of respondents received and read the follow up letters.
Predictors of using materials
Table 3 displays the reported use of the video at 2 months after the intervention by demographic characteristics (age, gender, education), perceived and estimated skin cancer risk, and previously noted predictors of TSSE (receiving physician advice, availability of a partner, availability of a wall mirror). Respondents who reported watching the video were on average 3.5 years older. None of the other factors examined were associated with watching the video.
Table 3.
Associations of intervention components with demographics and TSSE predictors % respondents in each response category unless otherwise specified
| Did you watch the video? |
Did you find the health educator helpful?* |
Did you read the follow up letters? |
Did you use the hand mirror? |
Did you use the shower card? |
Did you use the refrigerator magnet? |
Did you use the ACS Brochure? |
Did you use the sample photos? |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | P | No | Yes | P | No | Yes | P | No | Yes | P | No | Yes | P | No | Yes | P | No | Yes | P | No | Yes | P | |
| Education n | 108 | 214 | .8 | 46 | 334 | .03 | 62 | 257 | .5 | 55 | 327 | .133 | 258 | 110 | .5 | 247 | 127 | .7 | 133 | 240 | .2 | 97 | 278 | .6 |
| Less hs | 7 | 9 | 0 | 6 | 10 | 5 | 2 | 6 | 5 | 7 | 5 | 6 | 5 | 5 | 4 | 6 | ||||||||
| Hs grad | 22 | 27 | 17 | 27 | 26 | 25 | 25 | 26 | 25 | 25 | 27 | 23 | 33 | 23 | 30 | 24 | ||||||||
| After hs | 29 | 26 | 24 | 28 | 26 | 30 | 20 | 30 | 27 | 31 | 27 | 32 | 26 | 30 | 29 | 28 | ||||||||
| College | 42 | 38 | 59 | 38 | 39 | 40 | 53 | 38 | 43 | 36 | 42 | 39 | 36 | 42 | 37 | 42 | ||||||||
| Age n | 108 | 214 | .036 | 46 | 334 | 62 | 257 | 55 | 327 | 258 | 110 | 247 | 127 | 133 | 240 | 97 | 278 | |||||||
| Mean age | 5.8 | 54.3 | 52.1 | 55.1 | .16 | 53.8 | 54.7 | .9 | 53.1 | 55.1 | .3 | 53.6 | 56.6 | .06 | 54.7 | 54.7 | 1 | 52.8 | 55.9 | .047 | 54.1 | 54.9 | .6 | |
| Gender n | 108 | 214 | .8 | 46 | 334 | .7 | 62 | 257 | .5 | 55 | 327 | .098 | 258 | 110 | .03 | 247 | 127 | .023 | 133 | 240 | .2 | 97 | 278 | .8 |
| Male | 47 | 46 | 43 | 47 | 48 | 43 | 56 | 44 | 50 | 37 | 50 | 38 | 50 | 44 | 47 | 46 | ||||||||
| Female | 53 | 54 | 57 | 53 | 52 | 57 | 44 | 56 | 50 | 63 | 50 | 62 | 50 | 56 | 53 | 54 | ||||||||
| Perceived risk n | 104 | 207 | .9 | 46 | 326 | .037 | 59 | 254 | .3 | 54 | 320 | 1 | 253 | 107 | .2 | 241 | 125 | .3 | 127 | 238 | .059 | 97 | 270 | .2 |
| Very High | 6 | 6 | 7 | 6 | 3 | 7 | 7 | 6 | 7 | 5 | 7 | 6 | 4 | 8 | 9 | 6 | ||||||||
| High | 13 | 12 | 20 | 12 | 20 | 12 | 13 | 13 | 12 | 13 | 12 | 14 | 7 | 15 | 16 | 11 | ||||||||
| Moderate | 45 | 43 | 59 | 43 | 37 | 46 | 46 | 45 | 43 | 47 | 42 | 50 | 47 | 45 | 37 | 49 | ||||||||
| Low | 24 | 24 | 9 | 23 | 24 | 21 | 19 | 22 | 21 | 27 | 22 | 22 | 26 | 19 | 22 | 22 | ||||||||
| Very Low | 12 | 15 | 7 | 15 | 15 | 15 | 15 | 14 | 17 | 8 | 17 | 9 | 15 | 13 | 15 | 13 | ||||||||
| Estimated risk n | 107 | 213 | .6 | 43 | 332 | .9 | 62 | 254 | .7 | 55 | 322 | .4 | 254 | 109 | 1 | 242 | 127 | .9 | 131 | 237 | .3 | 95 | 275 | .091 |
| High | 22 | 26 | 23 | 24 | 19 | 24 | 22 | 25 | 25 | 24 | 24 | 26 | 21 | 26 | 33 | 21 | ||||||||
| Moderate | 32 | 32 | 30 | 33 | 35 | 33 | 27 | 34 | 32 | 32 | 33 | 32 | 31 | 35 | 29 | 34 | ||||||||
| Low | 47 | 42 | 47 | 42 | 45 | 43 | 51 | 41 | 43 | 44 | 43 | 42 | 48 | 39 | 38 | 44 | ||||||||
| Dr advice n | 104 | 211 | 1 | 46 | 326 | .049 | 61 | 251 | .9 | 54 | 320 | .6 | 255 | 108 | .2 | 240 | 126 | .082 | 131 | 235 | .3 | 93 | 274 | .6 |
| No | 65 | 65 | 80 | 66 | 67 | 68 | 64 | 68 | 70 | 64 | 71 | 62 | 71 | 66 | 70 | 67 | ||||||||
| Yes | 35 | 35 | 20 | 34 | 33 | 32 | 35 | 32 | 30 | 36 | 29 | 38 | 29 | 34 | 30 | 33 | ||||||||
| Wall Mirror n | 108 | 214 | .062 | 46 | 334 | .8 | 62 | 257 | .8 | 55 | 327 | .6 | 258 | 110 | .8 | 247 | 127 | .19 | 133 | 240 | .8 | 97 | 278 | .3 |
| No | 28 | 19 | 20 | 21 | 21 | 20 | 24 | 20 | 21 | 23 | 19 | 24 | 22 | 20 | 25 | 20 | ||||||||
| Yes | 72 | 81 | 80 | 79 | 79 | 80 | 76 | 80 | 79 | 77 | 81 | 76 | 78 | 80 | 75 | 80 | ||||||||
| Partner n | 108 | 214 | .3 | 46 | 334 | .2 | 62 | 257 | .4 | 55 | 327 | .3 | 258 | 110 | .7 | 247 | 127 | .6 | 133 | 240 | .7 | 97 | 278 | .4 |
| No | 10 | 14 | 11 | 18 | 21 | 17 | 22 | 17 | 16 | 17 | 16 | 18 | 16 | 18 | 20 | 16 | ||||||||
| Yes | 90 | 86 | 89 | 82 | 79 | 83 | 78 | 83 | 84 | 83 | 84 | 82 | 84 | 83 | 80 | 84 | ||||||||
Table Notes: less hs=less than high school; Hs grad=high school graduate; after hs=Some after high school; College=college graduate
Dr advice=Received physician advice to perform skin self-exam; Wall Mirror=Availability of a wall mirror; Partner=Availability of a partner
No=Not very or not helpful; Yes=Very helpful/helpful
The demographic characteristics, perceived and estimated skin cancer risk, and TSSE predictors were also examined with use of specific intervention materials other than the video, reported helpfulness of the health educator, and reported use of the follow-up letters. Respondents who found the health educator helpful were more likely to be less educated, to have received physician advice to perform skin self-exam, and to have a lower perceived skin cancer risk. More women than men reported using the shower card and refrigerator magnet. Respondents using the ACS brochure were older than those who did not use the brochure. None of the other demographic factors or TSSE predictors were associated with finding the health educator helpful, reading the letters, or using the other materials (Table 3).
Associations of intervention components with TSSE performance
We assessed multiple components of the intervention for the associations of the reported use or helpfulness with performance of TSSE. Use of the hand mirror was the single component most strongly associated with performance of TSSE at both 2 and 12 months. Other components significantly associated with TSSE at both time points included watching the video and using the ACS brochure. Finding the health educator helpful and using the shower card was associated with performing TSSE at 12 months, and using the sample photos was associated with performing TSSE at 2 months. Using the refrigerator magnet and reading the follow up letters was not significantly associated with performing TSSE at either time points (Table 4).
Table 4.
Associations of intervention components with TSSE performance
| Time point TSSE | Did you watch the video? | Did you find the health educator helpful?* | Did you read the follow up letters? | Did you use the hand mirror? | Did you use the shower card? | Did you use the refrigerator magnet? | Did you use the ACS brochure? | Did you use the sample photos? |
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | ||||||||
| TSSE 12 mo | 1.8(1.0–3.0) | 2.2 (1.1–4.2) | 1.6 (.91–2.8) | 3.0 (1.6–5.6) | 2.1 (1.3–3.3) | 1.2 (.80–1.9) | 1.6 (1.1–2.5) | 1.4 (.86–2.2) |
| TSSE 2 mo | 2.7 (1.7–4.4) | 1.7 (.87–3.5) | 1.4 (.76–2.5) | 3.0 (1.5–5.8) | 1.4 (.87–2.2) | 1.2 (.77–1.9) | 1.9 (1.2–3.0) | 2.0 (1.2–3.3) |
Table notes: Response values: No=0, Yes=1
No=not very or not helpful; Yes=very helpful/helpful
Discussion
While melanoma remains a growing problem worldwide, it is curable if detected and excised at an early stage. Monthly thorough skin self-examination (TSSE) has been associated with reduced melanoma mortality.8 It has been previously shown that the Check-It-Out intervention produced a sustained increase in the performance of skin self-examinations with only a transient increase in skin surgieries.4 The goal of this study was to examine the use and perceived helpfulness of the Check-It-Out intervention components and their associations with adopting the practice of TSSE.
We identified intervention components that may be particularly important in promoting TSSE performance in patients currently not performing TSSE. The video was watched by a majority of the participants and more participants reported using the hand mirror than any other item. The ACS brochure and sample photos were also used by a majority of the participants, while the shower card and refrigerator magnet were used by about a third of the respondents. Most respondents found the hand mirror, shower card, ACS brochure, and sample photos very helpful.
The low percentage of patients reporting using the shower card (29%) given the finding that use of the shower card was associated with performing TSSE at 12 months suggests that skin examination reminders and cues may be effective for increasing TSSE even though fewer patients report using them. The higher percentage of patients reporting using the hand mirror, ACS brochure, and sample photos may be due to the use of these materials by patients to perform or to learn how to perform skin examinations. Previous reports have also documented the utility of photos to augment the performance of skin self-examinations.9 The strong association of using the hand mirror with performing TSSE suggests that interventions to enhance TSSE behavior should directly address the need for skin self-exam aids.
Our finding that older persons were more likely to use the video and ACS brochure is particularly relevant for skin cancer prevention as melanoma incidence and mortality increases with age.10 The finding that the shower card and refrigerator magnet were more likely to be used by women than men suggests that cues targeted to men would be useful in developing future interventions. This type of targeting is appropriate since melanoma mortality is particularly high in older men.11
Less highly educated participants reported greater helpfulness of the health educator, which may be due to lack of previous exposure for this group, and the more highly educated patients finding the messages of the health educator redundant with other materials they received or representing concepts they already knew. Patients who reported lower perceived skin cancer risk may have not previously been exposed to skin cancer education and were more receptive to the messages of the health educator. The observation that respondents who found the health educator helpful were more likely to report receiving physician advice may indicate that the health educator messages serve to effectively reinforce physician messages. This finding has implications for development of future physician and health educator collaborations to more effectively persuade patients to adopt health prevention behaviors.
This study has a number of limitations. While the overall initial study population was randomized into skin and diet groups, use of the provided materials was determined by the participant and not randomly assigned. Furthermore, the causal sequence of using the intervention materials and performing TSSE is uncertain. For example, the provision of a hand mirror might have been a motivating factor in performing TSSE, or an implement of convenience to complete TSSE that was otherwise motivated. With these data, we are only able to make associations and cannot infer that particular intervention materials caused patients to perform TSSE, although the overall intervention did. The data from this analysis also relied on self-report of using the intervention materials and TSSE performance, and we were not able to verify that respondents actually used the materials and performed TSSE. In addition, while skin self-examination may decrease melanoma mortality, its usefulness may be dependent on the ability of individuals to obtain medical care, which was available to participants in this study since they were recruited at the time of a medical visit. Finally, the health educators used in the study trained with a semi-structured scripted interview, but were not trained to adhere to a formal script. The same three health educators were used throughout the study at all sites and all patients were randomized without regard to the assignment of the health educator, however, variability amongst the three educators was not controlled for by the study and were not measured.
A strength of this study is that it is based within a randomized controlled trial in which the intervention was proven effective. Also, because participants were recruited from primary care physician practices and were not restricted to high-risk individuals, these results are potentially applicable to a general patient population. The identification of the most useful components may be directly applicable to clinical and health educator practices.
Skin self-examination is a promising practice to decrease melanoma mortality. We conducted a successful intervention to increase the performance of thorough skin self-examinations. These analyses identify which components of the intervention were most important so that future interventions may be further improved. Improved efforts to facilitate behavioral change in patients currently not performing TSSE may be instrumental to increasing earlier detection of skin cancer.
Acknowledgments
Funding Sources: This research was supported by grant R01CA78800 from the National Cancer Institute. Dr. Weinstock is also supported by CSP562 from the Department of Veterans Affairs, and grants R01CA106592, R01AR49342, R25CA087972, and R01CA106807 from the National Institutes of Health.
Abbreviations Used
- TSSE
Thorough skin self-examination
- ACS
American Cancer Society
Footnotes
Conflict of Interest Disclosure: None declared.
Prior Presentation: Contents of the manuscript have not been previously published or presented and are not currently submitted elsewhere.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Cancer Society. [Accessed November 28, 2007];Cancer facts and figures 2007. Available at: www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf.
- 2.Weinstock MA. Early detection of melanoma. JAMA. 2000;284:886–889. doi: 10.1001/jama.284.7.886. [DOI] [PubMed] [Google Scholar]
- 3.Martin RA, Weinstock MA, Risica PM, Smith K, Rakowski W. Factors associated with thorough skin self-examination for the early detection of melanoma. J Eur Acad Dermatol Venereol. 2007;21:1074–1081. doi: 10.1111/j.1468-3083.2007.02199.x. [DOI] [PubMed] [Google Scholar]
- 4.Weinstock MA, Risica PM, Martin RA, Rakowski W, Dube C, Berwick M, et al. Melanoma early detection with thorough skin self-examination: the "Check It Out" randomized trial. Am J Prev Med. 2007;32:517–524. doi: 10.1016/j.amepre.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstock MA, Risica PM, Martin RA, Rakowski W, Smith KJ, Berwick M, et al. Reliability of assessment and circumstances of performance of thorough skin self-examination for the early detection of melanoma in the Check-It-Out Project. Prev Med. 2004;38:761–765. doi: 10.1016/j.ypmed.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 6.Video. "Check It Out: Why and how to do Skin Self-Exam" can be ordered from the American Cancer Society (ACS code 2301.05)
- 7.American Cancer Society booklet "Why You Should Know About Melanoma". Downloadable from www.cancer.org.
- 8.Berwick M, Begg CB, Fine JA, Roush GC, Barnhill RL. Screening for cutaneous melanoma by skin self-examination. J Natl Cancer Inst. 1996;88:17–23. doi: 10.1093/jnci/88.1.17. [DOI] [PubMed] [Google Scholar]
- 9.Oliveria SA, Dusza SW, Phelan DL, Ostroff JS, Berwick M, Halpern AC. Patient adherence to skin self-examination. effect of nurse intervention with photographs. Am J Prev Med. 2004;26:152–155. doi: 10.1016/j.amepre.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Ries L, Eisner M, Kosary C, Hankey B, Miller B, Clegg L, et al. Bethesda MD: National Cancer Institute; SEER Cancer Statistics Review, 1975–2002. http://seer.cancer.gov/csr/1975_2002/, based on November 2004 SEER data submission, posted to the SEER web site 2005.
- 11.Geller AC, Swetter SM, Brooks K, Demierre MF, Yaroch AL. Screening, early detection, and trends for melanoma: current status (2000–2006) and future directions. J Am Acad Dermatol. 2007;57:555–572. doi: 10.1016/j.jaad.2007.06.032. [DOI] [PubMed] [Google Scholar]


