Abstract
Rectus abdominis muscle strains are common and debilitating injuries among competitive tennis players. Eccentric overload, followed by forced contraction of the non‐dominant rectus abdominis during the cocking phase of the service motion is the accepted injury mechanism. A tennis‐specific rehabilitation program emphasising eccentrics and plyometric strengthening of the abdominal wall muscles, contributes to the complete functional recovery in tennis players, and could help reduce recurrences.
Rectus abdominis (RA) muscle strain is one of the most specific tennis related injuries. True incidence of such injuries is not known, however several sports physicians consider them to be very common.1,2,3,4,5 Abdominal muscles strains are frequent in tennis players at all levels of competition, and are usually caused by indirect trauma. These debilitating injuries give rise to prolonged periods of discomfort and to withdrawal from competition, occurring mainly due to the inability to perform the service motion properly. Propensity to recurrence implies these injuries are usually considered severe, particularly for professional players. Most abdominal wall injuries involve the RA contralateral to the dominant arm; nevertheless, oblique muscle strains could also affect tennis players.6
This article examines the anatomy of the anterolateral abdominal wall, as well as abdominal muscles activation patterns in relation to tennis stroke biomechanics. A practical rehabilitation guide specifically designed for tennis players is outlined, emphasising the relevance of eccentric‐plyometric strengthening in achieving a complete recovery as well as for the prevention of recurrences.
Anatomy
The muscular layer of anterolateral abdominal wall is made up of four flat muscles, namely the external oblique (EO), the internal oblique (IO), the transverses (TA) and the rectus abominis (RA).7 The recti are paired straplike muscles, separated at the midline by the linea alba. Each muscle has two tendinous origins; a medial head arising from the anterior surface of the pubis symphysis, and a larger lateral portion originating from the upper border of the pubic crest, which together form the muscle mass inserting onto the fifth, sixth and seventh costal cartilages.7 The aponeuroses of the IO, EO and TA fuse to form the linea alba, a strong midline fibrous structure firmly attached to the xiphoid process above, and the pubic symphysis below. The muscle is partially interrupted by three fibrous bands or tendinous intersections, which blend inseparably with the anterior layer of the rectus sheath. They are found at the level of the umbilicus, the xiphoid process, and midway between the two. Nerve supply to the RA derives from the lower six thoracic nerves.7
The primary function of the RA is to flex the spine and compress the abdominal and pelvic cavities. Secondarily, it assists in respiration by pulling the chest downward and depressing the lower ribs.
The remaining anterolateral muscles exert secondary mobiliser functions and contribute significantly to core stability. The oblique orientation of the IO and EO muscles make them responsible for flexing and rotating the spine while simultaneously supporting the abdomen and pelvis.4 The TA muscle, a key pelvic stabiliser for running and throwing activities, contracts prior to lower extremity musculature in anticipation of a foot strike during running activities, and prior to arm and shoulder cocking during throwing, also supports the abdomen and the pelvis in combination with the other abdominal wall muscles.8
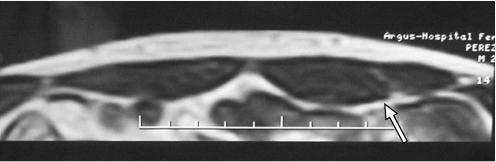
Contralateral RA muscle hyperthrophy (on the side of the non‐dominant arm) is a common finding among competitive tennis players3,9 (fig 1). Increased strain transferred through this muscle during the throwing phase of the serving action could lead to hypertrophy,10 and increased electromyographic (EMG) activity.
Figure 1 Axial MRI view of a 20‐year old male tennis player showing hyperthrophy of the left (non‐dominant) rectus abdominis (arrow). Informed consent was obtained for publication of this figure.
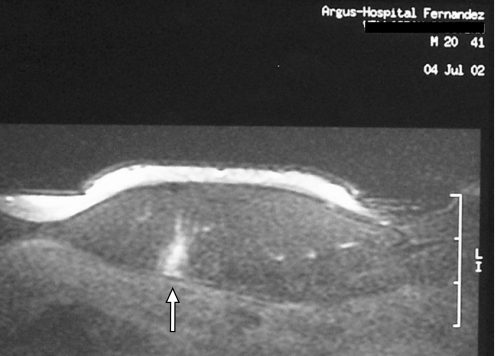
RA muscle fibril disruptions tend to occur along the deep epimysial surface below the umbilicus3,9 (fig 2), a potential site of weakness, where the muscle is not covered by the tendinous intersection and exposes a longer segment to strain.9
Figure 2 Axial proton density image of left rectus abdominis in a 20‐year old male tennis player shows a small hyperintense focal area compatible with muscle oedema, haemorrhage and fibril disruption on the deep epymisial surface (arrow). In cases of low severity RA injuries, MRI is useful to distinguish minor tears from delayed onset muscle soreness (DOMS) syndrome. Informed consent was obtained for publication of this figure.
Biomechanics
Depending upon their anatomical, biomechanical and physiological characteristics, abdominal wall muscles can be classified as belonging to one of two groups, stabilisers and mobilisers.11 The stabilisers are better equipped for postural holding with an anti‐gravitational function. The mobilisers are better setup for rapid ballistic movements and are often referred to as “task muscles”. The RA together with the lateral fibres of EO are considered the prime mobilisers of trunk flexion, while the IO and TA are the major stabilisers of trunk movements.11 Another distinguishing characteristic relevant for rehabilitation is that the stabiliser muscles tend to weaken and mobilisers tend to shorten.
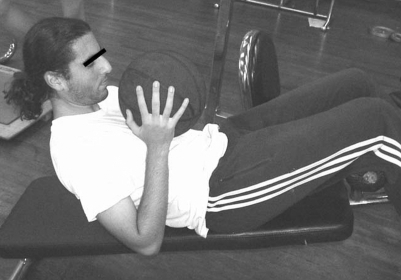
In tennis players, the abdominal musculature plays a significant role in trunk and core stability providing a mechanical link between the lower and upper limbs, and the service motion is undoubtedly involved in the injury mechanism of RA strain. During the serve, a large amount of angular momentum is transferred to the racquet; trunk rotation and flexion after lumbar extension are essential parts of force generation for the serve. During the cocking phase, players move the racquet away from the body by combining abduction with external rotation of the shoulder and lumbar spine hyperextenxion, in order to increase racket distance for speed and power generation12,13 (fig 3). When complete axial skeleton extension is achieved, the abdominal muscles are maximally stretched, storing elastic energy. Similar throwing motions have shown high EMG activity on the non‐dominant RA during this phase.14 On movement reversal, abdominal muscles contract powerfully, using the elastic energy stored while placing the non‐dominant RA at high risk for injury.
Figure 3 Late cocking phase of serve in a professional tennis player combine lumbar spine hyperextension and shoulder abduction and external rotation. Eccentric overload of the abdominal musculature during this phase is the accepted injury mechanism for RA muscle strains. Informed consent was obtained for publication of this figure.
Consequently, the most common injury mechanism of the RA in tennis players involves a forced concentric contraction of the abdominal musculature when the spine is completely hyperextended.2,3,6,9 This movement occurs when and overhead is hit behind the player like in the modern “kick serve”.
Chow et al10 have studied lower trunk muscle activity during different types of tennis services (flat, topspin, slice). No major differences in overall muscle pattern of activation across different type of services were found. Bilateral differences in muscle activation were more pronounced in RA and EO than in IO and erector spinae (ES). In general, lower trunk muscles became active toward the end of the windup phase. Peak EMG values were observed during the cocking and the acceleration phase. Regardless of the serve type executed, the non‐dominant RA showed greater activity than the dominant RA during all phases of the serve. Significant bilateral differences in EMG activity were found in the RA during the ascending wind up (average absolute differences 2.5%), as well as during the cocking phase (38.5%) and during the acceleration phase (25.5%).10
Although muscle activity was relatively low during the wind up phase, greater activation of muscles on the non‐dominant side indicated that onset of lateral trunk rotation towards the non‐dominant side, extension (ES), and axial rotation to the right (EO and ES) all occurred towards the end of this phase.10
The cocking phase was considered the coiling or loading of the upper body, which enhanced the force acting on the racquet during the acceleration phase; the longer distance resulted in higher racket velocity at ball impact. Because the trunk was flexing to the left (right handed players), falling backward, and rotating to the right at the same time, it was logical to consider the left RA and EO (a contralateral trunk rotator) as more active than their counterparts.
All muscles showed moderate to high activity during the acceleration phase. EMG activity of the RA, the EO and the IO suggested that these muscles were responsible for trunk flexion during this phase.10 During acceleration, most abdominal muscles were more active in the topspin serve than in other two types, although differences were statistically significant only in the right RA, the left EO and the right IO. The left and right EO muscles were very active (greater than 50% of peak muscle activity level) during the force production phase of the serve.13
All abdominal muscles showed drastic activity decrease after ball impact (follow‐through phase), while the ES muscle became more active.10
Abdominal muscles were more active during racquet up‐swing in the topspin serve than in other two types. Significant differences in EMG activity across different serve types were found in the left RA during the windup phase, and in the right RA during the cocking and acceleration phase.10
Most abdominal and lower back muscles undergo eccentric contractions during cocking and follow‐through phases. Moderate activity observed in these same muscles during eccentric contractions, suggest that eccentric training for the lower trunk muscles might be beneficial for tennis players.10
It is also important to consider the strength ratio between flexor and extensor groups of the trunk. Normal subjects have shown greater extension strength, while tennis players have shown a relative trunk extensor strength imbalance, showing greater trunk flexion strength.15 The implication of this adaptation is still unknown; however, the authors recommended emphasising on extensors strength such as ES, gluteus during tennis players conditioning.
Diagnosis
The diagnosis of a RA tear in tennis players is usually straightforward. An indirect muscle injury mechanism involving eccentric‐concentric action is the most prevalent. Acute direct blows to the abdominal wall are extremely rare, and intra‐abdominal illnesses are usually not difficult to differentiate from abdominal wall sport‐related injuries.
Typical clinical presentation occurs in a competitive player referring acute contralateral RA pain during service or post‐eccentrics pain pattern (delayed onset muscle soreness, DOMS). The latter usually progresses to more intense pain, preventing further tennis participation. A history of similar prior episodes is common.
Physical examination shows tenderness of the affected RA, usually below the umbilicus. A functional examination of the entire abdominal musculature during isometric, concentric, eccentric and plyometric contraction is warranted. These manoeuvres attempt to reproduce the injury mechanism previously described, and have been shown to be clinically useful in order to stratify lesion severity (Table 1).2
Table 1 Clinical grading system for rectus abdominis muscle strains2.
| Severity | Description |
|---|---|
| Severe | Painful isometric contraction (Valsalva manoeuvre) and simple overhead reaching |
| Moderate | Painful trunk “sit‐up” motion (concentric contraction) |
| Slight to mild | Previous manoeuvres do not elicit pain |
Figure 6 Abdominal strengthening exercises for the oblique abdominal muscles. Informed consent was obtained for publication of this figure.
Figure 7 Eccentric strengthening of the abdominal muscles. Low speed declined‐plane exercise with emphasis on downfall control. Informed consent was obtained for publication of this figure.
Imaging studies are not strictly necessary for the diagnosis of tennis‐related RA pain; nevertheless, these could help to determine the severity of the strain and to predict the recovery time. Some authors have recommended obtaining x‐rays in all cases in order to rule out a rib fracture.2 However, in these cases of indirect trauma in skeletally mature athletes, this was not considered necessary routinely. Diagnostic ultrasound has proven useful in this type of injury, but MRI contributes better quality information and more precise imaging of lesional extension. The use of surface coils is recommended, especially for re‐injury evaluation, given their capacity to detect scar tissue and intramuscular tissue changes.
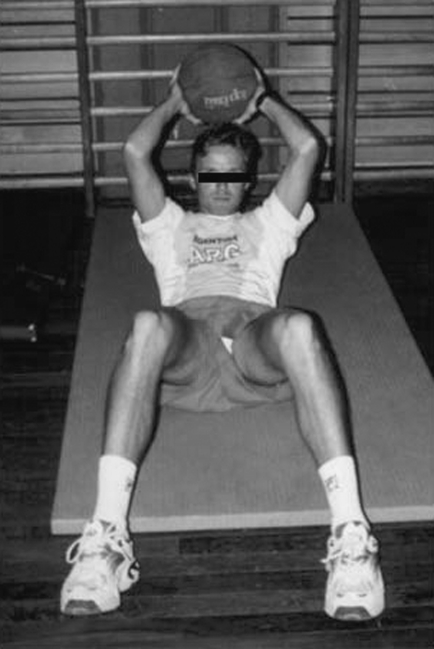
Figure 8 Sport‐specific throwing exercise with “medicine balls”. Informed consent was obtained for publication of this figure.
Figure 9 Plyometric exercise of the abdominal muscle wall using “medicine balls”. Informed consent was obtained for publication of this figure.
Ultrasound images of RA injuries are characterised by normal echogenic fibrillar pattern disruption, with fluid‐filled clefts traversing the disorganised muscle. This abnormality is thought to represent disrupted muscle fibrils, oedema and haemorrhage. The injury is usually seen on the deep surface of the muscle belly, with an average length on the coronal plane of 32 mm.9
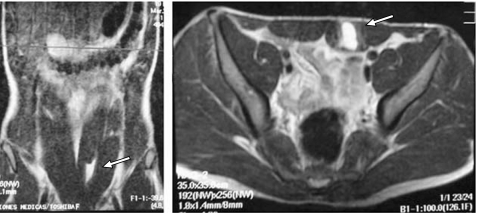
On MRI, a muscle tear shows focal high intensity signal areas with muscle disruption, whereas scar tissue generates a low intensity signal on all pulse sequences (fig 4). MRI is considered the modality of choice for muscle evaluation given its excellent definition, its unique capacity to differentiate between acute muscle strain and DOMS, as well as for chronic muscles injury and healing process evaluation (figs 2 and 5).
Figure 4 Coronal and axial MR images of 18 year‐old male tennis player suffering acute RA strain lesion. Extended area of haemorrhage and fibril disruption (arrow) corresponds to a severe injury. Informed consent was obtained for publication of this figure.
Figure 5 A 27 year‐old male professional tennis player suffering RA pain during serving; clinical history revealed four episodes of RA injury. Axial T1 MR image shows scar tissue within the left muscle (arrow). Informed consent was obtained for publication of this figure.
What is already known on this topic
Rectus abdominis muscles strains are common and debilitating injuries among competitive tennis players.
Eccentric overload, followed by forced contraction of the non‐dominant rectus abdominis during the cocking phase of the service motion is the accepted injury mechanism.
What this study adds?
A practical rehabilitation guide specifically designed for tennis players is outlined.
Emphasis is placed upon the relevance of eccentric‐plyometric strengthening in achieving a complete recovery.
Treatment
Initial treatment of RA strains includes abstaining from the offending activity and cryotherapy. Players suffering moderate and severe injuries should avoid tennis practice. Those athletes complaining of DOMS or slight strains, confirmed through imaging studies, can be allowed to play, but only under special circumstances.
A five‐step program, designed to guide treatment of RA strains and reduce re‐injury risk has been described by these authors.3,16 The steps involved are: (a) pain and inflammation control, rest; (b) isometric strengthening and stretching; (c) concentric strengthening; (d) eccentric‐plyometric strengthening; and (e) maintenance and re‐injury prevention (Table 2).
Table 2 Rehabilitation program for RA injuries in tennis players.
| Stage | Tasks |
|---|---|
| 1. Control of pain and inflammation, and protection | Rest is the hallmark of this stage – avoid any participation in tennis |
| Cryotherapy on painful area (20 min every 2–3 h) | |
| Physical therapy | |
| Evaluation of entire kinetic chain and core stability | |
| 2. Isometric strengthening and stretching | Start isometric contractions in a supine position, with the knee and hip flexed (3 sets of 10–20 repetitions, twice a day) |
| Progressive passive stretching, starting with the supra‐umbilical portion of the RA | |
| Conditioning of uninjured links (shoulder, hip, and knee) of the service kinetic chain and core stability training | |
| 3. Concentric strengthening | Common abdominal exercises with the hip and knee flexed (“crunches”), and sets of 20–30 repetitions, progressing to more dynamic exercises (eg, bent knee sit‐ups) |
| Increase time of stretching position to 7–20 s | |
| Add strengthening exercises for oblique abdominal muscles (fig 6) and the lower RA muscle (eg, “reverse crunches”, “hanging knee‐up”), and core stability training | |
| Tennis practice can be allowed, avoiding overhead shots (service, smash, high ground strokes and volleys) | |
| 4. Eccentric strengthening and plyometrics | Declined plane exercise (low speed) (fig 7) with the emphasis on proper downfall control |
| Progression to faster movements, alternating with weights and, finally, moving on to fast exercises with light to moderate weights | |
| Start hitting second services and overhead ground strokes, and start playing matches | |
| Technical correction of service motion errors that predispose to this type of injury: too high ball toss, lumbar hyperextension, excessive top spin shot, etc. | |
| Throwing exercises with free weights and medicine balls (fig 8), and multiarticular movements | |
| Plyometric training (final phase of the rehabilitation programme) – exercises with appropriate shortening‐stretching cycle times (similar to the service cycle), with sets of 6–8 repetitions, progressing to maximum power (figs 9 and 10) | |
| Tennis service practice (interval – full) | |
| Return to competition | |
| 5. Maintenance and re‐injury prevention | Keep up exercises of phases 3–4 during the competitive period, 2–3 times per week |
The main objective of staging the rehabilitation program is to monitor results while keeping the player motivated; tasks described for each stage can nevertheless overlap to establish a program continuum. Full recovery, allowing a safe competition comeback, usually requires lengthier periods than those initially estimated by players (ranging from 3 to 8 weeks, depending on injury severity). Re‐injury is common among ranked players, and treating physicians should share responsibility for poor results. Clinical experience has shown the authors that common mistakes during rehabilitation include early return to competition, and insufficient eccentric strengthening of abdominal musculature. This rehabilitation program was evaluated in a clinical prospective cohort study design, including 21 competitive tennis players (18 men, 3 women, age average 21.3±3.2 years) suffering RA strains. Ultrasound and/or MRI images were obtained in all patients. All players presented non‐dominant RA hypertrophy. Clinical grading revealed, 6 minor, 11 moderate and 4 severe injuries. Average time to full return to sport was 4.5 weeks (range 2–8 weeks). No re‐injuries had occurred by the time of last follow‐up visit (mean follow‐up duration was 13 months, range 6–18 months). The authors conclude that eccentric‐plyometric strengthening helped competitive tennis players to attain complete functional recovery after suffering a RA strain. Sport‐specific exercises also contributed to recurrence prevention.
Understanding how different abdominal exercises elicit particular muscle activity is essential for sports physician and physical therapists developing rehabilitation programmes specifically for tennis players. Several studies have analysed trunk muscle activity during abdominal muscle exercises.17,18 Out of several exercises evaluated by Escamilla et al,17 the “power wheel roll‐out” and the “hanging knee‐up” showed highest EMG activity of the lower RA muscle (fig 10). Interestingly, the same exercises were effective in activating the IO and extraneous (non‐abdominal) muscles such as the latissimus dorsi. The “power wheel roll‐out” is a highly effective exercise for abdominal musculature, and should be included in the eccentric strengthening stage of RA strains rehabilitation, remembering to supervise execution under proper technique.
Figure 10 During the roll‐out portion of the “power‐wheel roll‐out”, the abdominal musculature contracts eccentrically to resist the attempt of gravity to extend the trunk and rotate the pelvis. Informed consent was obtained for publication of this figure.
A complete review of eccentric‐plyometric muscle activity is beyond the scope of this article. Nevertheless, some practical issues regarding rehabilitation should be outlined. Eccentric contraction represents muscle loading involving an external application, with tension increasing during physical lengthening of the musculotendinous unit.19 Several studies have shown that eccentric training has a preponderant roll in improving sport performance and rehabilitation.19,20,21,22 There is evidence to suggest that eccentric exercises function best during the subacute period, once necessary soft tissue healing constraints have been overcome, and successful tolerance to isometric and concentric exercises has been reached.19 Depending on the degree of injury severity and on anti‐inflammatory treatment success, the subacute phase should be completed within seven days, at which time submaximal, slow speed eccentrics (90–120°/s) can be introduced. Collagen maturation proceeds progressively, reaching moderate tensile strength within three weeks.23 Early strength changes or gains (within the first three weeks), can be rapid and dramatic; prolonged strength changes are gradual and represent structural or morphologic adaptations in muscle.24 Manheimer25 established that eccentric exercises produce greater strengthening that concentrics exercises, only in the first nineteen days after injury, potentially due to a differential effect on the neuromuscular system. Because of low oxygen requirement needed during eccentric muscle exercising, rest periods between training bouts do not need to last long. Just 30 s to 1 min are sufficient to permit controlled repeat sets in most patients.26 Optimal strengthening effects appear to be gained in 3 to 20 repetitions divided into a maximum of three sets. It is also clinically useful to structure training stimuli with timed bouts of 30 s, in which patients are not required to count repetitions. Recommended eccentric training frequency is usually three times a week. Studies indicating four weekly training sessions showed minimal strength improvement, and in some cases even caused loss of force.21,27 In fact, the physiological process underlying DOMS resolution would indicate that the safest frequency is probably twice a week.
Although a single session of eccentric exercises can cause significant muscle damage, it also confers considerable protection against similar injuries during subsequent sessions.28,29 One possible explanation for this phenomenon could be that initial eccentric sessions destroy the muscle fibres originally causing DOMS, repeated bouts find fewer susceptible fibres available as targets, thus leading to symptom reduction. Contractions in the shortest position of the abdominal muscles (“inner range exercises”) are also advisable, in an attempt to restore normal length muscle, especially in cases of lumbar hyperlordosis. Eccentric activity combined with “inner range” exercises, have shown in some studies to generate improved serial sarcomere adaptation.11
Plyometric exercise can be characterised as a rapid eccentric loading of the musculoskeletal complex, with quick powerful movements involving a pre‐stretching session that activates the stretch–shortening cycle.30 The objective of plyometric training is to heighten the excitability of the nervous system in order to improve neuromuscular reactive ability. Any exercise incorporating the series elastic component of muscle together with the myotatic reflex, will generate a more powerful muscular response, and is therefore considered plyometric. The goal of plyometric training is to reduce amortisation phase duration, or the time between undergoing a yielding eccentric phase and initiating an overcoming concentric contraction.
Several authors have shown that an eccentric contraction immediately preceding a concentric contraction will heighten elastic energy storage, significantly increasing the force generated concentrically. The mechanism for this in concentric force increase is the ability of the muscle to use the force produced by the serial elastic component. During eccentric contraction, the load is transferred to the elastic component and stored as elastic energy. As the muscle undergoes concentric contraction, the elastic energy stored in the non‐contractile elements can be recovered, and used to contribute to the shortening contraction. The ability to use stored elastic energy is affected by three variables: time, magnitude of stretch and velocity of stretch.30 Concentric contraction enhancement is most effective when the preceding eccentric contraction is of short range and is performed quickly and without delay. The faster a muscle is eccentrically loaded or lengthened, the greater the resultant concentric load produced. In summary, successful plyometric training relies more on the rate of stretching rather than its length. In addition, if the amortisation phase is slow, elastic energy is wasted as heat and the stretch reflex is not activated. However, the more quickly an athlete can switch from yielding work to overcoming work, the more powerful the response. Plyometric training is a key factor in the rehabilitation of RA muscles injuries in tennis players, given its ability to increase the strength loads that the neuromuscular system is able to accept. Competitive junior tennis players are likely to suffer RA muscle strains when they start hitting powerful services. Eccentric training should be indicated with caution in this population of younger players, whose immature CNS and lower Golgi tendon organ threshold might not tolerate the excessive eccentric loads produced by plyometric training.30
Tennis service biomechanic principles should be considered when designing a rehabilitation program for RA strains, for which close collaboration with the coach and trainer is recommended. During early recovery stages, slice serving is useful in an attempt to unload the injury site as well as avoid a high ball toss. Once healing is achieved, coaches and trainers should encourage the “push through” serving motion, emphasising proper use of ground reaction force, knee flexion, hip‐trunk counter rotation, scapular retraction and long axis rotation.31
Abbreviations
DOMS - delayed onset muscle soreness
EMG - electromyograph
EO - external oblique muscle
ES - erector spinae muscle
IO - internal oblique muscle
RA - rectus abdominis muscle
TA - transverse muscle
Footnotes
Competing interests: None declared.
Informed consent was obtained for publication of figures 1–10.
References
- 1.Cousteau J P. Meet the expert. Med Sci Tennis 2001317 [Google Scholar]
- 2.Lehman R C. Thoracoabdominal musculoskeletal injuries in racquet sports. Clin Sports Med Vol 19887267–276. [PubMed] [Google Scholar]
- 3.Maquirriain J, Ghisi J P, Mazzucco J.et al Abdominal muscle strain injuries in the tennis player: treatment and prevention. Med Sci Tennis 2002314–15. [Google Scholar]
- 4.Johnson R. Abdominal wall injuries: rectus abdominis strains, oblique strains, rectus sheath hematoma. Curr Sports Med Rep 2006599–103. [DOI] [PubMed] [Google Scholar]
- 5.Pluim B, Safran M. Injuries of the trunk and spine. In: Pluim B, Safran M, eds. From breakpoint to advantage. Vista, California: Racquet Tech Publishing, 2004
- 6.Maquirriain J, Ghisi J P. Uncommon abdominal muscle injury in a tennis player: internal oblique strain. Br J Sports Med 200640462–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Willams PL, Warwick R, eds. Gray's anatomy, 36th edn. London: Churchill Livingstone 1985
- 8.Hodges P W, Richardson C A. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehab 1999801005–1012. [DOI] [PubMed] [Google Scholar]
- 9.Connell D, Ali K, Javid M.et al Sonography and MRI of rectus abdominis muscle strain in elite tennis players. Am J Roentgen 20061871457–1461. [DOI] [PubMed] [Google Scholar]
- 10.Chow J W, Shim J S, Lim Y T. Lower trunk muscle activity during the tennis serve. J Science Med Sports 20034512–518. [DOI] [PubMed] [Google Scholar]
- 11.Norris C M. Functional load abdominal training: part 1. Phys Ther Sports 2001229–39. [Google Scholar]
- 12.Elliot B. Biomecánica de los golpes de Tenis. In: Maquirriain J, ed. En Medicina Deportiva Aplicada al Tenis. Beunos Aires: International Tennis Federation, 200227–38.
- 13.Anderson M B. Comparison of muscle patterning in the overarm throw and tennis serve. Res Q 197950541–553. [Google Scholar]
- 14.Watkins R G, Dennis S, Dillin W H.et al Dynamic EMG analysis of torque transfer in professional baseball players. Spine 198914404–408. [DOI] [PubMed] [Google Scholar]
- 15.Roetert E P, McCormick T J, Brown S W.et al Relationship between isokinetic and functional trunk strength in elite junior tennis players. Isokin Ex Sci 1996615–20. [Google Scholar]
- 16.Maquirriain J, Ghisi J P, Kokalj A M. Lesiones de los músculos abdominales en el tenista. In: Maquirriain J, Pluim B, Ghisi JP, eds. En Medicina Deportiva Aplicada al Tenis. Buenos Aires: International Tennis Federation, 2005
- 17.Escamilla R F, Babb E, DeWitt R.et al Electomyographic analysis of traditional and nontraditional abdominal exercises: implications for rehabilitation and training. Phys Ther 200686656–671. [PubMed] [Google Scholar]
- 18.Konrad P, Schmitz K, Denner A. Neuromuscular evaluation of trunk‐training exercises. J Athletic Training 200136109–118. [PMC free article] [PubMed] [Google Scholar]
- 19.Albert M.Eccentric muscle training in sports and orthopaedics. 2nd edn. New York: Churchill Livingstone, 1995
- 20.Dean E. Physiology and therapeutic implications of negative work. A review. Phys Ther 198868233. [DOI] [PubMed] [Google Scholar]
- 21.Duncan P W, Chandler J M, Cavanaugh D K.et al Mode and speed specificity of eccentric and concentric exercise training. J Orthop Sports Phys Ther 19891170. [DOI] [PubMed] [Google Scholar]
- 22.Hinton R Y. Isokinetic evaluation of should rotational strength in high school baseball pitchers. Am J Sports Med 198816274. [DOI] [PubMed] [Google Scholar]
- 23.Hardy M A. The biology of scar formation. Phys Ther 1989691017. [DOI] [PubMed] [Google Scholar]
- 24.Moritani T, Devries H A. Neural factors versus hypertrophy in the time course of muscle strength gain. Am J Phys Med 197958115. [PubMed] [Google Scholar]
- 25.Manheimer J S. A comparison of strength gain between concentric and eccentric contractions. Phys Ther 1969491207. [DOI] [PubMed] [Google Scholar]
- 26.Laycoe R R, Marteniuk R G. Learning and tension as factors in static strength gains produced by static and eccentric training. Res Q 197142304. [PubMed] [Google Scholar]
- 27.Komi P V, Burkirk E R. Effect of eccentric and concentric muscle conditioning on tension and electrical activity of the human muscle. Ergonomics 197215417. [DOI] [PubMed] [Google Scholar]
- 28.Ebbeling C B, Clarkson P M. Muscle adaptation prior to recovery following eccentric exercise. Eur J Appl Physiol Occupat Physiol 19906026. [DOI] [PubMed] [Google Scholar]
- 29.McHugh M P. Recent advances in the understanding of the repeated bout effect: the protective effect against muscle damage from a single bout of eccentric exercise. Scand J Med Sci Sports 20031388–97. [DOI] [PubMed] [Google Scholar]
- 30.Voight M L, Draovitch P. Tippett. Plyometrics. In: Albert M, ed. Eccentric muscle training in sports and orhtopaedics. New York: Churchill Livingstone 1995
- 31.Kibler W B. Fundamentos para la generación de potencia en el tenis: el jugador de 4000 watts. In: Maquirriain J, Pluim B, Ghisi JP, eds. En Medicina Deportiva Aplicada al Tenis. Buenos Aires: International Tennis Federation, 2005