Abstract
Prevention of ankle sprain, the most common sporting injury, is only possible once risk factors have been identified. Voluntary strength, proprioception, postural sway, and range of motion are possible risk factors. A systematic review was carried out to investigate these possiblities. Eligible studies were those with longitudinal design investigating ankle sprain in subjects aged ⩾15 years. The studies had to have measured range of motion, voluntary strength, proprioception, or postural sway before monitoring incidence of lateral ankle sprain. Dorsiflexion range strongly predicted risk of ankle sprain. Postural sway and possibly proprioception were also predictors. Therefore the preliminary evidence suggests that people with reduced ankle dorsiflexion range may be at increased risk of ankle sprain.
Keywords: lateral ankle sprain, prediction, dorsiflexion
A large number of people do not recover after an ankle sprain and continue to experience disabling consequences such as functional instability, recurrence, and pain six months after injury.1,2 The development of prevention programmes or preventive behaviours is strongly related to the identification of those at high risk of sprain and/or the factors that increase risk of ankle sprain.
Several extrinsic and intrinsic factors may increase the risk of future sprain. Possible intrinsic factors include postural sway, range of motion, muscle strength, proprioception, and previous sprains. A cursory inspection of the research that has attempted to identify predictors of ankle sprains yields confusing results.3 For example, Beynnon and colleagues investigated muscle strength in two separate studies and reported an association between low inversion/eversion ratios and risk of future sprains in one study4 but not in the other.5 The same group5 reported that range of motion was not associated with risk of ankle sprain, but Pope et al6 found a strong association. Tropp et al7 found an association between increased postural sway and risk of lateral ankle sprain, but Beynnon et al5 did not.
The aim of this study was to systematically review evidence that measures of voluntary strength, proprioception, range of motion, or postural sway can predict lateral ankle sprain. A secondary aim was to quantify the risk of lateral ankle sprain.
Methods
Inclusion criteria
Studies were included if they used a longitudinal design and investigated first or recurrent lateral ankle sprain in subjects aged ⩾15 years. To be included in the review, the study must have measured at least one of the following possible intrinsic predictors before monitoring incidence of ankle sprain: range of motion, any measurement of voluntary strength, proprioception, or postural sway. Use of surgical procedures was an exclusion criterion, although clinical trials of surgical interventions that included a group of subjects who had not undergone surgery were included.
Identification of studies and assessment of methodological quality
Studies were identified through a search of the Medline, Cinahl, Embase and SportDiscus databases from the earliest date to February 2006. The search protocols were specifically designed to identify observational studies (table 1). Key search terms were recurrence, ankle sprain, inversion, supination, and ankle injuries. No language restriction was imposed. All papers identified by the search strategy were screened independently by two researchers, and ambiguities were resolved by mutual consent.
Table 1 Search strategy for the study.
| 1 epidemiologic studies/ |
| 2 exp case control studies/ |
| 3 exp cohort studies/ |
| 4 exp prospective studies/ |
| 5 exp “outcomes (health care)”/ |
| 6 exp outcome assessment/ |
| 7 exp prognosis/ |
| 8 exp risk factors/ |
| 9 exp Follow‐Up Studies/ |
| 10 exp Epidemiological Research/ |
| 11 odds ratio/ |
| 12 natural history.tw. |
| 13 time factors/ |
| 14 exp clinical trials/ |
| 15 recurrence/ |
| 16 incidence/ |
| 17 (case and control).tw. |
| 18 risk$.tw. |
| 19 etiol$.tw. |
| 20 aetiol$.tw. |
| 21 odds ratio$.tw. |
| 22 (causation or causal$).tw. |
| 23 cohort$.tw. |
| 24 (observational adj (study or studies)).tw. |
| 25 longitudinal.tw. |
| 26 prognos$.tw. |
| 27 outcome$.tw. |
| 28 predict$.tw. |
| 29 course$.tw. |
| 30 retrospective.tw. |
| 31 or/1–30 |
| 32 (talocrural or talo‐crural or talocalcaneal or talo‐calcaneal or talofibular or talo‐fibular).tw. |
| 33 inversion.tw. |
| 34 supination.tw. |
| 35 ankle$.tw. |
| 36 or/32–35 |
| 37 exp joint instability/ |
| 38 sprain$.tw. |
| 39 injur$.tw. |
| 40 exp “Sprains and Strains”/ and “strains”/ |
| 41 or/37–40 |
| 42 36 and 41 |
| 43 exp ankle injuries/ |
| 44 42 or 43 |
| 45 31 and 44 |
This strategy was used to search Medline. The strategy was modified for searches of other databases.
Quality of the studies was assessed by two researchers independently (MdN, KR) using a six item scale developed for prognostic studies by Pengel et al.8 Ambiguities were resolved by mutual consent or by a third researcher (RH) when necessary.
Data extraction and analysis
Data on the following study characteristics were extracted from eligible papers: target population, sample size, specific injury reported, and time of follow up (table 2). Measures of association between range of motion, voluntary strength, proprioception, or postural sway and risk (incidence proportion or incidence rate of ankle sprain) were also extracted when possible. The independent variables considered in the analysis were selected from those measured at baseline, before the monitoring period. All the analyses reported here were of between‐individual differences as opposed to between‐ankle because that was the approach used in all but one of the available publications.4 We intended to conduct a meta‐analysis where more than one study provided measures of the same associations for similar populations.
Table 2 Characteristics of studies included in the review.
| Reference | Participants | Design | Type of injury | Follow up |
|---|---|---|---|---|
| Gabbe et al 20049‐ns | 122 Australian football players | Prospective cohort study | 14 ankle sprains | 5 months |
| Arnason et al 200410‐ind/rec | 306 soccer players | Prospective cohort study | 20 ankle sprains | 4 months |
| Beynnon et al 20015‐ind | 118 varsity athletes | Prospective cohort study | 20 ankle sprains | 2 seasons |
| Soderman et al 200111‐ind/rec | 199 female soccer players (22 drop outs) | Prospective cohort study | 28 ankle sprains (23 athletes) | 7 months |
| Leanderson et al 199612‐ind/rec | 53 dancers + 23 active subjects | Prospective cohort study | 6 ankle sprains | 19 months |
| Wiesler et al 199613‐ind/rec | 148 dance students | Prospective cohort study | 23 ankle sprains | 9 months |
| Shambaugh et al 199114‐ns | 45 basketball players | Prospective cohort study | 6 ankle sprains | 4 months |
| Ekstrand/Gillquist 198315‐ind/rec | 180 soccer players | Prospective cohort study | 43 ankle sprains | 12 months |
| Payne et al 199716‐ind/rec1 | 42 basketball players | Prospective cohort study | 8 ankle injuries | 2.1 months |
| Tropp et al 19847‐ind/rec | 127 soccer players | Prospective cohort study | 23 ankle injuries | 12 months |
| Willems et al 200517‐ind/rec¥ | 159 female physical education students | Prospective cohort study | 32 inversion ankle sprains | 12–36 months |
| Willems et al 200518‐ind/rec¥ | 241 male physical education students | Prospective cohort study | 44 inversion ankle sprains | 12–36 months |
| McGuine et al 200019‐ind/rec2 | 210 high school basketball players | Prospective cohort study | 20 inversion sprain | 12 months |
| Pope et al 19986‐ind/rec | 1093 army recruits | Randomised clinical trial | 27 lateral ankle sprains | 2.57 months |
| Baumhauer et al 19954‐ind/rec¥ | 145 lacrosse, soccer or field hockey athletes | Prospective cohort study | 15 lateral ankle sprains | 12 months |
| Hopper et al 199520‐ns | 72 netball players | Prospective cohort study | 8 lateral ankle sprain | 14 weeks |
| Milgrom et al 199121‐ind/rec | 390 infantry recruits | Prospective cohort study | 69 lateral ankle sprains | 14 weeks |
| Holme et al 199922‐rec | 92 recreational athletes (67 followed up) | Randomised clinical trial | 13 recurrences | 12 months |
| Eiff et al 1994 23‐rec | 77 patients | Randomised clinical trial | 6 recurrences | 12 months |
| Watson et al 199924‐ns | 80 Gaelic football and hurling athletes | Prospective cohort study | 122 ankle sprains | 48 months |
| Twellaar et al 199725‐ns | 136 students | Prospective cohort study | Not stated | 48 months |
ns, Information about analysing index and/or recurrent injury not stated; ind, only index injuries were analysed; ind/rec, index injuries and recurrent injuries were analysed; ind/rec1, index injuries and recurrent injuries longer than 6 months were analysed; ind/rec2, index injuries and recurrent injuries longer than 12 months were analysed; ind/rec¥, index injuries and recurrent injuries of grade I (considering graduation from I to III); rec, only recurrent injuries were analysed.
Results
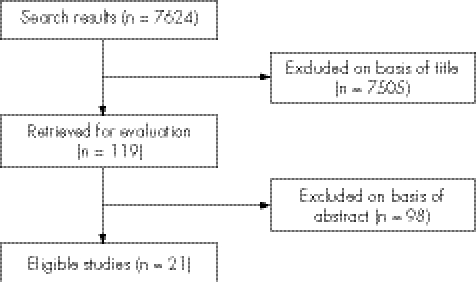
The search identified 7624 articles, of which 21 met all the inclusion criteria and were included in this review (fig 1, table 2). Of the 21 studies, nine reported the ankle injuries as “ankle sprains”—that is, they did not specify whether sprains were lateral or medial5,9,10,11,12,13,14,15,24—and two studies reported the incidents as “ankle injuries” and did not indicate what proportion of injuries were sprains, fractures, or other injuries.7,16 Only seven studies specified that the injuries were lateral ankle sprains.4,6,17,18,19,20,21 In some studies, subjects had a prior sprain, and recurrences were monitored, and in others subjects had no history of sprain and time to the first sprain was monitored (table 2). Two studies monitored sprain recurrences in subjects who had been admitted to the emergency room for an acute ankle sprain.22,23 One study gave no clear indication of the type of ankle injury sustained.25
Figure 1 Flow chart of the search process.
The 21 included studies consisted of three randomised clinical trials6,22,23 and 18 prospective cohort studies.4,5,7,9,10,11,12,13,14,15,16,19,20,21,24,25 In 15 of the 21 studies,4,5,7,9,10,11,12,13,14,15,16,19,20,22,24 participants were athletes. In the other seven studies, participants were students,17,18,25 army recruits,6,21 or recruited from a mixed population.23 Because the studies were heterogeneous and the body of evidence for each outcome was too small, we did not conduct a meta‐analysis.
Methodological quality
The two reviewers scored 126 quality criteria and agreed on 93 (73.8% agreement). The intraclass correlation coefficient (ICC2,1) for the total quality score was 0.42. Nine studies (43%) defined the sample, five (24%) clearly described methods for assembling a representative sample, 12 (57%) reported follow up of at least 80%, and most studies (86%) quantified prognosis. No study reported blinded assessment of outcome measures. Seven studies (33%) reported statistical adjustments (table 3).
Table 3 Assessment of methodological quality.
| Reference | Defined sample* | Representative sample† | Complete follow up‡ | Prognosis§ | Blinded outcome¶ | Statistical adjustment** | Final score |
|---|---|---|---|---|---|---|---|
| Gabbe et al 20049 | Yes | No | Yes | Yes | No | No | 3 |
| Arnason et al 200410 | No | No | Yes | Yes | No | No | 2 |
| Beynnon et al 20015 | Yes | No | Yes | Yes | No | Yes | 4 |
| Soderman et al 200111 | No | No | No | Yes | No | Yes | 2 |
| Leanderson et al 199612 | No | No | Yes | Yes | No | No | 2 |
| Wiesler et al 199613 | No | No | Yes | Yes | No | Yes | 3 |
| Shambaugh et al 199114 | No | No | Yes | Yes | No | Yes | 3 |
| Ekstrand and Gillquist 198315 | No | Yes | No | Yes | No | No | 2 |
| Payne et al 199716 | Yes | No | Yes | Yes | No | Yes | 4 |
| Tropp et al 19847 | No | Yes | No | No | No | No | 1 |
| Willems et al 200517 | Yes | No | No | Yes | No | No | 2 |
| Willems et al 200518 | Yes | Yes | No | Yes | No | No | 3 |
| McGuine et al 200019 | Yes | No | Yes | Yes | No | Yes | 4 |
| Pope et al 19986 | Yes | Yes | Yes | Yes | No | Yes | 5 |
| Baumhauer et al 19954 | Yes | No | Yes | Yes | No | No | 3 |
| Hopper et al 199520 | No | No | No | Yes | No | No | 1 |
| Milgrom et al 199121 | No | No | No | Yes | No | No | 1 |
| Holme et al 199922 | No | No | No | Yes | No | No | 1 |
| Eiff et al 199423 | Yes | Yes | Yes | No | No | No | 3 |
| Watson 199924 | No | No | Yes | Yes | No | No | 2 |
| Twellaar et al 199725 | No | No | No | No | No | No | 0 |
A “yes” is only awarded if the criterion is clearly satisfied. A “no” is awarded if the criterion is clearly not satisfied or if it is unclear if the criterion is satisfied.
*Description of source of subjects and inclusion/exclusion criteria.
†Subjects were selected by random selection or were consecutive cases.
‡At least one prognostic outcome was available from at least 80% of the study population at the three month follow up or later.
§Studies provided raw data, percentages, survival rates, or continuous outcomes.
¶Assessor was unaware of at least one prognostic factor, used to predict the prognostic outcome, at the time they measured the prognostic outcome.
**For at least two prognostic factors with the adjustment factor reported.
NA, Study did not evaluate prognostic factors.
Risk of injury
Cumulative incidence proportions (the proportion of people injured at least once in a defined time) and 95% confidence intervals (CI) were reported or could be calculated for 17 of the 21 studies (fig 2). We grouped the studies according to the specificity of the reported injury (table 2). Cumulative incidence proportions varied from 0.02 at 2.8 months6 to 0.24 at 12 months.5 The remaining four studies17,18,24,25 did not present data in a way that enabled calculation of incidence proportions, although Willems et al17 reported a sprain incidence rate of 0.75 per 1000 hours of sports exposure.
Figure 2 Cumulative incidence proportion of unspecified ankle sprains, ankle injuries, lateral ankle sprains, and recurrences from 17 studies. Each data point is the estimated incidence proportion from a single study. The error bars are 95% confidence intervals.
Range of motion
Range of motion was evaluated as a predictor of ankle sprain in 13 studies.4,6,9,10,11,13,14,15,16,17,18,23,25 However, five of these4,10,15,18,25 only reported p values for the difference in range of motion between subjects who were subsequently injured or not injured. Baumhauer et al4 (quality score 3) reported a significantly greater baseline range of motion for subtalar eversion in the injured group.
Five studies did not report any data on the strength of the association (predictive accuracy) and therefore could not be included in the analysis.9,11,13,14,23 Two studies reported the strength of the association of ankle range of motion. Pope et al6 (quality score 5) reported that subjects with the most inflexible ankles (34° of dorsiflexion range) had nearly five times the risk of suffering an ankle sprain as subjects with average flexibility (45° of dorsiflexion range). Willems et al17 reported that risk of ankle sprain increased by about 3% per degree of range of the first metatarsophalangeal joint. Thus a subject with 2 standard deviations (30°) more metatarsophalangeal joint extension would have 2.5 times the risk of a person with average metatarsophalangeal range.17
Voluntary strength
The predictive value of voluntary strength was examined in 10 studies.4,5,9,11,15,16,17,18,21,22 Five9,11,15,16,22 did not provide data that could be used to assess the predictive value of voluntary strength for lateral ankle sprains. The remaining five studies4,5,17,18,21 presented p values for the difference in means, but not raw data on the effect of voluntary strength as a risk factor. Baumhauer et al4 (quality score 3) reported a significantly higher eversion/inversion strength ratio in the injured group, Willems et al17,18 reported stronger dorsiflexors for the injured group in female students17 but stronger dorsiflexors for the uninjured group in male students.18 No other comparison was significant in any of these studies.
Proprioception
Four studies investigated the predictive accuracy of proprioception.16,17,18,22 Payne et al16 (quality score 4) reported that position sense predicted left but not right ankle injury. This seems hardly credible, and may well reflect a type I or type II statistical error, so it suggests that one or both of the findings are spurious. They also reported that deficits in joint position sense in right dorsiflexion and right eversion predicted sprains, but not left dorsiflexion or left eversion, creating the same doubts about statistical validity. Holme et al22 (quality score 1) reported the number of recurrences, but did not give the strength of associations between measures of proprioception and risk of recurrence.
Willems et al17 reported better position sense for the uninjured group, suggesting that people with 2 standard deviations (about 11°) more error in sensing inversion passive position at the ankle would have about 2.3 times the risk of a person with average position sense.17
Postural sway
Seven studies measured postural sway using a force platform to determine centre of pressure displacement.5,7,12,17,18,19,22 Neither Leanderson et al12 (quality score 2) nor Holme et al22 (quality score 1) provided data that could be used to determine the value of postural sway as a predictor of lateral ankle sprain. Beynnon et al5 (quality score 4) compared the mean centres of pressure displacement in groups who were subsequently injured or not, but did not find statistically significant differences. Willems et al18 (quality score 3) compared 16 variables in groups who were subsequently injured or not and did not find any difference between groups except for what they called “limit of stability directional control” which they reported as being higher for the uninjured group. The analysis reported by Beynnon et al5 and Willems et al18 gives no information on the predictive accuracy of the measured variables for lateral ankle sprains.
McGuine et al19 (quality score 4) dichotomised postural sway and found that subjects with high levels of centre of pressure displacement had greater risk of lateral ankle sprain of subjects with low levels of displacement (incident rate ratio 6.7, odds ratio 10.2). They reported that subjects who suffered ankle sprains had a mean (SD) sway of 2.0 (0.32)°/s, whereas healthy subjects had a mean sway of 1.7 (0.31)°/s. Tropp et al7 (quality score 1) also presented the data in dichotomous terms: subjects had either normal or abnormal centre of pressure displacement values. From their data, we calculated that the likelihood ratio for a sprain within 12 months among people with abnormal postural sway was 3.2 (95% CI 1.8 to 5.7), and the likelihood ratio for people with normal postural sway was 0.57 (95% CI 0.37 to 0.89).
Willems et al17 (quality score of 3) measured what they called “limits of stability” (a measure of maximum distance that a person can intentionally displace the centre of gravity in standing), among other variables. They found that, in females, a 2 SD increase in the limits of stability would confer about 45% higher chance of having an ankle sprain.17
Two other studies investigated the prognostic accuracy of balance.20,24 Hopper et al20 (quality score 1) measured static balance, but did not report the type of injuries sustained. Watson24 (quality score 2) also measured balance, which he called “proprioception”. Normal performance was defined as the ability to maintain steady balance on one leg for more than 15 seconds. The likelihood ratio for people with abnormal balance performance was 2.5 (95% CI 1.3 to 4.6), and the likelihood ratio among those with normal balance performance was 0.46 (95% CI 0.30 to 0.73).
Discussion
The studies reviewed here suggest that people with inflexible ankles (34° dorsiflexion range of motion) have nearly five times the risk of ankle sprain of people with an average flexibility (45°).6 Three studies7,17,24 also suggest that postural sway may play a role as a predictive factor, although estimates of the predictive accuracy of postural sway range from weak to strong. Passive inversion position sense may also be a predictive factor for ankle sprains, although only one study presented such findings.17
Few longitudinal studies explicitly stated that their main aims were to study prediction of lateral ankle sprains4,6,19,20,21, and in some cases prediction was clearly not the main focus of the study.6,22,23 Consequently the methodology of most studies was not the most appropriate for the purpose intended in this review. The predictive validity of predictors can be increased by determining if the predictors perform well on an independent dataset.26 Unfortunately none of the papers in this review validated their predictors on a validation set.
Not all studies treated lateral ankle sprains separately from other ankle injuries. However, two studies reported the number of lateral ankle sprains as a proportion of other ankle injuries.19,20 Hopper et al20 reported that 88.9% of their ankle injuries were lateral ankle sprains, and McGuine et al19 reported that 87% of their ankle injuries were lateral ankle sprains. It seems reasonable to expect that the proportion of lateral ankle sprains in other studies that did not present separate results for ankle sprains would be similar to those presented by Hopper et al20 and McGuine et al.19
We found evidence from two studies that dorsiflexion range of motion predicted future lateral ankle sprain.6,18 One other study investigated the same outcome and did not have the same finding,4 but this study only reported p values (not the strength of the association) and it had a relatively low methodology quality. Baumhauer et al4 also reported that decreased subtalar eversion predicted an increased risk of sprains, but, as the strength of the association was not investigated, the importance of this result remains unclear. Although more studies are necessary to confirm this finding, it appears that ankle dorsiflexion is a strong predictor of risk, at least in army recruits undergoing initial training.
Postural sway was the most widely studied factor of all the predictor variables included in this review, and yet the results are inconclusive. Nine studies5,7,11,12,17,18,19,20,22 investigated the predictive value of some form of balance measurement, but owing to inappropriate analysis, lack of data, or difference in the methods used, little can be concluded from these studies. Likelihood ratios calculated from data provided by Tropp et al7 and Watson24 provide preliminary evidence that decreased ability to balance may weakly predict future ankle sprains. Willems et al17 presented hazard ratios of 0.96 (95% CI 0.93 to 1.00) for limit of stability end point excursion and 0.94 (95% CI 0.89 to 0.99) for limit of stability maximum end point excursion. Although the methods for testing were different (standing on one leg for Tropp et al7 and Watson24 and standing on both legs for Willems et al17), this finding supports the findings that decreased ability to balance may predict future sprains. However, because there were 16 different comparisons for balance measures, this finding could be a type I error, and should be interpreted with caution.
We found no evidence that voluntary strength predicts lateral ankle sprain. Three studies4,17,18 each found one comparison to be statistically significant, but predictive accuracy was not reported in these studies, and the direction of the effect was inconsistent. Another two studies5,21 reported statistically non‐significant differences between groups. The role of voluntary strength in ankle sprain therefore remains unknown.
Although impaired proprioception is widely considered to cause ankle sprain,27,28 only one study17 presented enough evidence to support such a belief. One of the studies that found sense of movement to be a predictor of ankle sprain reported that this finding held only for left ankles,16 which would appear unlikely. Willems et al17 reported that passive inversion position sense was a strong predictor of ankle sprain. As there is evidence that performance in different proprioception tests is not correlated,29 future investigations may also be directed to other aspects of proprioception, such as movement detection, as predictors of future ankle sprain.
The cumulative incidence proportions for ankle sprains in our review did not increase as the follow up time increased—that is, the incidence proportion appeared to reach a maximum of 24% at 12 months and did not increase further with increasing time (fig 2). In interpreting these findings, it is important to consider that the apparent insensitivity of risk to time could be confounded by study level or individual patient level characteristics.
Our review found that high quality investigations on predictors of lateral ankle sprain are scarce. The factors we found to predict ankle sprains are dorsiflexion range of motion, postural sway, and perhaps proprioception. These findings should be considered preliminary. Dorsiflexion range of motion appears to be the best predictor to date considering the strength of the results and the quality of the respective studies. Perhaps the key for prediction of ankle sprains is the interaction of variables such as range of motion, proprioceptive factors, and postural sway.
Acknowledgements
MdN is a scholarship holder funded by CAPES (Coordenação de aperfeiçoamento de pessoal de nível superior) from the Brazilian government.
Footnotes
Competing interests: none declared
References
- 1.Braun B L. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med 19998143–148. [DOI] [PubMed] [Google Scholar]
- 2.Garrick J G, Requa R K. The epidemiology of foot and ankle injuries in sports. Clin Podiatr Med Surg 19896629–637. [PubMed] [Google Scholar]
- 3.Beynnon B D, Murphy D F, Alosa D M. Predictive factors for lateral ankle sprains: A literature review. J Athl Train 200237376–380. [PMC free article] [PubMed] [Google Scholar]
- 4.Baumhauer J F, Alosa D M.et al A prospective study of ankle injury risk factors. Am J Sports Med 199523564–570. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon B D, Renstrom P A, Alosa D M.et al Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res 200119213–220. [DOI] [PubMed] [Google Scholar]
- 6.Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre‐exercise calf muscle stretching on injury risk in Army recruits. Aust J Physiother 199844165–172. [DOI] [PubMed] [Google Scholar]
- 7.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc 19841664–66. [PubMed] [Google Scholar]
- 8.Pengel L H, Herbert R D, Maher C G.et al Acute low back pain: systematic review of its prognosis. BMJ 2003327323–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabbe B J, Finch C F, Wajswelner H.et al Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med 20041456–63. [DOI] [PubMed] [Google Scholar]
- 10.Arnason A, Sigurdsson S B, Gudmundsson A.et al Risk factors for injuries in football. Am J Sports Med 2004325s–16s. [DOI] [PubMed] [Google Scholar]
- 11.Soderman K, Alfredson H, Pietila T.et al Risk factors for leg injuries in female soccer players: a prospective investigation during one out‐door season.[see comment]. Knee Surg Sports Traumatol Arthrosc 20019313–321. [DOI] [PubMed] [Google Scholar]
- 12.Leanderson J, Eriksson E, Nilsson C.et al Proprioception in classical ballet dancers. A prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med 199624370–374. [DOI] [PubMed] [Google Scholar]
- 13.Wiesler E R, Hunter D M, Martin D F.et al Ankle flexibility and injury patterns in dancers. Am J Sports Med 199624754–757. [DOI] [PubMed] [Google Scholar]
- 14.Shambaugh J P, Klein A, Herbert J H. Structural measures as predictors of injury basketball players. Med Sci Sports Exerc 199123522–527. [PubMed] [Google Scholar]
- 15.Ekstrand J, Gillquist J. The avoidability of soccer injuries. Int J Sports Med 19834124–128. [DOI] [PubMed] [Google Scholar]
- 16.Payne K A, Berg K, Latin R W. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train 199732221–225. [PMC free article] [PubMed] [Google Scholar]
- 17.Willems T M, Witvrouw E, Delbaere K.et al Intrinsic risk factors for inversion ankle sprains in females: a prospective study. Scand J Med Sci Sports 200515336–345. [DOI] [PubMed] [Google Scholar]
- 18.Willems T M, Witvrouw E, Delbaere K.et al Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med 200533415–423. [DOI] [PubMed] [Google Scholar]
- 19.McGuine T A, Greene J J, Best T.et al Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med 200010239–244. [DOI] [PubMed] [Google Scholar]
- 20.Hopper D M, Hopper J L, Elliott B C. Do selected kinanthropometric and performance variables predict injuries in female netball players? J Sports Sci 199513213–222. [DOI] [PubMed] [Google Scholar]
- 21.Milgrom C, Shlamkovitch N, Finestone A.et al Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle 19911226–30. [DOI] [PubMed] [Google Scholar]
- 22.Holme E, Magnusson S P, Becher K.et al The effect of supervised rehabilitation on strength, postural sway, position sense and re‐injury risk after acute ankle ligament sprain. Scand J Med Sci Sports 19999104–109. [DOI] [PubMed] [Google Scholar]
- 23.Eiff M P, Smith A T, Smith G E. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med 19942283–88. [DOI] [PubMed] [Google Scholar]
- 24.Watson A W. Ankle sprains in players of the field‐games Gaelic football and hurling. J Sports Med Phys Fitness 19993966–70. [PubMed] [Google Scholar]
- 25.Twellaar M, Verstappen F T, Huson A.et al Physical characteristics as risk factors for sports injuries: a four year prospective study. Int J Sports Med 19971866–71. [DOI] [PubMed] [Google Scholar]
- 26.Harrell F E, Jr, Lee K L, Mark D B. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors [review; 72 refs]. Stat Med 199615361–387. [DOI] [PubMed] [Google Scholar]
- 27.Anderson S J. Practice Essentials Series editors: Harmon KG, Rubin A. Acute ankle sprains keys to diagnosis and return to play. Phys Sportsmed 20023029. [DOI] [PubMed] [Google Scholar]
- 28.Lentell G, Baas B, Lopez D.et al The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther 199521206–215. [DOI] [PubMed] [Google Scholar]
- 29.de Jong A, Kilbreath S L, Refshauge K M.et al Performance in different proprioceptive tests does not correlate in ankles with recurrent sprain. Arch Phys Med Rehabil 2005862101–2105. [DOI] [PubMed] [Google Scholar]