Abstract
Objective
To determine whether moderate water loss (∼1.5–2% of body mass (BM)) represents a significant impairment to soccer match‐play and the related fitness variables.
Methods
11 moderately active male soccer players (mean (SD) age 24.4 (3) years, BM 74.03 (10.5) kg, peak oxygen consumption 50.91 (4.0) ml/kg/min) volunteered to participate. The experimental procedure comprised: (1) a 45 min pre‐match period of cycle ergometry exercise (90% of individual ventilatory threshold); (2) the completion of a 45 min soccer match; and (3) the immediate post‐match performance of sport‐specific and mental concentration tests. The subjects completed the procedure on three occasions each in a different experimental condition (fluid intake (FL), no fluid (NF) and mouth rinse (MR)) in an individually randomised order. Core temperature (Tc), heart rates, plasma and urine osmolalities, BM, sweat rates and heat storage were all measured.
Results
The only condition‐dependent difference during the match‐play element of the protocol was a significantly increased Tc in the NF condition compared with the FL condition (39.28°C (0.35°C) and 38.8°C (0.47°C), respectively; p<0.05). The immediate post‐match performance of a sport‐specific fitness test was significantly impaired where FL had been denied (p<0.01). The post‐test evaluation of rating of perceived exertion and thirst indicated that the NF condition was perceived to be the most challenging (p<0.05).
Conclusions
The condition‐dependent differences in match‐play and post‐match tests demonstrate that moderate dehydration is detrimental to soccer performance. However, it remains unclear whether this could be attributable to water loss in itself or the negative psychological associations derived from a greater perception of effort in that condition.
Only a limited amount of recent information is currently available on the thermoregulatory responses of soccer players during competitive match‐play,1,2 and particularly the extent to which moderate levels of dehydration might affect performance.
Several studies have examined individual responses to soccer‐related activities including soccer‐simulated indoor shuttle running tests,3,4 soccer training drills5 and brief periods of a small‐sided indoor game.6 However, these studies were not specifically designed to address the issue of whether moderate water loss in itself elicits a physiologically detrimental effect to sports such as soccer. In addition, a recent study7 proposed that the outcome measures of exercise performed in windstill, indoor, conditions might not be directly related to outdoor sports performance owing to impaired heat dissipation as a result of limitations in convective cooling.
Although losses of ∼5% of body mass (BM) have been reported to occur in hot conditions,8 it is unclear whether the relatively small pre‐match to post‐match alterations in BM typically experienced in thermoneutral conditions (∼1.5–2% for players and referees)1,2,9 are sufficient to elicit a detrimental effect on soccer performance. It is well known that evaporation of sweat secreted on to the skin helps to limit the rise in core temperature (Tc),10 but it seems unlikely that, in the absence of any impairment to convective cooling, Tc values in a self‐paced game would reach critical levels in well‐conditioned players. It is also questionable whether excessive fluid intake (FL) is of value to performance when the time course to make water physiologically useful following ingestion, gastric emptying, intestinal absorption and changes in osmotic flow could be between 40 and 60 min.11,12 However, acute short‐term imbalances between body water compartments induced by match‐play could lead to a rapid increase in plasma osmolality (Posm),13 which would be disruptive to homeostasis.
It is also possible that negative associations between moderate dehydration and performance are driven by psychological factors associated with perceived discomfort where FL is denied or restricted rather than the physiological need to replace water loss in itself. For example, the tongue provides the first internal analysis of potentially ingestible stimuli and the sensory mechanisms embedded in the lingual epithelium are used to extract information about fluid.14 Mechanisms that affect water intake (through thirst) and water reabsorption (through antidiuretic hormone secretion) are subsequently invoked.13 Because of this, it is conceivable that frequent mouth rinsing with water might temporarily suppress this process.
It was the aim of this study to determine whether exercise induced, moderate dehydration significantly affects the physiological responses to a focused period of outdoor match‐play and the immediate post‐match performance of tests designed to ascertain whether relevant physiological and psychological characteristics were affected in this condition.
Methods
Experimental design
The study used a cross‐over design, with each subject performing the protocol on three separate occasions in three different conditions in an individually randomised order: (1) FL; (2) mouth rinse (MR) only; and (3) no fluid (NF) intake.
The exercise trials were held at the same time of the day on each of the three occasions to avoid diurnal variations in body temperature, and were each separated by 1 week. The experimental protocol comprised four main parts that all subjects completed simultaneously:
A 45 min period of laboratory exercise on cycle ergometers at an intensity equivalent to 90% of individual ventilatory threshold (24–25°C, 47–55% relative humidity, wind speed nil) to standardise pre‐match energy expenditure.
Following a 15 min rest period, all subjects participated in a well‐balanced and competitive 8 vs 8 outdoor soccer match of 45‐min duration on a full‐size 11‐aside Astroturf pitch (19–21°C, 46–57% relative humidity, wind speed 0.2–2.2 km/h).
At the conclusion of the 45 min soccer match, all subjects performed the Yo‐Yo Intermittent Recovery Test (YYIRT, level 2)15 as an indication of sport‐specific fitness across the three experimental conditions.
All subjects then completed a test of mental concentration to conclude the protocol.
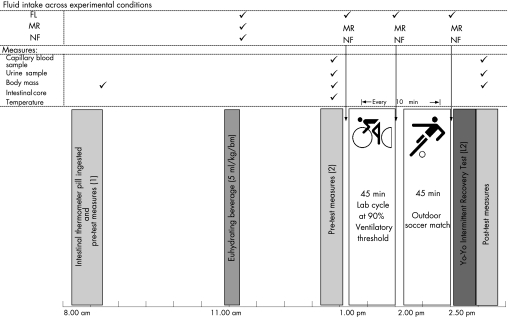
Figure 1 shows a schematic representation of the experimental protocol.
Figure 1 A schematic view of the experimental (soccer simulation) protocol. This schedule was replicated for each of the three experimental trials, with each subject following an individually randomised order of fluid intake (FL; mouth rinse (MR) and no fluid (NF)) across the trials.
Participants
Eleven moderately active male soccer players (mean (SD) age 24.4 (3) years, BM 74.03 (10.54) kg, height 1.75 (0.07) m, peak oxygen consumption 50.91 (3.95) ml/kg.min) volunteered to participate in the study, which was performed according to the Declaration of Helsinki and was approved by the Central Regional Ethics Committee of New Zealand. Two of the participants were unavailable for the MR condition, which, according to their individualised schedules, occurred on the final trial (week three). All subjects were requested to refrain from consuming alcohol and caffeinated products for 24 h before each experimental trial. The dietary and FL guidelines were provided for the subjects over 3‐day periods before each trial.
On each of the three dates of the experimental trials, subjects consumed morning breakfast, a mid‐morning snack and fluids at will. No food was consumed by the subjects between 2.5 h and the start of the experimental protocol. All subjects consumed a beverage of water 2 h before the start of the test (5 ml/kg·BM) to ensure comparable euhydration between subjects12 and thereafter followed their individual fluid intake condition.
Preliminary testing
Baseline cardiopulmonary fitness was assessed in all subjects before participation in the three exercise trials. All subjects completed an incremental test to volitional exhaustion (25 W/min) on a cycle ergometer (Monark 825E, Monark, Germany) for the assessment of peak oxygen uptake and ventilatory threshold. Cycle ergometry was used as the exercise modality in preference to treadmill running so as to facilitate the accurate, subsequent, identification of comparable work‐rate intensities for the first part of the experimental protocol. Gaseous exchange was measured at the mouth (True‐One Gas Analyser, Parvomedics, East Sandy, Utah, USA) and each individual's work rate corresponding to ventilatory threshold was identified following examination of carbon dioxide production/oxygen consumption parameters using the V slope method.16
Post‐match performance tests (soccer‐specific fitness and mental concentration)
Performance in the YYIRT has been shown to be positively associated with the amount of high‐intensity running performed during a competitive soccer game15 and distinguishes between soccer players of differing standards.17 The test comprises running coupled 20 m shuttles separated by a 10 s jog. Running speed during the test is incremental and dictated by audio signals. Maximal performance is adjudged to coincide with the inability to maintain the automated activity pattern and performance is measured according to the total distance covered (m).
The subjects also completed a mental concentration test.18 This test involved the identification of numbers ascending from 1 to 100 from a randomised grid. The subjects had to identify as many numbers as possible within 1 min and were given a different random grid in each of the three trials.
Water allocations across the three conditions
Individual water allocations were estimated on the basis that players would lose approximately 2% of BM over the protocol. Water was allocated according to 80% of estimated weight loss7 (2% estimated weight loss from baseline BM) and the total allocation was divided into three brief periods corresponding to drinking opportunities common in soccer match‐play: (1) 15 min before the start of the experimental trial (25% of total intake); (2) at half‐time—immediately following the 45 min cycle (50% of total intake); and (3) immediately following the conclusion of the 45 min match—before the YYIRT (25% of total intake). Fluid was ingested at room temperature for all trials (20–24°C).19
In the MR condition, subjects were given an individualised bottle at the same three points as in the FL condition. On each occasion, subjects were given a volume corresponding to 2 ml/kg BM of water and a separate spittle for the collection and subsequent measurement of the solution volume.
Tc and heart‐rate measurements
Tc was measured in the intestine using a silicon‐coated thermometer pill (CorTemp2000, HQ, Palmetto, Florida, USA) which was swallowed by all subjects 5 h before exercise so as to ensure that it would be past the stomach and insensible to swallowed hot or cold liquids.20 The calibration of the ingestible pills was checked at four different temperatures against a certified mercury thermometer in a water bath at temperatures ranging from 30°C to 42°C. In accordance with our earlier work, a linear regression of the relationship between the measured temperatures and those from the certified thermometer was used after the test to adjust pill measurements.1
Measurements were taken of Tc and heart rates throughout both the 45 min cycle and 45 min soccer match (30 s samples). Heart‐rate measurements were transmitted during games by the Polar heart rate chest belts (S610i, Polar, Kempele, Finland), time aligned and batched into 10 min intervals for the purposes of statistical comparisons.
A rating of perceived exertion (RPE) was recorded at the conclusion of each of the three experimental trials using the Borg Category Ratio Scale.21 This information was collected to rank the overall effort in response to the experimental protocol in each condition. Post‐protocol evaluation was conducted to rank perceived thirst for each trial among the subjects.
Blood and urine measures of hydration
Whole blood was sampled from the fingertip at rest before testing, and immediately following the conclusion of the YYIRT. In the pre‐test measure, the fingers of each subject were prewarmed and a small incision was made using a single‐use disposable lancet; 250 μl of whole blood was collected into an EDTA‐coated Eppendorf tube (Microtainer; Becton Dickinson, New Jersey, USA) for subsequent microcentrifugation. Immediately following this process, 100 μl of plasma was alloquated into two vessels for the duplicate assessment of Posm by the freezing point‐depression method (automatic cryoscopic osmometer, Gonotec Osmotat 030, Gonoter, Berlin, Germany).
Urine samples were obtained from all subjects before and after the test for subsequent analyses of osmolality and specific gravity. Urine osmolality (Uosm) was measured in duplicate using the same analysis procedure as for Posm. Urine specific gravity (Usg) was measured indirectly using the standard method of refractive index (WYA Abbe Refractometer, 2WA‐J, Shanghai Precision Scientific Instrument, Shanghai, China).
Sweat rate
Sweat rates over the experimental protocol were estimated from the following equation and subsequently transformed for expression as rate per hour:
Sweat rate (l/h) = (Pre‐BM (kg)+fluid ingested (l)−post‐BM (kg))/duration×60
This calculation does not take into account weight loss due to irreversible fuel oxidation and respiratory fluid loss, but it is unlikely that these would differ between conditions.
Heat storage
Each subject's heat storage for the laboratory exercise and soccer match was calculated using the following formula:
Hs = 0.965×BM×T/AD
where Hs is storage in J/m2, T the change in body temperature, BM the mean body mass over duration of the trial in kg, AD the body surface area in m2 and 0.965 = a heat capacity factor for the body in J/kg/° C.22
The value for heat storage was then divided by the duration of the trial to estimate heat storage as an hourly rate.
Body surface area (AD)
Body surface area (AD) was calculated using the following formula23:
AD = 0.202BM0.425×height0.725
where AD is the body surface area in m2, BM the mean body mass over the duration of the trial in kg and height the the subject's height in m.
Statistical analysis
Data are shown as mean (SD). A two‐way analysis of variance for repeated measures (trials×time) was used to establish whether any significant differences existed between the subjects' responses. When differences were noted, a post hoc Tukey's honestly significant difference test was used to determine where they lay. Statistical comparisons made with the MR condition were conducted using 9 datasets as 2 of the 11 subjects did not complete that condition. A natural logarithm was taken of urine osmolality measures to minimise the random effects of pre‐test to post‐test fluctuations observed in this measurement. Pearson's correlation coefficient was used to test for correlations.
Friedman's analysis of variance was used to compare the rank order of the RPE and thirst scores across the three conditions. The level of significance in this study was set at p<0.05.
Results
Laboratory‐exercise and soccer‐match measurements
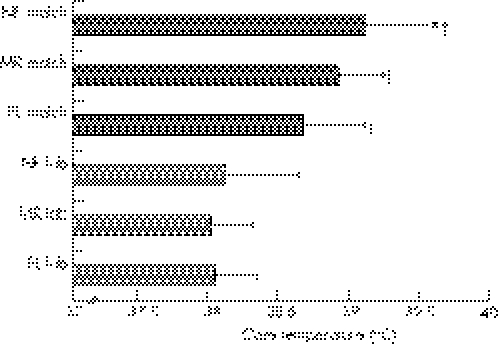
There was no difference in inter‐individual or intra‐individual Tc measurements across the three laboratory sessions demonstrating that, regardless of the condition, the physical challenge of 45 min cycling at 90% of ventilatory threshold was equally challenging on each test occasion. The mean Tc was significantly increased in the NF condition in the soccer match when compared with FL (p<0.05), but there were no differences in Tc in comparisons with MR (fig 2).
Figure 2 Mean core temperature measurements from the laboratory (lab) ‐exercise and soccer‐match (match) activities across the three conditions: fluid intake (FL), mouth rinse (MR) and no fluid (NF). *Significant difference between NF and FL (p<0.05). †Significant difference between laboratory exercise and soccer match (p<0.01).
Averaged heart‐rate measurements for the laboratory exercise were significantly lower than for the soccer matches (p<0.01), and although there was a tendency for higher heart rates in the soccer match while subjects were in the NF condition, this observation was not of statistical significance (table 1).
Table 1 Averaged heart rate measurements across the three conditions in both the 45 min laboratory exercise and 45 min soccer match.
| Fluid intake (n = 11) | Mouth rinse (n = 9) | No fluid (n = 11) | |
|---|---|---|---|
| Laboratory exercise | 136.2 (16.7) | 139.1 (18.4) | 138.3 (18.7) |
| Soccer match | 157.6 (10.2) | 159.2 (11.5) | 159.5 (10.2) |
Values are mean (SD).
Rank order evaluations of RPE taken at the conclusion of each experimental condition were significantly higher in the NF condition than in FL (NF: 16.6 (1.3), FL: 15 (1.1), p<0.05), but not in MR (16 (1.1)). Rank order evaluation demonstrated that thirst was perceived to be greatest in the NF condition (p<0.01).
Blood and urine analysis
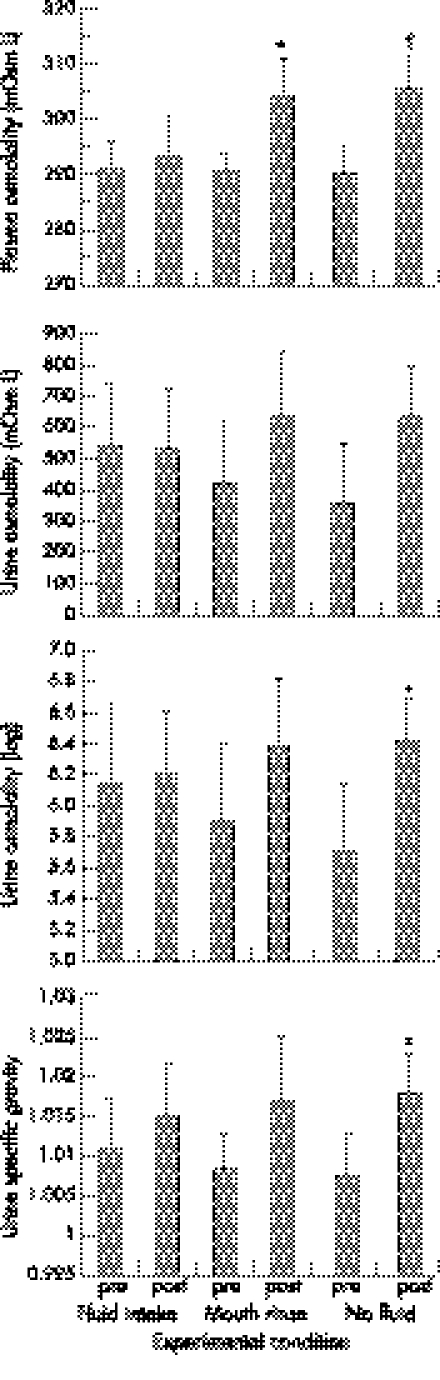
Posm increased from pre‐exercise to post‐exercise in both MR (p<0.05) and NF (p<0.01) conditions. The increase in Posm from pre‐exercise to post‐exercise in the FL condition was not of statistical significance (fig 3).
Figure 3 Pre‐protocol and post‐protocol measurements of plasma osmolality, urine osmolality and specific gravity in response to the experimental conditions (fluid intake, mouth rinse and no fluid). *Significant difference from pre‐protocol to post‐protocol (p<0.05). †Significant difference from pre‐protocol to post‐protocol (p<0.01).
In the urinary measures, Usg increased significantly from pre‐test to post‐test in the NF condition (p<0.05), but there was no significant change in either MR or FL. Pre‐test to post‐test Uosm in the NF condition approached significance (p = 0.062) and was subsequently log transformed to ascertain whether the observed wide pre‐test to post‐test fluctuations may have disguised an underlying effect in this measure. This process identified a significant pre‐exercise to post‐exercise increase in the NF condition (p<0.05), with no significant change in FL or MR conditions (fig 3).
Pre‐test and post‐test changes in BM, heat storage and sweat rates
Post‐match BM was significantly reduced in each of the three conditions. This was statistically of greatest significance in the NF (p<0.01) and MR (p<0.01) conditions and least in the FL condition (p<0.05; table 2). There were no differences in sweat rates or heat storage across the three conditions (table 2).
Table 2 Pre‐test and post‐test body masses, heat storage, body and sweat loss in the three conditions.
| Fluid intake (n = 11) | Mouth rinse (n = 9) | No fluid (n = 11) | |
|---|---|---|---|
| Pre‐BM (kg) | 73.86 (10.6) | 72.50 (11.2) | 74.09 (10.7) |
| Post‐BM (kg) | 73.33 (10.6)* | 70.96 (11.0)† | 72.30 (10.5)† |
| BM loss (%) | 0.73 (0.4)* | 2.14 (0.6)†‡ | 2.4 (0.8)†‡ |
| Sweat rate (l/h) | 0.83 (0.3) | 0.78 (0.2) | 0.90 (0.3) |
| Hs1 (J/m2/h) | 14.49 (7.6) | 13.05 (5.3) | 14.83 (6.5) |
| Hs2 (J/m2/h) | 32.33 (11.5)§ | 31.02 (6.4)§ | 36.28 (6.1)§ |
BM, body mass; Hs1, heat storage from the 45 min laboratory exercise; Hs2, heat storage from the 45 min soccer match.
Values are mean (SD).
*Significant difference pre‐test to post‐test (p<0.05).
†Significant difference pre‐test to post‐test (p<0.01).
‡Significant difference in comparison to the fluid condition (p<0.01).
§Significant difference between laboratory exercise and soccer match (p<0.01).
Immediate post‐match performance tests
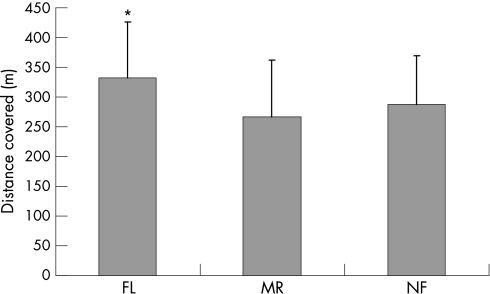
The immediate post‐match performance of the YYIRT identified that the greatest distance covered was accomplished in the FL condition in comparison to both MR (15% mean decrement in distance covered compared with FL) and NF (13% mean decrement in distance covered compared with FL) conditions (p<0.01). There was no significant difference between the subjects' YYIRT performance for MR or NF conditions (fig 4).
Figure 4 Yo‐Yo Intermittent Recovery Test (level 2) performances in the three experimental conditions: fluid intake (FL), mouth rinse (MR) and no fluid (NF). Each of the three tests was performed at the conclusion of 90 min protocol (45 min cycle and 45 min soccer match). *Significant difference (p<0.01).
There were no significant differences between performances across the three conditions in the mental concentration test (FL 17.81 (5.31), MR 19.22 (7.45) and NF 16.27 (5.48) words/min).
Discussion
The main finding of the present study was that the immediate post‐match performance of a sport‐specific fitness test (YYIRT) was significantly impaired in both experimental conditions (MR and NF) where fluid ingestion had been denied (p<0.01). This resulted in 13–15% decrements in total distance covered when compared with the FL condition and shows that acute, moderate water loss corresponding to ∼2% of BM is detrimental to the physiological performance of the soccer performance variables in this study.
The significant post‐test losses in BM for both MR and NF conditions (2.14% and 2.4%, respectively; p<0.01) satisfied the experimental aims of examining the physiological responses to match and post‐match variables in conditions of dehydration similar to competitive match performance.1,2,9 Interestingly, the FL condition in this study (80% of pre‐estimated fluid loss replaced at time points replicating match‐play opportunities for rehydration) was sufficient to maintain BM (0.7% loss of BM) and Posm (no significant change) relatively well, thus restricting exercise‐induced water loss in that condition. This suggests that similar fluid intake strategies during match‐play are probably adequate to minimise negative outcomes of dehydration in thermoneutral outdoor conditions. However, it should be noted that this volume of fluid was well in excess to that of players' usual practice and was at the limit of tolerance.
The greatest pre‐protocol to post‐protocol change in Posm occurred in the NF condition, which was also the condition where the greatest weight loss was observed (2.4% loss in BM in that condition). As Posm represents a homeostatically defended variable, alterations in BM through greater water retention would be initiated more vigorously in the NF condition to return temporal changes in Posm to normal parameters.13
Posm better tracked changes in BM across the three conditions than either of the urine measures in this study, which supports earlier observations.10,13 Fluctuations from pre‐test to post‐test urine measures were most prevalent in the FL condition when both Uosm and Usg fell in several of the subjects. The most likely explanation for this is that, in the FL condition, the kidney would still filter excess fluid ingested throughout the duration of the protocol. As a consequence, the measures of renal function may have been temporarily disassociated with the controlled variable (in this case, extracellular fluid osmolality as measured by Posm) while functioning to correct an alteration in fluid balance.
Tc values and heart rates from the 45 min pre‐match period of standardised cycle ergometry were similar between the three trials (week to week) and between the three experimental conditions. This suggests that the subjects worked equally hard in each of the laboratory sessions, and thus this element proved an adequate means of ensuring that all participants began the 45 min soccer match in a similar physical condition, all having worked at a standardised level of intensity so that subsequent inter‐individual and intra‐individual differences in match‐play activities could not be attributable to alterations in pre‐match glycogen storage, between either subjects or experimental conditions.
The only intervention‐specific difference observed during the match‐play element was an increased mean Tc in the NF condition (p<0.05). The mean Tcs and heart rates reported from the soccer match in this study were similar to those reported previously from the second 45 min period of competitive matches,1,2 which indicates that the soccer match intensities in each trial were sufficiently challenging.
Although moderate dehydration has been shown to negatively affect the physiological performance indicators in this study, the cause of this observation has not been established. It is possible that the findings could be attributable to either a cardiovascular limitation, or perhaps negative psychological factors subconsciously affecting perceived effort while being denied fluids.
What is already known on this topic
Earlier laboratory‐based studies of physiological performance have tended to suggest that moderate water loss is detrimental to sports performance through impaired sweat responses and a reduced plasma volume.
In self‐paced activities such as outdoor soccer match‐play, moderate water losses and core temperatures are unlikely to reach critical levels, questioning whether earlier conclusions are applicable to soccer.
What this study adds
Moderate water loss was detrimental to several physiological parameters derived from the outdoor match‐play element of this study.
However, it is equivocal whether water loss in itself was the cause of reduced performances, as these may be due to either physiological aspects mediating thermal strain or negative psychological factors surrounding a greater perception of effort while dehydrated.
The increased thermal strain of completing the test in the NF condition did promote a greater loss of BM and this may have increased fluid loss to a level that impaired soccer performance. For example, the significant increase in post‐test Posm in the NF condition suggests that the composition of circulating blood contained inadequate water. Reductions in blood plasma over the course of the protocol could have led to a reduction in the blood supply to both exercising muscles and the skin, thus reducing oxygen transport to the working muscles and also diminishing the ability to dissipate heat as body water deficit increased.24 However, sweat rates that accounted for fluid loss were not different between trials. Previous studies7,10 have demonstrated similar sweat rates across experimental conditions where subjects experienced weight loss in excess of this study and generally concurred that fatigue was associated with the inability of the environment to facilitate effective heat dissipation.7,10,22 As the soccer match in this study was performed outdoors and the wind velocity remained low, but fairly consistent (0.2–2.2 km/h), it is unlikely that the environment proved a differential limitation to performance.
An alternative explanation for the observed findings could be attributable to a psychological rather than a physiological limitation identified from the increased RPE in the NF condition (p<0.05). Despite the mean Tc in the NF condition (39.28°C (0.35°C)) being significantly increased in comparison with the FL condition (38.8°C (0.47)°C; p<0.05), this was still below a level considered critical at the point of fatigue during prolonged exercise (∼40–40.5°C).25,26 It is plausible that while RPEs and rank order evaluations of thirst demonstrated that the subjects perceived the NF condition to be the most challenging, the relatively small but significant increases in Posm and Tc in the NF condition may have stimulated intrinsic anticipatory mechanisms in the brain which recognised that heat storage was occurring rapidly and invoked performance limitations to avoid future physical damage.27 Therefore, the combination of an increased fluid loss and increased Posm might not be representative of a physiological requirement for water in itself, but rather, a greater perceived discomfort in an unfamiliar condition and the subconscious desire to complete the protocol in a reasonable state of hydration.
One aim of this study was to examine whether the inclusion of a MR condition might be a sufficient temporary stimulus to either reduce or possibly remove negative psychological feelings associated with dry mouth. The findings of this study did not support the use of a MR condition for this purpose at the match‐play opportunities used here. The mean Tc during match‐play was, to some extent, suppressed in the MR condition in comparison with NF, which could be interpreted as a beneficial temporary adaptation, but post‐match performances of the YYIRT were similar to the NF condition and do not support this contention. The timing of MR availability was designed to represent typical opportunities for rehydrating in soccer match‐play conditions and although this schedule may have been ecologically valid to the game, it was probably insufficiently frequent to remove the psychological drive to drink in that condition.
The post‐test evaluation of mental concentration did not demonstrate any difference across the three conditions. This indicates that decision making in soccer is unaffected by moderate dehydration, and this would be consistent with recent observations made from the performance of choice reaction time at different levels of hydration and heat stress.28
Conclusions
In conclusion, the denial of water was detrimental to the immediate post‐match performance of the validated YYIRT after 90 min of exercise. The subjects perceived the NF trial as the experimental condition where most effort was required, and it seems clear that the denial of water was detrimental to the performance variables in this study. However, it is equivocal whether this is due to physiological aspects mediating thermal strain or to negative psychological factors surrounding the greater perception of effort while dehydrated. Further work is required to examine whether water loss in itself is detrimental to performance.
Acknowledgements
We thank Rakai Timutimu, Pamela Gatchell and Andre Van der Walt for their enthusiasm and technical support during this project.
Abbreviations
BM - body mass
FL - fluid intake
MR - mouth rinse
NF - no fluid
Posm - plasma osmolality
RPE - rating of perceived exertion
Tc - core temperature
Uosm - urine osmolality
Usg - urine specific gravity
YYIRT - Yo‐Yo Intermittent Recovery Test
Footnotes
Competing interests: None declared.
References
- 1.Edwards A M, Clark N. Thermoregulatory observations in soccer match‐play: professional and recreational level applications using an intestinal pill system to measure core temperature. Br J Sports Med 200640133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohr M, Krustrup P, Nybo L.et al Muscle temperature and sprint performance during soccer matches—beneficial effect of re‐warm‐up at half‐time. Scand J Med Sci Sports 200414156–162. [DOI] [PubMed] [Google Scholar]
- 3.McGregor S J, Nicholas C W, Lakomy H K.et al The influence of intermittent high intensity shuttle running and fluid ingestion on the performances of a soccer skill. J Sports Sci 199917895–903. [DOI] [PubMed] [Google Scholar]
- 4.Nicholas C W, Lakomy H K, Phillips A.et al Influence of ingesting a carbohydrate‐electrolyte solution on endurance capacity during intermittent, high‐intensity shuttle running. J Sports Sci 199513283–290. [DOI] [PubMed] [Google Scholar]
- 5.Maughan R J, Merson S J, Broad N.et al Fluid and electrolyte intake and losses in elite soccer players during training. Int J Sport Nutr Exerc Metab 2004333–346. [DOI] [PubMed]
- 6.Leiper J B, Prentice A S, Wrightson C.et al Gastric emptying of a carbohydrate‐electrolyte drink during a soccer match. Med Sci Sports Exerc 2001331932–1938. [DOI] [PubMed] [Google Scholar]
- 7.Saunders A G, Dugas J P, Tucker R.et al The effects of different air velocities on heat storage and body temperature in humans cycling in a hot, humid environment. Acta Physiol Scand 2005183241–255. [DOI] [PubMed] [Google Scholar]
- 8.Mustafa K Y, Mahmoud N E. Evaporative water loss in African soccer players. J Sports Med Phys Fitness 197919181–183. [PubMed] [Google Scholar]
- 9.Da Silva A L, Fernandez R. Dehydration of football referees during a match. Br J Sports Med 200337502–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong L E, Maresh C M. Effects of training, environment and host factors on the sweating response to exercise. Int J Sports Med 199819S103–S105. [DOI] [PubMed] [Google Scholar]
- 11.Noakes T, Rehrer N, Maughan R. The importance of volume in regulating gastric emptying. Med Sci Sports Ex 199123307–313. [PubMed] [Google Scholar]
- 12.Montain S J, Coyle E F. Influence of graded dehydration on cardiovascular drift and hyperthermia during exercise. J Appl Physiol 1992731340–1350. [DOI] [PubMed] [Google Scholar]
- 13.Popowski L A, Oppliger R A, Lambert G P.et al Blood and urinary measures of hydration status during progressive acute dehydration. Med Sci Sports Exerc 200133747–753. [DOI] [PubMed] [Google Scholar]
- 14.Katz D B, Nicolelis M A L, Simon S A. Nutrient tasting and signalling mechanisms in the gut. IV. There is more to taste than meets the tongue. Am J Physiol Gastrointest Liver Physiol 2000278G6–G9. [DOI] [PubMed] [Google Scholar]
- 15.Krustrup P, Mohr M, Amstrup T.et al The Yo‐Yo Intermittent Recovery Test: physiological response, reliability, and validity. Med Sci Sports Exerc 200335697–705. [DOI] [PubMed] [Google Scholar]
- 16.Beaver W L, Wasserman K, Whipp B J. A new method for detecting the anaerobic threshold by gas exchange. J Appl Physiol 1986602020–2027. [DOI] [PubMed] [Google Scholar]
- 17.Mohr M, Krustrup P, Bangsbo J. Match performances of high‐standard soccer players with special reference to the development of fatigue. J Sports Sci 200321519–528. [DOI] [PubMed] [Google Scholar]
- 18.Hardy L, Jones G, Gould D.Concentration and attention control. Understanding psychological preparation for sport: theory and practice of elite performers. Chichester, UK: Wiley, 1996141–168.
- 19.Wimer G S, Lamb D R, Sherman W M.et al Temperature of ingested water and thermoregulation during moderate‐intensity exercise. Can J Appl Physiol 199722479–493. [DOI] [PubMed] [Google Scholar]
- 20.Sparling P B, Snow T K, Millard‐Stafford M L. Monitoring core temperature during exercise: ingestible sensor vs. rectal thermistor. Aviat Space Environ Med 199364760–763. [PubMed] [Google Scholar]
- 21.Borg G A. Psychological bases of perceived exertion. Med Sci Sports Exerc 198214377–381. [PubMed] [Google Scholar]
- 22.Adams W C, Mack G W, Langhans G H.et al Effects of varied air velocity on sweating and evaporative rate during exercise. J Appl Physiol 1992732668–2674. [DOI] [PubMed] [Google Scholar]
- 23.Du Bois D B S, Du Bois E F. A formula to estimate the approximate body surface area if height and weight be known. Arch Int Med 191617963–971. [Google Scholar]
- 24.Nadel E R, Fortney S M, Wenger C B. Effect of hydration state on circulatory and thermal regulation. J Appl Physiol 198049715–721. [DOI] [PubMed] [Google Scholar]
- 25.Byrne C, Lee J K W, Chew S A N.et al Continuous thermoregulatory responses to mass‐participation distance running in heat. Med Sci Sports Exerc 200638803–810. [DOI] [PubMed] [Google Scholar]
- 26.González‐Alonso J, Teller C, Andersen S L.et al Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol 1999861032–1039. [DOI] [PubMed] [Google Scholar]
- 27.St Clair Gibson A, Noakes T D. Evidence for complex system integration and dynamic neural regulation of skeletal muscle recruitment during exercise in humans. Br J Sports Med 200438797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serwah N, Marino F E. The combined effects of hydration and exercise heat stress on choice reaction time. J Sci Med Sport 20069157–164. [DOI] [PubMed] [Google Scholar]