Abstract
Background
Eccentric overload training seems to be a promising conservative intervention in patients with chronic Achilles tendinopathy. The efficacy of eccentric overload training on the outcome measures of pain and physical functioning are not exactly clear.
Study design
Systematic review of the literature.
Methods
Electronic databases were searched for randomised clinical trials concerning eccentric overload training in patients with chronic Achilles tendinopathy. The Delphi list was used to assess the methodological quality of the studies.
Results
Nine clinical trials were included. Only one study had sufficient methodological quality. The included trials showed an improvement in pain after eccentric overload training. Because of the methodological shortcomings of the trials, no definite conclusion can be drawn concerning the effects of eccentric overload training in patients with chronic Achilles tendinopathy.
Conclusion
The effects of eccentric exercise training in patients with chronic Achilles tendinopathy on pain are promising; however, the magnitude of the effects cannot be determined. Large, methodologically sound studies from multiple sites in which functional outcome measures are included are warranted.
Achilles tendinopathy is a frequent disorder among recreationally active people and among recreational and professional athletes. Achilles tendinopathy occurs in men and women of all age categories, but especially in men of middle age (35–45 years).1,2,3,4 The prevalence of the disorder is higher in sports that involve running or jumping.2,5,6,7,8,9 About 7%–9% of professional athletes participating in these sports are confronted with this disorder and in 6%–18% of all injuries in recreational runners the Achilles tendon is involved.1,10,11,12 Remarkably, in recent studies it was shown that 33% of patients with chronic Achilles tendinopathy are not physically active, and that physical activity does not correlate with histopathological findings of the Achilles tendon.5,13,14,15 Physical load on the Achilles tendon should be more seriously considered as a factor that provokes the disorder and not as an aetiological factor.6,13,14,15
There is no clear, widely accepted definition or test for the diagnosis of chronic Achilles tendinopathy. Many predisposing factors have been reported, but the exact aetiology of Achilles tendinopathy is unknown. Patients have a slowly developing pain in the Achilles tendon, initially only during Achilles tendon loading activities but later also during rest. Achilles tendinopathy causes many patients to significantly reduce their physical activity level or to quit their sporting activities completely, with a potentially negative effect on their overall health and general wellbeing.1,2,4,5,6,14,15,16 Typical for chronic Achilles tendinopathy is pain at the initiation of exercise and stiffness.2,17 The degree of pain and stiffness is a good indicator of severity of the tendinopathy.2
Physical therapeutic interventions for the treatment of patients with chronic Achilles tendinopathy are mostly conservative.1 Treatments include therapeutic applications, such as ultrasound and deep transverse friction, and remedial treatment, such as strengthening and flexibility exercises. Currently, eccentric overload training is much used and seems to be promising. The eccentric overload training model that is used in most studies was described by Alfredson et al.18 This model consists of two types of eccentric exercises, done under the guidance of a physical therapist: (1) with the knee straight, to maximise the activation of the gastrocnemius muscle, and (2) with the knee bent, to maximise the activation of the soleus muscle.
It is not exactly clear why eccentric overload training results in a direct histological effect on the injured tendon resulting in a reduction in stiffness and better functioning of the patient.3 The question for this systematic review was: what is the effectiveness of eccentric overload training in patients with chronic Achilles tendinopathy?
Methods
To examine the effectiveness of eccentric overload training in patients with chronic Achilles tendinopathy, a systematic literature search was performed.
Strategy for literature search
Two researchers independently searched the electronic databases of CINAHL, PubMed, Medline, Cochrane Library, EMBASE, PEDro and Google Scholar from 1966 to December 2005. The following keywords were used in various compositions: Achilles tendon, tendinopathy, tendinosis, tendonitis, physical therapy, exercise, eccentric training, eccentric overload, treatment, calf muscle, pain, stiffness and physical function.
Method of selecting studies found by the literature search
Two independent reviewers carried out the selection of studies in two consecutive screening phases. In the initial screening phase, selection criteria were applied only to the titles and abstracts of the articles. In case of lack of clarity, the studies were advanced to the second screening phase, in which the selection criteria were applied to the full‐text articles.
Studies were included if they met the following five selection criteria:
The study population consisted of men and/or women with a diagnosis of chronic Achilles tendinopathy.
The study was a randomised clinical or clinical controlled trial.
The intervention was contained in the professional domain of the general‐practice physical therapist and included at least eccentric overload training.
The study used at least one patient‐oriented outcome measure such as pain, stiffness or physical functioning.
The study had to be in Dutch or English and must have been published as a full‐text article in a peer‐reviewed journal. Abstracts and congress reports were not included.
Evaluation of methodological quality
The Delphi list for quality assessment of randomised clinical trials19,20 was used to evaluate the methodological quality of the individual studies. This is a list of criteria that measures the three dimensions of quality: internal validity, external validity and statistical considerations.19,21 It can be used to report the methodological quality per dimension or as a total score.19,22 The Delphi list consists of nine items, all given the same weights; hence it yields a non‐weighted score. The total score for methodological quality consists of the number of items that are evaluated as satisfactory (yes) and are scored 1. The list therefore has a range of 0–9 points.
Two reviewers independently evaluated the methodological quality of the studies. Their scores were compared, to detect any differences in scoring. These differences were discussed by the reviewers during a consensus meeting to identify why they had arisen. A consensus on how to score the specific items was reached by discussion. Those studies in which initially there were differences in scoring between the two reviewers were jointly rescored together by the reviewers, resulting in an overall score for methodological quality. The studies that received an overall score of ⩾5 were considered to be of high quality.19
Evaluation of conclusive power of the studies' conclusions
The studies' conclusions were evaluated for conclusive power according to the classification system of the Dutch Institute for Healthcare Improvement (table 1).
Table 1 Classification of the substantiation in level and degree of evidence in the conclusions of the studies.
| For articles concerning: intervention (prevention or therapy) | |
| A1 | Systematic reviews that include at least some studies of level A2, in which the results of the separate studies are consistent |
| A2 | Randomised controlled clinical trial of good‐quality, random, double‐blind controlled trials, of sufficient size and consistency |
| B | Randomised clinical trials of moderate quality or insufficient size or other comparative studies (not‐randomised, comparative cohort study, patient–control study) |
| C | Non‐comparative studies |
| D | Opinion of experts |
| Degree of evidence of the conclusions | |
| 1 | One systematic review (A1, or at least two independently conducted studies of degree of A1 or A2) |
| 2 | At least two independently conducted studies of degree B |
| 3 | One study of degree A2 or B or one or more studies of degree C |
| 4 | Opinion of experts |
1, strong evidence; 2, moderate evidence; 3, poor or conflicting evidence; 4, no evidence.
Source: Dutch Institute for Healthcare Improvement.23
On the basis of methodological quality, every study was assigned a certain status (A1, A2, B, C, D). Thereafter, it was evaluated how much conclusive power could be awarded to the physical therapy. This was done according to the number of studies that described the physical‐therapy interventions and by means of the status of the study. This procedure gave us a level of conclusive power.
Two reviewers independently performed the evaluation of conclusive power. The researchers reached definite scores during a consensus meeting, resulting in an overall score for the conclusive power of each individual study.
Results
Literature search strategy
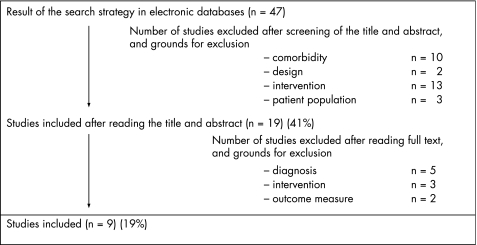
We identified 47 primary studies for possible inclusion in our study; 28 (59%) were excluded on the basis of the title and the abstracts (because of comorbidity such as tendon rupture, study designs such as case descriptions, medical interventions and study population such as status after surgery). The remaining 19 (41%) studies were included for the second phase of the screening procedure, in which 10 (21%) studies were excluded on the basis of diagnosis (n = 5), intervention (n = 3) or outcome measures (n = 2) after evaluation of the full text (fig 1).
Methodological quality
Only moderate agreement for the overall scores of methodological quality (κ = 0.521) was found preceding the consensus meeting between the two independent reviewers, because of their different interpretations of item 1A and a lack of information in item 3. During the consensus meeting the reviewers decided to use the interpretation of item 1A by Verhagen et al,19,20 namely, that a point can be awarded to item 1A when the article provides a detailed description of the randomisation procedure, but not if it only mentions that a randomisation procedure was performed.19,20
Table 2 shows the scores for methodological quality of the included studies. The overall Delphi scores ranged from 0 to 9 points (mean 2.8). Only one (11%) study was considered to be of sufficient quality (score = 6); the remaining eight (89%) were of insufficient methodological quality. In five (56%) the population samples had comparable baseline measures. In six (67%), the point estimates and the measures of variability were described in the article and were evaluated as sufficient.
Table 2 Scoring of the included studies for methodological quality according to the Delphi list.
| Study | Items* | Level of evidence | Degree of evidence | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1A | 1B | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Score | |||
| Roos et al (2004)23 | + | + | + | + | – | – | – | + | + | 6/9 | B | 2 |
| Mafi et al (2001)24 | + | + | + | + | – | – | – | – | – | 4/9 | B | 2 |
| Niesen‐Vertommen et al (1992)25 | – | – | + | + | + | – | – | – | – | 3/9 | C | 2 |
| Silbernagel et al (2001)4 | – | – | + | + | + | – | – | + | – | 4/9 | B | 2 |
| Alfredson et al (1998)18 | – | – | + | + | – | – | – | + | – | 3/9 | B | 2 |
| Fahlström et al (2003)26 | – | – | – | + | – | – | – | + | – | 2/9 | B | 2 |
| Shalabi et al (2004)27 | – | – | – | + | – | – | – | + | – | 2/9 | C | 2 |
| Alfredson et al (2003)28 | – | – | – | – | – | – | – | + | – | 1/9 | C | 3 |
| Stanish et al (1986)29 | – | – | – | – | – | – | – | – | 0/9 | C | 3 | |
For a description of the degree and the level of evidence, see table 1. +, answer to question is yes; –, answer to question is no.
*1A, was a method of random performed for the treatment allocation?; 1B, was the treatment allocation concealed?; 2, were the groups similar at baseline regarding the most prognostic indicators?; 3, were the eligibility criteria specified?; 4, was the outcome assessor blinded?; 5, was the care provider blinded?; 6, was the patient blinded?; 7, were point estimates and measures of variability presented for the primary outcome measures?; 8, did the analysis include an intention‐to‐treat analysis?
In only two (22%) of the studies was a detailed description given of the randomisation procedure and the method of concealment of the treatment allocation. Two (22%) studies were given points for the items of blinding with regard to the assessor. None were given points for the items of blinding with regard to the care provider.
Conclusive power of the studies' conclusions
Moderate agreement regarding the conclusive power of the studies' conclusions (level of evidence κ = 0.550; degree of evidence κ = 0.609) was found preceding the consensus meeting between the two independent reviewers.
Table 2 shows the evaluation of the conclusive power of the conclusions of the studies included as a result of the consensus meeting. In all, five (56%) of the studies represent level B evidence—that is, they were based on randomised clinical trials of moderate methodological quality or insufficient size or on other comparative studies. In four (44%) of the studies, the conclusions were substantiated on non‐comparative studies (level C). The substantiation of the studies included can therefore be considered insufficient.
Accordingly, the conclusive power of the degree of evidence of the conclusions of these studies was low. In 78% (n = 7) of the studies the degree of evidence of the conclusions is on level 2 and, in the remaining two (22%) it is on level 3.
Effect of eccentric overload training
Nine studies (100%)—three randomised control trials4,23,24 and six controlled trials18,25,26,27,28,29—investigated the effect of eccentric overload training in patients with chronic Achilles tendinopathy (table 3). All the studies used a prospective design and included only patients diagnosed with Achilles tendinopathy, whose mean duration of symptoms was between 3.6 and 22 months.
Table 3 Effectiveness of eccentric overload training in patients with chronic Achilles tendinopathy according to the studies included.
| Authors | Participants (n) | Method | Inclusion criteria | Intervention | Outcome measure | Duration of intervention | Result in intervention group | Result in control group |
|---|---|---|---|---|---|---|---|---|
| Roos et al (2004)23 | 44 | RCT | Chronic Achilles tendinopathy | I: Eccentric training | FAOS | 12 weeks | ↓ 37% | C1: ↓ 23% |
| C1: Eccentric training with night splint | C2: ↓ 13% | |||||||
| C2: Night splint | ||||||||
| Mafi et al (2001)24 | 44 | RCT | Chronic Achilles tendinopathy | I: Eccentric training | VAS | 12 weeks | ↓ 83% | ↓ 86% |
| C: Concentric training | ||||||||
| Niesen‐Vertommen et al (1992)25 | 17 | RCT | Chronic Achilles tendinopathy | I: Eccentric training | Ordinal Scale | 12 weeks | ↓ 78% | ↓ 46% |
| C: Concentric training | ||||||||
| Silbernagel et al (2001)4 | 40 | RCT | Chronic Achilles tendinopathy | I: Eccentric training | VAS | 12 weeks | ↓ 29% | ↓ 15% |
| C: Concentric training | ||||||||
| Alfredson et al (1998)18 | 30 | CT | Chronic Achilles tendinopathy | I: Eccentric training | VAS | 12 weeks | ↓ 94% | ↓ 70% |
| C: Surgery | ||||||||
| Fahlström et al (2003)26 | 78 | CT | Chronic Achilles tendinopathy. (A) Mid‐portion of the Achilles tendon and (B) insertion of the Achilles tendon | I: Eccentric training | VAS | 12 weeks | A: ↓ 85% | |
| B: ↓ 81% | ||||||||
| Shalabi et al (2004)27 | 25 | CT | Chronic Achilles tendinopathy | I: Eccentric training | Ordinal Scale | 12 weeks | ↓ 40% | |
| Alfredson et al (2003)28 | 6 | CT | Chronic Achilles tendinopathy | I: Eccentric training | VAS | 12 weeks | ↓ 75% | |
| Stanish et al (1986)29 | 200 | CT | Chronic Achilles tendinopathy | I: Eccentric training | Ordinal Scale | 6 weeks | ↓ 87% |
C, control group; CT, clinical trial; I, intervention group; FAOS, Foot and Ankle Outcome Score; RCT, randomised clinical trial; VAS, visual analogue scale; ↓, improvement in pain score.
Six (66%) studies18,23,24,26,27,28 used the eccentric‐overload‐training model as described by Alfredson et al.18 Three (33%) studies4,25,29 used a training model containing eccentric exercises and such cointerventions as stretching and application of ice. The durations of the eccentric overload training were 630 or 12 weeks.4,18,23,24,25,26,27,28 Eccentric overload training was compared with concentric training in three (33%) studies,4,24,25 with surgery in one (11%)18 and with a night splint or combined with a night splint in one (11%).23 4 (44%) studies did not include a control group.26,27,28,29
Figure 1 Flow chart of the search strategy.
Pain was the primary outcome measure in eight (89%) studies.4,18,23,24,25,26,28,29 Six (66%) used a visual analogue scale,4,18,24,26,28,29 pain during Achilles tendon loading activities was measured in five (55%) studies,4,18,23,24,26,28 pain on palpation in one (11%) study4 and pain in general was also measured in one (11%).29 Two (22%) studies used an ordinal scale25,29 and one (11%) used the Foot and Ankle Outcome Score23 to measure pain.
All the studies reported a reduction in pain for both the eccentric overload training group and the control group. Because of the great heterogeneity of the study populations and of the interventions and outcome measures, no statistical pooling of the results of the studies could be performed.
For all nine included studies, the mean reduction in pain for the eccentric overload training group was 60% (CI 29% to 94%); for the control group it was 33% (CI 13% to 86%). All studies using a control group reported greater reductions in pain for the eccentric overload training group than for the control group, except the study of Mafi et al,24 in which the control group showed a greater reduction in pain.
The mean number of participants in the included studies was 53.7 (SD 58.4) with a range of 6–200. For the evaluation of significant outcome differences, the included studies were relatively underpowered with regard to participants.
Discussion
Our purpose was to systematically review the efficacy of eccentric overload training in patients with chronic Achilles tendinopathy as regards the outcome measures of pain and function. A total of nine studies were included in the review, of which only one received a satisfactory score for methodological quality. Statistical pooling of results was not possible for the outcome measures of pain and function, due to the heterogeneity in patients and interventions; most of the studies did not evaluate function and/or sporting activities. Although the effects of eccentric exercise training on pain in chronic Achilles tendinopathy are promising, the magnitude of the effects cannot be determined. Moreover, recent observations have raised a question as to whether eccentric exercise training is as effective in non‐athletic patients as has been reported for athletes.31
It is remarkable that during the scoring of the methodological quality assessment, none of the studies received points for the items about blinding of the care provider and blinding of the patient. A possible explanation is that these types of blinding are often not feasible in physical therapy research. The domain of physical therapy is situated in human functioning and participation in a social environment. Controlled studies in this domain, therefore, should use outcome measures and interventions that are adapted to activities and participation. Outcome measures and interventions that are adapted to activities and participation are expressed in the use of performance tests and the comparison of physically strenuous interventions. Owing to these physical components, it is often not feasible to keep the care providers and the patients blinded. However, scoring lists for assessing methodological quality in physical therapy research still include these items on blinding.32
The descriptions of the eccentric overload training models and the control interventions lack sufficient information for reproducibility in the clinic. The number of repetitions and series is described concisely in most studies, but the speed of movement and possible interventions preceding the actual eccentric overload training were not described.
All the included studies have used a training model containing eccentric overload training as well as cointerventions, such as stretching and ice applications, and most of the research projects involved the originators of the technique. In all these studies, the effect of eccentric overload training on reduction of pain intensity could be contaminated by the cointerventions.4,25,29 To evaluate the actual effect of eccentric overload training in patients with chronic Achilles tendinopathy, it is imperative that eccentric overload training is evaluated as a single intervention and not as a part of a training model containing confounding cointerventions. Moreover, studies performed in other centres are desirable.
One shortcoming of this review is a possible selection bias. We selected only full‐text, peer‐reviewed papers published in English and Dutch, which might have resulted in a language bias.33 The inclusion of only full‐text, peer‐reviewed papers secures a certain quality for the included studies; however, it could result in a publication bias, since trials with no effect have a larger chance of not being published.34
Recommendations for future research
Pain intensity was used as a primary outcome measure in all included studies. In physical therapy, this outcome measure is too limited by itself to evaluate the effect of eccentric overload training in patients with chronic Achilles tendinopathy. It would be more clinically relevant to use outcome measures focusing on the function of the Achilles tendon and patients' activities, as well as patients' (sporting) participation.
For the evaluation of outcome of the intervention, generic outcome measures were used in the studies. Disease‐specific measures, such as the Victorian Institute of Sport Assessment‐Achilles (VISA‐A) Questionnaire35 are probably more sensitive to small clinical changes occurring over short periods, can discriminate between different health levels in the most severely affected patients and contain questions that are more familiar and comprehensible to patients and more relevant to clinicians.30,36 The VISA‐A Questionnaire is an index of the clinical severity of Achilles tendinopathy and evaluates three domains that are clinically relevant to patients: pain, function in daily living and sports activity. The VISA‐A has been successfully used to monitor clinical progress of Achilles tendinopathy.31 We therefore recommend its use as an outcome measure in future research.
What is already known on this topic
Achilles tendinopathy is a major cause of chronic pain and disability.
Eccentric overload training is a widely used and promising conservative intervention in patients with chronic Achilles tendinopathy.
What this study adds
Studies on the effectiveness of eccentric overload training in patients with Achilles tendinopathy show many methodological shortcomings
Studies use “pain” as the only primary outcome measure
There is a lack of studies in which functional outcome measures are used
The Victorian Institute of Sport Assessment‐Achilles Questionnaire is recommended as a valid and reliable functional outcome measure
Conclusion
No definite answer can be given to the question of whether eccentric overload training in patients with chronic Achilles tendinopathy has a beneficial effect on pain and function, because of the methodological shortcomings of the studies. The studies did show that eccentric overload training resulted in a decrease in pain intensity in patients with chronic Achilles tendinopathy. The effect of such training on function and (sports) participation cannot be established definitely at the moment. Large, methodologically sound studies from multiple sites in which functional outcome measures are included are warranted.
Abbreviations
VISA‐A - Victorian Institute of Sport Assessment‐Achilles tendon
Footnotes
Competing interests: None declared.
References
- 1.Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med 200029135–146. [DOI] [PubMed] [Google Scholar]
- 2.Cook J L, Khan K M, Purdam C. Achilles tendinopathy. Man Ther 20027121–130. [DOI] [PubMed] [Google Scholar]
- 3.Kannus P. Tendon pathology: basic science and clinical applications. Sport Exerc Inj 1997362–75. [Google Scholar]
- 4.Silbernagel K G, Thomee R, Thomee P.et al Eccentric overload training for patients with chronic Achilles tendon pain – a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports 200111197–206. [DOI] [PubMed] [Google Scholar]
- 5.Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med 200322727–741. [DOI] [PubMed] [Google Scholar]
- 6.Alfredson H. The chronic painful Achilles and patellar tendon: research on basic biology and treatment. Scand J Med Sci Sports 200515252–259. [DOI] [PubMed] [Google Scholar]
- 7.Almekinders L C, Temple J D. Etiology, diagnosis, and treatment of tendonitis: an analysis of the literature. Med Sci Sports Exerc 1998301183–1190. [DOI] [PubMed] [Google Scholar]
- 8.Hunter G. The conservative management of Achilles tendinopathy. Phys Ther Sports 200016–14. [Google Scholar]
- 9.McLauchlan G J, Handoll H H. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Database Syst Rev 2001CD000232. [DOI] [PubMed]
- 10.Fahlström M, Lorentzon R, Alfredson H. Painful conditions in the Achilles tendon region in elite badminton players. Am J Sports Med 20023051–54. [DOI] [PubMed] [Google Scholar]
- 11.Schepsis A A, Jones H, Haas A L. Achilles tendon disorders in athletes. Am J Sports Med 200230287–305. [DOI] [PubMed] [Google Scholar]
- 12.Sorosky B, Press J, Plastaras C.et al The practical management of Achilles tendinopathy. Clin J Sport Med 20041440–44. [DOI] [PubMed] [Google Scholar]
- 13.Astrom M. Partial rupture in chronic achilles tendinopathy. A retrospective analysis of 342 cases. Acta Orthop Scand 199869404–407. [DOI] [PubMed] [Google Scholar]
- 14.Kader D, Saxena A, Movin T.et al Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med 200236239–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luscombe K L, Sharma P, Maffulli N. Achilles tendinopathy. Trauma 20035215–225. [Google Scholar]
- 16.Paavola M, Kannus P, Jarvinen T A.et al Achilles tendinopathy. J Bone Surg Am 200284‐A2062–2076. [DOI] [PubMed] [Google Scholar]
- 17.Bom L P A. Tendinopathie van de Achillespees (in Dutch). Geneesk Sport 2002353–6. [Google Scholar]
- 18.Alfredson H, Pietila T, Jonsson P.et al Heavy‐load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 199826360–366. [DOI] [PubMed] [Google Scholar]
- 19.Verhagen A P, de Vet H C, de Bie R A.et al The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998511235–1241. [DOI] [PubMed] [Google Scholar]
- 20.Verhagen A P, de Vet H C, Vermeer F.et al The influence of methodologic quality on the conclusion of a landmark meta‐analysis on thrombolytic therapy. Int J Technol Assess Health Care 20021811–23. [PubMed] [Google Scholar]
- 21.Assendelft W J J, Scholten R J P M, Eijk J TMv.et al The practice of systematic reviews. III. Evaluation of methodological quality of research studies (In Dutch). Ned Tijdschr Geneeskd 1999143714–719. [PubMed] [Google Scholar]
- 22.Verhagen A P, de Bie R A, Lenssen A F.et al Impact of quality items on study outcome. Treatments in acute lateral ankle sprains. Int J Technol Assess Health Care 2000161136–1146. [DOI] [PubMed] [Google Scholar]
- 23.Roos E M, Engstrom M, Lagerquist A.et al Clinical improvement after 6 weeks of eccentric exercise in patients with mid‐portion Achilles tendinopathy—a randomized trial with 1‐year follow‐up. Scand J Med Sci Sports 200414286–295. [DOI] [PubMed] [Google Scholar]
- 24.Mafi N, Lorentzon R, Alfredson H. Superior short‐term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc 2001942–47. [DOI] [PubMed] [Google Scholar]
- 25.Niesen‐Vertommen S L, Taunton J E, Clement D B.et al The effect of eccentric versus concentric exercise in the management of Achilles tendonitis. Clin J Sport Med 1992109–113.
- 26.Fahlström M, Jonsson P, Lorentzon R.et al Chronic Achilles tendon pain treated with eccentric calf‐muscle training. Knee Surg Sports Traumatol Arthrosc 200311327–333. [DOI] [PubMed] [Google Scholar]
- 27.Shalabi A, Kristoffersen‐Wilberg M, Svensson L.et al Eccentric training of the gastrocnemius‐soleus complex in chronic achilles tendinopathy results in decreased tendon volume and intratendinous signal as evaluated by MRI. Am J Sports Med 2004321286–1296. [DOI] [PubMed] [Google Scholar]
- 28.Alfredson H, Lorentzon R. Intratendinous glutamate levels and eccentric training in chronic Achilles tendinosis: a prospective study using microdialysis technique. Knee Surg Sports Traumatol Arthrosc 200311196–199. [DOI] [PubMed] [Google Scholar]
- 29.Stanish W D, Rubinovich R M, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res 198665–68. [PubMed]
- 30.Sarasqueta C, Gabaldon O, Iza I.et al Cross‐cultural adaptation and validation of the NASS outcomes instrument in Spanish patients with low back pain. Eur Spine J 200514586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sayana M K, Maffulli N. Eccentric calf muscle training in non‐athletic patients with Achilles tendinopathy. J Sci Med Sport 20071052–58. [DOI] [PubMed] [Google Scholar]
- 32.Bhogal S K, Teasell R W, Foley N C.et al The PEDro scale provides a more comprehensive measure of methodological quality than the Jadad scale in stroke rehabilitation literature. J Clin Epidemiol 200558668–673. [DOI] [PubMed] [Google Scholar]
- 33.Juni P, Holenstein F, Sterne J.et al Direction and impact of language bias in meta‐analyses of controlled trials: empirical study. Int J Epidemiol 200231115–123. [DOI] [PubMed] [Google Scholar]
- 34.Dickersin K. The existence of publication bias and risk factors for its occurrence. JAMA 19902631385–1389. [PubMed] [Google Scholar]
- 35.Robinson J M, Cook J L, Purdam C.et al The VISA‐A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med 200135335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Silbernagel K G, Thomee R, Karlsson J. Cross‐cultural adaptation of the VISA‐A questionnaire, an index of clinical severity for patients with Achilles tendinopathy, with reliability, validity and structure evaluations. BMC Musculoskelet Disord 2005612. [DOI] [PMC free article] [PubMed] [Google Scholar]