Abstract
A 30‐year‐old male athlete with exercise‐related syncopal symptoms spontaneously exhibited a type 1 Brugada ECG and was inducible during electrophysiology study. He was diagnosed with symptomatic Brugada syndrome and deemed at high risk of sudden cardiac death. Thus, he received a cardioverter/defibrillator and was advised to abstain from further competitive sports activities. This case points to a role of the ECG in pre‐participation screening. It also demonstrates that, in athletes with Brugada syndrome, repolarisation anomalies may be markedly attenuated during vigorous exercise and considerably increased immediately after exercise. The observed J‐wave amplitude dynamics suggests enhancement of pre‐existing autonomic dysfunction through heavy exertion.
Case report
A 30‐year‐old male endurance cyclist was diagnosed with right bundle branch block and transferred to our institution for further investigation. Detailed history disclosed that, since he had started on heavy training in the year before admission, he experienced around ten short episodes of light‐headedness and one episode of syncope. These symptoms always occurred in a seated position in the initial minutes after aerobic endurance training and were associated with disagreeable palpitations. Training sessions (five per week) included cycling and distance running. On examination, the young man was completely asymptomatic, had no thoracic anomalies and a negative family history of premature deaths. Blood analyses were not indicative of an inflammation reaction or any other abnormality.
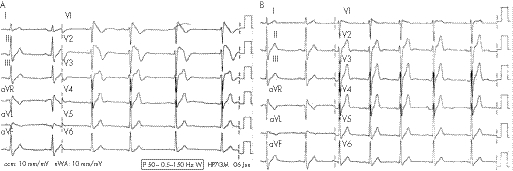
On admission, the standard ECG at rest showed sinus rhythm (75 bpm), and durations of P wave, PR, QRS, QT and QTc intervals (lead II) of 90, 185, 150, 350 and 388 ms, respectively. Precordial leads showed a type 1 Brugada ECG pattern (fig 1A) with increased J‐wave amplitudes (JWA): 3.5 mm (V1), 5.5 mm (V2) and 4 mm (V3). By contrast, an earlier ECG obtained at a non‐exercise period showed only a slight saddleback‐type ST‐segment elevation (1.6 mm) in V1 (fig 1B).
Figure 1 (A) Type 1 Brugada ECG spontaneously manifesting on admission. Note the markedly increased J‐wave amplitudes in V1–V3 and the coved type ST‐segment elevations in V1 and V2. (B) ECG obtained in a non‐exercise period before admission. Note the absence of the typical ECG signature. Only a slight saddleback‐type ST‐segment elevation (1.6 mm) is present in V1.
Echocardiography disclosed normal intracardiac dimensions, and neither ventricle showed structural or functional abnormalities. During an active orthostasis test, no symptoms were induced.
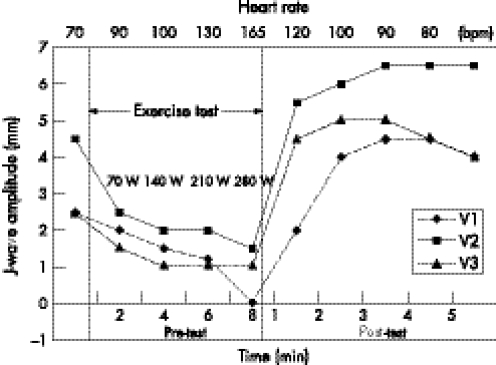
During graded exercise testing, the athlete completed a work load of 280 W without any symptoms. The JWA in leads V1–V3 progressively decreased with increasing work load and showed a minimum value of 0 mm (V1), 1.5 mm (V2) and 1 mm (V3) at the highest work load. During recovery, JWA increased significantly, exceeding pre‐test levels by 80% (V1), 44% (V2) and 100% (V3) 3 min after the test (fig 2). Blood pressure exhibited normal behaviour and recovered to baseline values within 1 min after exercise. Heart rate is indicated in fig 2.
Figure 2 Time course of J‐wave amplitudes in the right precordial leads, before, during and after exercise testing. Note that the time scale (lower abscissa) referring to the exercise period is indicated in 2 min steps, whereas for the pre‐ and post‐test (post) period it is given in 1 min steps. The numbers on top (upper abscissa) represent mean heart rate; the inserted figures represent the work load in watts.
Owing to the spontaneous manifestation of a Brugada type 1 ECG, the athlete was diagnosed with Brugada syndrome, and because of the syncopal episodes was deemed to be at high risk of sudden cardiac death.1,2,3 Electrophysiological testing showed normal sinus node function, normal atrioventricular physiology, normal H‐V interval and no accessory pathways. Ventricular stimulation was performed using three drive cycle lengths (600, 500 and 400 ms) and two premature beats that were started in late diastole and whose coupling intervals were reduced in decrements of 10 ms until refractoriness was reached. Sustained polymorphic ventricular tachycardia with a cycle length of 220 ms was induced at the right ventricular apex. Mode of induction was 400 ms/210 ms/190 ms. An implantable cardioverter/defibrillator was inserted, and the patient agreed to abstain from further competitive activities. During follow‐up (9 months), he remained asymptomatic and implantable cardioverter/defibrillator interrogation did not show repetitive ectopic activity.
Discussion
The Brugada syndrome was first described in 1992 by the Brugada brothers.1 Recently, strict diagnostic criteria and risk stratification for the identification of high‐risk patients with Brugada syndrome patients have been suggested.3 Thus, the diagnosis of Brugada syndrome can only be made on the basis of a typical ECG pattern and only a coved type ECG (Brugada type 1) is diagnostic of the disease and, if spontaneously occurring, apparently has a poorer prognosis.3
Although for European countries only scanty data exist as to the prevalence of the disease in the general population,4,5 the situation is even worse among endurance‐trained athletes. In the sole systematic study,6 155 male athletes were screened for ECG abnormalities of the Brugada type, and 139 were diagnosed with an early repolarisation phenomenon. Of the latter, 8.6% exhibited an ECG pattern that the authors deemed suspicious. However, the representative ECG shown in their paper6 does not fulfil the strict Brugada criteria.3
Recurrent exercise‐related syncope in endurance‐trained athletes is believed not to be associated with an adverse outcome, if structural abnormalities of the heart are absent.7 This, however, does not hold for syncope in individuals with Brugada syndrome, which is a potentially life threatening primary electrical disease.1,2,3 Individuals with a Brugada ECG and a history of syncope have a high risk for sudden cardiac arrest which amounts to 27% if they are inducible.2 In rare cases, syncope in Brugada syndrome may be due to a vasovagal mechanism.8 This, however, seems unlikely in our patient as his symptoms were unrelated to postural challenge.
Key points
Brugada syndrome is a genetically defined electrical disorder characterised by a typical ECG pattern (Brugada type 1 ECG: coved ST‐segment elevation ⩾2 mm and a negative T wave in more than one right precordial lead) and syncopal episodes or survived cardiac arrest. Symptomatic patients with Brugada syndrome bear a high risk of sudden arrhythmic death, and require implantation of a cardioverter/defibrillator.
This case demonstrates that symptoms may occur in athletes with Brugada syndrome after vigorous exercise.
It also shows that the diagnostically important repolarisation anomalies are highly variable and pronounced changes of precordial J wave amplitudes can be induced by exercise. The latter suggests that autonomic imbalance may be enhanced immediately after heavy exertion.
Although this case points to a role of the ECG in pre‐participation screening,9 it also shows the potential diagnostic fallacies (fig 1) linked to the variable nature of repolarisation in Brugada syndrome.3 The fact that we observed markedly attenuated ST‐segment elevations during vigorous exercise and markedly increased JWA immediately after exercise suggests enhancement of pre‐existing autonomic dysfunction10 through heavy exertion. Thus, in athletes with Brugada syndrome, repolarisation anomalies may be enhanced, if not unmasked, by exercise stress testing.
Acknowledgements
We thank Hans‐Christian Esperer and Julia C Graney for their excellent technical assistance.
Footnotes
Competing interests: None.
References
- 1.Brugada P. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol 1992201391–1396. [DOI] [PubMed] [Google Scholar]
- 2.Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation 20031083092–3096. [DOI] [PubMed] [Google Scholar]
- 3.Antzelevitch C, Brugada P, Borggrefe M.et al Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005111659–670. [DOI] [PubMed] [Google Scholar]
- 4.Litmann L, Monroe M H, Kerns W P.et al Brugada syndrome and “Brugada sign”: clinical spectrum with a guide for the clinician. Am Heart J 2003145768–778. [DOI] [PubMed] [Google Scholar]
- 5.Hermida J S, Lemoine J L, Aoun F B.et al Prevalence of the Brugada syndrome in apparently healthy population. Am J Cardiol 20008691–94. [DOI] [PubMed] [Google Scholar]
- 6.Bianco M, Bias S, Gianfelici A.et al Does early repolarization in the athlete have analogies with the Brugada syndrome? Eur Heart J 200122504–510. [DOI] [PubMed] [Google Scholar]
- 7.Colvicchi F, Ammirati F, Biffi A.et al Exercise‐related syncope in young competitive athletes without evidence of structural heart disease: clinical presentation and long‐term outcome. Eur Heart J 2002231125–1130. [DOI] [PubMed] [Google Scholar]
- 8.Patruno N, Pontillo D. Brugada syndrome and vasovagal syncope (letter to the editor). Pacing and Clin Electrophysiol 200629215–310. [DOI] [PubMed] [Google Scholar]
- 9.Corado D, Pelliccia A, Bjornstad H H.et al Cardiovascular pre‐participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus statement of the study group of sport cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial disease of the European Society of Cardiology. Eur Heart J 200526516–524. [DOI] [PubMed] [Google Scholar]
- 10.Wichter T, Matheja P, Eckardt L.et al Cardiac autonomic dysfunction in Brugada syndrome. Circulation 2002105702–706. [DOI] [PubMed] [Google Scholar]