Abstract
Objective
Depression is commonly seen, but infrequently adequately treated, in primary care clinics. Improving access to depression care in primary care clinics has improved outcomes in clinical trials; however, these interventions are largely unstudied in clinical settings. This study examined the effectiveness of a quality improvement project improving access to mental healthcare in a large primary care clinic.
Methods
A before–after study evaluating the efficacy of the integration of a primary mental healthcare (PMHC) clinic into a large primary care clinic at the White River Junction, Vermont Veterans Affairs Medical Center (VAMC). In the before period (2003), a traditional referral and schedule model was used to access mental healthcare services. Patients who had screened positive for depression using a depression screen for 6 months after entry into either model were retrospectively followed. VA clinics without a PMHC were used as a control. The proportion of patients who received any depression treatment and guideline‐adhering depression treatment in each model was compared, as well as the volume of patients seen in mental health clinics and the wait time to be seen by mental health personnel.
Results
383 and 287 patients screened positive for depression at VAMC and the community‐based outreach clinic, respectively. Demographics of the before and after cohorts did not differ. The PMHC model was associated with a greater proportion of patients who had screened positive for depression obtaining some depression treatment (52.3% vs 37.8%; p<0.001), an increase in guideline‐adherent depression treatment for depression (11% vs 1%; p<0.001).
Conclusions
Implementation of the PMHC model was associated with more rapid and improved treatment for depression in the population of patients who screened positive for depression. More widespread implementation of this model should be investigated.
Depression is the second most commonly seen disorder in primary care settings, accounting for one of every eight visits.1,2 Although the condition is common in primary care settings, the diagnosis and treatment of depression is often suboptimal.3,4 Several studies have redesigned primary care clinics in an effort to optimise treatment for patients with depression. It has been found that integrating mental health services into a primary care clinic can improve access and outcomes for patients with depression,5,6 as well as the quality of treatment for depression.7 Adding care management for depressed patients treated in primary care has improved outcomes when used either alone or with other interventions.8,9
There is little evidence that these practices are being adopted into clinical practice, in part because there has been limited evaluation of the implementation of recommended changes into clinical settings.10 Therefore, we report the results of a quality improvement project that used a model of mental health services delivery which was integrated into a primary care setting to improve the quality and timeliness of depression treatment of depression found in a primary care setting.
Method
We followed an approach developed for the publication of quality improvement research.11 The project was approved by Dartmouth Medical School's Committee for the Protection of Human Subjects, Hanover, New Hampshire, USA (CPHS No. 17305).
Setting
This quality improvement project was conducted in the primary care and mental healthcare clinics at White River Junction Veterans Affairs Medical Center (VAMC) in White River Junction, Vermont, and its associated community‐based outreach clinics.
Function
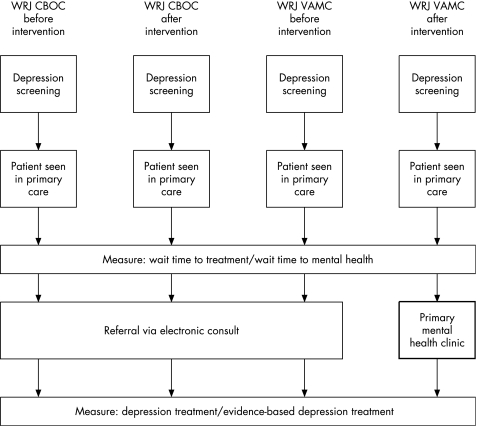
The project focused on improving the referral methods and patient transitions between these clinics. To evaluate effectiveness of the model, we used two comparison groups: a before period at the White River Junction VAMC as well as a contemporaneous evaluation of the community‐based outreach clinics in both the before and after periods. The design allowed for comparison of four groups (fig 1). During both periods, all VA patients were screened for depression in primary care clinics using a common, electronically implemented two‐question screening instrument.12 Group members were identified by having a positive depression screen—defined as a single positive answer on the two‐question depression screening instrument—in August or September of either 2003 (before) or 2004 (after).13 We limited our analysis to this time period because of administrative changes that occurred after this time period, which could have potentially influenced results obtained in later periods. More than 95% of eligible patients were screened during these months.
Figure 1 Design of the quality improvement project. CBOCs, community‐based outreach clinics; VAMC, Veteran Affairs Medical Center; WRJ, White River Junction.
In the before observation period at White River Junction and in both years at the community‐based outreach clinics, patients screening positive for depression in the primary care clinics received treatment as usual for their depression. In treatment as usual, the primary care doctor further evaluated patients for the diagnosis of depression, and either treated them or referred them to the mental health service by use of an electronic consult.
Intervention
In July 2004, the mental health service at the White River Junction VAMC opened the primary mental healthcare (PMHC) clinic which had been developed by the department over the preceding 18‐month period using evidence‐based models for treatment of depression in primary care clinics. The clinic had three central features:
mental health services co‐located in the primary care clinic working collaboratively with primary care staff14;
advanced or open access to mental health providers in the primary mental health clinic3;
use of common, standardised assessment instruments for depression and other mental health conditions.15
The clinic won a 2005 American Psychiatric Association Gold Award for excellence in health services delivery.16
The PMHC at the White River Junction VAMC is located at the primary care clinic. It operates from 08:00 h to 17:00 h Monday to Friday. The week is divided into 10 half‐day shifts. Each shift is staff by a therapist (either masters or doctoral level) and a psychiatrist. Patients arriving at the clinic receive standardised rating scales including the post‐traumatic stress disorder (PTSD) clinician checklist, Beck Depression Inventory and State/Trait Anxiety Scale. The patient then sees the therapist, who takes a psychosocial history, and then a psychiatrist who takes a medical and disease state history. The therapist, psychiatrist, and patient then meet to arrive at a treatment plan. The PMHC clinic is staffed with existing mental health staff and no staff were added when the clinic opened. The only start‐up cost was that associated with the electronic forms of mental health rating scales.
Measures
We identified all patients who screened positive for depression at White River Junction and all White River Junction VA‐affiliated community‐based outreach clinics during both time periods. We retrospectively reviewed all medical records, including pharmacy and appointment data, for 6 months after the patient screened positive for depression. We collected patient demographics and three measures for each patient group. First, we categorically determined whether each patient received optimal, guideline defined depression treatment (table 1). Optimal treatment was defined as meeting all four criteria in table 1. Second, we determined whether each patient obtained any part of the guideline defined treatment. Lastly, for each patient we collected information on access to treatment, defined as the number of days between screening positive and completing a mental health appointment. For comparison purposes, we grouped patients into those who completed a mental healthcare appointment in less than each of 4, 30, and 90 days, and more than 90 days.
Table 1 Guidelines for optimal care of depression.
| (1) | Treatment is started within 72 h of a positive depression screen |
| (2) | Antidepressant prescribed at an adequate dose as defined by the Antidepressant Treatment History Form17 or 10‐weekly psychotherapy sessions18 |
| (3) | There must be at least three contacts with the patient within 60 days19,20 |
| (4) | The patient must have continued on any depression treatment for at least 90 days20 |
To evaluate the effectiveness of the intervention, we used the χ2 test to compare categorical variables and the Student t test to compare continuous variables among the four groups. We hypothesised that we would find no differences over time for the community‐based outreach clinic groups, in which no intervention occurred, but that the quality and access of care provided in the White River Junction VAMC clinics would improve after the intervention.
Results
In the before period, 320 patients screened positive for depression by answering “yes” to either of the screening questions. Of those 320 patients, 186 (58%) received care at the White River Junction VAMC and 134 received care at an affiliated community‐based outreach clinic. Similarly, in the period after the intervention started, 350 patients screened positive for depression by answering “yes” to either of the screening questions. Of those 350 patients, 197 (56%) received their care at the White River Junction VAMC and 153 received their care at a community‐based outreach clinic. Overall, patients were primarily male (87%) and white (97%). Comparing 2004 to 2003, there were no differences in age, gender, or race for either the White River Junction VAMC or the outreach clinic; however, for both years the patients seen in White River Junction were older than those seen at the outreach clinic (table 2).
Table 2 Demographic characteristics of the study population.
| Community‐based outreach clinic | White River Junction VAMC | |||
|---|---|---|---|---|
| Before (treatment as usual) | After (treatment as usual) | Before (treatment as usual) | After (PHMC) | |
| Screened with depression | 134 | 153 | 186 | 197 |
| Mean (SD) age | 61.8* (13.1) | 62.4* (12.4) | 68.1* (11.1) | 69.2* (6.8) |
| Male, % (n) | 87 (117) | 90 (138) | 86 (160) | 88 (173) |
| White, % (n) | 97 (130) | 96 (147) | 98 (182) | 98 (193) |
PMHC, primary mental healthcare (clinic).
*p<0.05 for comparison of White River Junction and community‐based outreach clinic mean age.
The introduction of the PMHC model was associated with many changes in the treatment of patients with a positive screen for depression at the White River Junction VAMC that were not reflected in the treatment at community‐based outreach clinics. First, significantly more patients who screened positive for depression received any depression treatment (52.3% vs 37.8%, respectively; p<0.001) and optimal depression treatment (11.2% vs 1.1%, respectively; p<0.001) (table 3).
Table 3 Comparison of treatment for depression in the PMHC model of care and treatment as usual.
| Community‐based outreach clinic | White River Junction VAMC | |||
|---|---|---|---|---|
| Before (treatment as usual) | After (treatment as usual) | Before (treatment as usual) | After (PMHC) | |
| Any treatment, % (n) | 35.1 (47) | 35.3 (54) | 37.8 (70) | 52.3** (103) |
| Optimal treatment, % (n) | 3.0 (4) | 0.7 (1) | 1.1 (2) | 11.2** (22) |
| Seen in mental health, % (n) | 3.0 (4) | 5.9 (9) | 9.0 (16) | 36.03** (71) |
| Time to appointment for those seen in mental health | ||||
| <4 days, % (n) | 0 (0) | 0 (0) | 5.9 (4) | 67.63** (70) |
| <30 days, % (n) | 50 (23) | 33.3 (18) | 17.6 (12) | 80.33** (83) |
| >90 days, % (n) | 0 (0) | 33.3 (18) | 17.6 (12) | 5.63** (3) |
PMHC, primary mental healthcare (clinic).
*p<0.05 in χ2 comparison of White River Junction VA Medical Center (VAMC) before vs after.
**p<0.001 in χ2 comparison of White River Junction VAMC before vs after.
Importantly, after implementation of the PMHC, fewer patients who screened positive for depression received no depression treatment (94 (47.7%) vs 115 (62.2%)). None of these measures of depression treatment quality changed over time at the community‐based outreach clinics, and the measures did not differ in the before period when comparing the outreach clinics with the White River Junction VAMC.
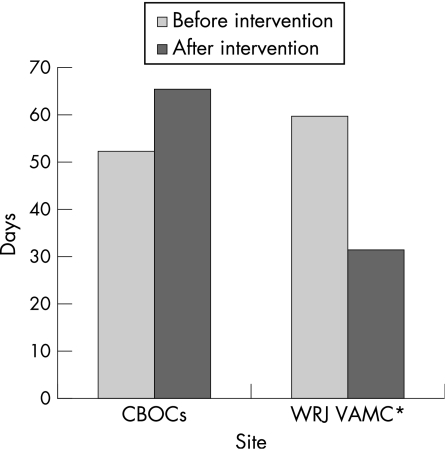
After implementation of the PMHC, access to mental health services improved. Substantially more patients who screened positive were seen in the mental health clinic (36.03% vs 9%; p<0.001), and a much greater proportion of patients were seen in mental health sooner (table 3, bottom). At the White River Junction VAMC, mean (SD) wait times decreased from 59.8 (24.2) to 31.3 (17.8) days (p<0.05) whereas at the community‐based outreach clinics mean wait times increased from 52 (22.3) to 65 (23.4) days (fig 2).
Figure 2 Wait times to mental healthcare treatment before and after primary mental healthcare (PHMC) implementation. *p<0.05 in t test comparing White River Junction VA Medical Center (VAMC) 2004 vs 2003. CBOC, community‐based outreach clinic.
Conclusion
In this before–after study with a contemporaneous control site, we found that the introduction of the PMHC clinic that used an evidence‐based design was associated with significant improvements in the quality of care for patients who screened positive for depression. Some of this improvement appeared to be facilitated by improved access to mental healthcare professionals. The improvement that we found did not seem to be the result of a secular improvement trend, as evidenced by the lack of improvement in quality of care, and worsening of improvement in access to care, at the community‐based outreach clinics during the same time period.
Our findings suggest that the implementation of an integrated mental health clinic within a primary care setting is an effective way to improve the quality of and access to mental healthcare in non‐research settings. However, the findings also suggest that mere implementation of a new model of care will not achieve ideal results: although the intervention increased the use of guideline‐based care and improved access to mental health services, nearly half of the patients who screened positive for depression still received no treatment after intervention. A first impression suggests that this level of improvement is inadequate. However, two other sources of data help interpret this level of improvement. First, the specificity and predictive value positive of the two‐question screening instrument are 74.7% and 38.3%, respectively.21 Second, studies offering treatment to similar patients screened for depression in primary care have shown that 20–29% will decline treatment.5,14 Therefore, the highest quality care that an intervention might achieve is to treat about 50–72% of patients who have an initial positive depression screen. Therefore, the improvement made with our intervention, although not perfect, represented a substantial gain towards an achievable benchmark.
There are several important limitations of our study. First, our design did not allow us to randomise patients into the different treatment modalities; therefore, we cannot rule out the possibility that the improvements we found resulted from factors not related to the changes that occurred in clinical services under the PMHC model. However, the stability of results from care provided at the community‐based outreach clinics during the same time period suggests that the new model was a substantial contributor to the observed improvements. Second, this trial examined only 2 months in each model of care. A longer period of observation would increase the reliability of these results. Finally, the study was conducted in a single VA Medical Center and its affiliated community‐based outreach clinics—the service population is largely white, male, and rural. Results might not be generalisable to dissimilar settings.
Nevertheless, our study suggests that a structural change that integrates mental healthcare and primary healthcare can result in improve access to mental healthcare professionals and the quality of mental healthcare services provided: a structural change improved process of care measures. More research is needed to explore how well these models work in other primary care clinical settings and to identify critical factors for successful implementation.
Abbreviations
PMHC - primary mental healthcare (clinic)
VAMC - Veterans Affairs Medical Center
Footnotes
Funding: This work was supported in part by VA Health Services Research and Development Grant REAP 03‐098.
Competing interests: None declared.
The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs or of the United States government. BW had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Spitzer R L, Kroenke K, Linzer M.et al Health‐related quality of life in primary care patients with mental disorders. Results from the PRIME‐MD 1000 Study. JAMA 19952741511–1517. [PubMed] [Google Scholar]
- 2.Kirchner J E C G, Aikens J. Datapoints: Detecting depression in VA primary care clinics. Psychiatric Serv 200455350. [DOI] [PubMed] [Google Scholar]
- 3.Solberg L I, Korsen N, Oxman T E.et al The need for a system in the care of depression. J Fam Pract 199948973–979. [PubMed] [Google Scholar]
- 4.Stettin G D, Yao J, Verbrugge R R.et al Frequency of follow‐up care for adult and pediatric patients during initiation of antidepressant therapy. Am J Manag Care 200612453–461. [PubMed] [Google Scholar]
- 5.Bartels S J, Coakley E H, Zubritsky C.et al Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at‐risk alcohol use. Am J Psychiatry 20041611455–1462. [DOI] [PubMed] [Google Scholar]
- 6.Pincus H A P C, Keyser D, Bachman J.et al Depression in primary care: learning lessons in a national quality improvement program. Adm Policy Ment Health 2006332–15. [DOI] [PubMed] [Google Scholar]
- 7.Solberg L I, Crain A L, Sperl‐Hillen J M.et al Effect of improved primary care access on quality of depression care. Ann Fam Med 2006469–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruce M L, Ten Have T R, Reynolds C F., 3rdet al Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA 20042911081–1091. [DOI] [PubMed] [Google Scholar]
- 9.Oxman T E, Dietrich A J, Schulberg H C. Evidence‐based models of integrated management of depression in primary care. Psychiatr Clin North Am 2005281061–1077. [DOI] [PubMed] [Google Scholar]
- 10.Hogan M F. The President's New Freedom Commission: recommendations to transform mental health care in America. Psychiatr Serv 2003541467–1474. [DOI] [PubMed] [Google Scholar]
- 11.Davidoff F, Batalden P. Toward stronger evidence on quality improvement. Draft publication guidelines: the beginning of a consensus project, Qual Saf Health Care 200514319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whooley M A, Avins A L, Miranda J.et al Case‐finding instruments for depression: Two questions are as good as many. J Gen Intern Med 199712439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spitzer R L, Williams J B, Kroenke K.et al Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME‐MD 1000 study. JAMA 19942721749–1756. [PubMed] [Google Scholar]
- 14.Unutzer J, Katon W, Callahan C M.et al Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial. JAMA 20022882836–2845. [DOI] [PubMed] [Google Scholar]
- 15.Williams J W, Jr, Noel P H, Cordes J A.et al Is this patient clinically depressed? JAMA 20022871160–1170. [DOI] [PubMed] [Google Scholar]
- 16.The Primary Mental Health Care Clinic at the White River Junction VA Medical Center 2005 APA Gold Award: improving treatment engagement and integrated care of veterans. Psychiatr Serv 2005561306–1308. [DOI] [PubMed] [Google Scholar]
- 17.Oquendo M A, Baca‐Garcia E, Kartachov A.et al A computer algorithm for calculating the adequacy of antidepressant treatment in unipolar and bipolar depression. J Clin Psychiatry 200364825–833. [DOI] [PubMed] [Google Scholar]
- 18.Schulberg H C, Block M R, Madonia M J.et al Treating major depression in primary care practice. Eight‐month clinical outcomes. Arch Gen Psychiatry 199653913–919. [DOI] [PubMed] [Google Scholar]
- 19.Schulberg H C, Katon W, Simon G E.et al Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry 1998551121–1127. [DOI] [PubMed] [Google Scholar]
- 20.NCQA HEDIS 2004 Technical Specifications. Washington, DC: National Committee for Quality Assurance, 2003
- 21.Mitchell A J, Coyne C J. Do ultra‐short screening instruments accurately detect depression in primary care? A pooled analysis and meta‐analysis of 22 studies. Br J Gen Pract 200757144–151. [PMC free article] [PubMed] [Google Scholar]