Abstract
Objectives
This report describes the thermal stresses and strains during competitive singles tennis.
Methods
Thermoregulatory responses were investigated during best of three set tennis matches among 25 players. A total of 86 observations were made from 43 matches played, covering each season, with ambient temperatures ranging from 14.5 to 38.4°C. Core body temperature and skin temperature were recorded each minute throughout the match, whilst heart rate was logged every 15 s. Body mass and fluid intake were measured before the match, after 30 min of play and at the completion of the match to determine sweat rate. Subjective ratings of thermal strain included thermal comfort, sweatiness and perceived exertion. The thermal environment was assessed by dry bulb, wet bulb and natural wet bulb temperatures, globe temperature and wind speed.
Results
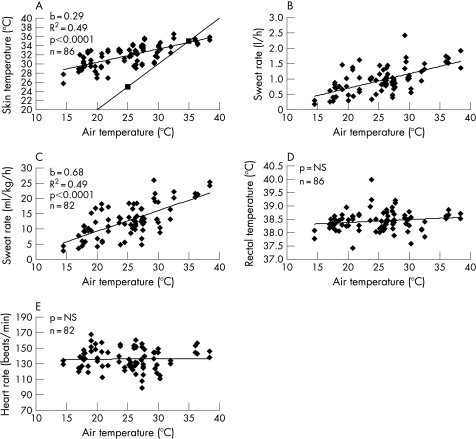
Mean (SD) core temperature after 30 min of play was 38.4°C (0.4°C), and demonstrated no association with air temperature or wet bulb globe temperature. Mean skin temperature was 31.8°C (2.3°C) ranging from 25.7 to 36.5°C, and showed a positive association with air temperature (p<0.001). Heart rate varied widely during play, resulting in a mean (SD) response of 136.1 (13.7) beats/min and no association with air temperature. Sweat rate averaged 1.0 (0.4) litres/h (0.2–2.4 litres/h) or 12.8 (5.5) ml/kg/h (2.7–26.0 ml/kg/h), and demonstrated a positive relationship with air temperature (p<0.001). All subjective responses showed positive correlations with air temperature (p<0.001).
Conclusions
Stressful environmental conditions produce a high skin temperature and rating of thermal discomfort. However, overall thermoregulatory strain during tennis is moderate, with core temperature remaining within safe levels.
Tennis is played by people of all ages and standards around the world in a wide range of climates. Despite this, the thermoregulatory stresses and strains experienced by tennis players are poorly understood.
All tennis players, whether professional or amateur, would benefit from a greater understanding of the environmental stresses and thermoregulatory strains associated with playing tennis. Individuals and organisations with a duty of care towards players also require objective information on which to base recommendations and policies for managing heat stress in training and competition.
Thermal stress is the combination of six factors that combine to burden the thermoregulatory system in the effort to maintain core body temperature within tolerable limits.1 The six factors comprising heat stress are: (1) metabolic heat production, (2) air temperature, (3) absolute humidity, (4) radiant temperature, (5) air movement, and (6) clothing.1 Thermal strain refers to the thermoregulatory and subjective responses to a thermal stress. Thermoregulatory strains include core body temperature, skin temperature, sweat rate, and heart rate, whilst subjective strains include thermal sensation and perceived exertion.1 Empirical observations of thermal stress and the corresponding thermoregulatory strains during tennis play are required to determine whether players are at risk of heat illness, and similarly to determine whether they are able to maintain thermal comfort.
No previously published studies have made a thorough assessment of the thermal environment and players' corresponding thermoregulatory responses during tennis. Heart rate, oxygen consumption, core body temperature, skin temperature, and sweat rate have been measured during tennis in a number of studies.2,3,4,5,6,7,8,9,10 However, in general these studies have not described the demands of tennis in competition in a wide range of environmental conditions and have not represented the wider tennis community. Only one known study included both genders,6 and one other study was the only one to make observations during a best of three sets singles match12 rather than a time‐restricted match. All of these studies used a relatively small sample of subjects and often only one match was played per subject. A number of the observations in these studies caused disruption to normal player behaviour and performance, and/or the rules of tennis. For example, observations were often measured at various intervals during play, which might not be representative of the activity periods of a real match. The heart rate response in tennis demonstrates a wide variation, therefore continuous recording throughout the match at frequent intervals would be more accurate. It was also be advantageous to continuously record core body temperature throughout the match in order to determine: (1) whether thermal equilibrium is achieved and core temperature is controlled or rises continuously, and (2) the change in core temperature. A single measurement at the end of the match would not provide such information. Furthermore, air temperature and relative humidity were the only environmental stresses measured, not providing a complete assessment of the thermal stress.
This paper reports the thermoregulatory and subjective responses to singles tennis in a wide range of thermal environments. This information is required as the basis for developing predictive models for assessing heat stress in tennis.
Methods
Subjects
A total of 25 regular tennis players (19 male and 6 female) participated in this study. Players ranged from recreational players (n = 13) to semi‐professional players and professional coaches (n = 12). The mean (SD) age, height, body mass, maximum aerobic power (VO2max), maximum heart rate (HRmax), sum of 9 skinfold thickness and predicted body fat for the subjects were as follows. Males: age = 23.9 (5.1) years; height = 180 (9) cm; body mass = 76.7 (10.1) kg; VO2max = 55.3 (8.1) ml/kg/min; HRmax = 197.3 (8.8) beats/min; sum 9 skinfolds = 90.4 (34.8) mm; predicted body fat = 10.2 (5.1)%. Females: age = 21.8 (2.3) years; height = 165(3) cm; body mass = 60.1 (5.6) kg; VO2max = 56.0 (3.4) ml/kg/min; HRmax = 192.8 (4.1) beats/min; sum 9 skinfolds = 92.6 (29.5) mm; 16.0 (4.9)%. Each player gave his or her written informed consent, and the project was approved by the University of Sydney Human Research Ethics Committee.
Procedures
A total of 86 observations were made from 43 best of three tie‐break set singles matches were played on a hard court surface tennis court between subjects of a similar standard. All matches adhered to the rules set by the International Tennis Federation.13 Three new tennis balls were used for each match, with players retrieving balls between points. Conventional tennis attire was worn for all matches.
Thermal environment
The thermal environment on the tennis court was recorded throughout the match. Dry bulb temperature and wet bulb temperature were measured on court every 20 min using a whirling psychrometer shielded from sunlight. Natural wet bulb temperature for the wet bulb globe temperature index (WBGT) was measured using an unshielded wet bulb thermometer. Globe temperature for the assessment of radiant temperature was measured using a calibrated thermistor at the centre of a 15 cm blackened copper bulb. A short arm anemometer set 1.5 m from the ground was used to measure wind speed. Globe temperature and wind speed were recorded continuously using a customised Davis Perception II weather station and WeatherLink (Davis Instruments Corp., Hayward, California, USA). These instruments were placed on the court to equilibrate 1 h before the match.
Physiological responses
Before the match, the playing clothes and filled drink bottles of each subject were weighed on electronic balance scales (K‐Tron Model DS‐1, Scottsdale, Arizona, USA) accurate to 1 g. Subjects then dressed in their playing clothes and inserted a calibrated YSI rectal thermistor 10 cm beyond the anal sphincter. Four YSI thermistors were attached to the skin using Opsite adhesive tape at the chest, arm, thigh and leg for estimation of weighted mean skin temperature.14 These temperatures were recorded every minute using a 180 g multi‐channel data logger worn on a belt around the waist. A Polar (S610i) heart rate monitor was worn by each subject, which recorded heart rate every 15 s during play. Subjects were weighed dressed in their playing clothes, temperature logger and heart rate monitor using electronic balance scales (K‐Tron Model DP‐3W) accurate to 10 g. The drink bottles and subjects were re‐weighed fully dressed and equipped after 30 min of play as a steady sweating rate is established after approximately 30 min. The final weighing of each fully dressed and equipped subject occurred at the completion of the match. The drink bottles were also re‐weighed at this point. Players consumed fluids during the change of ends on an ad libitium basis throughout the match. Each subject reported subjective responses during the change of ends after game 5, then after every six games (ie, after game 5, 11, 17 etc). The time taken to complete these subjective responses did not exceed the legal 90 s for the change of ends. Subjective responses were:
-
Rating of thermal comfort:15 responses were to the printed question “How warm do you feel?”
-
-
7 Much too warm
-
-
6 Just too warm
-
-
5 Comfortably warm
-
-
4 Neither warm nor cool
-
-
3 Comfortably cool
-
-
2 Just too cool
-
-
1 Much too cool
-
-
-
Rating of sweatiness: responses were to the printed question “How sweaty do you feel?”
-
-
4 Dripping wet
-
-
3 Wet
-
-
2 Moist
-
-
1 Sticky
-
-
0 Dry
-
-
-
Rating of perceived exertion:16 responses were to the printed question “How strenuous does this work feel?”
-
-
20
-
-
19 Very, very hard
-
-
18
-
-
17 Very hard
-
-
16
-
-
15 Hard
-
-
14
-
-
13 Somewhat hard
-
-
12
-
-
11 Fairly light
-
-
10
-
-
9 Very light
-
-
8
-
-
7 Very, very light
-
-
6
-
-
Statistical analyses were performed using SPSS V.15.0. Multivariate and univariate analysis of variance, and analysis of covariance were performed using the General Linear Model to identify the effect of air temperature, gender and standard. Simple bivariate regressions were performed for the thermoregulatory responses against air temperature. Data is expressed as mean (SD). The significance level was set at p<0.05.
Results
In the present investigation only air temperature was used to represent environmental stress. Air temperature is a major thermal stress because it is the primary determinant of skin temperature and of the thermal gradient for convective heat transfer between the environment and the skin, and affects thermal comfort. Therefore, only air temperature will be used for analysis in the present investigation.
Table 1 presents the air temperatures and WBGT, and thermoregulatory and subjective strains measured during competitive singles tennis in this investigation.
Table 1 Air temperature, wet bulb globe temperatures (WBGT) and thermoregulatory strains during competitive singles tennis.
| Variable | Male | Female | Air temperature | Gender | Standard | ||
|---|---|---|---|---|---|---|---|
| Elite (n = 33) | Recreational (n = 34) | Elite (n = 7) | Recreational (n = 12) | ||||
| Air temperature (°C) | 25 (3.8) | 24.9 (6.4) | 26.9 (6.4) | 23.3 (7.1) | NS | NS | |
| WBGT (°C) | 23.0 (3.0) | 22.1 (4.7) | 24.4 (4.9) | 20.9 (6.2) | NS | NS | |
| Core temperature (°C) | 38.5 (0.4) | 38.4 (0.4) | 38.4 (0.3) | 38.2 (0.3) | NS | NS | NS |
| Skin temperaturei (°C) | 31.7 (2.0) | 32.1 (2.1) | 32.0 (2.8) | 31.1 (3.6) | *** | *** | NS |
| Sweat rate (litres/h) | 1.2 (0.2) | 0.8 (0.3) | 1.0 (0.2) | 0.6 (0.4) | *** | NS | NS |
| Sweat rate (ml/kg/h) | 14.5 (5.2) | 11.1 (4.3) | 17.3 (4.4) | 9.2 (6.4) | *** | NS | NS |
| Heart rate (beats/min) | 140.3 (13.1) | 131.3 (13.2) | 149.6 (6.5) | 126.8 (8.9) | NS | NS | * |
| Thermal comfort | 5.1 (1.0) | 5.1 (0.9) | 4.8 (1.00 | 5.1 (1.0) | *** | NS | NS |
| Sweatiness | 2.0 (1.0) | 1.8 (1.1) | 2.3 (1.1) | 1.5 (0.7) | *** | NS | NS |
| Perceived exertion | 12.9 (1.8) | 12.8 (2.3) | 13.2 (1.0) | 12.3 (2.0) | ** | NS | NS |
Data are presented as mean (SD). n = number of observations.
iInteraction between gender and air temperature for skin temperature. NS, not significant; *<0.05; **<0.01; ***<0.001. Thermal comfort: 1 = “much too cool”, 7 = “much too warm”; sweatiness: 0 = “dry”, 4 = “dripping wet”; perceived exertion: 6 = “very very light”, 20 = “very very hard”.
Figure 1 presents the associations between thermoregulatory strains and environmental stresses (air temperature and wet bulb globe temperature) during competitive singles tennis.
Figure 1 (A) Skin temperature vs air temperature; (B) Sweat rate (litres/h) vs air temperature; (C) Sweat rate (ml/kg/h) vs air temperature; (D) Rectal temperature vs air temperature; (E) Heart rate vs air temperature. NS, not significant.
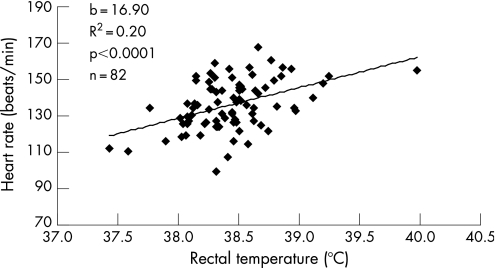
Figure 2 presents the association between the two measures of exercise intensity during tennis. Rectal temperature and heart rate are two indicators of exercise intensity, hence are positively correlated (R2 = 0.20; p<0.001). The overall average heart rate of 136.1 (13.7) beats/min (table 1) equates to approximately 67% of maximum heart rate. This is similar to the 61% of maximum oxygen consumption predicted from the mean rectal temperature of 38.4°C according to the regression equation relating rectal temperature to % VO2max given by Davies et al.17
Figure 2 Heart rate vs rectal temperature.
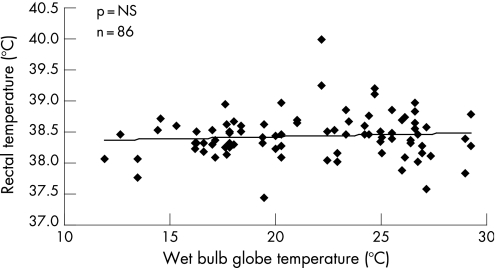
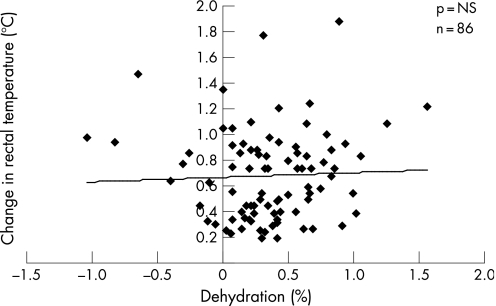
Figure 3 illustrates the lack of association between rectal temperature and the WBGT index. Figure 4 indicates the association between rectal temperature and % dehydration, and fig 5 presents the associations between subjective responses and air temperature.
Figure 3 Rectal temperature vs wet bulb globe temperature (WBGT).
Figure 4 Rectal temperature vs % dehydration.
Figure 5 (A) Rating of thermal comfort vs air temperature; (B) Rating of sweatiness vs air temperature; (C) Rating of perceived exertion vs air temperature. NS, not significant
Discussion
There is community concern in Australia about the risks of heat illness in sport with widespread anecdotal evidence of dizziness, nausea, vomiting and exhaustion during tennis in hot and humid weather. Death and severe injury from sport‐related heat stroke is rare, yet cases have been reported from time to time.18,19 Heat stress during tennis is of particular interest as competitions are often held in the middle of summer with air temperatures exceeding 40°C. Furthermore, the physiological and subjective strains experienced by tennis players are poorly understood, which makes the prevention and management of heat stress difficult. Therefore, players, coaches, parents and organisations or officials would all benefit from objective information relating to thermal stresses and strains in tennis.
What is already known on this topic
Thermal stress and strain has been widely investigated in occupation and the military but less so in sport.
Previous studies have measured various components of thermal stress and strain including air temperature, relative humidity, heart rate, oxygen consumption, core body temperature, skin temperature, and sweat rate.
What this study adds
This paper reports the thermoregulatory and subjective responses to singles tennis in a wide range of thermal environments.
Thermoregulatory and subjective response information is required as the basis for developing predictive models for assessing heat stress in tennis.
Thermoregulatory responses
At rest, core body temperature is within tight physiological limits of between 36.5°C and 37.5°C.20 However, during exercise it has been shown that core temperatures up to a maximum of 41.9°C can be safely tolerated.21 The mean rectal temperature of 38.4°C observed in the present investigation (table 1), agrees with previously published studies in tennis.4,5,11 In the present investigation, four men recorded a mean rectal temperature greater than 39.0°C whilst one woman averaged 38.9°C during play, which whilst higher than rest is not unsafe during exercise. Body core temperature should remain controlled independently of the environment for a given workload—within the prescriptive zone.22 This is illustrated through the lack of association between rectal temperature and air temperature (fig 1D) or rectal temperature and WBGT (fig 3). At the Australian Open, play is suspended when air temperature reaches 35°C and WBGT reaches 28°C.23 Observations in this study were obtained in conditions exceeding this threshold yet body core temperature remained controlled (table 1, and figs 1D and 3). The WBGT threshold of 28°C used at the Australian Open is based on recommendations by the American College of Sports Medicine for distance running.24 This study shows no evidence of excessive increase in core temperature at a WBGT of 28°C, therefore it appears that this threshold is not appropriate for tennis. This is due to the lower metabolic heat production in tennis (approximately 850 W for 64% VO2max) compared with approximately 1200 W for running intensities around 80% VO2max.25,26,27 Core temperature in this study was controlled over a wide range of air temperatures because sweat rate increased to compensate for the loss of convective cooling with increasing air temperature (figs 1B,C). Evaporative cooling is the sole method of heat dissipation when air temperature exceeds skin temperature and heat is gained via convection.28,29 This is illustrated in fig 1A by comparing the trend line for the observations from this investigation with the line of unity. The interaction between the two lines at approximately 35°C indicates the point where skin and air temperatures are equal, demonstrating convective heat loss in temperatures less than 35°C and convective heat gain in temperatures greater than 35°C. The regression equation for fig 1A (y = 0.2902x+24.559) can be used to predict skin temperature at a given air temperature, and thus determine when evaporative cooling becomes the sole form of heat loss. In order to achieve thermal equilibrium, the rate of metabolic heat production and heat gain from the environment via convection and radiation, must be dissipated through the evaporation of sweat. The regression equation from fig 1C (y = 0.6804x –4.3708) can be used to determine the evaporation of sweat required to maintain thermal equilibrium and avoid an increase in core body temperature. Therefore, understanding of sweat rates induced in tennis provides valuable information that can be used to predict when the environment might pose a threat to a player's health and safety. It has been suggested that the level of dehydration is involved with a higher rectal temperature, thereby increasing the risk of heat illness.30,31 However, fig 4 demonstrates that the level of dehydration did not produce a greater change in rectal temperature. This finding occurred because it is the exercise intensity or metabolic rate that is the driving mechanism behind rectal temperature, not dehydration.27,32 Figure 4 also demonstrates the relatively low levels of dehydration, which is likely a reflection of the ability for tennis players to regularly consume fluids during each change of ends. This study found players consumed a mean (SD) of 0.77 (0.48) litres of fluid during the match with a maximum of 2.08 litres. This adequate hydration means the common trend for heart rate to be higher during exercise in more stressful environmental conditions (cardiovascular drift) was avoided, and is illustrated by the lack of association between heart rate and air temperature in fig 1E. The moderate thermal strains, particularly the control of rectal temperature, means thermoregulation is successful, and the environment poses minimal risk to player health and safety.
Comfort and perceived exertion
Rating of thermal comfort is defined as the “subjective satisfaction with the thermal environment”.33 Thermal comfort is an important factor during tennis not only because it enhances the enjoyment of the sport but it might also serve as a protective mechanism to modify behaviour and protect core body temperature.34 Presumably increasing perception of exertion/fatigue might also prompt behavioural change. Skin temperature plays a major role in a player's thermal comfort as the two are directly related.35,36,37,38,39,40 This is evident in the present investigation, which has demonstrated a positive association between skin temperature and air temperature (fig 1A) and between thermal comfort and air temperature (fig 5A). Further analysis has also found thermal comfort and skin temperature to also be positively correlated (R2 = 0.46; p<0.001). Therefore in warmer weather, a player's skin temperature increases and they sense thermal discomfort.
Conclusion
The present investigation offers descriptive information on the thermoregulatory and subjective strains experienced by tennis players over a range of environmental air temperatures. Thermal stress in tennis generally does not impose a risk to health and safety due to hyperthermia probably because of the moderate overall exercise intensity. Body core temperature was controlled in the range of air temperatures (14.5–38.4°C). Despite the moderate thermoregulatory strains, warm conditions result in marked thermal discomfort due to high skin temperature.
Acknowledgements
The authors gratefully acknowledge the International Tennis Federation Sport Science Research Grant Programme for the invaluable support given to this study.
Abbreviations
WBGT - wet bulb globe temperature index
Footnotes
Competing interests: None declared.
References
- 1.Brotherhood J R. The practical assessment of heat stress. In: Hales JRS, Richards DAB, eds. Heat stress: physical exertion and environment. London: Elsevier, 1987451–468.
- 2.Bergeron M F, Maresh C M, Kraemer W J.et al Tennis: a physiological profile during match play. Int J Sports Med 199112474–479. [DOI] [PubMed] [Google Scholar]
- 3.Christmass M A, Richmond S E, Cable N T.et al Exercise intensity and metabolic response in singles tennis. J Sports Sci 199816739–747. [DOI] [PubMed] [Google Scholar]
- 4.Dawson B, Elliott B, Pyke F.et al Physiological and performance responses to playing tennis in a cool environment and similar intervalized treadmill running in a hot climate. J Hum Mov Stud 19851121–34. [Google Scholar]
- 5.Elliott B, Dawson B, Pyke F. The energetics of singles tennis. J Hum Mov Stud 19851111–20. [Google Scholar]
- 6.Ferrauti A, Bergeron M F, Pluim B M.et al Physiological responses in tennis and running with similar oxygen uptake. Eur J Appl Physiol 20018527–33. [DOI] [PubMed] [Google Scholar]
- 7.Novas A M P, Rowbottom D G, Jenkins D G. A practical method of estimating energy expenditure during tennis play. J Sci Med Sport 2003640–50. [DOI] [PubMed] [Google Scholar]
- 8.Seliger V, Ejem M, Pauer M.et al Energy metabolism in tennis. Int Z Angew Physiol 197331333–340. [DOI] [PubMed] [Google Scholar]
- 9.Smekal G, von Duvillard S P, Pokan R.et al Changes in blood lactate and respiratory gas exchange measured in sports with discontinuous load profiles. Eur J Appl Physiol 200389489–495. [DOI] [PubMed] [Google Scholar]
- 10.Therminarias A, Dansou P, Chirpaz‐Oddou M F.et al Effects of age on heart rate response during a strenuous match of tennis. J Sports Med Phys Fitness 199030389–396. [PubMed] [Google Scholar]
- 11.Therminarias A, Dansou P, Chirpaz‐Oddou M F.et al Hormonal and metabolic changes during a strenuous tennis match. Effect of Ageing. Int J Sports Med 19911210–16. [DOI] [PubMed] [Google Scholar]
- 12.Reilly T, Palmer J. Investigations of exercise intensity in male singles lawn tennis. J Sports Sci 199311543–558.7906740 [Google Scholar]
- 13.International Tennis Federation Rules of tennis. London: International Tennis Federation. http://www.itftennis.com/abouttheitf/rulesregs/rules.asp (accessed 30 January 2007)
- 14.Ramanathan N L. A new weighting system for mean surface temperature of the human body. J Appl Physiol 196419531–533. [DOI] [PubMed] [Google Scholar]
- 15.Bedford T.The warmth factor in comfort at work. London, Industrial Health Research Board; 1936, Report No. 76.
- 16.Borg G A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 198214377–381. [PubMed] [Google Scholar]
- 17.Davies C T M, Brotherhood J R, Zeidifard E. Temperature regulation during severe exercise with some observations on effects of skin wetting. J Appl Physiol 197641772–776. [DOI] [PubMed] [Google Scholar]
- 18.Forgan‐Smith Exertion‐induced heatstroke. Med J Aust 1987146154–155. [PubMed] [Google Scholar]
- 19.Savdie E, Prevedoros H, Irish A.et al Heat stroke following rugby league football. Med J Aust 1991155636–639. [DOI] [PubMed] [Google Scholar]
- 20.Brooks G A, Fahey T D, White T P.et alExercise physiology. Human bioenergetics and its applications. 3rd edn. Mountain View, California: Mayfield Publishing Company, 2000;476,
- 21.Maron M B, Horvath S M. The marathon: a history and review of the literature. J Med Sci Sports 197810137–150. [PubMed] [Google Scholar]
- 22.Lind A R. A physiological criterion for setting thermal environmental limits for everyday work. J Appl Physiol 19631851–56. [DOI] [PubMed] [Google Scholar]
- 23.Tennis Australia Australian Open Program 2006. Melbourne, Australia: Tennis Australia 2006
- 24.American College of Sports Medicine Position stand on heat and cold illnesses during distance running. Med Sci Sports Exerc. 1996;28:i‐x [PubMed]
- 25.Davies C T M, Thompson M W. Aerobic performance of female marathon and male ultramarathon athletes. Eur J Appl Physiol 197941233–245. [DOI] [PubMed] [Google Scholar]
- 26.Costill D L, Fox E L. Energetics of marathon running. Med Sci Sports Exerc 1969181–86. [Google Scholar]
- 27.Noakes T D, Myburgh K H, du Plessis J.et al Metabolic rate, not percent dehydration, predicts rectal temperature in marathon runners. Med Sci Sports Exerc 199123443–449. [PubMed] [Google Scholar]
- 28.Nadel E R. Control of sweating rate while exercising in the heat. Med Sci Sports Exerc 19791131–35. [PubMed] [Google Scholar]
- 29.Snellan J W, Mitchell D, Wyndham C H. Heat of evaporation of sweat. J Appl Physiol 19702940–44. [DOI] [PubMed] [Google Scholar]
- 30.Montain S J, Coyle E F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol 1992731340–1350. [DOI] [PubMed] [Google Scholar]
- 31.Sawka M N. Physiological consequences of hypohydration: exercise performance and thermoregulation. Med Sci Sports Exerc 199224657–670. [PubMed] [Google Scholar]
- 32.Berggren G, Christensen E H. Heart rate and body temperature as indices of metabolic rate during work. Eur J Appl Physiol 195014255–260. [DOI] [PubMed] [Google Scholar]
- 33.Bligh J, Johnson K G. Glossary of terms for thermal physiology. J Appl Physiol 197335941–961. [DOI] [PubMed] [Google Scholar]
- 34.Frank S M, Raja S N, Bulcao C F.et al Relative contribution of core and cutaneous temperatures to thermal comfort and autonomic responses in humans. J Appl Physiol 1999861588–1593. [DOI] [PubMed] [Google Scholar]
- 35.Adair E R. Skin, preoptic, and core temperatures influence behavioural thermoregulation. J Appl Physiol 197742559–564. [DOI] [PubMed] [Google Scholar]
- 36.Adams W C, Fox R H, Fry A J.et al Thermoregulation during marathon running in cool, moderate, and hot environments. J Appl Physiol 197581030–1037. [DOI] [PubMed] [Google Scholar]
- 37.Bleichert A, Behling K, Scarperi M.et al Thermoregulatory behaviour of man during rest and exercise. Pflügers Arch 1973338303–312. [DOI] [PubMed] [Google Scholar]
- 38.Chatonnet J, Cabanac M. The perception of thermal comfort. Int J Biometeorol 19659183–193. [Google Scholar]
- 39.Robinson S. Physiological adjustments to heat. In: Newburgh, LH, eds. Physiology of heat regulation and the science of clothing. Philadelphia, Pennyslvania: WB Saunders, 1949193–231.
- 40.Weiss B, Laties V G. Behavioural thermoregulation. Science 19611331338–1344. [DOI] [PubMed] [Google Scholar]