Abstract
Introduction
According to national organisations, obstetric services should be able to initiate a caesarean delivery within 30 minutes of the decision to operate. This is uniquely challenging in a small, rural hospital. In 2001, the authors' hospital was unable to meet this guideline reliably. This project demonstrates how we improved our emergency caesarean delivery response time.
Methods
The caesarean delivery process was examined, project co‐chairs were selected and key personnel were identified. Four working groups (doctors, nurses, anaesthesia, operating room personnel) were formed to analyse and improve component parts of the process. Over time, multiple small changes were made, initially by each working group and then by the entire caesarean delivery team. Decision‐to‐incision time was the main outcome measure. The authors also measured standard birth statistics and tracked the percentage of caesarean deliveries that were classified as an emergency.
Results
Forty emergency caesarean deliveries occurred during the study. The mean decision‐to‐incision time dropped from 31 to 20 minutes and the treatment to goal ratio increased from 0.5 to 1.0. The percentage of caesarean deliveries that were classified as emergencies dropped significantly. There has been no change in the overall caesarean delivery rate or other markers of obstetric quality.
Conclusions
A small, rural community hospital with limited resources can consistently meet the 30 minute decision‐to‐incision guideline for emergency caesarean delivery.
The American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (ACOG), two of the main accrediting organisations in the US, recommend 30 minutes from decision‐to‐incision for emergency caesarean delivery.1 A review of the literature suggests that many hospitals struggle to meet this guideline and small, rural facilities are no exception.2,3,4,5,6 Small facilities have limited resources and, more importantly, those resources may not be immediately available. Often, critical personnel are not “in‐house” at critical times. Additionally, birth attendants, such as Certified Nurse Midwives (CNMs) or Family Practice physicians, who often attend deliveries at small, rural hospitals, may not be able to perform a caesarean delivery. Responding to obstetric emergencies in such a setting is uniquely challenging.
In early 2001, a sentinel event at our facility led us to evaluate our caesarean delivery response times. Although we sporadically had the ability to initiate an emergency caesarean delivery within 30 minutes of the decision to operate, we could not do so consistently. Without this consistency, the safety of our obstetric patients was potentially compromised. Additionally, because the ACOG has clearly stated that facilities with obstetric services should have “… personnel to permit the start of a cesarean delivery within 30 minutes of the decision to perform the procedure”,7 we were not compliant with the recommendation of a leading professional organisation. Therefore, the purpose of our improvement project was to improve the consistency and reliability of the caesarean delivery process and to achieve emergency caesarean delivery response times of less than 30 minutes.
Methods
Setting
Alice Peck Day Memorial Hospital (APD) is a 32 bed hospital located in Lebanon, New Hampshire, USA. The birthing centre has six labour/delivery/recovery/postpartum rooms and a Level I nursery. This unit is usually staffed by a minimum of two nurses. During delivery, one‐on‐one nursing is provided. When this project started in 2001, two independent physician groups, employing four providers, admitted obstetric patients. Paediatric services were provided by 16 physicians distributed among four independent practices. Three anaesthesia practitioners provided continuous coverage. Caesarean deliveries are performed in the hospital's main operating room. The operative team consisted of the attending obstetrician, the first assistant, the paediatric provider, the anaesthesiologist, two operating room staff and the birthing centre nurse.
As the hospital has grown, physician groups have expanded, consolidated and changed practice patterns. Currently, three obstetricians and three CNMs are employed by the hospital. One additional CNM has a small independent practice. The majority of in‐house paediatric services are now provided by one hospital‐owned practice that employs four family practitioners and two paediatricians. Anaesthesia and operating room services are unchanged; although, we no longer consistently have a first assistant at all caesarean deliveries.
Interventions
In early 2001, an unanticipated intrapartum fetal demise occurred. A root cause analysis was conducted and numerous contributing factors were identified. Although it was not definitely identified as one of the root causes, caesarean delivery response time was identified as a potential problem area and the root cause analysis committee asked for an appraisal of the hospital's capabilities. When that appraisal revealed an inability to meet the 30 minute guideline consistently, one of the obstetricians (SEM) and the birthing centre nurse manager (WS) were asked to co‐chair a Quality Improvement Project. The project goal was to decrease decision‐to‐incision times for all emergency caesarean deliveries to less than 30 minutes.
Phase I of the project began by mapping the current process for a routine caesarean delivery. This work identified key personnel which led the project co‐chairs to form four working groups that consisted of: (1) birthing centre nurses, (2) obstetric and paediatric providers, (3) anaesthesia providers, and (4) operating room personnel (OR). Each working group met to identify and improve “their” components of the routine caesarean delivery process. The most critical improvements, which were achieved in each of the four working groups, are described in detail in table 1. Initially, during Phase I of the project, the working groups independently improved their “piece” of the process while the co‐chairs integrated the improvements into the whole. However, as component parts of the pathway were refined, changes spread across working groups. Phases II and III involved members of all working groups who worked to improve the common processes. During phase I of the project, we collected significant amounts of data after each emergency caesarean delivery. In addition to evaluating the overall decision‐to‐incision time, we also evaluated intermediate times such as the “time to contact the team” and the “time from birthing centre to operating room”. The collection of this information allowed us to better understand the process of caesarean delivery and to identify the true barriers to efficiency.
Table 1 Summary of working group improvement efforts by phase of implementation.
| Phase | Date complete | Interventions by working groups | |||
|---|---|---|---|---|---|
| Birthing centre nurses | Providers | Anaesthesia | Operating room | ||
| 1 | Summer 2002 | • Analysed tasks | • Established dedicated CD phone line | • Created OB anaesthesia questionnaire | • Purchased dedicated OR infant “stabilet” |
| • Reassigned inappropriate tasks | • Programmed on‐call team members into computer | • Placed completed questionnaire on birthing centre | • Prepare OR for “STAT” CD each evening | ||
| • Eliminated unnecessary tasks (eg transfer of patient to stretcher) | • Programmed birthing centre phones with CD line on speed dial | • Developed process for antenatal anaesthesia consults | • Trained birthing centre nurses to check “stabilet” and OR preparedness each evening | ||
| • Organised supplies into CD kits | • Instituted nightly test of system with mandatory call back requirement | • Review OB high risk and VBAC lists each week | |||
| • Replaced OR checklist with CD specific checklist | • Designated codes to indicate “STAT” v routine CD | • Recommend CBC, type and screen on all labouring women | |||
| 2 | Spring 2003 | • Used mock CDs to identify steps in routine process that could be eliminated during emergency | • Developed standardised terminology | • Worked with providers to develop standardised terminology | • Synchronised OR clocks with birthing centre clocks |
| • Distributed flow charts of “STAT” process | • Created standardised brief operative note | • Assisted with development of “STAT” process map | • Assisted with development of “STAT” process map | ||
| • Finalised “STAT” process map | • Assisted with development of “STAT” process map | ||||
| 3 | Spring 2004 | • Participated in OR skills day and “STAT” pathway mock drills | • Participated in OR “skills day” and “STAT” pathway mock drills | • Participated in OR “skills day” and “STAT” pathway mock drills | • Participated in OR “skills day” and “STAT” pathway mock drills |
| • Empowered nurses and CNMs to transport patients to OR in emergency | |||||
| • Trained nurses in anaesthesia set up | |||||
| • Trained nurses in OR set up | |||||
CD, caesarean delivery; OR, operating room.
Measures and analysis
Alice Peck Day Memorial Hospital's standard birthing centre statistics include total number of births, total number of caesarean deliveries, total number of primary caesarean deliveries, five5 minute Apgar scores < 7, and transfers to a regional neonatal intensive care unit. Yearly rates of these core measures were compared using “test for trend” analysis with significance set at p<0.05 (Statistical Software R, 2005, R Development Core Team, Vienna, Austria). Additionally, we used a p‐type control chart to evaluate the variation in caesarean deliveries as a proportion of total deliveries over time.8
Our main outcome measure was the decision‐to‐incision time for each emergency caesarean delivery. These are individual, variable type data, so are best analysed on an XmR control chart that evaluates variation over time.8 Additionally, this type of chart allows us to determine compliance with the 30 minute guideline. Data are collected by the birthing centre nurse manager who reviews the medical record after each caesarean delivery. An emergency caesarean delivery is defined as one that the attending obstetrician believes should be done in less than 30 minutes. A “brief operative note” template that classifies preoperative diagnoses as emergency or non‐emergency is used to help physicians decide the acuity of the situation (a copy of this template is provided in the Appendix). This template also allows the birthing centre nurse manager to identify retrospectively all emergency caesarean deliveries. The decision time is defined as the time that the phone call to the answering service is placed. Incision times are documented on the operative record.
Since our goal was to reach a benchmark of less than 30 minutes consistently, we calculated a treatment‐to‐goal ratio for the initial system of care and for the system that emerged in response to our quality improvement efforts.8 (A treatment to goal ratio can be calculated when an established standard is used in conjunction with a control chart. The denominator is the total number of data points within the study period. The numerator is the number of data points that meet the standard). Finally, we evaluated the proportion of caesarean deliveries that were classified as an emergency by quarter. This final analysis was conducted with a p‐type control chart. All charts were created with Microsoft Excel SPC XL 2000 software (Microsoft Corporation, Redmond, Washington, USA).
Results
Phase I: evolution of the working groups
The project began with the creation of four working groups that met regularly to work on specific component parts of the pathway. The results from each working work are summarised on table 1 and discussed in detail below.
The birthing centre nurses focused on organising preoperative supplies and clarifying nursing tasks. This began with an analysis of the preoperative nursing tasks. The nurses classified each task as appropriate, inappropriate or unnecessary. Because the nurses felt that tasks such as maintaining the call schedule were inappropriate, such duties were reassigned to administrative personnel. Unnecessary tasks, such as transferring the patient to a stretcher were eliminated. A final list of nursing tasks was created and the supplies needed to accomplish them were placed in dedicated caesarean delivery prep kits. A plan for stocking and maintaining the kits was created. Using the task and supply lists that they had developed, the nurses were able to create a caesarean delivery preoperative checklist that replaced the pre‐existing surgery form which had routinely caused delay and frustration.
The provider working group—obstetricians, family practitioners, paediatricians and anaesthesia providers—worked to improve identification and notification of the call team members. Prior to this improvement effort, members of the caesarean delivery call team were listed on the main hospital call schedule in multiple places. This disorganisation made it difficult to contact the necessary personnel efficiently in an emergency. In order to better organise the information, a process change was instituted whereby, each week, an administrative assistant identified the caesarean delivery call team members and recorded their names, pager numbers and home telephone numbers on a one page grid. The current and upcoming weeks' grids were then filed in a binder on labour and delivery. Difficulties arose, however, because although nurses could now readily identify team members, they were still responsible for paging each person individually and critical time was lost waiting for return phone calls. Additionally, at such a small facility, last‐minute telephone number changes are common and the call grid often contained inaccurate information. For these reasons, these initial changes did not substantially decrease the time required to contact all of the team members. In response, an answering service that provides a dedicated caesarean delivery phone line was set up by the hospital. The answering service now maintains the on‐call list and takes responsibility for contacting individual team members via computer dialing and tracking. Last‐minute number changes are easily programmed into the computer. Team identification and notification, which used to take upwards of 20 minutes, is now accomplished within 5 minutes because the dedicated phone line is programmed on speed dial at the birthing centre. More importantly, nurses are able to focus on patient care rather than the phones.
The efforts of the third working group, anaesthesia services, centred on improving communication between the obstetric and anaesthesia providers. The team created a standardised “anaesthesia” questionnaire that is now administered to all prenatal patients at about 28 weeks estimated gestational age. This document contains medical questions pertinent to anaesthesia administration (for example, is there a family history of malignant hyperthermia?) and is reviewed by an anaesthesia provider antenatally so that patients at high risk of anaesthetic complication are identified and evaluated well before delivery. The questionnaire is then placed in the inpatient record, where it is readily accessible in the event of an obstetric emergency.
The fourth working group consisted of individuals representing operating room management and staff. They worked to prepare the operating room for an emergency caesarean delivery each evening. Necessary supplies are now readily available. A dedicated infant stabilet (warming table for newborns), purchased with money donated by the hospital auxiliary, is placed outside the operating room each evening. Birthing centre nurses have instituted a nightly check of the stabilet and operating room preparedness.
During phase I (table 1) of the project, these four groups met regularly. The two co‐chairs were present at all meetings and acted as liaisons. As the working groups began meeting, key “time” metrics (for example, time to contact team members, time from birthing centre to operating room, etc) were collected at every caesarean delivery. This information was analysed by the co‐chairs and reported back to the working groups so that all were aware of the process performance.
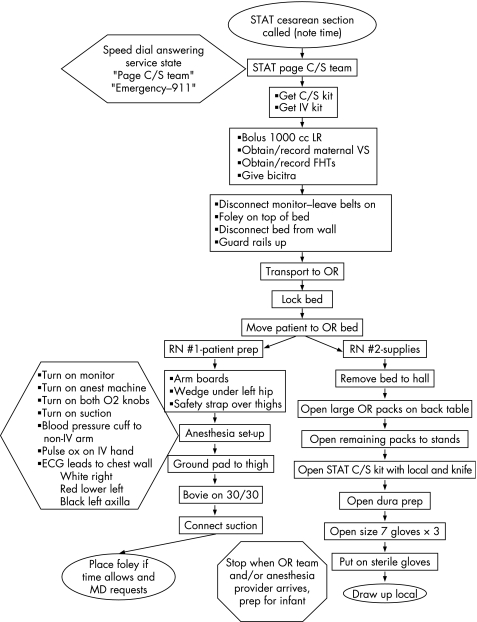
Phases II and III: assembling the component parts
Phase II of the project began when we had defined and standardised the routine process well enough to begin working on the emergency caesarean delivery process that we named the STAT pathway. Selected members of each working group were brought together to simulate the routine process multiple times. These sessions, which involved repeated physical “walk‐throughs” of the process, resulted in clarification of roles and definitions as well as the reordering of some steps. (Readers who are interested in learning more about our walk‐through simulations for caesarean deliveries should contact the primary author). Additionally, we reached consensus as to which steps could be eliminated in the event of an emergency. The STAT pathway that was created was then represented on a flowchart and posted on the birthing centre. Feedback and comments were solicited from each of the four working groups and a final process map was created (fig 1). During phase III of the project, the STAT pathway flowchart was used to train the birthing centre nurses to prepare the operating room and patient for an emergency caesarean delivery. Additionally, nurses and CNMs were empowered to transport patients to the operating room under selected circumstances (for example, cord prolapse, haemorrhage, bradycardia). A plan for scheduled drills was developed. Decision‐to‐incision time from those drills and from emergency caesarean deliveries is evaluated by the project co‐chairs in order to monitor the process continuously. The STAT pathway is also now used to orient new nurses to the unit and it is included in the annual assessment of nursing core competencies. The STAT pathway is dynamic, so additional interventions are implemented on an “as needed” basis.
Figure 1 “STAT” caesarean delivery process map.
Clinical outcomes
The hospital's core obstetric statistics for 2001–6 (quarters 1 and 2) were stable (table 2). Although there appears to be some variation year to year, there is no statistical difference in these measures as determined by a “test for trend”. The caesarean delivery rate was further evaluated with a p‐chart (fig 2) and there is only common cause variation over 22 quarters of data.
Table 2 Alice Peck Day Memorial Hospital birthing centre statistics (2001–6).
| Year | Births (n) | Caesarean deliveries total (primary)* | % Cesarean deliveries total (primary) | % Vaginal birth after caesarean (VBAC rate)† | Infants with 5 minute APGAR <7‡ | Infants transferred to neonatal intensive care unit‡ |
|---|---|---|---|---|---|---|
| 2001 | 209 | 38 (25) | 18 (13) | 28 | 3 | 2 |
| 2002 | 224 | 53 (32) | 24 (16) | 13 | 2 | 4 |
| 2003 | 235 | 43 (25) | 18 (12) | 18 | 1 | 2 |
| 2004 | 243 | 59 (34) | 24 (16) | 19 | 2 | 6 |
| 2005 | 242 | 35 (23) | 14 (10) | 33 | 5 | 5 |
| 2006§ | 125 | 21 (16) | 17 (14) | 50 | 2 | 4 |
All p values as measured by a “test for trend” are greater than 0.05.
*Primary caesarean deliveries are first surgery performed. Total number of caesarean deliveries includes repeat operations.
†VBAC rate is the number of successful vaginal births after caesarean delivery divided by all women with prior caesarean deliveries.
‡Data from these two columns indicates total number of infants per year.
§At time of this report, only data from first two quarters of 2006 were available.
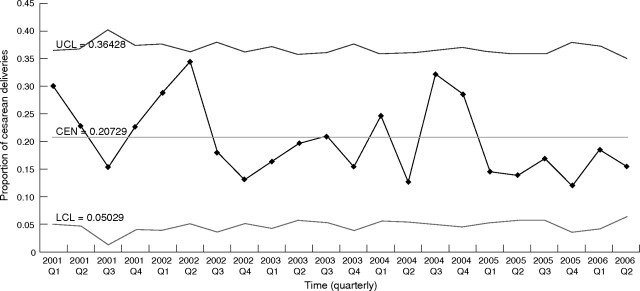
Figure 2 The p‐type control chart of caesarean delivery rate as proportion of total births by quarter (2001–6).
A total of 40 emergency caesarean deliveries have occurred during the timeframe under study which began in the Autumn of 2001 and continued through the second quarter of 2006. The decision‐to‐incision time was highly variable when the project started (fig 3). As the impact of the changes emerged, the decision‐to‐incision times became less variable (points 13–26 on fig 3) and eventually we experienced eight consecutive points below the initial mean of 30.6 minutes (points 27–34 on fig 3). This indicated a special cause within our system, so the control limits were redrawn starting with point 27. A new, stable system is seen in points 27–40 with only common cause variation and a mean decision‐to‐incision time of 20 minutes.
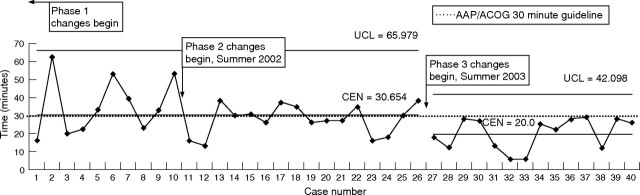
Figure 3 XmR type control chart of emergency caesarean delivery response times by consecutive case. Lower control limit is eliminated as it plots below zero. Moving R chart is not shown as there were no out‐of‐control signals.
The success of our interventions is also demonstrated by the treatment‐to‐goal ratio. As demonstrated by points 1–26 on figure 3 only 13 of the 26 emergency caesarean deliveries performed were initiated in less than 30 minutes; therefore, the original system performed at a treatment‐to‐goal ratio of 0.5. Once the new, stable system emerged, (points 27–40 on fig 3) all 14 emergency caesarean deliveries were initiated in less than 30 minutes and a treatment‐to‐goal ratio of 1.0 was achieved. Additionally, once the new system emerged, the proportion of caesarean deliveries that were classified as emergent dropped. This is demonstrated on figure 4. The control limits on this chart were split after point “04 Q2” when it became apparent that a new, stable system had emerged.
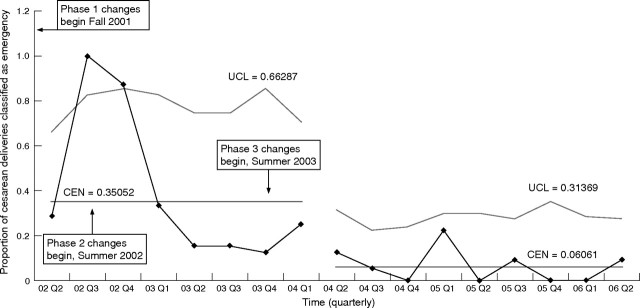
Figure 4 The p‐type control chart showing proportion of caesarean deliveries classified as emergent by quarter (2002–6). Lower control limit is eliminated as it plots below zero.
Discussion
Our results show that a small, rural, community hospital can improve caesarean delivery response times. More importantly, such improvement is sustainable over time. It is tempting to distill this project into a few key principal changes that can be readily adopted in other settings. Upon further reflection, however, it appears that the success of this project stems from the cumulative effects of multiple small changes over time. Ultimately, we were not able to identify any one change that was any more important than another. We believe that it is our change process, rather than any one of our specific changes, that is generalisable to other settings. The cornerstones of our process include a clear goal, shared leadership and teamwork.
Our project clearly illustrates the necessity of data collection coupled with “real time” feedback to the frontline workers and shows that when attempting to improve a complex process, it is reasonable to begin by working on the component parts in relative isolation. Such a strategy requires that the project leaders facilitate integration of the parts into a whole as the work progresses. As the project evolves, the independent groups will begin to work together as they come to recognise the interdependent nature of the process.
An interesting and unanticipated phenomenon that accompanied this improvement work is the decrease in the number of caesarean deliveries that are classified as emergent (fig 4). Despite this decrease, there has been no change in other markers of obstetric quality (table 2). The exact cause of this decline is unknown. Although it is possible that this trend reflects a change in the patient population, we believe that this is unlikely because our risk profile has remained constant. It is also possible that this trend reflects changing practice patterns, although this also is unlikely because the change occurred at a time when there were no significant personnel changes. We believe that this trend most likely is an indirect result of this improvement project. Specifically, it appears that our work has led to improved risk awareness/management and better communication among team members coupled with increased confidence in the process of emergency caesarean delivery. Through rational redesign of process with input from frontline personnel, we optimised the use of the resources which were available to us. Doing so allowed us to recognise that, despite its small size, APD is a resource‐rich environment.
Our process still faces challenges and our work is not yet complete. For example, we have not fully developed guidelines for caesarean delivery using only local anaesthesia. The need for this may arise if anaesthesia personnel are unavailable. Additionally, we have not optimised our process for maintenance of skills. Mock caesarean delivery drills are critical to the continuing success of this project and yet they are challenging to schedule and execute. Successful drills require a high level of coordination and cooperation. Currently we attempt to hold drills quarterly, although we do not know if this is adequate to maintain preparedness. Because we debrief extensively after these drills, they are continuously evolving as we improve our understanding of the process of emergency caesarean delivery.
While we are encouraged by our results, there are limitations to our findings. For example, early in the project, we noticed that the clocks in the operating room and the birthing centre were not synchronised; therefore, early decision‐to‐incision times lack some accuracy. Also, while we are confident in the time analysis with control charts, this project had no control group, so improvement may have occurred because of secular trends. Additionally, although our mean decision‐to‐incision time is currently 20 minutes, until the upper control limit is below 30 minutes, we do not have a system that is capable of predictably operating within the guideline (that is, points could be within the common cause variation in the new system that would be within the control limits, but above the standard time limit). Because of this, more changes may still be needed to ensure that the system will predictably produce emergency caesarean deliveries with decision‐to‐incision times of less than 30 minutes. Finally, because APD is a small, rural hospital and because emergency caesarean deliveries are now rare events, the statistical validity of our data is limited by small numbers. Despite this limitation, for the past three years our redesigned process has consistently allowed us to meet the AAP/ACOG “30 minute” guideline for emergency caesarean delivery.
The importance of this work may be questioned because a large amount of time and effort was expended to meet a guideline that is not evidence based. Recently some have challenged the usefulness of a 30 minute standard because emerging data indicate that performing a caesarean delivery within the recommended timeframe may not change perinatal outcomes.2,3,4,6,9,10,11,12 Despite this controversy, we believe that non‐academic facilities such as ours have an obligation to comply with published professional guidelines until the guideline is disproved or revised. In an effort to improve those guidelines and as a way to share knowledge of “best practices”, we encourage other facilities to begin the process of tracking and publicly reporting their emergency caesarean delivery response times. Our work demonstrates the feasibility and value of such an endeavour.
Acknowledgements
We would like to acknowledge the administration at Alice Peck Day Memorial Hospital, especially Mark Nunlist, MD and Cindy Casale. We would also like to thank Paul Batalden, MD for his comments and support and Todd MacKenzie for his assistance with statistics.
Abbreviations
AAP - American Academy of Pediatrics
ACOG - American College of Obstetricians and Gynecologists
APD - Alice Peck Day Memorial Hospital
CNM - Certified Nurse Midwife
Footnotes
This material is based upon work supported by the Office of Academic Affiliations, Department of Veterans Affairs, and used facilities at the White River Junction VA.
The opinions and findings contained herein are those of the authors and do not necessarily represent the opinions or policies of the Department of Veterans Affairs, Alice Peck Day Hospital, or Dartmouth Medical School.
References
- 1.American Academy of Pediatrics, The American College of Obstetricians and Gynecologists Guidelines for perinatal care. Fifth edition. Washington, (DC): American Academy of Pediatrics [and] The American College of Obstetricians and Gynecologists, 2002147
- 2.Nasrallah F K, Harirah H M, Vadhera R.et al The 30 minute decision‐to‐incision interval for emergency cesarean delivery: fact or fiction? Am J Perinatol 20042163–68. [DOI] [PubMed] [Google Scholar]
- 3.Mackenzie I Z, Cooke I. What is a reasonable time from decision‐to‐delivery by caesarean section? Evidence from 415 deliveries. BJOG 2002109498–504. [DOI] [PubMed] [Google Scholar]
- 4.Tuffnell D J, Wilkinson K, Beresford N. Interval between decision and delivery by caesarean section‐are current standards achievable? BMJ 20013221330–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helmy W H, Jolaoso A S, Ifaturoti O O.et al The decision‐to‐incision interval for emergency Cesarean delivery: is 30 minutes a realistic target? BJOG 2002109505–508. [DOI] [PubMed] [Google Scholar]
- 6.Chauhan S P, Magann E F, Scott J R.et al Emergency cesarean delivery for non‐reassuring fetal heart rate tracing. Compliance with ACOG guidelines. J Reprod Med 200348975–981. [PubMed] [Google Scholar]
- 7.American College of Obstetricians and Gynecologists Optimal goals for anesthesia care in obstetrics. ACOG Committee Opinion #256. American College of Obstetricians and Gynecologists, Washington (DC) 2001
- 8.Carey R G. Improving healthcare with control charts—basic and advanced SPC methods and case studies. Milwaukee, WI: American Society for Quality, 2003
- 9.Chauhan S P, Roach H, Naef RW I I.et al Cesarean delivery for suspected fetal distress. Does the decision‐incision time make a difference? J Reprod Med 199742347–352. [PubMed] [Google Scholar]
- 10.Bloom S L, Leveno K J, Spong C Y.et al Decision‐to‐incision times and maternal and infant outcomes Obstet Gynecol 20061086–11. [DOI] [PubMed] [Google Scholar]
- 11.Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ 2004328665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holcroft C J, Graham E M, Aina‐Mumuney A.et al Cord gas analysis, decision to delivery interval, and the 30‐minute rule for emergency cesareans. J Perinatol 200525229–235. [DOI] [PubMed] [Google Scholar]