Abstract
Surgeons' intraoperative decision making is a key element of clinical practice, yet has received scant attention in the surgical literature. In recent years, serial changes in the configuration of surgical training in the UK have reduced the time spent by trainees in the operating theatre. The opportunity to replace this lost experience with active teaching of decision making is important, but there seem to have been very few studies that have directly examined the cognitive skills underlying surgical decision making during operations. From the available evidence in surgery, and drawing from research in other safety‐critical occupations, four decision‐making strategies that surgeons may use are discussed: intuitive (recognition‐primed), rule based, option comparison and creative. Surgeons' decision‐making processes should be studied to provide a better evidence base for the training of cognitive skills for the intraoperative environment.
In response to a variety of drivers, surgical curricula are moving away from immersion learning, and the traditional time‐served apprenticeship approach is being replaced by more formal, structured, competency‐assessed programmes. Work schedules are being regulated in many countries by legislation directed at health and safety considerations for both doctors and patients. The consequent reduction in attendance in the operating theatre produces a concomitant reduction in exposure to clinical situations and in the requisite number of operative procedures.1 The loss of experience in making decisions, both in the operating theatre and during perioperative management, needs to be compensated by improved teaching by expert surgeons and structured practice in simulated environments. To do this effectively, the cognitive processes used by surgeons need to be identified.
So how do surgeons make decisions under conditions of time pressure, increasing risk, and when unexpected conditions or unanticipated problems emerge during the operation? This is not only relevant to emergency surgery; unforeseen conditions requiring new decisions and/or a change of plan may also occur in elective surgery. Good judgement and sound decision making have high standing as surgical attributes,2,3 but the literature on surgeons' decision making concentrates on the preoperative stages of diagnosis and treatment planning, especially on investigative pathways and algorithms of care.4,5,6,7 Studies on intraoperative decisions are rare, and tend to focus on the technical aspects of surgical procedures8,9 or on the surgeon's physiology.10 The few studies that do address surgeons' cognition during operations are discussed below within a decision‐making framework derived from high‐risk work settings. The focus of this paper is only on the individual surgeon. It is acknowledged that there will often be significant involvement of other team members for a surgical decision, but team decision making or distributed cognitive processes are beyond the scope of this paper.
Naturalistic decision making
Classical decision theory, which deals with selecting the optimal solution,11 tends to be based on laboratory experiments, and, although it offers sophisticated techniques, the derived methods can be impractical to apply in risky, time‐driven environments. In dynamic work settings, reaching a satisfactory solution to gain control of a problem is often the decision‐maker's aim, rather than attempting to devise a perfect or optimal response. By the late 20th century, many professionals were working in safety‐critical domains, where risk and time pressures meant that decisions had to be made rapidly, with maximum accuracy.12 Consequently, a new approach has emerged, called naturalistic decision making, where psychologists study expert decision makers in operational environments, such as firegrounds, flight decks or military command.13,14,15
Researchers involved in naturalistic decision making strive to describe how experts make decisions in conditions of high uncertainty, inadequate information, shifting goals, high time pressures and risk, usually working in teams and subject to organisational constraints. These are all conditions experienced in the operating theatre, and it is likely that surgeons use similar cognitive techniques to make decisions during operations. This naturalistic approach has already been deemed to be applicable in other fields of medicine where uncertainty, suboptimality and value‐based judgements are common16 (eg, anaesthesia).17,18
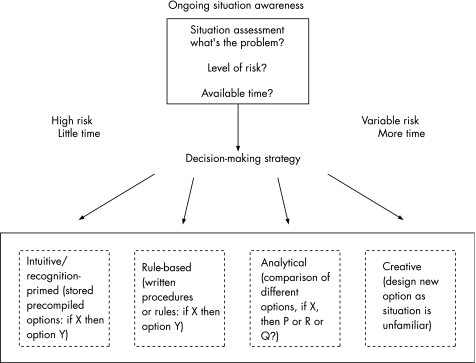
In dynamic work environments, a continuous cycle of (a) monitoring to assess the situation, then (b) taking appropriate actions and (c) re‐evaluating the results, is required. A model of dynamic decision making is given in fig 1, (adapted from research with pilots),19 followed by a brief description of each component and its possible application to surgery. Although the correspondence between pilots and surgeons can be over‐played, pilots' decision making has been extensively studied and the task demands of in‐flight decisions (risk, time pressures and limited resources) do share a number of features with intraoperative conditions. The model shows a two‐stage process: (1) situation assessment and (2) choosing a course of action.
Figure 1 Two‐step model of surgeons' intraoperative decision making (based on Orasanu and Fischer19).
Situation assessment
The continuous cognitive monitoring component in skilled performance is known as situation awareness,20 defined as “the perception of the elements in the environment within a volume of time and space, the comprehension of their meaning and the projection of their status in the near future”.21 When a significant change of state is detected, then a more focused situation assessment takes place, as fig 1 illustrates—this is the first step of the decision‐making process. It involves attending to a selection of the available cues, assembling them into a pattern (mental picture) and searching long‐term memory to recognise the problem.17 This is akin to medical diagnosis, but, in dynamic environments, the time available to take actions as well as the level of current risk must also be assessed.19 It may have to be a very rapid process: police officers have to evaluate many operational situations in less than 3 min22 (eg, in firearms incidents, they may have to do this in seconds, before they decide to shoot or not).
Situation assessment involves anticipating how the current state of events could change in the immediate future. This mental projection requires a significant level of expertise. In surgery, cases can deteriorate very rapidly. “A slow but steady and sustained blood loss in a child during surgery may result in few or subtle changes in hemodynamics for some time until a rapid decompensation occurs. If the weak signs of the developing problem were not detected, the ensuing catastrophe may seem to have occurred ‘suddenly'”.17
Consultant surgeons were asked to recount a challenging case (as part of a study to develop a behavioural rating system for surgeons' non‐technical skills).23 Their reports were analysed to identify components of decision making. (This method has been used to examine shift supervisors' decision making during microincidents on nuclear power plants.)24 Situation assessment was frequently mentioned by the surgeons (although not labelled as such). They said they had to recognise sequences of problems as they unfolded, and that they could anticipate potential developments through mental projection (see examples in table 1).
Table 1 Quotes from surgeons discussing situation assessment.
| Situation assessment | Quote |
|---|---|
| Perception | “The bone was extremely soft” |
| “The spinal fluid was still leaking out” | |
| “It is 2 hours into the operation and what we do is review the x‐rays and stop the operation” | |
| “We took the swabs off to find that it was pouring with blood” | |
| Comprehension | “I thought that the most likely thing was that the patient was becoming coagulopathic” |
| “Having thought about the situation, we decided…” | |
| Projection | “What we're trying to avoid is…” |
| “We decided that it would be technically very difficult to repair the hole in the lining of the spinal canal” |
Judgements of current and future risk pervaded each account, with some references to estimation of time. Factors influencing surgeons' situation assessment include the patient's condition and personal technical capability, as well as the competence of the assisting trainee (and communication with other team members) (Bleakley A, personal communication, 2006). These judgements are influenced by the mental models experienced surgeons store in memories of clinical situations and appropriate interventions. Way et al25 analysed 252 laparoscopic bile‐duct injuries according to the principles of “visual perception, judgment and human error”, and found that the errors stemmed mainly from misperception (ie, poor situation assessment) rather than from problems in skill or judgement. The importance of situation assessment was also underlined in a study of surgeons' decisions26 while watching a videotaped procedure, especially with regard to the detection of conditions determining the decision to convert from a laparoscopic cholecystectomy to open surgery.
Choosing a course of action: decision‐making strategies
In aviation,19 the calculation of time and risk determines the type of decision strategy a pilot is likely to adopt. Where there is little time and high risk, pilots use fast intuitive or rule‐based decision strategies. With more time, they may opt for a slower, but more rigorous, analytical strategy to evaluate alternative courses of action. In the intuitive and rule‐based methods, only one response option is considered at a time. In analytical decision making, several optional courses of action are generated and then compared simultaneously. In the creative option, the situation is judged to be totally unfamiliar and requiring a novel response. Table 2 shows quotations from consultant surgeons that fit with the first three decision methods. Each of the decision methods is discussed below.
Table 2 Quotes from surgeons discussing decision making.
| Decision‐making method | Quote |
|---|---|
| Considering options Intuitive (RPD) | “I am under extreme time pressure—there is no time to make decisions—the bleeding must be controlled rapidly and I have 20 minutes before the kidney dies. I tell the anaesthetist immediately as I find the source of bleeding and arrange for it to be clamped. I need to keep the good kidney alive so get some cold saline into the kidney.” |
| Rule based | “If damage is occurring then you want to stop, especially according to clinical governance guidelines. Part of the expertise lies in doing but the other part is recognising when you are struggling and knowing that ‘first do no harm' so I decided to stop and get a second opinion.” |
| Analytical | “There were three options to consider and at this stage we had to balance the potential risk of problems in the post‐op phase with the risks of doing something intraoperatively.” |
RPD, recognition‐primed decision making.
Intuitive
The intuitive method of decision making27 can also be called recognition‐primed decision making (RPD).28 The problem is recognised and the solution quickly recalled from a memorised rule or a personal/observed technique used in a previous encounter with a similar situation. In this method, choosing a course of action is likely to be experienced as an automatic process, with little conscious deliberation. Anaesthetists use RPD because “.. many problems require ‘decisions under uncertainty' with quick action to prevent a rapid cascade to a catastrophic adverse outcome. For these problems, deriving a solution through formal deductive reasoning from ‘first principles' is too slow. In complex, dynamic domains the initial responses of experts to the majority of events stem from pre‐compiled rules or response plans for dealing with a recognised event. .. once the event is identified, the response is well known.”18 This method is used by experienced practitioners working with relatively familiar situations, especially under high time pressures, and it may be reasonably resistant to the effects of acute stress.29 It is unlikely to be used by novices, as by definition they have limited domain experience and thus possess fewer memories of relevant events.
RPD or intuitive decision making was implicit in many of the cases discussed by the surgeons. Massoudy et al30 emphasised the importance of rapid decision making during cardiac surgery, although they did not specify the decision method. Abernathy and Hamm31 have shown how surgeons rely on intuitive decision making in a whole range of situations.
Rule based
The rule‐based method involves identifying the situation encountered, and remembering or looking up in a manual the procedure that applies. In medicine, this could involve reference to an evidence base or implementation of guidelines from an established authority such as the National Institute for Health and Clinical Excellence. This process involves more mental effort than intuition. The individual is consciously searching his or her memory store to recall the matching rule, or physically consulting a procedures manual/checklist to find the given response. High‐risk industries are governed by standard procedures, and operating personnel are often required to consult the manual before taking an action.
Rule‐based decision making is used extensively by novices who learn standard procedures for frequent or high‐risk situations. With practice, this becomes automatic and the rule can be retrieved from memory with little conscious effort (ie, recognition‐primed). It is also useful when justifying a particular decision after the event, as the protocol can be blamed if the response was incorrect. Over‐reliance on rule‐based decision making may cause a degree of skill decay. If an unexpected, unfamiliar situation arises and no rule exists, will the decision maker be able to formulate a novel course of action?
During surgery, an analogy is the implementation of guidance set out in textbooks of operative surgery. The surgeons interviewed rarely reported formal rule‐based decision making (ie, consulting checklists or textbooks), perhaps due to the diversity of options that often exist. Moreover, textbooks cannot identify context in anything other than broad descriptions of situations, and are relatively inaccessible during the course of an operation.
Option comparison
The method of comparing options is often called analytical or rational choice decision making. The decision maker recalls a number of possible courses of action and compares them simultaneously to determine which one best fits the needs of the situation. There are a multitude of cumbersome mathematical and statistical techniques to aid in selection of the optimal choice (eg, multi‐attribute decision theory, Bayesian modelling). The problem with this method is that it requires considerable time and mental concentration to conduct a thorough analytical comparison.
Surgeons may utilise some kind of limited form of analytical option comparison with particular algorithms for estimating relative risks, akin to the fast and frugal heuristics used in other dynamic domains.32 Velanovich33 considers decision heuristics during surgery; similarly, Aziz et al34 discuss how surgeons rely on rules of thumb/tricks of the trade to solve problems (eg, using packs to provide exposure, tensioning tissue to facilitate dissection) and report that there is a need to identify the heuristics that surgeons use. The surgeons interviewed did describe both analytical and heuristic approaches when decisions had to be made during surgery. This usually took the form of generating options and simultaneously (rather than sequentially) comparing them to weigh the relative risks and feasibility.
Creative
This type of decision making seems to be infrequently used in high time‐pressure environments, as it requires devising a novel course of action for an unfamiliar situation. Pilots rarely seem to use this method successfully, although one famous example is the DC‐10 (United Airlines flight 232) that crash‐landed at Sioux City with a high number of survivors.35
Creative decision making (devising a novel course of action) was not mentioned by the surgeons interviewed and is likely, as in other domains, to be infrequently used in high time pressure, high‐risk surgical situations. However, examples of creative surgical decisions might include the original use of intraoperative endoscopy in the search for an occult bleeding source in gastrointestinal haemorrhage—or for an intraoperative, colonic lavage to permit primary anastomosis in an otherwise adverse operative environment.
In summary, dynamic decision making can be conceptualised as a two‐stage process, assessing and diagnosing the situation, and then using one or more decision methods to select a course of action. Correct identification of the situation is paramount. Pilots make more decision errors by way of misidentifying the situation and applying the stipulated procedure, than they do in correctly identifying the situation, but then taking the wrong actions.19 Dynamic decision makers will typically switch between intuition, rules and analysis, depending on the time available, familiarity and task demands.36 As Crosskerry37 notes when comparing intuitive and analytical methods with clinical decision making, “the trick is in matching the appropriate cognitive activity to the particular task”.
Some form of fusion of the different types of decision making may also probably take place, depending on context (eg, elective vs emergency, familiarity of the procedure, predictability of events). In the case of a sudden, adverse event—for example, catastrophic bleeding—the first intuitive decision will be to secure haemostasis by achieving proximal and distal control, and thus create time to assess the situation and to consider the options that may currently be available. Experienced surgeons may rely more on intuitive, pattern‐matching techniques than trainees, who will have to make more laborious comparisons of optional courses of action for a given problem.
Whatever the method of decision making that is used, it is advisable that a review stage is included after implementation, to ensure that the chosen course of action resolves the problem as anticipated. Discussion of intraoperative decisions should be included during post‐case debriefing, although this safety procedure seems to be used far less frequently in medicine than in other safety‐critical professions.
Conclusion
Decision making during surgery, particularly during emergency surgery, is a key element in clinical practice that merits better preparation than is currently delivered. Current techniques in surgical training allow little opportunity for reflection, and perhaps there is now place for a more careful scrutiny of surgeons' cognition, using the naturalistic decision research methods. Techniques are being developed to enhance situation awareness and decision‐making skills using low‐fidelity methods,29,38 and these could be easily adapted for surgeons. It appears that post‐event interviewing to extract components of cognitive expertise might be usefully adapted to study surgeons' decision making, and the resulting data could constitute important ingredients of a tuition package. In other professions, where situation awareness and decision making are regarded as safety‐critical skills, they are addressed explicitly in basic training.39,40 Kohls‐Gatzoulis et al41 have demonstrated decision training for surgeons to be both possible and effective. Some of the new courses on surgeons' non‐technical skillsi are beginning to incorporate material on decision making.42 If clinical decision making is to be valued as highly as technical skills, then a better understanding of surgeons' cognitive skills must accrue, so that the processes can be studied, and reconstituted as a skill that can be applied by the practising surgeon. This learning must be applied with a sense of expediency, given the rapidly changing educational environment for future cadres of surgical specialties.
Acknowledgements
We thank Mr Paterson‐Brown and Mr Cassar for their comments on this paper.
Abbreviations
RPD - recognition‐primed decision
Footnotes
i For instance, the Royal College of Surgeons Edinburgh Safer Operative Skills course and the Royal College of Surgeons England Safety and Leadership Interventional Procedures and Surgery course both include modules on decision making.
Competing interests: None declared.
References
- 1.Poulose B, Ray W, Arbogast P.et al Resident work hour limits and patient safety. Ann Surg 2005241847–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yule S, Flin R, Paterson‐Brown S.et al Non‐technical skills for surgeons: a review of the literature. Surgery 2006139140–149. [DOI] [PubMed] [Google Scholar]
- 3.Hall J, Ellis C, Hamdorf J. Surgeons and cognitive processes. Br J Surg 20029010–16. [DOI] [PubMed] [Google Scholar]
- 4.Nugent W. Decision support in clinical practice: guidelines, pathways, algorithms, protocols and risk stratification. In: Manuel B. Nora P, eds. Surgical patient safety. Chicago: American College of Surgeons, 2004
- 5.De Cossart L, Fish D.Cultivating a thinking surgeon. Shrewsbury: TFM, 2005
- 6.McIntyre R, Stiegmann G, Eiseman B.Surgical decision making. 5th edn. Philadelphia: Elsevier, 2004
- 7.Sevdalis N, McCulloch P. Teaching evidence based decision making. Surg Clin North Am 20068659–70. [DOI] [PubMed] [Google Scholar]
- 8.Roberts J. Minimally invasive surgery in the treatment of empyema: intraoperative decision making. Ann Thorac Surg 200376225–230. [DOI] [PubMed] [Google Scholar]
- 9.Bolotin G, Kypson A, Nifong W.et al A technique for evaluating competitive flow for intraoperative decision making in coronary heart surgery. Ann Thorac Surg 2003762118–2120. [DOI] [PubMed] [Google Scholar]
- 10.Czyzewska E, Kicka K, Czarnecki A.et al The surgeon's mental load during decision making at various stages of operations. Eur J Appl Physiol Occup Physiol 198351441–446. [DOI] [PubMed] [Google Scholar]
- 11.Connolly T, Arkes H, Hammond K.Judgment and decision making. Cambridge: Cambridge University Press, 2000
- 12.Flin R.Sitting in the hot seat: leaders and teams for critical incident management. Chichester: Wiley, 1996
- 13.Flin R, Salas E, Strub M.et alDecision making under stress. Aldershot: Ashgate, 1997
- 14.Lipshitz R, Klein G, Orasanu J.et al Taking stock of naturalistic decision making. J Behav Decis Making 200114331–352. [Google Scholar]
- 15.Zsambok C, Klein G.Naturalistic decision making. Mahwah, NJ: Lawrence Erlbaum, 1997
- 16.Falzer P. Cognitive schema and naturalistic decision making in evidence‐based practices. J Biomed Inform 20043786–98. [DOI] [PubMed] [Google Scholar]
- 17.Gaba D. Dynamic decision making in anaesthesia: cognitive models and training approaches. In: Evans D, Patel V, eds. Advanced models of cognition for medical training and practice. Berlin: Springer‐Verlag, 1992
- 18.Rall M, Gaba D. Human performance and patient safety. In: Miller R, ed. Miller's anesthesia. Philadelphia: Elsevier, 20053027
- 19.Orasanu J, Fischer U. Finding decisions in natural environments: the view from the cockpit. In: Zsambok C, Klein G, eds. Naturalistic decision making. Mahwah, NJ: Lawrence Erlbaum, 1997
- 20.Banbury S, Tremblay S.A cognitive approach to situation awareness. Aldershot: Ashgate, 2004
- 21.Endsley M, Garland D.Situation awareness. Analysis and measurement. Mahwah, NJ: LEA, 20005
- 22.Flin R, Wujec L, Grant V.et al Police officers' assessments of operation situations. Policing 2007. In press
- 23.Yule S, Flin R, Maran N.et al Developing a taxonomy of surgeons' non‐technical skills. Med Educ 2006401098–1104. [DOI] [PubMed] [Google Scholar]
- 24.Carvalho P, Santos I, Vidal M. Nuclear power plant shift supervisor's decision making during microincidents. Ind Ergon 200535619–644. [Google Scholar]
- 25.Way L, Stewart L, Gantert W.et al Causes and prevention of laparoscopic bile duct injuries. Ann Surg 2003237460–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dominguez C, Flach J, McDermott P, Smith K, Johnston P.et al The conversion decision in laparoscopic surgery: knowing your limits and limiting your risks. In: eds. Psychological investigations of competence in decision making. Cambridge: Cambridge University Press, 2004
- 27.Claxton G.Hare brain, tortoise mind. Why intelligence increases when you think less. London: Fourth Estate, 1997
- 28.Klein G. A recognition‐primed decision (RPD) model of rapid decision making. In: Klein G, Orasanu J, Calderwood R, Zsambok C, eds. Decision making in action. New York: Ablex, 1993
- 29.Klein G.Sources of power. How people make decisions. Cambridge: MIT Press, 1998
- 30.Massoudy P, Kim Y, Cetin M.et al Internal thoracic artery malperfusion: fast decision for an additional vein graft has impact on patient outcome. Ann Thorac Surg 2004772061–2065. [DOI] [PubMed] [Google Scholar]
- 31.Abernathy C, Hamm R.Surgical intuition. Philadelphia: Belfus, 1993
- 32.Gigerenzer G, Goldstein D. Reasoning the fast and frugal way: models of bounded rationality. Psychol Rev 1996103650–669. [DOI] [PubMed] [Google Scholar]
- 33.Velanovich V. Operative decisions. Theor Surg 1991638–40. [Google Scholar]
- 34.Aziz F, Khalil A, Hall J. Evolution of trends in risk management. ANZ J Surg 200575603–607. [DOI] [PubMed] [Google Scholar]
- 35.Haynes A. United 232: coping with the ‘one chance‐in‐a‐billion' loss of all flight controls. Flight Deck 199235–21. [Google Scholar]
- 36.Hammond K. Judgment and decision making in dynamic tasks. Inf Decis Technol 1988143–14. [Google Scholar]
- 37.Crosskerry P. The theory and practice of clinical decision‐making. Can J Anaesth 200552R1–R8. [Google Scholar]
- 38.Crichton M, Flin R, Rattray W. Training decision makers ‐tactical decision games. J Contingencies Crisis Manage 20028208–217. [Google Scholar]
- 39.Flin R, Maran N. Identifying and training non‐technical skills in acute medicine. Qual Saf Health Care 200413(Suppl 1)i180–i184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flin R, O'Connor P, Crichton M.Safety at the sharp end. A Guide to non‐technical skills. Aldershot: Ashgate, 2007. In press
- 41.Kohls‐Gatzoulis J, Regehr G, Hutchison C. Teaching cognitive skills improves learning in surgical skills courses: a blinded, prospective, randomized study. Can J Surg 200447277–283. [PMC free article] [PubMed] [Google Scholar]
- 42.Flin R, Yule S, Maran N.et al Teaching surgeons about non‐technical skills. Surgeon 2007586–89. [DOI] [PubMed] [Google Scholar]