Abstract
Ulnar collateral ligament (UCL) insufficiency is potentially a career threatening, or even a career ending, injury, particularly in overhead throwing athletes. The evolution of treating modalities provides afflicted athletes with the opportunity to avoid premature retirement. There have been several clinical and basic science research efforts which have investigated the pathophysiology of UCL disruption, the biomechanics specific to overhead throwing, and the various types of treatment modalities. UCL reconstruction is currently the most commonly performed surgical treatment option. An in depth analysis of the present treatment options, both non‐operative and operative, as well as their respective results and biomechanical evaluation, is lacking in the literature to date. This article provides a comprehensive current review and comparative analysis of these modalities. Over the last 30 years there has been an evolution of the original UCL reconstruction. Yet, despite the variability in modifications, such as the docking technique, interference screw fixation, and use of suture anchors, the unifying concepts of UCL reconstruction are that decreased dissection of the flexor‐pronator mass and decreased handling of the ulnar nerve leads to improved outcomes.
Keywords: ulnar collateral ligament, injury, elbow, treatment
The first report documenting elbow problems in professional baseball players was published in 1941.1 Shoulder and elbow pain was subsequently recognised as a possible complication from repetitive overhead throwing. Afflicted athletes, namely baseball pitchers, were diagnosed with a “generic dead arm” and forced to retire prematurely.
In the 1960s and early 1970s, the incidence of shoulder and elbow pain in professional baseball pitchers approached 50%.2 Adaptive changes secondary to prolonged and repetitive throwing, such as hypertrophy of the dominant extremity, flexion contracture, and valgus deformity of the throwing elbow, became commonly described.3 In addition, nearly 67% of pitchers were found to have radiographic evidence of degenerative elbow disease,2 such as ulnar traction spurs and olecranon loose bodies.1
The failure of pitchers to reach and/or maintain their peak performance led to investigative efforts into throwing mechanics. Extreme valgus stress, particularly during the acceleration phase of throwing, was felt to be responsible for most of the symptoms. The term “medial elbow‐stress syndrome” was described as a unifying concept.3 Anatomically, it was believed that valgus stress led to a sequential failure of the medial elbow musculature, the ulnar collateral ligament (UCL), the medial joint capsule, and, lastly, the joint itself.
In the mid 1970s, despite a heightened awareness and new understanding of the pathophysiology behind elbow pain in throwing athletes, treatment remained centred around non‐operative treatment. In one of the first reports of surgical management,4 the anterior oblique ligament was transferred anteriorly, when the UCL was present but attenuated. This was abandoned because: (a) the remaining ligament was weaker; (b) the transferred position was not isometric; (c) elbow extension was limited.5 Primary repair of midsubstance ruptures was also attempted, but similarly discontinued when success rates did not match those of reconstruction.5
The first UCL reconstruction was performed in 1974. Lead surgeon, Frank Jobe, gave LA Dodgers pitcher, Tommy John, a 1% chance of avoiding retirement. In 1976, Tommy John returned to baseball. The success of this surgery led to a revolution. Today, UCL reconstruction is no longer considered experimental; the most commonly quoted success rate is 85%. Surgical success is defined as the ability of afflicted athletes to return to a preinjury level of play for at least one year.6,7
Over the last three decades, interest in UCL reconstruction of the elbow in overhead throwing athletes has grown substantially. Other overhead sports have been associated with UCL injury, but baseball, primarily pitching, is the most common. Recent statistical data reveal that more than 75 pitchers who have appeared in the major leagues since 2001 have had this surgery—that is, about one in nine (Dodd; USA TODAY, 2003). A recent retrospective cohort study8 of the period 1988–2003 revealed that not only has there been a dramatic overall increase, but an approximately 50% increase in UCL reconstruction in high school players (aged 15–19) in recent years.
An in depth analysis of the present treatment options, both non‐operative and operative, as well as their respective results and biomechanical evaluation, is lacking in the literature to date. A comprehensive review and comparative analysis of these modalities is necessary to fully understand the options available.
Biomechanics
There are six phases of throwing: (a) wind up; (b) early cocking; (c) late cocking; (d) acceleration; (e) deceleration; (f) follow through. The combination of large valgus loads initiated in the late cocking phase with the rapid elbow extension generated in acceleration produces compression overload laterally, shear stress in the posterior compartment, and tensile overload medially. This phenomenon, termed “valgus extension overload syndrome”,9 forms the basic pathophysiological model behind most common elbow injuries in the throwing athlete.
The mean valgus stress per pitch in an adult is 64 N.m.10 Consequently, a 64 N.m varus counter torque is needed to resist this massive torque; a 64 N.m varus torque applied to the elbow is equivalent to holding 150 baseballs. The UCL provides 54% of this varus counter torque or roughly 34 N.m.11 Specifically the anterior band of the anterior bundle is the primary restraint to valgus stress at 30°, 60°, and 90° of elbow flexion. This restraint increases with greater angles such that, at 90°, it provides 55% of the resistance to valgus stress and 78% of the resistance to elbow distraction. This is relevant because the elbow is flexed 90° during the late cocking/early acceleration phases of throwing when valgus stress is the greatest. Because the ultimate valgus torque of the UCL is only about 33 N.m,10 every pitch approaches maximum torque on the UCL complex. Consequently the enormous medial elbow tensile forces generated during late cocking/acceleration may exceed the failure strength of the UCL, leading to attenuation or rupture. Despite the tremendous medial forces sustained at the elbow, injuries are still fairly rare, because the UCL complex is protected by arm muscle activity termed dynamic stabilisation, provided by the triceps, anconeus, flexor‐pronator mass, and internal rotation of the shoulder.12,13,14,15 Recent biomechanical analysis has found that coupling of shoulder internal rotation and forearm pronation forms the physiological basis of varus acceleration to minimise valgus elbow load.16
Diagnosis
Diagnosis of UCL injury is often difficult, requiring an integrative summation of a detailed history, thorough physical examination, and supportive imaging modalities. Differential diagnosis of medial elbow pain in overhead throwing athletes includes medial tension overuse injury, flexor‐pronator tendon disruption, fascial compression syndrome, UCL instability, valgus extension overload, ulnar neuropathy, subluxating ulnar nerve, and medial antebrachial cutaneous nerve injury.17
Medial elbow pathology is often linked to the posteromedial compartment. Cadaveric biomechanical studies18,19 have confirmed the relation between the UCL and the posteromedial articulation by showing altered contact with increasing UCL insufficiency. In an in vitro cadaveric study, an increase in flexion angle, an increase in valgus torque, and resection of ⩾ 6 mm led to an increase in strain in the anterior bundle of the medial collateral ligament.19 The non‐uniform change in strain related to 3 mm of resection suggests that resections of the posteromedial aspect of the olecranon >3 mm may jeopardise the function of the anterior bundle.19 Clinically, a similar relation between the posteromedial compartment and the UCL has been reported; after resection of elbow posteromedial osteophytes in baseball pitchers, as many as 25% required UCL reconstruction.20 Thus treating bony impingement with osteotomy may convert an asymptomatic medially lax elbow into an unstable painful elbow. Alternatively, the UCL may be insufficient but clinically stable secondary to osteophyte formation. In fact, several studies have shown that lesions of the posterior compartment, including olecranon osteophytes and loose bodies, are the most common diagnoses that require surgery in baseball players.20,21,22 Therefore, to accurately assess the degree of UCL stability, every UCL should be evaluated in patients who present with posteromedial elbow pain.
Clinical presentation of UCL injury involves medial elbow pain, typically chronic and episodic more often than acute. Symptoms of instability are seldom reported by patients. However, for 85% of the time, pain is associated with the acceleration phase of throwing21 after an inadequate warm up period. Patients may report a previous history of pain and subsequent corticosteroid injection. A “pop” may be heard or felt if the injury is acute. On the contrary, if the injury is chronic, pitchers report diminished accuracy, velocity, control, stamina, and/or strength. Finally, chronic valgus stress at the elbow can lead to a traction neuropraxic injury to the ulnar nerve. Clinical reports indicate a 40% incidence of ulnar neuritis, most commonly limited to sensory changes.17
Examination
The neck and upper extremities should be evaluated during the physical examination as cervical spine, shoulder, back, and/or lower extremity pathology may contribute to poor mechanics and lead to the development of elbow problems. Specific to the thrower's elbow, flexion contractures are common in elite level pitchers. The incidence approaches 50%.13 Flexion contractures are believed to be an adaptive change to the valgus extension overload sustained at the elbow during repetitive throwing, secondary to hypertrophy of the soft tissue and osseous structures in the posterior elbow, which typically do not affect performance if less than 25°.21
Specific tests to evaluate the integrity of the UCL include: the valgus stress test9,23; the milking test11; the moving valgus stress test.17 These tests are positive if they reproduce either medial elbow pain or increased laxity >1 mm.9 Pain is more commonly elicited and has been found to have a greater interobserver reliability than laxity.17,21 Valgus instability is difficult to elicit on manual testing, and therefore comparison with the contralateral elbow is essential to differentiate physiological from pathological laxity.23
The initial imaging series should include anterior‐posterior, lateral, and 110° oblique radiographic views. Additional studies include stress radiographs, magnetic resonance imaging, computed tomography arthrogram, and ultrasound. Computed tomography arthrograms are the most accurate for detecting partial undersurface UCL tears, visualised as the “T sign”. The usefulness of each of these modalities has been scrutinised. For example, with respect to stress radiographs, an increase in opening >0.5 mm is considered indicative of UCL injury, but reports of increased medial laxity in uninjured pitchers have prevented establishment of standard normal values.23
Arthroscopy can be used to identify and remove loose bodies as well as offer visualisation of ligamentous pathology. Through the anterolateral portal, 20–30% of the anterior band is visible. A valgus stress test may be performed under arthroscopic visualisation to confirm suspicion of a UCL tear. Fresh‐frozen cadaveric elbows have been used to evaluate the extent to which the medial collateral ligament must be injured before arthroscopic evidence of valgus instability is seen, the amount of ulnohumeral joint opening that occurs after such an injury, and the elbow position that maximises visualisation of this opening.25 With the elbow flexed to 90° and the forearm pronated, the test is positive if valgus stress leads to >1–2 mm articular opening between the humerus and ulna.25 The entire anterior bundle of the UCL must be cut to demonstrate instability.25
Non‐operative treatment
In most situations, non‐throwing athletes and low demand patients are treated non‐operatively. The general principles are to offer palliative modalities that minimise pain and inflammation, subsequently focusing on an extensive and graduated rehabilitation regimen stressing flexibility and strengthening. Acutely, early rehabilitation focuses on stretching and strengthening the flexor‐pronator mass, rotator cuff, and scapular stabilisers to control pain and inflammation in the injured elbow. When symptoms resolve, an interval throwing programme is initialised and progressed towards the goal of returning to competitive play.26
Physiotherapy consists of a progressive and comprehensive elbow and shoulder programme. Clinical research has found that the elbow serves as a link in the kinetic chain of force development, regulation, and transfer.27 Thus the risk of elbow injury is minimised when all the components of this kinetic chain, such as the shoulder, efficiently function to optimise performance.
The flexor carpi ulnaris (FCU), more so than the flexor digitorum superficialis, is optimally positioned to provide direct in line support to the UCL.14 In addition, an in vitro biomechanical analysis generated kinematic data that confirm that the flexor‐pronator mass, primarily the FCU, serves as a dynamic stabiliser.15 Electromyography studies have shown decreased activity of the pronator teres and FCU in pitchers with UCL insufficiency.28 The results of these studies offer credence to the theory that flexor‐pronator mass injury occurs before or concurrently with UCL injury. Consequently, strengthening of this musculature will optimise its dynamic role, thereby decreasing the risk of future injury.
A biomechanical analysis of throwing skills16 provided invaluable insight into the protective role of the shoulder. Shoulder internal rotation provided the largest contribution to the varus counter torque at the elbow. Specifically the loads generated are 64 N.m of varus torque at the elbow and 67 N.m of internal rotation torque and 310 N of anterior force at the shoulder.10 Consequently, it is the combination of shoulder internal rotation and forearm pronation that forms the physiological basis of the varus counter torque that combats the enormous valgus elbow load generated during the late cocking phase of overhead throwing.
The results of non‐operative treatment in the lower demand patient cohort and non‐throwing athlete show that such treatment arrests the progression of instability and functional impairment.29 In fact, in a retrospective review of the National Football League from 1991 to 1995, 100% (18/18) of players with UCL injuries (four receivers, ten linemen, two running backs, and two quarterbacks) were successfully treated non‐operatively.30 The mean time lost was 0.64 games.30
Similar success rates, however, have not been seen in the non‐operative treatment of higher demand overhead throwing athletes. Barnes and Tullos reported that 50% of 100 symptomatic throwing athletes returned to play.31 Rettig et al32 found that only 42% of 31 overhead throwing athletes (20 pitchers, nine infielders, and two javelin throwers) returned to play an average of 24.5 weeks after diagnosis. The mean age of these athletes was 18 years; the mean follow up in this study was 2.5 years.
Operative management
Surgical indications include: (a) throwing athletes with a complete UCL tear; (b) partial tears that have failed rehabilitation; (c) symptomatic non‐throwing athletes after a minimum of three months of rehabilitation.7,17,21,33 Current surgical options include reconstruction or direct repair. Reconstruction is the most widely accepted surgical modality today,21,33 whereas direct repair is typically only considered in the presence of an acute traumatic avulsion.34
Repair
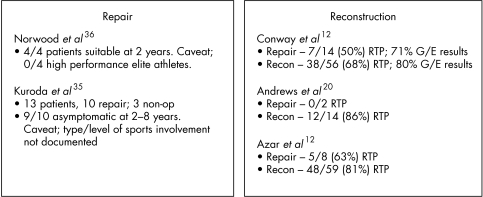
Early studies support UCL repair; the applicability of these studies to the current patient population is limited because they did not include high performance elite athletes or document the type/level of sports involvement.35,36 Thus application of these findings to the treatment of overhead throwing athletes is difficult. Numerous recent comparisons have found UCL reconstruction to be more effective than direct repair in correcting medial elbow instability and returning overhead throwing athletes to a preinjury level of play in less than one year.6,12,20Figure 1 details a comprehensive quantitative comparison of all the studies to date that document the success of UCL repair versus reconstruction.
Figure 1 Comparison of repair versus reconstruction for ulnar collateral ligament injury. RTP, Return to preinjury level of play; Recon, reconstruction.
Reconstruction
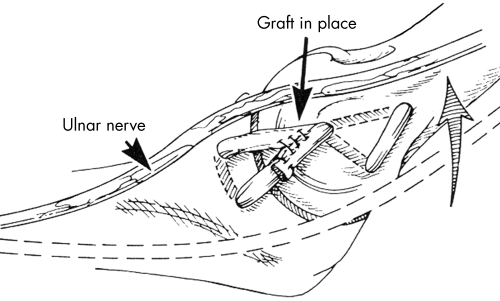
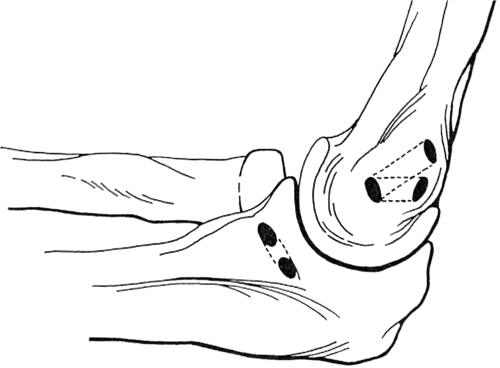
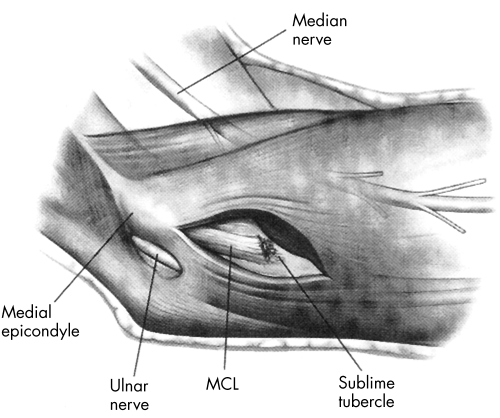
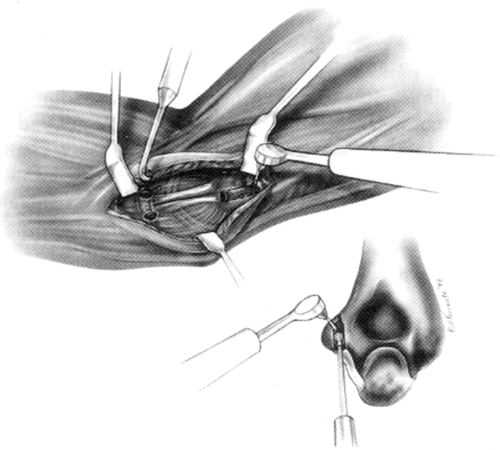
In the original UCL reconstruction, the flexor‐pronator mass was detached and elevated from the medial epicondyle of the humerus and a submuscular ulnar nerve transposition (UNT) was performed (fig 2). The anterior bundle of the UCL was reconstructed with a harvested autograft in a figure of eight fashion through two drill holes in the ulna and three in the medial epicondyle; the posterior cortex of the humerus was penetrated, and the graft was sutured to itself (fig 3).
Figure 2 Jobe technique: anterior ulnar nerve transposition.
Figure 3 Jobe technique: bone tunnels.
The palmaris longus is the most common graft. Typically 15–17 cm is needed.37 Its use is supported by biomechanical studies,38 which document a failure load (357 N) greater than that of the anterior bundle of the UCL (260 N). Minimal morbidity is associated with its removal; however, the surgeon must avoid damaging the adjacent median nerve. Azar et al6 found that the compromise of using the ipsilateral palmaris longus on pitching mechanics is minimal.
In 1986, Dr Jobe published his landmark article7. At a minimum two year follow up, 63% of 16 elite throwing athletes returned to a preinjury level of throwing for at least one year. Of the remaining six, one had returned to a lower level, and five had quitted the sport, despite a lack of instability or pain. However, despite the ground breaking success of this procedure, the rate of complications was high at 31%. Postoperative dysfunction of the ulnar nerve was the most commonly cited complication. Two of five patients with ulnar neuropathy required a secondary decompression.
A subsequent larger study of 71 patients was published in 1992.12 The UCL was directly repaired in 14 patients and reconstructed with an autograft in the 56 others. At a follow up period of 2–15 years, 68/71 (96%) were available for postoperative evaluation. Half of those patients treated with a direct repair had returned to a preinjury level of play after a mean period of nine months. In comparison, 68% of those managed with reconstruction had returned to the same level of sport after a mean period of 12 months. Postoperative ulnar nerve dysfunction occurred in 21%. Nine of these 15 patients subsequently required revision decompression. At an average follow up period of three to eight years, five complained of persistent ulnar nerve paresthesias, and one had distinct wasting of the intrinsic musculature.
Publication of these results prompted the natural development of surgical modifications to simplify the technique, evade dissection and detachment of the flexor‐pronator mass, and limit handling of the ulnar nerve.
Muscle splitting
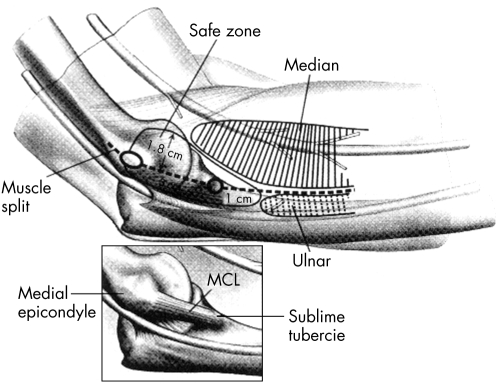
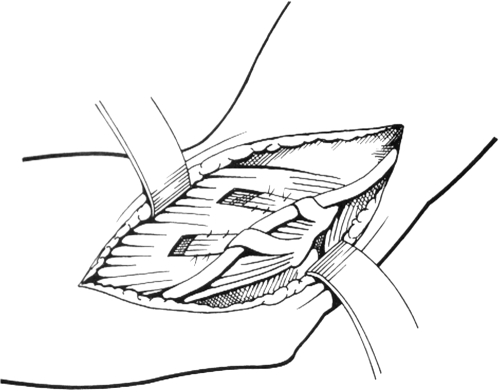
In 1996, Smith et al39 described the “safe zone” of the medial elbow—that is, an internervous plane of exposure to the medial ulnohumeral articulation (fig 4) which extends from the medial epicondyle to 1 cm distal to the insertion of the UCL on the sublime tubercle of the ulna, between the medial and ulnar nerve sites of innervation of surrounding muscles (fig 5). It involves a muscle split through the posterior third of the common flexor bundle—that is, the most anterior fibres of the FCU.
Figure 4 Muscle splitting approach: internervous plane. MCL, Medial collateral ligament.
Figure 5 Muscle splitting approach. MCL, Medial collateral ligament.
In the series of 22 patients reported by Smith et al,39 there were neither neuropathies nor denervations at a minimum follow up of one year. Follow up examinations averaged two years and two months (range 13 months to 4 years). The proposed advantages of this approach are: take down of the flexor‐pronator mass is avoided; the UCL is under the anterior FCU; “routine” UNT is avoided.
The clinical results of this operative technique were reported in a larger series of 83 UCL reconstructions published five years later.40 The UCL was reconstructed using Jobe's original technique after a muscle splitting dissection without a UNT. In this study, 82% of 33 elite throwers followed up for two years returned to play; this number increased to 93% in patients without prior surgery. This return to competitive play occurred at a mean of 13 months. With regard to associated complications, in the immediate postoperative periods, only 5% of the 83 patients had transient ulnar nerve problems. All of these resolved without surgery.
Biomechanical studies41 have been performed to test the stability of the elbow to valgus stress before and after reconstruction of the UCL using the Jobe technique and muscle splitting approach. Each of the 14 cadaveric specimens was secured in a materials test frame, and a 5 N.m valgus moment was applied in 30°, 60°, 90°, and 120° of flexion. The stability was measured at baseline, after the anterior bundle had been sectioned, and again after the UCL had been reconstructed using the Jobe technique. The only significant difference between intact and reconstructed samples was at 120°.
American Sports Medicine Institute (ASMI) modification
Andrews and colleagues6,8,20 modified Jobe's original technique by retracting the FCU anteriorly and by performing a subcutaneous, not submuscular, UNT (fig 6).
Figure 6 ASMI modification.
Azar et al6 published the results of Andrews et al in a retrospective review comparing UCL reconstruction with repair in 91 throwing athletes performed by a single surgeon over a six year period. All patients were male; age range was 15–39 years (mean 21.6 years). Thirteen patients had a direct repair, and the remaining 78 were managed with reconstruction. At a follow up of one to six years (mean 35.4 months), 67 (eight repairs, 59 reconstructions) were available for postoperative evaluation. More than three quarters (79%) managed with reconstruction returned to a preinjury level of play an average of 9.8 months after surgery. In comparison, after the same time period, 63% of those patients treated with a direct repair returned to the same level of sport. Only one had transient postoperative ulnar nerve changes. In fact, nine out of ten patients with preoperative ulnar neuritis experienced resolution.
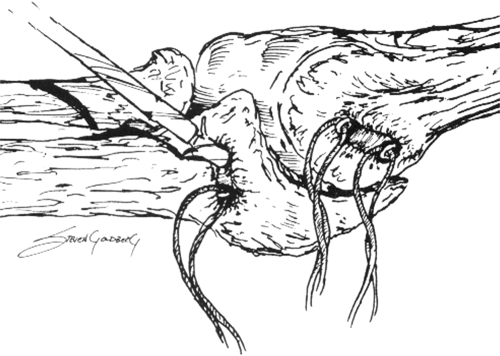
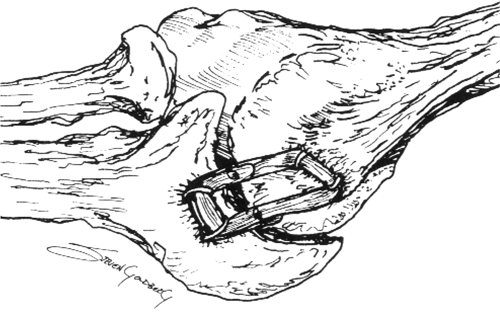
Suture anchor method
In the mid 1990s, suture anchors were introduced in an attempt to further simplify UCL reconstruction (figs 7 and 8). In a cadaveric study by Hechtman et al,42 31 specimens were used: 15 underwent reconstruction with the use of bone tunnels and 16 with suture anchors. The strength of each reconstruction was compared with the original strength of the elbow. The following results were found: (a) no significant difference in reconstruction strength between suture anchor (76.3%) and bone tunnel (63.9%); (b) suture anchors reproduced normal UCL anatomy and mechanical function more closely than bone tunnels; (c) both methods produced reconstructions that were significantly weaker than the intact UCL.
Figure 7 Suture anchor technique: placement of anchors.
Figure 8 Suture anchor technique: graft incorporation.
Despite the apparent success of this cadaveric work, this technique was reportedly terminated when clinical application yielded a failure rate of 30%.43 Yet it determined that graft tension and placement within the bony tunnel are the key determinants of a successful reconstruction.
A modification of this technique using hybrid suture anchor fixation has recently been presented at the 24th Annual Meeting of the Arthroscopy Association of North America by members of the UHZ Sports Medicine Institute. Tendon graft is fixed through osseous tunnels at the sublime tubercle of the ulna and attached with either one or two suture anchors at the humeral origin of the native ligament.
Docking technique
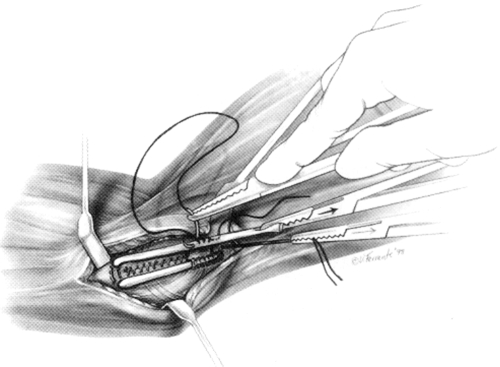
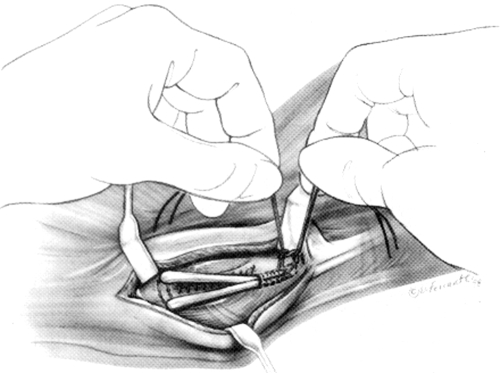
In 1996 Altchek et al44 first used a muscle splitting approach to modify UCL reconstruction in a technique called the “docking procedure”. Unlike Jobe's technique, in which the graft is placed in a figure of eight position, in this technique the graft is placed in a triangular configuration through a single humeral tunnel, and the limbs are brought out through separate bone punctures and tied over a bone bridge (figs 9–11).
Figure 9 Docking technique: tunnel creation.
Figure 10 Docking technique: placement of sutures.
Figure 11 Docking technique: suture limbs tied over bone bridge.
In an uncontrolled retrospective review by Rohrbough et al,44 33/36 (92%) patients returned to a preinjury level of play for at least one year. All of the 36 patients were available for follow up after a mean of 3.3 years. All 22 professional or collegiate athletes returned to or exceeded their previous competition level. Similarly, in an earlier series at the same institution, Hyman et al26 reported a return to preinjury level of 97%.
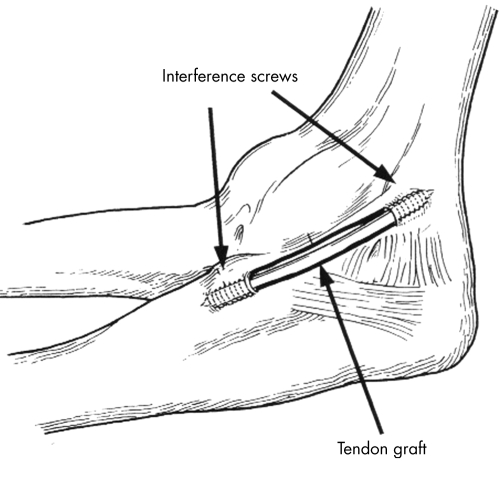
Interference technique
Ahmad and coworkers described an interference technique for fixation of the UCL graft. The goal is to reconstruct the central isometric fibres of the native UCL, which lie between the anterior one third and posterior two thirds of the anterior bundle of the UCL.45 Through a muscle splitting approach, grafts are fixed with interference screws placed in single bony tunnels in the humerus and ulna (fig 12). Unlike Jobe's original technique, only two bone tunnels are needed. The ulnar nerve is less at risk. Likewise, without an intervening bony bridge on the ulna, the risk of tunnel fractures, between the two tunnels, is theoretically eliminated.
Figure 12 Interference technique.
The biomechanical results of this technique are encouraging. In a cadaveric study by Ahmad et al,46 comparing intact with reconstructed elbows using the interference technique, the normal elbow kinematics were restored with UCL reconstruction using interference screw fixation. The failure strength of UCL reconstruction with interference screw fixation (30.55 ± 19.24 N.m) was similar to that of intact UCL (34.29 ± 6.9 N.m).
Lange and Fleischli recently presented a comparison of traditional UCL reconstruction versus interference screw fixation at the 24th Annual Meeting of the Arthroscopy Association of North America. The anterior bundle of the UCL was reconstructed in matched cadaveric elbow pairs using hamstring tendons with a Jobe figure of eight or metal interference screw technique. The biomechanical strength and stiffness of these techniques was compared with submaximal valgus loading at various flexion angles. Neither construct reproduced the overall stiffness of the intact UCL, yet the initial and overall stiffness of the traditional Jobe technique was better than interference screw fixation.
Reconstruction overview
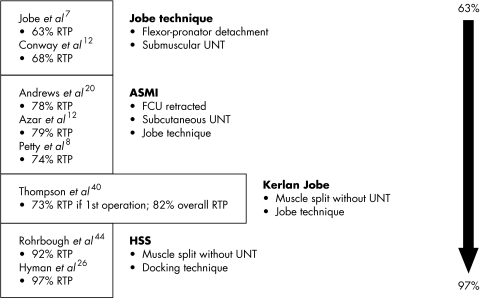
The success rates of reconstruction vary between 63% and 97% depending on the technique (fig 13). Reported complication rates are less than 10%.5 Despite the variability in techniques, the unifying features are that decreased dissection of the flexor‐pronator mass and decreased handling of the ulnar nerve leads to improved outcomes.
Figure 13 Evolution of ulnar collateral ligament reconstruction. UNT, Ulnar nerve transposition; RTP, return to preinjury level of play; FCU, flexor carpi ulnaris; ASMI, American Sports Medicine Institute in Birmingham, Alabama; Kerlan Jobe, Kerlan Jobe Orthopedic Clinic in Los Angeles, California; HSS, Hospital for Special Surgery in New York.
Four UCL reconstruction techniques have been compared biomechanically: (a) the docking procedure; (b) interference screw fixation; (c) figure of eight; (d) single stranded UCL reconstruction using an Endobutton for ulnar fixation. Armstrong et al37 subjected cadaveric specimens to pneumatic valgus loading and found that the peak load to failure of the reconstructed UCL was inferior to that of the intact ligament. No difference in strength was found between the docking and single stranded UCL reconstruction which used an EndoButton. Both of these reconstruction methods were stronger than the interference screw or figure of eight technique.
Ulnar nerve transposition
The original UCL reconstruction described by Jobe7 included submuscular UNT. In 1986, Jobe published his landmark article7; 63% of 16 elite throwing athletes returned to a preinjury level of throwing for at least one year. However, the rate of complications was high at 31%, typically related to postoperative dysfunction of the ulnar nerve. The growing interest surrounding this procedure led to modifications to simplify the technique and decrease handling of the ulnar nerve. For example, the FCU muscle splitting approach39 does not require a routine UNT. The ASMI modification,6 however, involves a subcutaneous, not submuscular, UNT. As previously detailed, both approaches have yielded good results and decreased postoperative complications involving the ulnar nerve.6,39 Current indications for concomitant UNT include preoperative symptoms of ulnar neuritis, intraoperative posterior compartment visualisation which requires dissection into the cubital tunnel, and operative discovery of heavy scar tissue and chronic degenerative change of the ulnar nerve.14,17,21,33
UCL reconstruction in high school baseball players
UCL injury has become a substantial problem in youth pitchers. About 150 reconstructions are carried out a year at the ASMI. According to recent information, 20% are major league pitchers, 20–25% are minor league throwers, and 60% are collegiate and high school athletes. Numerous reasons have been cited, but retrospective analysis reveals overuse to be the predominant risk factor.8
The clinical results of 31 UCL reconstructions performed on high school athletes in 1995–2000 were retrospectively reviewed8: 87% (27/31) were available for follow up; age range was 15.9–19 years (mean 17.4); mean time to surgery was six months after injury; 7% had transient ulnar nerve paresthesias that resolved without surgery; 74% (20/27) returned to preinjury level of play after a mean period of 11 months; 37% (10/27) went on to play collegiate baseball; 26% (7/27) failed to return to preinjury level of play (two retired secondary to continual pain, and four lost interest in the sport and abandoned their rehabilitation programme).
What is already known on this topic
UCL insufficiency is potentially a career threatening, or even a career ending, injury, particularly in overhead throwing athletes
The evolution of treating modalities provides afflicted athletes the opportunity to avoid a premature retirement; UCL reconstruction is currently the most commonly performed surgical treatment option
What this study adds
A comprehensive review and comparative analysis of the present treatment options, both non‐operative and operative, as well as their respective results and biomechanical evaluation, are provided
Despite the various modifications of UCL reconstruction (docking technique, interference screw fixation, use of suture anchors) that have evolved over the last 30 years, the unifying concepts are that decreased dissection of the flexor‐pronator mass and decreased handling of the ulnar nerve lead to improved outcomes
Summary
UCL insufficiency is potentially a career threatening, or even a career ending injury, particularly in overhead throwing athletes. The evolution of treating modalities provides afflicted athletes the opportunity to avoid premature retirement. Success of treatment is defined by most authors as the ability to return to a preinjury level of play for at least one year.6,7,8,12,20,40,44
Non‐throwing athletes and low demand patients are treated non‐operatively. Surgical management is reserved for throwing athletes with a complete UCL tear or those with partial tears that have failed rehabilitation, in addition to non‐throwing athletes who are still symptomatic after a minimum of three months of rehabilitation. The most common surgical option is UCL reconstruction.
Over the last 30 years the original UCL reconstruction has evolved. Yet, despite the variability in modifications, such as the docking technique, interference screw fixation, and use of suture anchors, the unifying concepts of UCL reconstruction are that decreased dissection of the flexor‐pronator mass and decreased handling of the ulnar nerve leads to improved outcomes.
Abbreviations
ASMI - American Sports Medicine Institute
FCU - flexor carpi ulnaris
UCL - ulnar collateral ligament
UNT - ulnar nerve transposition
Footnotes
Competing interests: none declared
References
- 1.Bennett G E. Shoulder and elbow lesions of the professional baseball pitcher. JAMA 1941117510–514. [Google Scholar]
- 2.Tullos H S, King J W. Throwing mechanism in sports. Orthop Clin North Am 19734709–720. [PubMed] [Google Scholar]
- 3.King J W, Brelsford H, Tullos H S. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop 196967116–123. [PubMed] [Google Scholar]
- 4.Schwab G H, Bennet J B, Woods G W.et al The biomechanics of elbow stability: the role of the medial collateral ligament. Clin Orthop 198014642–52. [PubMed] [Google Scholar]
- 5.Safran M R. Ulnar collateral ligament injury in the overhead athlete: diagnosis and treatment. Clin Sports Med 200423643–663. [DOI] [PubMed] [Google Scholar]
- 6.Azar F M, Andrews J R, Wilk K E.et al Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med 20002816–23. [DOI] [PubMed] [Google Scholar]
- 7.Jobe F W, Stark H, Lombardo S J. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg [Am] 1986681158–1163. [PubMed] [Google Scholar]
- 8.Petty D H, Andrews J R, Fleisig G S.et al Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004321158–1164. [DOI] [PubMed] [Google Scholar]
- 9.Wilson F D, Andrews J R, Blackburn T A.et al Valgus extension overload in the pitching elbow. Am J Sports Med 19831183–88. [DOI] [PubMed] [Google Scholar]
- 10.Fleisig G S, Andrews J R, Dillman C J.et al Kinetics of baseball pitching with implications about injury mechanism. Am J Sports Med 199523233–239. [DOI] [PubMed] [Google Scholar]
- 11.Morrey B F, An K N. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med 198311315–319. [DOI] [PubMed] [Google Scholar]
- 12.Conway J E, Jobe F W, Glousman R E.et al Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg [Am] 19927467–83. [PubMed] [Google Scholar]
- 13.Fleisig G S, Barrentine S W, Zheng N.et al Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech 1999321371–1375. [DOI] [PubMed] [Google Scholar]
- 14.Jobe F W, Kvitne R S. Elbow instability in the athlete. Instr Course Lect 19914017–23. [Google Scholar]
- 15.Park M C, Ahmad C S. Dynamic contributions of the flexor‐pronator mass to elbow valgus stability. J Bone Joint Surg [Am] 2004862268–2274. [DOI] [PubMed] [Google Scholar]
- 16.Marshall R N, Elliott B C. Long‐axis rotation: the missing link in proximal‐to‐distal segmental sequencing. J Sports Sci 200018247–254. [DOI] [PubMed] [Google Scholar]
- 17.David T S. Medial elbow pain in the throwing athlete. Orthopedics 20032694–103. [DOI] [PubMed] [Google Scholar]
- 18.Ahmad C S, Park M C, Elattrache N S. Elbow medial ulnar collateral ligament insufficiency alters posteromedial olecranon contact. Am J Sports Med 2004321607–1612. [DOI] [PubMed] [Google Scholar]
- 19.Kamineni S, ElAttrache N S, O'Driscoll S W.et al Medial collateral ligament strain with partial posteromedial olecranon resection. A biomechanical study. J Bone Joint Surg [Am] 2004862424–2430. [DOI] [PubMed] [Google Scholar]
- 20.Andrews J R, Timmerman L A. Outcome of elbow surgery in professional baseball players. Am J Sports Med 199523407–413. [DOI] [PubMed] [Google Scholar]
- 21.Chen F S, Rokito A S, Jobe F W. Medial elbow problems in the overhead‐throwing athlete. J Am Acad Orthop Surg 2001999–113. [DOI] [PubMed] [Google Scholar]
- 22.Kooima C L, Anderson K, Craig J V. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med 2004321602–1606. [DOI] [PubMed] [Google Scholar]
- 23.Ellenbecker T S, Mattalino A J, Elam E A.et al Medial elbow joint laxity in professional baseball pitchers. A bilateral comparison using stress radiography. Am J Sports Med 199826420–424. [DOI] [PubMed] [Google Scholar]
- 24.O'Driscoll S W, Lawton R L, Smith A M. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med 200533231–239. [DOI] [PubMed] [Google Scholar]
- 25.Field L D, Altchek D W. Evaluation of the arthroscopic valgus instability test of the elbow. Am J Sports Med 199624177–181. [DOI] [PubMed] [Google Scholar]
- 26.Hyman J, Breazeale N M, Altchek D W. Valgus instability of the elbow in athletes. Clin Sports Med 20012025–45. [DOI] [PubMed] [Google Scholar]
- 27.Kibler B W, Sciascia A. Kinetic chain contributions to elbow function and dysfunction in sports. Clin Sports Med 200423545–52, viii. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton C D, Glousman R E, Jobe F W.et al Dynamic stability of the elbow: electromyographic analysis of the flexor pronator group and the extensor group in pitchers with valgus instability. J Shoulder Elbow Surg 19965347–354. [DOI] [PubMed] [Google Scholar]
- 29.Miller C D, Savoie F H., III Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg 19942261–269. [DOI] [PubMed] [Google Scholar]
- 30.Kenter K, Behr C T, Warren R F.et al Acute elbow injuries in the National Football League. J Shoulder Elbow Surg 200091–5. [DOI] [PubMed] [Google Scholar]
- 31.Barnes D A, Tullos H S. An analysis of 100 symptomatic baseball players. Am J Sports Med 1978662–67. [DOI] [PubMed] [Google Scholar]
- 32.Rettig A C, Sherrill C, Snead D S.et al Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med 20012915–17. [DOI] [PubMed] [Google Scholar]
- 33.Cain E L, Dugas J R, Wolf R S.et al Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med 200331621–635. [DOI] [PubMed] [Google Scholar]
- 34.Salvo J P, Rizio L, 3rd, Zvijac J E.et al vulsion fracture of the ulnar sublime tubercle in overhead throwing athletes. Am J Sports Med 200230426–431. [DOI] [PubMed] [Google Scholar]
- 35.Kuroda S, Sakamaki K. Ulnar collateral ligament tears of the elbow joint. Clin Orthop Relat Res 1986208266–171. [PubMed] [Google Scholar]
- 36.Norwood L A, Shook J A, Andrews J R. Acute medial elbow ruptures. Am J Sports Med 1981916–19. [DOI] [PubMed] [Google Scholar]
- 37.Armstrong A D, Dunning C E, Ferreira L M.et al A biomechanical comparison of four reconstruction techniques for the medial collateral ligament‐deficient elbow. J Shoulder Elbow Surg 200514207–215. [DOI] [PubMed] [Google Scholar]
- 38.Regan W D, Korinek S L, Morrey B F.et al Biomechanical study of ligaments around the elbow joint. Clin Orthop 1991271170–179. [PubMed] [Google Scholar]
- 39.Smith G R, Altchek D W, Pagnani M J.et al A muscle splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am J Sports Med 199624575–580. [DOI] [PubMed] [Google Scholar]
- 40.Thompson W H, Jobe F W, Yocum L A.et al Ulnar collateral ligament reconstruction in throwing athletes: muscle‐splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg 200110152–157. [DOI] [PubMed] [Google Scholar]
- 41.Mullen D J, Goradia V K, Parks B G.et al A biomechanical study of stability of the elbow to valgus stress before and after reconstruction of the medial collateral ligament. J Shoulder Elbow Surg 200211259–264. [DOI] [PubMed] [Google Scholar]
- 42.Hechtman K S, Tjin‐A‐Tsoi E W, Zvijac J E.et al Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am J Sports Med 199826620–624. [DOI] [PubMed] [Google Scholar]
- 43.Williams R J, Urquhart E R, Altchek D W. Medial collateral ligament tears in the throwing athlete. Instr Course Lecture 200453579–586. [PubMed] [Google Scholar]
- 44.Rohrbough J T, Altchek D W, Hyman J.et al Medical collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med 200230541–548. [DOI] [PubMed] [Google Scholar]
- 45.Ochi N, Ogura T, Hashizume H.et al Anatomic relation between the medial collateral ligament of the elbow and the humeroulnar joint axis. J Shoulder Elbow Surg 199986–10. [DOI] [PubMed] [Google Scholar]
- 46.Ahmad C S, Lee T Q, ElAttrache N S. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med 200331332–337. [DOI] [PubMed] [Google Scholar]