Abstract
Objectives
To describe and compare the medium to long‐term effectiveness of hydrodilatation and post‐hydrodilatation physiotherapy in patients with primary and secondary glenohumeral joint contracture associated with rotator cuff pathology.
Methods
Patients with primary and secondary glenohumeral contractures associated with rotator cuff pathology were recruited into a 2‐year study. They all underwent hydrodilatation, followed by a structured physiotherapy programme. Patients were assessed at baseline, 3 days, 1 week, 3 months, 1 year and 2 years after hydrodilatation with primary outcome measures (Shoulder Pain and Disability Index, Shoulder Disability Index and percentage rating of “normal” function; SD%) and secondary outcome measures (range of shoulder abduction, external rotation and hand behind back). Comparisons in recovery were made between the primary and secondary glenohumeral contracture groups at all timeframes and for all outcome measures.
Results
A total of 53 patients (23 with primary and 30 with secondary glenohumeral contractures) were recruited into the study. At the 2‐year follow‐up, 12 patients dropped out from the study. At baseline, the two contracture groups were similar with respect to their demographic and physical characteristics. The two groups of patients recovered in a similar fashion over the 2‐year follow‐up period. A significant improvement was observed in all outcomes measures over this period (p<0.01), so that both function and range of movement increased. The rate of improvement was dependent on the outcome measure that was used.
Conclusions
Hydrodilatation and physiotherapy increase shoulder motion in individuals with primary and secondary glenohumeral joint contracture associated with rotator cuff pathology. This benefit continues to improve or is maintained in the long term, up to 2 years after hydrodilatation.
The stiff, painful shoulder is one of the most common conditions of the shoulder,1 yet there is little consensus regarding its cause, classification or optimal treatment. Often, the assumption is made that a stiff, painful shoulder is the same as a “frozen shoulder”; however, this seems to be an umbrella term with little consensus regarding the diagnostic criteria for this disorder.2,3 Thus, many clinicians suggest that the stiff and painful shoulder should be classified into glenohumeral joint contracture types, such as primary and secondary contracture,2,3,4,5,6 based on the history regarding the onset of shoulder pain and stiffness.
Many treatment options have been proposed for glenohumeral joint contractures, irrespective of the type of contracture. These include exercise, physiotherapy, manipulation under anaesthetic, glucocorticosteroid injections and oral treatment, hydrodilatation and arthroscopic release in refractory cases.7,8,9 However, there is a paucity of data to support the efficacy of these interventions.10,11 Previous studies have often lacked explicit inclusion and exclusion criteria, failed to consider the type or degree of shoulder stiffness and have not described the method used or psychometric properties (validity, reliability and responsiveness) of the outcome measures. Hence, there is no consensus regarding the most appropriate treatment for glenohumeral joint contracture.
Hydrodilatation, sometimes referred to as distension arthrography, has been proposed as a therapeutic procedure for glenohumeral joint contracture.7,12,13,14 It is proposed that its benefits are derived from a combination of the anti‐inflammatory effect of cortisone with the mechanical effect of joint distension (reflected by radiological distension of the subscapularis bursa), thereby reducing the stretch on pain receptors in the glenohumeral joint capsule and its periosteal attachments.15 Hydrodilatation was first used by Andren and Lundberg16 in 1965, who reported variable results ranging from extremely effective to extremely painful. More recent studies have also cited variable results.7,8,12,13,14,15,17,18,19 This may be a consequence of varying hydrodilatation techniques and post‐hydrodilatation treatment regimens (such as physiotherapy), small sample sizes, lack of explicit inclusion criteria and variable methods of outcome measurement. Despite these limitations, most authors conclude that hydrodilatation has a role in the treatment of glenohumeral joint contracture,7,8,12,13,14,15,17,18,19 on the basis of results of short‐term studies (<3 months duration). The aim of medical and allied health treatment is to increase functional capacity of individuals in the long term. Thus, it is imperative that hydrodilatation is further investigated to determine its long‐term effectiveness in individuals with both primary glenohumeral joint contracture and secondary shoulder stiffness, as this is representative of the patient population frequently seen in clinical practice.2,6,20,21
This study aims to describe and compare the long‐term effectiveness (up to 2 years) of hydrodilatation and post‐hydrodilatation physiotherapy in patients and secondary glenohumeral joint stiffness associated with rotator cuff pathology. A secondary aim was to investigate whether the pre‐hydrodilatation range of motion (external rotation, abduction and hand behind the back) predicted outcome after hydrodilatation, as these motions are often used in clinical practice as measures of the extent of glenohumeral joint restriction.2,3,7 As such, a longitudinal, cohort study design was used to meet these aims.
Patients and methods
Patient selection
Patients were recruited over a 6‐month period from those presenting for a medical consultation for their shoulder problems, to either the Melbourne Orthopaedic Group, Windsor, Victoria, Australia, or Lifecare Prahran Sports Medicine Centre, Prahran, Victoria, Australia. An independent medical officer (either an orthopaedic surgeon or a sports physician) assessed each patient for eligibility to participate in the study. All medical officers (n = 4) had extensive experience treating patients with glenohumeral joint contractures. Patients were assessed using a standard battery of clinical tests and radiological examinations (box 1). Those patients who met the selection criteria were invited to participate in the study (box 2). Those who agreed to participate signed a consent form before the start of the study.
On the basis of the results of the clinical tests, patients were classified as having either primary or secondary glenohumeral joint contracture. For the purpose of this study, primary glenohumeral joint contracture was defined as an idiopathic condition with spontaneous onset of pain, no or minor incident precipitating onset of pain (eg, reaching into back seat of car), restricted active/passive restriction of movement >2 planes.2,3 Secondary glenohumeral joint contracture was defined as a stiff and painful shoulder with restricted active/passive restriction of movement >2 planes with an identifiable cause that may be associated with the development of restricted motion—for example, rotator cuff disease.2,3,4,5 Table 1 lists the underlying pathologies in patients with secondary contracture included in this study. The initial intent of this study was to examine the several subgroups of secondary glenohumeral joint contracture (such as contracture due to rotator cuff pathology and fracture). However, owing to insufficient patient numbers, only patients with rotator cuff pathology were included in this study.
Table 1 Pathology of patients presenting with secondary glenohumeral joint contracture.
| Type of pathology | Number of patients |
|---|---|
| Impingement | 6 |
| Rotator cuff tears | |
| Partial thickness | 4 |
| Full thickness | 4 |
| Degenerative cuff signs | |
| Calcific tendinosis | 2 |
| Enthesopathy and degeneration | 14 |
Box 1 Clinical and radiological tests to determine subject eligibility
Clinical examination
Subjective assessment and history
Localisation of the area of tenderness from palpation
Active/passive shoulder range of motion
-
Resisted rotator cuff tests (for a full discussion of test sensitivity/specificity refer to the sighted article)
Radiological examination
All radiological examinations were performed by the one senior radiologist (FB)
Ultrasound
X Ray.
Note: During the passive examination, care was taken to passively stabilise the scapula while the glenohumeral joint was examined to ensure restriction of glenohumeral joint range of motion was not missed.
Once patients were recruited into the study, they were assessed by the same, independent assessor (a physiotherapist) who was blinded to the glenohumeral joint contracture type. Patients were assessed by the same independent assessor at baseline (before hydrodilatation), 3 days, 1 week, 3 months, 1 year and 2 years after hydrodilatation, using the same outcome measures in a standardised order.
Outcome measures
A variety of outcome measures were used in this study, as there is no gold standard outcome assessment battery for glenohumeral joint contracture and results can substantially differ depending on the outcome measure used.29,30 Outcome measures selected were based on accepted and widely used tests in clinical practice and research, and consisted of evaluation of the functional capacity of the individual and shoulder range of motion. A separate assessment of shoulder pain was not undertaken in this study to reduce respondent burden. Moreover, an evaluation of pain is included in the Shoulder Pain And Disability Index (SPADI),31 one of the primary outcome measures.
Primary outcome measures
Functional capacity was considered as the primary outcome after hydrodilatation. This was assessed by each subject completing:
The SPADI, which provides a combined score for functional capacity and pain. It has acceptable test–retest reliability and responsiveness in patient31,32 and normal populations.33
The Shoulder Disability Index (SDI), which assesses functional capacity only,10 has acceptable reliability, validity and responsiveness in patient populations.33
A self‐rating of function of their affected shoulder, as a percentage of the contralateral, “normal” shoulder (SD%). This outcome measure is often used in clinical practice as a generic indicator of function/recovery and has acceptable face validity.34
Secondary outcomes
Active range of shoulder external rotation, abduction and hand behind the back were selected as secondary outcomes as they assess the integrity of the glenohumeral joint capsule and are the motions most often cited in the literature as being restricted in glenohumeral joint contracture.2,3,7 The range of motion of shoulder external rotation was measured with the arm resting by the participant's side using a gravity inclinometer according to standardised protocols.35 Hand behind back was measured by recording the level of the spinous process the patients could touch with their thumb. Using these standardised protocols, these measurements have high intrarater reliability in a mixed shoulder patient population.35
Hydrodilatation technique
All patients underwent hydrodilatation performed by the same senior radiologist (FB) using a technique developed by two of the senior authors (RD and FB). Using an aseptic technique, a 21‐gauge spinal needle was inserted into the glenohumeral joint, via an anterior approach. The intra‐articular position of the needle was confirmed with a small amount of air or radio‐opaque contrast medium. Volumes of 1 ml of Kenacort A‐40 (triamcinolone acetonide) and 10 ml bupivacaine 0.5% were injected. Sterile sodium chloride 0.9% was then injected, with progressive distension of the capsule being monitored with fluoroscopy. Distension was continued until there was full distension of the subscapular bursa, rupture down the long head of biceps sheath or the procedure was terminated because it was too painful. Capsular distension was recorded by two methods: (1) volume of sodium chloride injected and (2) subjective rating by the radiologist of the distension on a four‐point ordinal scale: none, poor, good and excellent (referring to the distension achieved of both the axillary recess and the subscapular bursa).
Box 2 Eligibility criteria (inclusion and exclusion) for participating in the study.
-
Inclusion criteria:
-
-
Symptoms of pain and stiffness in predominantly one shoulder for 6 weeks
-
-
Restriction of passive motion of shoulder in ⩾2 planes of movement, measured to onset of pain with a gravity inclinometer
-
-
Adults 18 years of age
-
-
Patients consenting to hydrodilation
-
-
Patients were likely to undergo hydrodilatation and physiotherapy programme
-
-
-
Exclusion criteria:
-
-
Systemic inflammatory disease (including rheumatoid and osteoarthritis, polymyalgia rheumatica)
-
-
Glenohumeral joint arthritis
-
-
Diabetes
-
-
Tumour
-
-
Contraindications to arthrogram and/or hydrodilatation such as warfarin therapy; allergy to local anaesthetic or iodinated contrast
-
-
Pregnancy
-
-
Acute trauma, fracture or shoulder surgery incomplete data that is required to classify the type of glenohumeral joint contracture.
-
-
Post‐hydrodilatation protocol
After hydrodilatation, patients were instructed to rest their arm freely by their side for 2 days and avoid loaded or overhead activities. They then started a standardised physiotherapy programme to increase the function and to normalise the range of motion (appendix 1, available as supplementary material on http://bjsm.bmj.com/supplemental). Physiotherapy continued once a week (30 min sessions) for 8 weeks after hydrodilatation, and then as deemed necessary by the physiotherapist. Six physiotherapists, who were experienced manual therapists, delivered all treatments. All therapists underwent extensive training with a senior therapist (LW) regarding use of the standardised physiotherapy protocol (appendix 1).
Statistical analysis
All data were analysed using SPSS V.13.13 Descriptive statistics were used to describe the demographic characteristics of the sample, the type of glenohumeral joint contracture and the extent of hydrodilatation (amount of fluid injected, subjective rating of joint and subscapularis bursa distension).
Patients who failed to complete data collection were noted over the 2‐year period of assessment. Where possible, comparisons were made between those who dropped out and those who completed the study. Demographic characteristics, pre‐hydrodilatation outcomes measures and the extent of hydrodilatation were also compared for the primary and secondary glenohumeral joint contracture groups using the χ2 statistic and independent t tests or their non‐parametric equivalents. The level of significance was set at p<0.05. Comparisons, using independent t tests, were also made between contracture groups at each time of assessment for each outcome measure, to determine whether the classification of glenohumeral joint contracture influenced outcome. As multiple comparisons were made, the level of significance was set at p<0.01.
To document recovery after hydrodilatation, with physiotherapy, a repeated‐measures analysis of variance was used to determine the change in each of the outcome measures over time. A significant change was identified by p<0.05. Post hoc analyses (paired t tests) were subsequently used to determine the periods of time when significant change occurred. The critical value was set at p<0.01.
To investigate whether outcome of hydrodilatation can be predicted by pre‐hydrodilatation range of motion, Pearson correlation coefficients were calculated for primary outcome measures at 3 months, 1 year and 2 years after hydrodilatation. The strength of association was classified according to Munro36 as 0–0.25, little association; 0.26–0.49, weak association; 0.5–0.69, moderate association; 0.7–0.89, strong association; 0.9–1, very strong association.
Results
Fifty three patients participated in this study. At the 2‐year assessment, 12 participants had dropped out of the study. Four subjects who failed to complete the study reported that they were better and did not wish to continue in the study. Eight subjects declined to complete the primary outcome measures owing to time or travel constraints. There were no significant differences in demographic characteristics, primary outcomes, pre‐hydrodilatation outcome measures and intra‐hydrodilatation findings, and pre‐hydrodilatation on status between individuals who had dropped out and those who completed the study at 2 years after hydrodilatation, except for dominance of injury. Subjects who dropped out of the study were more likely to have injured their dominant shoulder compared with those who completed the study (χ2 = 4.7, p = 0.04). Moreover, there was an almost even spread of drop‐outs between the primary and secondary glenohumeral contracture groups.
Comparison of baseline measures per type of shoulder stiffness
At baseline, there was an almost even spread of subjects between the contracture groups, with 23 (43%) diagnosed with primary glenohumeral contracture and 30 (57%) with secondary shoulder stiffness. Table 2 illustrates that before hydrodilatation there were no significant differences between individuals with primary and secondary glenohumeral joint contractures, with respect to sex, demographic or hydrodilatation variables, other than dominance of injury. Individuals with primary glenohumeral joint contracture more frequently reported symptoms in their non‐dominant shoulder, whereas those with secondary contracture injured their dominant shoulder (χ2 = 4.7, p = 0.04).
Table 2 Comparison of primary and secondary contracture groups at baseline.
| Primary contracture (n = 23) | Secondary contracture (n = 30) | Difference between contracture groups | |
|---|---|---|---|
| Demographic characteristics | |||
| Sex | |||
| Female (n) | 17 | 21 | χ2 = 2.3 |
| Male (n) | 6 | 9 | p = 0.13 |
| Dominance of injury | |||
| Dominant (n) | 10 | 22 | χ2 = 4.7 |
| Non‐dominant (n) | 13 | 8 | p = 0.04 |
| Mean (95% CI) age of subjects (years) | 53.3 (49.1 to 57.5) | 56.1 (53 to 59.2) | t = 0.1, p = 0.89 |
| Median (IQR) symptom duration (months) | 6.5 (4.8–13) | 9 (4–20) | z = −0.6, p = 0.57 |
| Pre‐hydrodilatation primary outcome measures, mean (95% CI) | |||
| SDI | 10.2 (8.3 to 12.1) | 10.24 (8.7 to 11.7) | t = 0.3, p = 0.80 |
| SD% | 51.5 (43.6 to 59.4) | 50.2 (43 to 57) | t = 1.3, p = 0.21 |
| SPADI | 61.8 (50.1 to 73.5) | 57.4 (44.3 to 63.9) | t = 0.3, p = 0.74 |
| Intra‐hydrodilatation findings | |||
| Mean (95% CI) volume injected (ml) | 38.7 (28.1 to 46.1) | 36.9 (22.6 to 31.2) | t = 1.4, p = 0.17 |
| Joint distension | |||
| Satisfactory to excellent | 17 | 25 | χ2 = 1.2, p = 0.28 |
| None to poor | 6 | 5 | |
| Subscapularis distension | |||
| Satisfactory to excellent | 15 | 21 | χ2 = 0.8, p = 0.58 |
| None to poor | 7 | 9 | |
IQR, interquartile range.
Influence of type of glenohumeral joint contracture on primary and secondary outcomes
In general, there were no significant differences in outcome for subjects with primary and secondary glenohumeral joint contracture, irrespective of the time of measurement. The only exception was at 3 months after hydrodilatation, where subjects with primary glenohumeral joint contracture had higher SD% (mean (SD) 87.9 (9.6)) compared with those with secondary contracture (72.2 (22.4); t = 3.4; p = 0.001). As there was little difference in outcome between the contracture groups, their data were pooled so that trends in outcome could be identified across the 2‐year time period after hydrodilatation.
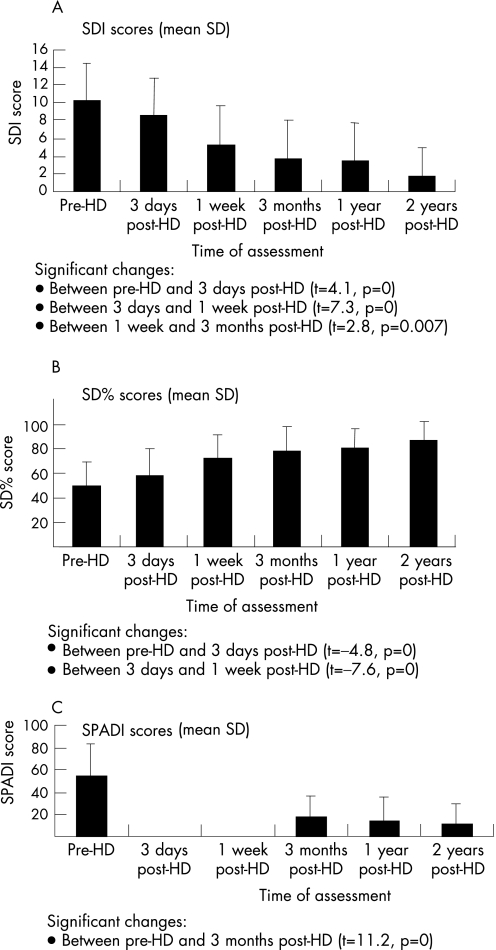
Trends in primary outcome measures
Individuals reported that their upper limb function had increased after hydrodilatation. This is illustrated in fig 1, which shows that scores for the SDI and SPADI decreased and those of the SD% increased over time since hydrodilatation. All primary outcome measures showed a significant change over the 2‐year assessment period (SDI: F = 119.51, p = 0; SPADI: F = 73.14, p = 0; SD%: F = 1205.44, p = 0). The greatest magnitude of significant change in the SDI and SD% occurred between 3 days and 1 week after hydrodilatation (SDI: mean change of 3.3 points; SD%: mean change of 14.8 points). This is in contrast with the SPADI where the greatest change occurred between pre‐hydrodilatation and 3 months post‐hydrodilatation (mean change of 38.1 points). The SPADI was not assessed at 3 days and 1 week after hydrodilatation owing to time constraints. Significant changes also occurred between pre‐hydrodilatation and 3 days post‐hydrodilatation for the SDI and SD%, between 1 week and 3 months afterhydrodilatation for the SDI and between 1 and 2 years after hydrodilatation for the SDI. At 2 years after hydrodilatation, slight deficits in shoulder function were still reported by most subjects, irrespective of the outcome measure used.
Figure 1 Change in primary outcome measures over a 2‐year period after hydrodilatation
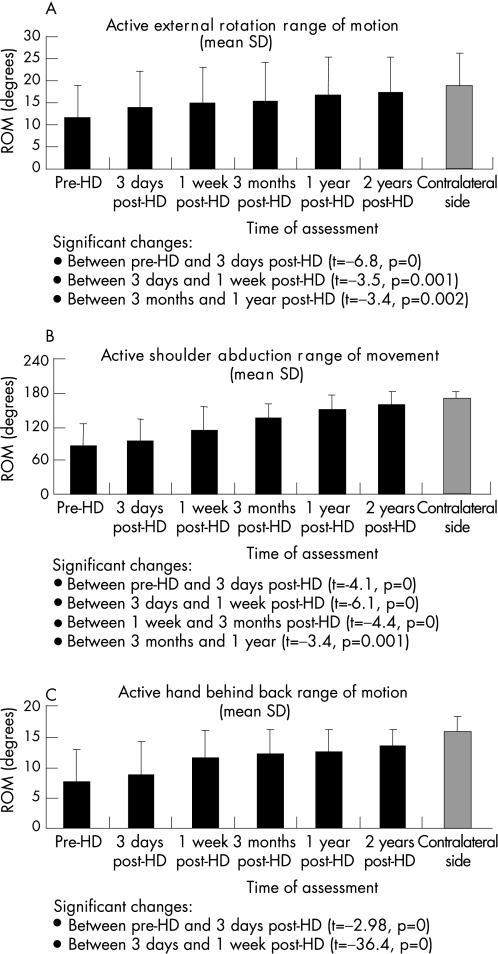
Trends in secondary outcome measures
All individuals were able to perform shoulder external rotation (in 0° of elevation), abduction and hand behind back before hydrodilatation. Before hydrodilatation, hand behind back was the most limited of these movements, being on average 48% of the contralateral side (compared with abduction being 50% and external rotation being 62% of the asymptomatic side). The active range of these movements increased significantly over the 2‐year period after hydrodilatation (fig 2). Improvements in range of movement occurred at different rates depending on the direction of movement. The greatest change in external rotation (mean change of 2.4°) occurred within 3 days after hydrodilatation, whereas the greatest change in hand behind back occurred between 3 days and 1 week after hydrodilatation (mean change of 2.7 spinous process levels). Shoulder abduction was the slowest to improve, with the greatest change in range occurring between 1 week and 3 months after hydrodilatation (mean change of 22.6°). However, slight deficits in range of movement remained 2 years after hydrodilatation. Hand behind back was the most limited, being on average 86% of the contralateral side (external rotation 93% and abduction 95% of the contralateral side). This equates to an average difference of <10°. Given that inclinometer has a ±5°‐measurement error, these deficits are on average negligible. Figure 2 also illustrates that range of movement plateaued between 1 and 2 years after hydrodilatation and there was no deterioration in range over time.
Figure 2 Change in secondary outcome measures over a 2‐year period after hydrodilatation
Prediction of outcome after hydrodilatation
Moderate‐to weak‐strength associations were observed between the primary outcome measures (function) at 3 months, 1 and 2 years after hydrodilatation, and before hydrodilatation range of external rotation, abduction and hand behind back (table 3). In all, <14% of functional capacity at 3 months after hydrodilatation can be accounted for by pre‐hydrodilatation range of motion.
Table 3 Ability of pre‐hydrodilatation to predict functional outcome at 3 months, 1 and 2 years after hydrodilatation (Pearson's correlation coefficient).
| Primary (functional) outcome measure | Time of assessment | Direction of motion | ||
|---|---|---|---|---|
| External rotation | Shoulder abduction | Hand behind back | ||
| SPADI | 3 months | −0.21 (0.127) | −0.37 (0.005) | −0.26 (0.054) |
| 1 year | −0.19 (0.195) | −0.28 (0.053) | −0.27 (0.058) | |
| 2 years | −0.23 (0.313) | −0.21 (0.19) | −0.14 (0.372) | |
| SDI | 3 months | −0.35 (0.008) | −0.35 (0.008) | −0.284 (0.037) |
| 1 year | −0.19 (0.184) | −0.23 (0.115) | 0.18 (0.214) | |
| 2 years | −0.26 (0.092) | −0.21 (0.183) | −0.1 (0.522) | |
| SD% | 3 months | 0.31 (0.018) | 0.36 (0.006) | 0.25 (0.062) |
| 1 year | 0.184 (0.203) | 0.14 (0.321) | 0.11 (0.457) | |
| 2 years | −0.27 (0.084) | 0.25 (0.106) | 0.16 (0.294) | |
SD%, shoulder disability percentage; SDI, Shoulder Disability Index; SPADI, Shoulder Pain and Disability Index.
Italics denotes a significant result.
Discussion
This is the first study that has documented the long‐term effect of hydrodilatation in individuals with primary and secondary glenohumeral joint contracture. By contrast with previous authors, who evaluated outcome at 3 months after hydrodilatation,7,8,12,14 this study assessed outcome up to 2 years after hydrodilatation. Therefore, more robust conclusions regarding the results of hydrodilatation can be drawn from this study. Moreover, the timeframes chosen for assessment reflect the aims of medical and allied health treatment, which is to increase function in the long term.16,17 A limitation of this study is the lack of a control group: that is a group that did not receive hydrodilatation or physiotherapy or both interventions. Therefore, conclusions cannot be made regarding the relative effectiveness of hydrodilatation and physiotherapy compared with other treatments and time.
The results of this study indicate that hydrodilatation and physiotherapy, in patients with primary contracture and secondary glenohumeral joint contracture associated with rotator cuff pathology, increases functional capacity and range of motion in most individuals. Therefore, hydrodilatation and physiotherapy potentially have a positive effect on the stiff, painful shoulder, which concurs with the findings of other authors.7,12,19 There were no significant differences between the primary and secondary contracture groups, with respect to their rate or magnitude of recovery. This was an interesting finding as it showed that hydrodilatation may have a role in treating rotator cuff pathology with coexisting glenohumeral joint range of motion restrictions and, most importantly, that the presence of coexisting pathology did not limit the effectiveness of hydrodilatation.
The greatest magnitude of change in most primary and secondary outcome measures occurred between 3 days and 1 week after hydrodilatation. This occurred with the start of physiotherapy. Individuals showed improvement in all of the outcome measures over the next 3 months as the physiotherapy programme continued and progressed. This highlights that the outcomes observed could be attributed to the effect of hydrodilatation and physiotherapy, and are over and above that of the natural history of the disorder.37,38,39 Primary glenohumeral joint contracture is considered to be a self‐limiting disorder.37,38,39 It is likely that if a non‐treatment control group were included in the study, it would have findings similar to the treatment group at 2 years. The difference observed with the hydrodilatation and physiotherapy was with the more immediate effects. Patients begin to show improvement in pain and function quite early, rather than having the disability for a more prolonged period. This finding concurs with the findings of other authors40,41 who showed that physiotherapy in combination with injection therapy is more effective than either in isolation. Although this study and others in the literature10,19,42,43,44,45 seem to support the need for a well‐structured, non‐aggressive physiotherapy programme as part of the overall treatment for shoulder stiffness, some authors question the effectiveness of physiotherapy.46 Therefore, further studies, with an appropriate control group, are required to determine whether physiotherapy influences outcome after hydrodilatation.
Hydrodilatation and physiotherapy were equally effective in individuals with primary and secondary glenohumeral joint contractures associated with rotator cuff pathology. Thus, the results of this study suggest that patients with concurrent rotator cuff pathology are able to improve their functional capacity and active motion with this relatively low‐invasive treatment. The mechanism by which hydrodilatation reduces dysfunction associated with stiffness due to rotator cuff pathology is unclear. It may be due to the effect of cortisone on the vascular proliferation response associated with glenohumeral joint contracture.15,47
Despite significant improvement in all outcomes assessed, most subjects continued to report slight deficits in shoulder functional capacity and range of motion 2 years after hydrodilatation. Thus, total resolution of shoulder symptoms in individuals with glenohumeral joint contracture may not always be achieved with hydrodilatation and physiotherapy.4,48 However, normative data on functional capacity and active shoulder motion has not been fully established in this age group. For example, Brinker et al33 showed that there is great variation in SPADI scores (as evidenced by wide CIs) in men with normal shoulders who are >40 years of age. This indicates that many “normal” patients may experience loss of functional capacity (or pain) without being diagnosed with a shoulder disorder. In this study, the range of motion deficits 2 years after hydrodilatation were minimal, on average 10° less than the contralateral side. This falls within the reported normative range for variation in range of motion between the dominant and non‐dominant shoulders in the normal population in this age group.49 On the basis of these results, further research is required to more accurately establish realistic clinical end points of treatment, by studying the characteristics of populations with normal shoulder.
In this study, glenohumeral range of motion was established by frequently used, valid and reliable measure processes.35 This is in contrast with previous studies, where the method of measurement was not standardised, valid or reliable.2,7,19,20,21,50 The findings of this study indicate that there was no significant difference in range of motion between the primary and secondary glenohumeral joint stiffness groups. This suggests that rotator cuff pathology may be associated with the restriction of glenohumeral joint range of motion. Further investigation into shoulder stiffness attributed to other aetiologies, such as factures, would assist in determining whether aetiology affects the management of glenohumeral joint contracture.
What is already known on this topic
Hydrodilatation has been proposed as a therapeutic procedure for glenohumeral joint contracture.
Most recent studies have cited variable results.
This is potentially due to the variability in hydrodilatation techniques, after hydrodilatation treatment regimens, sample sizes, lack of explicit inclusion criteria and variable outcome measurements.
Despite these limitations, most authors conclude that hydrodilatation has a role in the treatment of glenohumeral joint contracture.
What this study adds
This trial documents the long‐ term effect of hydrodilatation and indicates that hydrodilatation and physiotherapy increases functional capacity and range of motion in most individuals, with both primary glenohumeral joint contracture and secondary contracture associated with rotator cuff pathology.
It also indicates that the pre‐hydrodilatation range of motion did not prove to be a predictor of outcome.
A secondary aim of this study was to investigate whether pre‐hydrodilatation range of motion (external rotation, abduction and hand behind the back) predicted outcome after hydrodilatation, as these measures are often used in clinical practice to determine prognosis. Generally, weak, non‐significant associations were found. This suggests that pre‐hydrodilatation range of motion is not an accurate predictor of functional capacity after hydrodilatation. Further investigation is warranted to determine predictors of long‐term outcome for hydrodilatation. Thus, at present, clinicians should refrain from using range of motion as a predictor of prognosis.
The results of this study show that hydrodilatation and physiotherapy have a significant effect in increasing functional capacity and shoulder range of motion in individuals with primary and secondary glenohumeral joint contracture associated with rotator cuff pathology. Hydrodilatation and physiotherapy appear to have an effect on the natural history of the disorder by increasing functional capacity. Benefits associated with hydrodilatation and physiotherapy continue to improve, in the long term (up to 2 years after hydrodilatation) for most individuals. Therefore, hydrodilatation and physiotherapy seem to be effective and relatively low‐risk interventions for the stiff and painful shoulder.
Supplementary Material
Abbreviations
SD% - shoulder disability percentage
SDI - Shoulder Disability Index
SPADI - Shoulder Pain And Disability Index
Footnotes
Competing interests: None declared.
References
- 1.Anton H A. Frozen shoulder. Can Fam Physician 1993391773–1777. [PMC free article] [PubMed] [Google Scholar]
- 2.Lundberg B J. The frozen shoulder. Acta Orthop Scand 19691191–59. [PubMed] [Google Scholar]
- 3.Zuckerman J D, Cuomo F, Rokito S. Definition and classification of frozen shoulder: a consensus approach. J Shoulder Elbow Surg 19943S5. [DOI] [PubMed] [Google Scholar]
- 4.Noel E, Thomas T, Schaeverbeke T.et al Frozen shoulder. Joint Bone Spine 200067393–400. [PubMed] [Google Scholar]
- 5.Loew M, Heichel T O, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg 20051416–21. [DOI] [PubMed] [Google Scholar]
- 6.Ide J, Takagi K. Early and long‐term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg 200413174–179. [DOI] [PubMed] [Google Scholar]
- 7.Bell S, Coghlan J, Richardson M. Hydrodilatation in the management of shoulder capsulitis. Aust Radiol 200347247–251. [DOI] [PubMed] [Google Scholar]
- 8.Halverson L. Shoulder joint capsule distension (hydroplasty): a case series of patients with “frozen shoulders” treated in a primary care office. J Family Pract 20025161–63. [PubMed] [Google Scholar]
- 9.Klinger H M, Otte S, Baums M H.et al Early arthroscopic release in refractory shoulder stiffness. Arch Orthop Trauma Surg 2002122200–203. [DOI] [PubMed] [Google Scholar]
- 10.Green S, Buchbinder R, Glazier R.et al Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessment and efficacy. BMJ 1998316354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall S. Dealing with frozen shoulder. Med Today 200089–90.
- 12.Buchbinder R, Green S, Lawler G.et al Efficacy of hydrodilatation for frozen shoulder (FS): results of a randomised double‐blind placebo‐controlled trial (abstract). Aust NZ J Med 200030527 [Google Scholar]
- 13.Callinan N, McPherson S, Cleaveland S.et al Effectiveness of hydroplasty and therapeutic exercise for treatment of frozen shoulder. J Hand Therapy 200316219–224. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs L G H, Barton M A J, Wallace W A.et al Intra‐articular distension and steroids in the management of capsulitis of the shoulder. BMJ 19913021498–1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rizk T, Gavant M D, Pinals R S. Treatment of adhesive capsulitis with arthrogrophic capsular distension and rupture. Arch Phys Med Rehab 199475803–807. [PubMed] [Google Scholar]
- 16.Andren L, Lundberg B. Treatment of rigid shoulders by joint distension during arthrography. Acta Orthop Scand 19653645–53. [DOI] [PubMed] [Google Scholar]
- 17.Fareed D, Gallivan W. Office management of frozen shoulder syndrome: treatment with hydraulic distension under local anaesthesia. Clin Orthop Relat Res 1989242177–183. [PubMed] [Google Scholar]
- 18.Mulcahy K A, Baxter A D, Oni O O A.et al The value of shoulder distension arthrograpy with intraarticular injection of steroid and local anaesthetic: a follow‐up study. Br J Radiol 199467263–266. [DOI] [PubMed] [Google Scholar]
- 19.Vad V B, Sakalkale D, Warren R F. The role of capsular distention in adhesive capsulitis. Arch Phys Med Rehabil 2003841290–1292. [DOI] [PubMed] [Google Scholar]
- 20.Gerber C, Espinosa N, Perren T G. Arthroscopic treatment of shoulder stiffness. Clin Orthop Relat Res 2001390119–128. [DOI] [PubMed] [Google Scholar]
- 21.Hollaway B G, Schenk T, Williams G R.et al Arthroscopic capsular release for the treatment of refractory postoperative or post‐fracture shoulder stiffness. J Bone Joint Surg 200183‐A1682–1687. [DOI] [PubMed] [Google Scholar]
- 22.Jobe F W, Jobe C M. Painful athletic injuries of the shoulder. Clin Orthop 1983173117–124. [PubMed] [Google Scholar]
- 23.Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg 199678A1015–1023. [DOI] [PubMed] [Google Scholar]
- 24.Hertel R, Ballmer F T, Lombert S M.et al Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 19965307–313. [DOI] [PubMed] [Google Scholar]
- 25.Crenshaw A H, Kilgore W E. Surgical treatment of bicipital tenosynovitis. J Bone Joint Surg 196648A1496–1502. [PubMed] [Google Scholar]
- 26.Neer CS I I. Impingement lesions. Clin Orthop 198317370–77. [PubMed] [Google Scholar]
- 27.Neer CS I I. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. A preliminary report. J Bone Joint Surg 197254A41–50. [PubMed] [Google Scholar]
- 28.Hawkins R J, Kennedy J C. Impingement syndrome in athletes. Am J Sports Med 19808151–158. [DOI] [PubMed] [Google Scholar]
- 29.Beaton D, Richards R R. Assessing the reliability and responsiveness of 5 shoulder questionnaires. J Shoulder Elbow Surg 19987565–572. [DOI] [PubMed] [Google Scholar]
- 30.Romeo A A, Bach B R, O'Halloran K L. Scoring systems for shoulder conditions. Am J Sports Med 199624472–476. [DOI] [PubMed] [Google Scholar]
- 31.Roach K E, Elly B M, Songsiridej N.et al Development of a Shoulder Pain and Disability Index. Arth Care Res 19914143–149. [PubMed] [Google Scholar]
- 32.Croft P, Pope D, Zonca M.et al Measurement of shoulder related disability: results of a validation study. Ann Rheum Dis 199453525–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brinker M R, Cuomo J S, Popham G J.et al An examination of bias in shoulder scoring instruments among healthy collegiate and recreational athletes. J Shoulder Elbow Surg 200211463–469. [DOI] [PubMed] [Google Scholar]
- 34.Kendall N. Developing outcome assessments: a step by step approach. NZ J Physiotherapy 19972511–17. [Google Scholar]
- 35.Green S. A standardized protocol for measurement of range of movement of the shoulder using the plurimeter V inclinometer and assessment of its intrarater and interrater reliability. Arthritis Care Res 19981143–52. [DOI] [PubMed] [Google Scholar]
- 36.Munro B H. ed. Correlation. Statistical methods for health care research 4th edn. Philadelphia: Lippincott‐Williams and Wilkins, 2001223–243.
- 37.CAodman E . ed. Tendinitis of the short rotators. Ruptures of the supraspinatus tendon and other lesions in or about the subacromial bursa. Boston: Thomas Todd, 1934216–224.
- 38.Grey R G. The natural history of “idiopathic” frozen shoulder. J Bone Joint Surg Am 197860564. [PubMed] [Google Scholar]
- 39.Simmonds F A. Shoulder pain. With particular reference to the “frozen shoulder. ” J Bone Joint Surg Br 194931426–432. [PubMed] [Google Scholar]
- 40.Bulgen D Y, Binder A l, Hazelman B L.et al “Frozen shoulder: prospective clinical study with and evaluation of three treatment regimes”. Ann Rheumatol Dis 198443353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buchbinder R, Green S, Youd J M. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 20031CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carette S, Moffet H, Tardif J.et al Intrarticular corticosteroids, supervised physiotherapy or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo‐controlled trial. Arthritis Rheum 200348829–838. [DOI] [PubMed] [Google Scholar]
- 43.Ryans I, Montgomery A, Galway R.et al A randomized controlled trial of intra‐articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology 1 200544529–535. [DOI] [PubMed] [Google Scholar]
- 44.Melzer C, Wallny T, Wirth C J.et al Frozen shoulder‐treatment and results. Arch Orthop Trauma Surg 199511487–91. [DOI] [PubMed] [Google Scholar]
- 45.Mao C, Jaw W C, Cheng H C. Frozen shoulder: correlation between the response to physical therapy and follow up shoulder arthrography. Arch Phys Med Rehab 199778857–859. [DOI] [PubMed] [Google Scholar]
- 46.Diercks R L, Stevens M. Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy‐seven patients with frozen shoulder syndrome. J Shoulder Elbow Surg 200413499–502. [DOI] [PubMed] [Google Scholar]
- 47.Hannafin J A, Strickland S M. Frozen shoulder. Curr Opin Orthop 200011271–275. [Google Scholar]
- 48.Shafter B, Tibone J E, Kerlan R K. Frozen shoulder: a long term follow up. J Bone Joint Surg 199274A738–746. [PubMed] [Google Scholar]
- 49.Barnes C J, Van Steyn S J, Fischer R A. The effects of age, sex and shoulder dominance on range of motion of the shoulder. J Shoulder Elbow Surg 200110242–246. [DOI] [PubMed] [Google Scholar]
- 50.Nobuhara K, Supapo A R, Hino T. Effects of joint distension in shoulder diseases. Clin Orthop Relat Res 199430425–29. [PubMed] [Google Scholar]
- 51.Maitland G D.Peripheral manipulation, 3rd edn. Oxford: Butterworth Heinemann 1991
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.