Abstract
Objectives
To study the long term effect of tibial shaft fractures treated by immobilisation in a long leg cast on the calf muscle bulk.
Methods
Computed tomography scans were performed at fixed points on the lower legs of 23 non‐professional athletes who sustained closed tibial fractures 16 years previously. Length of immobilisation was determined from the hospital records. All the fractures were treated non‐operatively. The cross sectional area of the various leg compartments was measured and compared with the non‐injured leg.
Results
There was a significant reduction in cross sectional area of the posterior compartment (p<0.001, Student's t test). No such difference was seen in the anterolateral compartment.
Conclusion
Tibial fractures treated non‐operatively are associated with significant long term calf muscle wasting.
Keywords: muscle wasting, fractures, young athletes, immobilisation, computed tomography
Tibial shaft fracture is a common injury in soccer and rugby players. For almost half of these players it marks the end of competitive sport.1 Most of these fractures are low energy injuries which are stable in configuration.2 Hence they tend to be treated non‐operatively. One of the most predictable consequences of cast immobilisation is loss of lean muscle mass.3,4 The extent of muscle atrophy is related to duration of immobilisation.5,6 Of most concern is the fact that the deleterious effects of immobilisation do not appear preventable or even fully recoverable.7,8 We investigated the long term effects of cast immobilisation on muscle bulk in 23 young non‐professional footballers.
Methods
Approval was obtained from the regional ethics committee. Hospital records showed that 28 patients with a sports related tibial shaft fracture were treated from January 1985 to June 1986. We successfully contacted 25 of them. Two refused to participate. The remaining 23 (21 male and two female) signed informed consent to take part in the study. The mean age at the time of injury was 18 years (range 15–34). All had a stable, low energy, diaphyseal tibial fracture (Arbeitsgemeinschaft für Osteosynthesefragen (AO) 4.2.A2/A3). They received standard treatment consisting of application of an above knee cast and mobilisation non‐weight bearing for three weeks. Isometric exercises were started on day 1. The cast was then changed to a patellar tendon bearing type, and partial weight bearing was allowed and continued until clinical fracture union (mean 10 weeks (range 8–14)). Range of motion exercises of the knee and ankle were started. The patients were then mobilised full weight bearing and followed up until the fractures were united radiologically (mean 14 weeks (range 10–17)).
Computed tomography (CT) scanning of the legs was carried out using a Somatom Plus scanner (Siemens). Leg length was measured clinically and on the pilot image of the CT scan. Cross sections of both legs were taken at a fixed point 10 cm below the tibial tuberosity. This cut was used to determine the cross sectional area (CSA) of the posterior compartment. Another cut was taken mid‐way between the tibial tuberosity and medial malleolus, and was used to determine the CSA of the anterolateral compartment. If there was a leg length discrepancy, an additional cross section was taken at a distance equal to the measured difference to minimise the error in calculation of the CSA. We chose CT scanning so that we could detect rotational malalignment in the first instance, and changes in muscle CSA was an unexpected but significant finding. Measurements were carried out using computer software (ImageJ 1.32j: National Institutes of Health, Bethesda, Maryland, USA). All data are expressed in square centimetres as seen on the CT scan with 100% magnification. This was achieved by placing a known length of white contrast with the CT scans during scanning. The image analysis software was then calibrated to this known length to obtain the required data in standard units.
The uninjured leg was used as the control. Student's t test was used to determine the statistical significance (taken as p<0.05).
Results
All the patients had satisfactory healing of the fracture. Only three of the 23 subjects were able to return to competitive sport. Of the remainder, 10 were able to return to active sport but at a non‐competitive level.
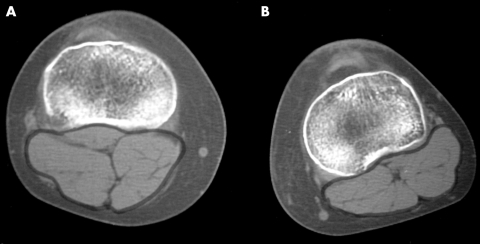
The mean (SD) CSA of the anterolateral compartment for the injured and contralateral limb was 4.83 (0.27) and 4.92 (0.38) cm2 respectively. For the posterior compartments there was a significant difference (fig 1): 6.90 (1.08) and 8.04 (1.39) cm2 respectively (p<0.001, Student's t test).
Figure 1 Computed tomography scan showing a cross section of the posterior compartment 10 cm distal to tibial spine of (A) the uninjured leg and (B) the injured leg.
Discussion
This study shows that significant loss of calf muscle bulk occurs in patients with a tibial shaft fracture treated by cast immobilisation. The advantages of cast immobilisation include a negligible risk of infection and no need for hardware removal. Operative treatment on the other hand would facilitate early weight bearing. One of the most predictable consequences of cast immobilisation is loss of muscle bulk.3,4 The other possible cause of muscle atrophy is a subclinical compartment syndrome. Decrease in muscle bulk is generally reflected as a decrease in muscle force. In functional terms, it usually means inability to return to competitive sport at the same level as before, as shown by our study. Isometric exercises are of limited help even if started early. This has been confirmed by other authors.9,10 There is no consensus on optimal treatment of these common injuries even among trauma experts.11 A meta‐analysis of the literature on closed treatment of tibial fractures12 showed that the published data were inadequate for decision making. In the light of the available evidence from our study, we recommend that early weight bearing be given the importance it deserves. Intramedullary nailing would facilitate early weight bearing and would conceivably cause less permanent damage to the musculature and thereby facilitate return to active sport. Prospective randomised studies with adequate power are required to confirm this.
Abbreviations
CSA - cross sectional area
CT - computed tomography
Footnotes
Competing interests: none declared
Approval for this study was obtained from the ethics committee of Mid‐Western Regional Hospital, Limerick, Ireland
References
- 1.Lenehan B, Fleming P, Walsh S.et al Tibial shaft fractures in amateur footballers. Br J Sports Med 200337176–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Court‐Brown C M, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg [Br] 199577417–421. [PubMed] [Google Scholar]
- 3.Goldspink D F. The influence of immobilization and stretch on protein turnover of rat skeletal muscle. J Physiol (Lond) 1977264267–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halkjaer‐Kristensen J, Ingemann‐Hansen T. Wasting of the human quadriceps after knee ligament injuries. Scand J Rehabil Med Suppl 1985135–11. [PubMed] [Google Scholar]
- 5.Max S R, Maier R F, Vogelsang L. Lysosomes and disuse atrophy of skeletal muscle. Arch Biochem Biophys 1971146227–232. [DOI] [PubMed] [Google Scholar]
- 6.Desplanches D, Mayet M H, Sempore B.et al Effect of spontaneous recovery or retraining after hindlimb suspension on aerobic capacity. J Appl Physiol 1987631739–1743. [DOI] [PubMed] [Google Scholar]
- 7.Goldspink D F. The influence of activity on muscle size and protein turnover. J Physiol (Lond) 1977264283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Widrick J J, Fitts R H. Peak force and maximal shortening velocity of soleus fibers after non‐weight‐bearing and resistance exercise. J Appl Physiol 199782189–195. [DOI] [PubMed] [Google Scholar]
- 9.Stillwell D M, McLarren G L, Gersten J W. Atrophy of quadriceps muscle due to immobilization of the lower extremity. Arch Phys Med Rehabil 196748289–295. [PubMed] [Google Scholar]
- 10.Halkjaer‐Kristensen J, Ingemann‐Hansen T. Wasting of the human quadriceps muscle after knee ligament injuries. IV. Dynamic and static muscle function. Scand J Rehabil Med Suppl 19851329–37. [PubMed] [Google Scholar]
- 11.Khalily C, Behnke S, Seligson D. Treatment of closed tibia shaft fractures. A survey from the 1997 Orthopaedic Truama Association and Osteosynthesis International: Gerhard Kuntscher Kreis meeting. J Orthop Trauma 200014577–581. [DOI] [PubMed] [Google Scholar]
- 12.Littenberg B, Weinstein L P, McCarren M.et al Closed fractures of tibial shaft: a meta‐analysis of three methods of treatment. J Bone Joint Surg [Am] 199880174–183. [DOI] [PubMed] [Google Scholar]