Abstract
Objective
To improve influenza vaccination rates for high‐risk children and adolescents.
Methods
During the 2004–5 influenza season, 5 regional cystic fibrosis (CF) centres, 6 hospital clinics that participated in a similar initiative the previous year, 4 new hospital clinics, and 39 community‐based paediatric practices implemented a multicomponent change package consisting of nine improvement strategies designed to increase immunisation of high‐risk patients. Each site was encouraged to adopt and customise the improvement strategies to meet their specific culture and needs. The main outcome measure was the proportion of the target population immunised. Surveys sent to the community practices were summarised.
Results
The intervention targeted a total of 18 866 high‐risk children and 9374 (49.7%) received the influenza vaccination. Community‐based practices that actively participated in the collaborative reported using significantly more intervention strategies (mean (SD) 7.4 (2.3) vs 4.6 (1.5), respectively, p = 0.001) and achieved higher immunisation rates (59.3% (13.6%) vs 43.7% (20.5%), respectively, p = 0.01) than non‐participating practices. The most frequently implemented change concepts were posters in the office, walk‐in clinics or same‐day appointments and reminder phone calls. The interventions deemed most helpful were weekend or evening “flu shot only” sessions, walk‐in or same‐day appointments, reminder calls and special mailings to families.
Conclusions
Implementation of the change package, based on evidence and diffusion of innovation theory, resulted in higher immunisation rates than typically reported in the medical literature, especially for the community‐based primary care practices.
Influenza is widely recognised as a serious illness in the elderly population.1 However, influenza is also responsible for substantial morbidity in children, especially those at high risk for influenza‐related complications due to underlying chronic medical conditions such as pulmonary and cardiac disorders.2,3,4,5,6,7
Although most developed and many rapidly developing countries recommend influenza immunisation for high‐risk children,2,6,8,9,10,11 use remains low. In primary care settings in the USA, only about 10% of children with asthma receive influenza immunisation.12,13 Vaccine uptake rates of less than 10% for high‐risk children have been reported by general practices in England and Wales.14 Higher rates are reported in specialty clinics in the USA.15,16 Missed opportunities, lack of a doctor's recommendation, low perceived susceptibility, difficulty in identifying high‐risk populations and, for patients with multiple providers, confusion about whom should vaccinate, all contribute to the low immunisation rates among children with chronic medical conditions.17,18,19,20
Although many practice‐based strategies have increased immunisation rates among adults,21,22,23,24,25 fewer published studies have shown the effect of specific efforts to improve immunisation in children. However, strong evidence suggests that patient reminder/recall systems, interventions that reduce out‐of‐pocket costs or increase access, multicomponent interventions that include education, reminders to providers, and assessment and feedback interventions improve vaccination coverage in children in a range of settings and populations.13,22,26,27,28
This report describes the expanded implementation of a successful, multicomponent influenza immunisation initiative to a large number of community practices, regional cystic fibrosis (CF) centres and hospital clinics. Using diffusion of innovation theory,29 we were able to move from reaching hundreds of high‐risk patients to thousands.
Methods
Setting and organisational context
Cincinnati Children's Hospital Medical Center (CCHMC) is a large, urban paediatric academic medical centre with over 23 000 inpatient admissions and 700 000 outpatient and emergency department visits in 2005. As part of its Pursuing Perfection initiative, funded by the Robert Wood Johnson Foundation, CCHMC committed to considerable institution‐wide improvement in care processes and outcomes.30
Background
Using a series of proved immunisation strategies, the CF clinic considerably increased the proportion of patients who received the influenza vaccination during the 2001–2 and 2002–3 seasons. For the 2003–4 influenza season, these successful improvement methods were spread to six additional CCHMC clinics.31 Each clinic team was given a toolkit containing supporting literature, sample goals, communication strategies, and team member roles and processes. Suggested improvement strategies included:
increased communication, such as reminder postcards sent to all families;
access enhancements, such as influenza shot clinics;
a standard influenza order set;
a web‐based registry and tracking system to identify and follow at‐risk patients;
in‐clinic reminders to patients and healthcare providers;
pre‐planning with suppliers to order vaccine;
posting weekly results;
recall phone calls;
a designated site leader.
The teams chose which strategies to implement. Overall, 60% of 1269 high‐risk children in six CCHMC clinics were immunised. Clinic‐specific rates ranged from 33% to 93%, with the highest rate reported in the CF clinic.
Current initiative
On the basis of these successes, the innovation was scaled up to a much larger population for the 2004–5 influenza season. Participants included five Ohio regional CF centres, the six CCHMC clinics that participated in 2003–4, four more CCHMC clinics treating high‐risk children, and 39 community‐based paediatric practices in the greater Cincinnati area comprising Ohio Valley Primary Care Associates, LLC, an independent practice association. The 164 doctors associated with the community paediatric practices were also involved in a larger asthma improvement initiative launched in October 2003.
Improvement strategies
Each clinic and participating practice formed a leadership team to select improvement strategies, devise implementation plans and deal with barriers. Strategies presented to teams were grounded in the previous year's work and modified on the basis of learnings from that initiative. Planning meetings, reminder emails and conference calls kept each site involved and committed.
All of the CCHMC clinics used the web‐based patient registry, except the primary care clinic which used an electronic health record and sent its data to the influenza tracking system weekly. It did not track patients who declined immunisation. Most clinics used postcards, letters, and/or follow‐up phone calls to remind patients to receive their immunisation. Other interventions included standard order sets, open access clinics, team collaboration, preparation with the pharmacy to ensure adequate vaccination supply, and educational materials for patients and clinicians. One clinic created a reminder sticker to place on patients' charts. Another developed a packet of educational information for staff and patients. All clinics employed multiple strategies.
The Ohio CF centres used the same influenza‐specific patient registry. In addition, each centre received a change package that included literature, a poster for displaying results, and a customisable reminder postcard.
Tracking influenza vaccination was required for community practices as part of the larger asthma improvement effort. However, active participation in the influenza improvement collaborative was voluntary. The practices that chose to be actively involved received additional follow‐up and support in the form of facilitated problem solving and sponsored conference calls. Data collection was facilitated by a centralised asthma patient registry. In addition, the asthma pay‐for‐performance programme with the region's largest commercial payor included rewards linked to network and practice‐level influenza immunisation results, with the network having to first meet a designated threshold before individual practices could be rewarded.
Outcome measures and data collection
The main outcome was the proportion of the target population immunised. Although the methods used to determine the target population varied somewhat between the participating practices, in general, patients were identified from billing records or from clinic lists that included patients seen within the past 1 or 2 years. CCHMC clinics (except the primary care clinic) and the CF centres recorded information on the date the immunisation was received or declined and the location where it was received (study site, inpatient setting, primary care office, open access clinic, other or unspecified) in their registries. The CF centres de‐identified their data before forwarding it to CCHMC. Graphs showing the number of patients immunised were updated weekly and made available via the tracking system.
Following the initiative, project leaders in the community practices completed an 11‐item web‐based survey (available from the authors on request) to evaluate intervention implementation and to identify barriers experienced. Respondents listed improvement strategies used and rated their helpfulness. Multiple reminder calls were made to non‐respondents.
Data analysis
To determine the rate of immunisation and the percentage of patients who declined immunisation, we extracted data from the registries maintained at CCHMC. For the 39 community‐based practices, exploratory analyses of factors associated with immunisation were undertaken at the practice level. Potential practice‐based predictors of the immunisation rate included the number of doctors in the practice, the number of active patients and the proportion of patients with asthma. The main outcome measure was the proportion of patients with asthma in the practice who were immunised. We used t tests to examine bivariate associations, and variables significantly associated with immunisation at the p = 0.1 level were entered into a stepwise linear regression model.
Human subject protection
The initiative was undertaken primarily for the purpose of quality improvement. The CCHMC institutional review board reviewed the intervention and analysis plans and waived the requirement for written informed consent, provided no individuals were identified.
Results
Characteristics of the practices and clinics are shown in table 1. The intervention targeted 18 866 high‐risk children and 9374 (49.7%) were immunised. Overall, the CF centres achieved the highest rate of immunisation (786/957, 82.1%), followed by the hospital clinics that had participated previously (714/1072, 66.6%), the community‐based practices (5503/10749, 51.2%) and the hospital clinics participating for the first time (2371/6088, 38.9%). A small proportion of patients, ranging from 0 to 12% per clinic, declined immunisation.
Table 1 Characteristics of participating practices and clinics.
| Participant | Target condition | Population size | Patients immunised, % | Patients declining immunisation, % |
|---|---|---|---|---|
| Ohio regional CF centres (n = 5) | Cystic fibrosis | 957 | 82.2 (SD 13.9) (range among clinics 62.0–95.5) | 1.8 |
| Experienced CCHMC clinics (involved in the 2003–2004 initiative) | ||||
| Teen health | Asthma, diabetes, sickle cell disease | 424 | 67.9 | 3.1 |
| Cardiology | Hypoplastic left heart | 27 | 100 | 0 |
| High‐risk infants | Bronchopulmonary dysplasia | 257 | 74.7 | 1.6 |
| Gastroenterology | Liver transplant | 219 | 35.3 | 0.5 |
| Nephrology | Renal failure | 103 | 96.1 | 1.9 |
| Pulmonary | Ventilator dependent | 42 | 73.8 | 9.5 |
| New CCHMC clinics | ||||
| Nutrition | Chronic parenteral/enteral feeds | 41 | 87.8 | 12.2 |
| Diabetes | Diabetes | 1364 | 66.3 | 7.1 |
| Rheumatology | Juvenile rheumatoid arthritis with immunosuppressive medication | 202 | 62.9 | 1.0 |
| Pediatric primary care | Asthma and children 6–23 months of age | 4481 | 29.1 | Not consistently recorded |
| Ohio Valley Primary Care Associates (39 community‐based paediatric practices) | Asthma | 10 749 | 52.5 (SD 18.4) (range among clinics 15.5–92.3) | Not consistently recorded |
CCHMC, Cincinnati Children's Hospital Medical Center.
Within the hospital, the clinics varied in size, and two of the new clinics (diabetes and primary care) were substantially larger than any of the experienced clinics. When we compared the average rate of immunisation in the new and the experienced clinics, the experienced clinics were 14% higher than the new ones (74.6% and 61.5%, respectively). Although clinically large, this difference was not statistically significant (t = 0.86, p = 0.21), probably due to the small number of clinics being compared.
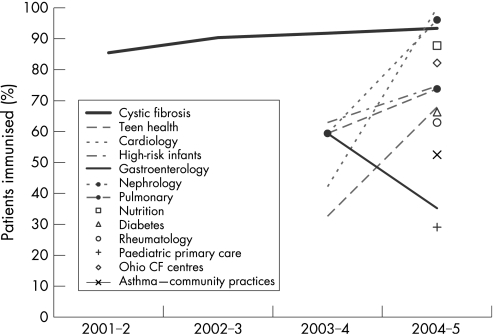
The clinic with the most experience with the change strategies, the CF clinic at CCHMC, continued to improve (fig 1). In addition, five of the six experienced clinics increased their immunisation rates over those observed during the previous influenza season.
Figure 1 Change in immunisation rates over time for participating clinics and practices.
Of the 39 community‐based practices, 22 actively participated in the collaborative by participating in follow‐up conference calls and adopting interventions from the change package. Twenty of 22 actively participating practices and 12 of 17 non‐participating practices completed the web‐based survey administered following the initiative (table 2). The most frequently implemented change concepts were posters in the office, walk‐in clinics or same‐day appointments and reminder phone calls. The interventions deemed most helpful were weekend or evening “flu shot only” sessions, walk‐in or same‐day appointments, reminder calls and special mailings to families. Thirteen practices developed additional strategies, including partnering with a local hospital to track influenza vaccine administration, pre‐booking appointments for high‐risk children and placing stickers on patient charts as a visual reminder to immunise.
Table 2 Interventions used by the community‐based practices (n = 32).
| Improvement strategy | Practices that used the strategy, % | Practices that rated the strategy as very helpful or extremely helpful, % |
|---|---|---|
| Posters in the office | 82 | 33 |
| Open access (walk‐in or same day) flu shot availability | 82 | 78 |
| Reminder calls to patients not immunised after a target date | 73 | 67 |
| Practice‐based team meetings | 64 | 48 |
| Weekend/evening “flu shot only” sessions | 58 | 84 |
| Reminder postcards mailed to families | 53 | 47 |
| Special mailings to families (eg, newsletter) | 36 | 66 |
| Posting results of immunisation project in office | 24 | 37 |
| “On‐hold” telephone message with flu shot reminder | 21 | 42 |
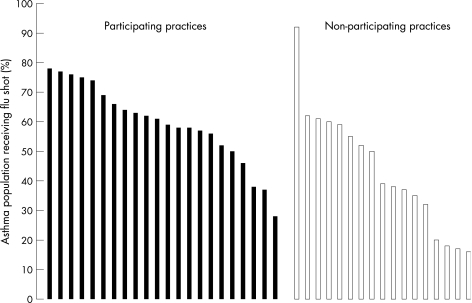
Practices participating in the collaborative (table 3) had a larger proportion of asthma patients in their practice and used significantly more interventions than non‐participating practices (mean (SD) 7.4 (2.3) and 4.6 (1.5), respectively, p = 0.001). Although variation was seen in the proportion of patients that received influenza immunisation (fig 2), overall, practices that actively participated reported higher immunisation rates than non‐participating practices (59.3% (13.6%) and 43.7% (20.5%), respectively, p = 0.01). Univariate and multivariable analyses revealed no significant associations between practice characteristics or the number of spread strategies employed and the proportion of patients with asthma immunised.
Table 3 Characteristics of community‐based paediatric practices actively participating in the collaborative compared with non‐participating practices.
| Characteristic | Participating practice | Non‐participating practice | p Value |
|---|---|---|---|
| Number | 22 | 17 | |
| Mean (SD) number of doctors | 4.0 (2.6) | 3.3 (2.8) | 0.47 |
| Mean (SD) patients per practice | 5891 (4354) | 5425 (4519) | 0.75 |
| Mean (SD) asthma prevalence | 6.5 (4.7) | 3.8 (3.1) | 0.045 |
Figure 2 Immunisation by community‐based paediatric practices actively participating in the collaborative and non‐participating practices.
Diffusion of innovation strategies were used to enhance adoption of interventions; table 4 shows an example involving the community practices.
Table 4 How diffusion of innovation characteristics29 were used to enhance adoption of interventions.
| Diffusion of innovation characteristics | Methods used to strengthen the characteristic |
|---|---|
| Relative advantage | • Financial incentive from larger asthma improvement initiative tied to immunisation rate achieved by network and individual practices |
| • Peer recognition by communicating results of high performing practices in the network | |
| Compatibility | • Reinforced extensive primary care experience administering vaccines |
| • Customised communications to families and practice teams regarding importance of immunisation for children with asthma (eg, posters, newsletters, “on hold” message, flu shot postcard) | |
| Complexity | • Refined previously developed “change package” to fit the practice setting |
| • Assisted in coordination of postcard mailing | |
| • Acknowledged additional work required and reinforced prior experience that it “gets easier every season” | |
| Trialability | • No additional strategies required since this initiative strongly met trialability characteristic |
| Observability | • Graph of influenza immunisation percentage, by week |
| • Waiting room poster with visual of current results | |
| • Patient lists with names of patients who have not yet received the vaccine | |
| • Transparent, comparative practice results |
Discussion
Half (50%) of the high‐risk children targeted by the intervention received the influenza vaccination. The CF centres achieved the highest influenza immunisation rates, followed by the clinics involved in a similar project during the 2003–4 influenza season.31 Although the average immunisation rate for the experienced clinics was 14% higher than for the new clinics, this difference was not statistically significant. All but one of the experienced CCHMC clinics improved their immunisation rates over the previous year. The lowest immunisation rates were observed for primary care practices, both community and hospital based.
The higher immunisation rates observed for subspecialty clinics and lower rates for primary care practices mirror those found in the literature. Kramarz et al12 reported influenza immunisation rates of 9–10% for children with asthma in a primary care setting, and Marshall et al16 reported that 79% of children with CF were vaccinated at a regional CF centre. Children in subspecialty care may be perceived, by providers and parents, to have more severe illness and be more at risk. Thus, parents or providers may believe influenza immunisation to be more important. Also, subspecialty settings may have more resources to devote to immunisation campaigns, compared with primary care locations. On the other hand, one would expect primary care practices to have a strong immunisation infrastructure in place, given their large role in routine preventive care.
The high degree of variation in influenza immunisation among the community‐based paediatric practices may have been due to differences in:
practice infrastructure (eg, single vs multiple providers, appointment access/office hours, electronic vs paper records, number of practice sites, payor mix, staffing and financial resources);
visible commitment of doctor leadership/doctor champion;
vaccine supply;
awareness of the interventions;
ability to implement/execute interventions;
reliability of internal processes to reduce missed opportunities;
past experience communicating the importance of immunisation to parents;
extent of efforts to address issues underlying parents' decision to decline immunisation;
use of performance data and reports available from the registry.
Future plans include conducting formal assessments of high‐performing practices to better understand key success factors, providing high‐performing practices with opportunities to communicate their experience to others, further refining the change package and registry reporting tools on the basis of feedback from practices, improving the reliability of workflow processes to reduced missed opportunities, and obtaining further knowledge of factors underlying why parents decline the immunisation.
The change package was built on best available evidence regarding interventions to improve vaccination rates for children and adults, such as reminder/recall programmes, patient registries and expanded hours of availability.22 Reminder/recall methods increased influenza immunisation rates to approximately 30% at two paediatric clinics at academic centres13,26 and to 42% at four private paediatric practices.27 However, these results are still far below the target goal of complete immunisation of high‐risk children. Zimmerman et al recently reported success, increasing the influenza vaccination rates of patients 6–23 months of age in five inner‐city health centres serving low‐income children by implementing a set of patient, provider and system‐level interventions,32 similar to the ones used in our study. Immunisation rates for this population were 5% at baseline, 25% after the first year and 37% after the second year.
The proved strategies used in our collaborative were tailored to facilitate adoption using the five critical elements of innovation outlined in Rogers' diffusion of innovation theory: relative advantage, compatibility, complexity, trialability and observability.29 We worked with teams to ease implementation and reduce barriers, allowed clinics and practices to adopt and modify interventions to best fit their needs and situations, and made results visible to reward success and reinforce sustainability.
Our experience during the 2003–4 influenza season suggests that teams new to the intervention require considerable assistance.31 The difference in outcomes between new and experienced hospital teams may reflect the benefits of experience or a need for additional support for new teams. It is not clear whether intense coaching to promote year‐one success or allowing teams to learn independently to promote ownership is the best long‐term strategy. Future studies could randomise practices to different levels of support and coaching.
We did not systematically assess why some community‐based practices actively participated in the collaborative and others did not. However, practices actively involved used considerably more change strategies and had markedly higher immunisation rates. This may reflect greater belief in the value of influenza immunisation or more practice resources available for the project. It may also reflect the need for redundancy to create reliable care systems.33
This study was conducted within a quality improvement framework. Data on the number of interventions used and immunisation rate were self‐reported and were not audited. Although it is possible that practices over‐reported their rates, it is unlikely, since rates were based on a population‐based registry. Recording errors are unlikely to be systematic. As there were patients for whom immunisation status remained unknown, it is possible that the immunisation rate for some practices was underestimated.
Because we had baseline data only for the experienced clinics, we could not determine if immunisation rates were improved in the new clinics over the previous influenza season. The results for most clinics and practices, however, were much higher than those previously reported in the literature. It is unclear if media reports of vaccine shortage for the 2004–5 season influenced immunisation rates. Data on patient health insurance coverage were available for only a minority of the population. Thus, we could not investigate the impact of patient insurance status on immunisation rates. We also did not have any data on the cost or cost‐effectiveness of the project. Finally, the analyses of factors potentially associated with higher immunisation rates in the practices should be considered exploratory. This was not the main focus of the project and the analyses were post‐hoc. Even though 39 practices and over 10 000 patients were involved, statistical power to detect associations was limited in these practice‐level analyses. Patient‐level analyses would have been inappropriate in this case, since interventions were undertaken at the practice level.
In addition, we only have counts of the number of interventions each practice implemented. The relative impact and synergy among interventions was not assessed. Additional research involving more practices and a factorial design will probably be required to determine which interventions are most effective. Although the relative impact of financially rewarding practices for achieving network and practice‐specific influenza immunisation targets cannot be discerned, we acknowledge that the pay‐for‐performance programme was a major motivating factor for practices to pursue improvement efforts.
Summary
Implementation of the change package resulted in higher immunisation rates than reported in the medical literature, especially for the community‐based primary care practices. The CF clinics were also particularly successful, possibly because the patients were perceived to be at higher risk. Experience with the innovations appears to be useful, as shown by the higher rates of immunisation reported by clinics involved for the second year.
Acknowledgements
The authors would like to thank Connie Meeks, Amy Anneken, Uma Kotagal, and the clinicians and staff of all the participating clinics and practices for their help in completing this project.
Abbreviations
CCHMC - Cincinnati Children's Hospital Medical Center
CF - cystic fibrosis
Footnotes
Funding: This work was funded, in part, by grants from the Robert Wood Johnson Foundation and the National Association of Pediatric Nurse Practitioners. These funding sources had no involvement in the study design, collection, analysis or interpretation of the data, writing of the report or decision to submit this paper for publication.
Competing interests: None.
References
- 1.Fleming D M, Elliot A J. The impact of influenza on the health and health care utilisation of elderly people. Vaccine. 2005;23(Suppl 1)S1–S9. [DOI] [PubMed]
- 2.Harper S A, Fukuda K, Uyeki T M.et al Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005541–40. [PubMed] [Google Scholar]
- 3.Neuzil K M, Mellen B G, Wright P F.et al The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med 2000342225–231. [DOI] [PubMed] [Google Scholar]
- 4.Neuzil K M, Wright P F, Mitchel E F., Jret al The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr 2000137856–864. [DOI] [PubMed] [Google Scholar]
- 5.Izurieta H S, Thompson W W, Kramarz P.et al Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 2000342232–239. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics Committee on Infectious Diseases Recommendations for influenza immunization of children. Pediatrics 20041131141–1147.15060211 [Google Scholar]
- 7.Loughlin J, Poulios N, Napalkov P.et al A study of influenza and influenza‐related complications among children in a large US health insurance plan database. Pharmacoeconomics 200321273–283. [DOI] [PubMed] [Google Scholar]
- 8.Zimmerman R K, Middleton D B. Vaccines for persons at high risk due to medical conditions, occupation, environment, or lifestyle, 2005. J Fam Pract 200554S27–S36. [PubMed] [Google Scholar]
- 9.Heininger U. An update on the prevention of influenza in children and adolescents. Eur J Pediatr 2003162828–836. [DOI] [PubMed] [Google Scholar]
- 10.van Essen G A, Palache A M, Forleo E.et al Influenza vaccination in 2000: recommendations and vaccine use in 50 developed and rapidly developing countries. Vaccine 2003211780–1785. [DOI] [PubMed] [Google Scholar]
- 11.Macroepidemiology of Influenza Vaccination (MIV) Study Group The macroepidemiology of influenza vaccination in 56 countries, 1997–2003. Vaccine 2005235133–5143. [DOI] [PubMed] [Google Scholar]
- 12.Kramarz P, DeStefano F, Gargiullo P M.et al Influenza vaccination in children with asthma in health maintenance organizations. Vaccine Safety Datalink Team. Vaccine 2000182288–2294. [DOI] [PubMed] [Google Scholar]
- 13.Szilagyi P G, Rodewald L E, Savageau J.et al Improving influenza vaccination rates in children with asthma: a test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics 199290871–875. [PubMed] [Google Scholar]
- 14.Joseph C, Goddard N, Gelb D. Influenza vaccine uptake and distribution in England and Wales using data from the General Practice Research Database, 1989/90–2003/4. J Public Health (Oxf) 200527371–377. [DOI] [PubMed] [Google Scholar]
- 15.Chung E K, Casey R, Pinto‐Martin J A.et al Routine and influenza vaccination rates in children with asthma. Ann Allergy Asthma Immunol 199880318–322. [DOI] [PubMed] [Google Scholar]
- 16.Marshall B C, Henshaw C, Evans D A.et al Influenza vaccination coverage level at a cystic fibrosis center. Pediatrics 2002109E80–0. [DOI] [PubMed] [Google Scholar]
- 17.Daley M F, Beaty B L, Barrow J.et al Missed opportunities for influenza vaccination in children with chronic medical conditions. Arch Pediatr Adolesc Med 2005159986–991. [DOI] [PubMed] [Google Scholar]
- 18.Rickert D, Santoli J, Shefer A.et al Influenza vaccination of high‐risk children. What the providers say. Am J Prev Med 200630111–118. [DOI] [PubMed] [Google Scholar]
- 19.Grant V J, Le Saux N, Plint A C.et al Factors influencing childhood influenza immunization. CMAJ 200316839–41. [PMC free article] [PubMed] [Google Scholar]
- 20.Esposito S, Marchisio P, Droghetti R.et al Influenza vaccination coverage among children with high‐risk medical conditions. Vaccine 2006245251–5255. [DOI] [PubMed] [Google Scholar]
- 21.Ndiaye S M, Hopkins D P, Shefer A M.et al Interventions to improve influenza, pneumococcal, and hepatitis B vaccination coverage among high‐risk adults: a systematic review. Am J Prev Med 200528248–279. [DOI] [PubMed] [Google Scholar]
- 22.Briss P A, Rodewald L E, Hinman A R.et al Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Task Force on Community Preventive Services. Am J Prev Med 20001897–140. [DOI] [PubMed] [Google Scholar]
- 23.Stone E G, Morton S C, Hulscher M E.et al Interventions that increase use of adult immunization and cancer screening services: a meta‐analysis. Ann Intern Med 2002136641–651. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman R K, Nowalk M P, Raymund M.et al Tailored interventions to increase influenza vaccination in neighborhood health centers serving the disadvantaged. Am J Public Health 2003931699–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hull S, Hagdrup N, Hart B.et al Boosting uptake of influenza immunisation: a randomized controlled trial of telephone appointing in general practice. Br J Gen Pract 200252712–716. [PMC free article] [PubMed] [Google Scholar]
- 26.Gaglani M, Riggs R, Kamenicky C.et al A computerized reminder strategy is effective for annual influenza immunization of children with asthma or reactive airway disease. Pediatr Infect Dis J 2001201155–1160. [DOI] [PubMed] [Google Scholar]
- 27.Daley M F, Barrow J, Pearson K.et al Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics 2004113e26–e33. [DOI] [PubMed] [Google Scholar]
- 28.Jacobson V J, Szilagyi P G. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev 2005CD003941. [DOI] [PMC free article] [PubMed]
- 29.Rogers E M.Diffusion of innovations. 4th edn. New York, NY: Free Press, 1995
- 30.Britto M T, Anderson J M, Kent W M.et al Cincinnati Children's Hospital Medical Center: transforming care for children and families. Jt Comm J Qual Patient Saf 200632541–548. [DOI] [PubMed] [Google Scholar]
- 31.Britto M T, Pandzik G M, Meeks C S.et al Combining evidence and diffusion of innovation theory to enhance influenza immunization. Jt Comm J Qual Patient Saf 200638426–432. [DOI] [PubMed] [Google Scholar]
- 32.Zimmerman R K, Nowalk M P, Lin C J.et al Interventions over 2 years to increase influenza vaccination of children aged 6–23 months in inner‐city family health centers. Vaccine 2006241523–1529. [DOI] [PubMed] [Google Scholar]
- 33.Luria J W, Muething S E, Schoettker P J.et al Reliability science and patient safety. Pediatr Clin North Am 2006531121–1133. [DOI] [PubMed] [Google Scholar]