Abstract
Background
Eccentric training has been shown to reduce pain and gain function in patients with chronic Achilles tendinopathy. However, currently no data are available regarding any potential adverse effects of an eccentric training intervention on Achilles tendon microcirculation.
Methods
59 patients (49 (12) years; body mass index 27 (5); 49 mid‐portion, 10 chronic insertional tendinopathy) with 64 symptomatic (54 mid‐portion, 10 insertional) Achilles tendons were prospectively enrolled. Baseline tendon microcirculation at four distinct tendon positions from the insertion to the proximal mid‐portion area was assessed using a laser Doppler system for capillary blood flow, tissue oxygen saturation and postcapillary venous filling pressure. A 12‐week daily painful home‐based eccentric training regimen was initiated (3×15 repetitions per tendon and day).
Results
Achilles tendon capillary blood flow was significantly reduced at the insertion (by 35%, p = 0.008) and the distal mid‐portion area (by 45%, p = 0.015) at 2 mm and by 22% (p = 0.007) and 13% (p = 0.122) at 8 mm tissue depths, respectively. Achilles tendon oxygen saturation was not decreased after the 12‐week eccentric training regimen throughout the insertion to the proximal mid‐portion area (insertion 72 (13) vs 73 (10), proximal mid‐portion 63 (13) vs 62 (11), both NS). Achilles tendon postcapillary venous filling pressures were significantly reduced at the insertion (51 (16) vs 41 (19), p = 0.001) and the distal mid‐portion (36 (13) vs 32 (12), p = 0.037) at 2 mm and at the insertion at 8 mm (63 (19) vs 51 (13), p = 0.0001). Pain was reduced from 5.4 (2.1) to 3.6 (2.4; p = 0.001) in the mid‐portion and from 6 (2.5) to 3.2 (2.7; p = 0.002) in the insertional tendinopathy group. No Achilles tendon rupture or any interruption during the eccentric training was noted among the 59 patients.
Conclusion
Daily eccentric training for Achilles tendinopathy is a safe and easy measure, with beneficial effects on the microcirculatory tendon levels without any evident adverse effects in both mid‐portion and insertional Achilles tendinopathy.
Eccentric exercise training in tendinopathy has been applied since the 1980s.1 In 1996, Alfredson et al2 showed that among 13 patients undergoing surgical treatment for chronic Achilles tendinopathy, 6 months of postoperative rehabilitation for chronic Achilles tendinitis was not enough to recover concentric and eccentric plantar flexion muscle strength compared with the non‐injured side. In 1998, 15 recreational athletes with chronic Achilles tendinopathy performed a calf muscle strength training >12 weeks, with all 15 patients back at their preinjury levels with full running activity after the eccentric training regimen.3 Currently, mid‐portion tendinopathy is believed to be superiorly reduced by eccentric training, with only limited effects in insertional tendinopathy.
Response rates to eccentric training vary, with highest rates reported among high‐level athletes and lower response rates of about 60% among sedentary patients, as shown recently by Sayana and Maffulli.4 The effects of a 12‐week eccentric training intervention on the pain level are evident about 6 weeks after initiation and last for at least 1 year.5 Among 25 patients, a decreased tendon thickness was noted for up to 3.8 years following a 12‐week eccentric training intervention.6
It seems that the neovascularisation is decreased by an eccentric training intervention, as demonstrated by colour Doppler sonography.7 Recently an increased collagen synthesis rate with increased carboxy terminal propeptide of type I collagen (3.9 (2.5) μg/l before to 19.7 (5.4) μg/l after, p<0.05) using microdialysis technology was found after 12 weeks of eccentric training among six soccer players with Achilles tendinopathy.8
Despite the accumulating published data regarding its effectiveness and possible pathophysiological effects among patients with chronic Achilles tendinopathy, no data are currently available regarding any potential associated adverse effects to the Achilles tendon microcirculation following painful eccentric training.
Laser Doppler flowmetry shows that baseline Achilles tendon microcirculation in healthy athletes differs from patients with either insertional or mid‐portion tendinopathy, where capillary blood flow is increased at the point of pain.9 We hypothesised that 12 weeks of eccentric training does not harm Achilles tendon microcirculatory parameters among patients with chronic Achilles tendinopathy.
Methods
A total of 59 patients (>18 years) were included after informed consent to participate in the study was obtained. The diagnosis of Achilles tendinopathy was made if patients exerted pain at the tendon at rest or at exercise, either at the insertional zone at the calcaneus or in the mid‐portion area of the Achilles tendon 2–6 cm proximal to the insertion associated with tenderness and swelling after conventional grey‐scale ultrasound showing hypoechogenic texture and tendon enlargement. All patients with insertional pain did not have any bony abnormality such as Haglund exostosis, spurs or fragments, but had pure tendon abnormalities with tendon enlargement at the insertion with hypoechogenic texture in grey‐scale ultrasound. Patients with prior Achilles tendon surgery were excluded. None of the patients included had any prior therapy by eccentric exercise training before the study. The daily eccentric training was performed with 3×15 repetitions per tendon per day (2 s each position) with straight knee only.
Mid‐portion and insertional tendinopathy
The distribution was 49 patients with chronic mid‐portion tendinopathy and 10 patients with chronic insertional tendinopathy with a total number of 64 symptomatic Achilles tendons (54 mid‐portion and 10 insertional with pure tendon problems without bony abnormalities).
Symptoms, function and foot and ankle‐related quality of life were evaluated by the Foot and Ankle Outcome Score (FAOS). The FAOS has been found to have a high test–retest reliability, indicating that the FAOS is an accurate measure with high ability to measure even small changes over time.5,10 Pain was assessed on a Visual Analogue Scale, ranging from 0 for no pain at all to 10 for the most imaginable pain.
A non‐invasive real‐time combined laser Doppler and spectroscopy system (Oxygen‐to‐see, LEA Medizintechnik, Giessen, Germany) was applied, which has been used clinically as mentioned before in the Achilles tendon as well as in studying the effects of combined cryotherapy and compression (Aircast Cryo/Cuff, Summit, New Jersey, USA) at the ankle level.11 The Oxygen‐to‐see system has been shown to have a high intraobserver and interobserver reliability.12
Every subject was measured at both legs at four positions, which were placed on the Achilles tendon. We determined the microcirculation at 2 and 8 mm tissue depths at each level at four tendon positions, which were exactly the same in each patient. All positions were determined in relation to the bony heel by measurement of length and were exactly the same on both legs in each patient:
Insertion of the Achilles tendon
2 cm proximal of the insertion as distal mid‐portion position
4 cm proximal of the insertion as middle mid‐portion position
6 cm proximal of the insertion as proximal mid‐portion position.
Statistics
The data are presented as median and range for continuous variables or number and percentages for dichotomous variables. Univariate analysis of categorical data was carried out using the χ2 or Fisher exact tests. Student's t test was applied for parametric, ordinal variables of connected samples. A p value <0.05 was considered to indicate significance. SPSS V.13.0 for Windows was used for statistical analysis.
Results
Tendon capillary blood flow
Achilles tendon capillary blood flow was significantly reduced at the insertion at 2 mm (by 35%, p = 0.008, fig 1) and at 8 mm tissue depth (98 (7) vs 76 (53), p = 0.007) in all patients with tendinopathies. Focusing only on the patients with insertional pure tendinopathies, insertional capillary blood flow was reduced superficially, not significantly, with only 10 tendons (24 (27) vs 15 (11), −37%, p = 0.325), an effect that was seen at the distal mid‐portion (20 (31) vs 11 (10), −45%, p = 0.112) and the middle mid‐portion (18 (11) vs 10 (9), −45%, p = 0.169) for insertional tendinopathy. At 8 mm tissue depth, in patients with insertional tendinopathy the capillary flow was reduced at the insertion (105 (81) vs 70 (48), −33%, p = 0.173), the distal mid‐portion (93 (71) vs 65 (37), −30%, p = 0.197) and the middle mid‐portion (83 (46) vs 53 (18), −36%, p = 0.085), not significantly, owing to the large standard deviation among the 10 insertional pain tendons. Furthermore, at the superficial distal mid‐portion area, the tendon capillary blood flow was reduced significantly (22 (32) vs 12 (10), p = 0.015). At all other positions, the capillary blood flow was reduced, but did not reach any level of significance among the 59 patients included. No increase of capillary blood flow was noted.
Figure 1 Achilles tendon capillary blood flow at 2 mm depth at baseline at the start of the study (left) and after (right) 12 weeks of daily painful eccentric training in chronic Achilles tendinopathy in 59 patients with 64 symptomatic tendons.
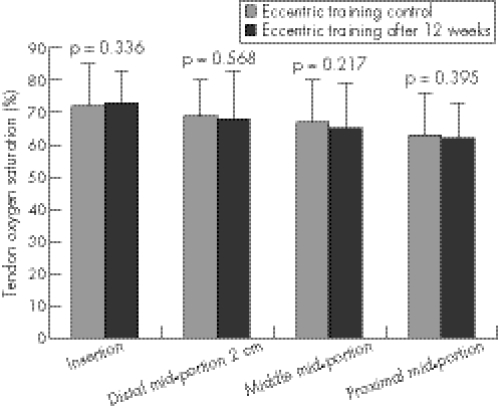
Tendon oxygen saturation
Eccentric training does not compromise tendon oxygen saturation throughout the entire tendon. From the insertion (72 (13) vs 73 (10), p = 0.336, fig 2) to the proximal mid‐portion area (63 (13) vs 62 (11), p = 0.395), no significant change was noted. Following division in insertional and mid‐portion tendinopathy, no significant changes of tendon oxygen saturation were evident throughout the tendon.
Figure 2 Achilles tendon oxygen saturation at the start of the study (left) and after (right) 12 weeks of daily painful eccentric training in chronic Achilles tendinopathy in 59 patients with 64 symptomatic tendons.
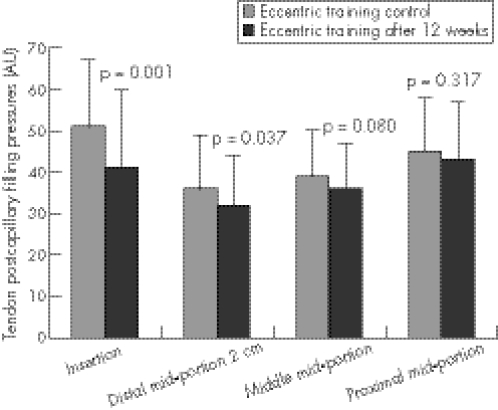
Figure 3 Achilles tendon postcapillary venous filling pressures at the start of the study (left) and after (right) 12 weeks of daily painful eccentric training in chronic Achilles tendinopathy in 59 patients with 64 symptomatic tendons.
Tendon post‐capillary venous filling pressures
Eccentric training decreases post‐capillary venous filling pressures throughout the entire Achilles tendon with predominant effects at the tendon insertion at 2 mm (51 (16) vs 41 (19), p = 0.001) and 8 mm tissue depths (63 (19) vs 51 (13), p = 0.0001, fig 3). No increase in tendon post‐capillary venous filling pressure was noted. Tables 1–3 show the differentiation for mid‐portion and insertional tendinopathy.
Table 1 Patient characteristics among 59 patients with 64 symptomatic Achilles tendons .
| Eccentric training, n = 59 patients with 64 tendons | |
|---|---|
| Men | 39 (61%) |
| Female | 25 (39%) |
| Age (years) | 49 (12) |
| Mid‐portion | 49 points with 54 tendons |
| Insertional (pure tendon problems, no bony abnormalities) | 10 points with 10 tendons |
| Body mass index (kg/m2) | 27 (5) |
| <19.9 | 4 (6%) |
| 20–24.9 | 18 (28%) |
| 25–29.9 | 31 (48%) |
| 30–34.9 | 6 (9%) |
| 35–39.9 | 3 (5%) |
| >40 | 2 (3%) |
| Profession | |
| Physically demanding job | 15 (23%) |
| Student | 2 (3%) |
| Retired | 8 (12.5%) |
| Teacher | 7 (11%) |
| Acadamic | 20 (31%) |
| Non‐acadamic | 35 (55%) |
| Training | |
| Healthy sports (walking, swimming, biking) | 46 (72%) |
| Running | 19 (30%) |
| Soccer | 5 (8%) |
| All other ball sports | 12 (19%) |
| Injuries | |
| Achilles tendon | 9 (14%) |
| Previous plantar fasciitis | 3 (6%) |
| Previous ankle sprain | 16 (25%) |
| Knee | 14 (22%) |
| Arthritis | 6 (43%) |
| Meniscus tear | 1 (7%) |
| Ligament injury | 5 (36%) |
| Others | 2 (14%) |
| Muscle injuries | 5 (8%) |
| Ankle arthritis | 9 (15%) |
| Injury at symptomatic tendon side | 25 (40%) |
| History | |
| None | 47 (76%) |
| Diabetes mellitus | 4 (6%) |
| Arterial hypertension | 16 (25%) |
| Smoking | |
| Never | 57 (89%) |
| <5 cigarettes/day | 1 (2%) |
| >5 cigarettes/day | 6 (9%) |
Table 2 Postcapillary venous filling pressures among 49 patients with mid‐portion tendinopathy with 54 symptomatic tendons.
| 2 mm | % | p Value | 8 mm | % | p Value | |
|---|---|---|---|---|---|---|
| Insertion | 51 (16) vs 41 (18) | −20 | 0.003 | 64 (18) vs 53 (13) | −17 | 0.001 |
| Distal mid‐portion | 36 (13) vs 32 (11) | −11 | 0.066 | 58 (21) vs 54 (19) | −7 | 0.253 |
| Middle mid‐portion | 38 (11) vs 36 (11) | −5 | 0.273 | 54 (18) vs 51 (14) | −6 | 0.167 |
| Proximal mid‐portion | 44 (14) vs 42 (13) | −5 | 0.282 | 60 (21) vs 57 (21) | −5 | 0.340 |
Table 3 Postcapillary venous filling pressures among 10 patients with insertional tendinopathy with 10 symptomatic tendons.
| 2 mm | % | p Value | 8 mm | % | p Value | |
|---|---|---|---|---|---|---|
| Insertion | 49 (24) vs 39 (25) | −20 | 0.438 | 65 (26) vs 53 (18) | −18 | 0.149 |
| Distal mid‐portion | 32 (8) vs 29 (16) | −9 | 0.437 | 54 (21) vs 55 (23) | 2 | 0.899 |
| Middle mid‐portion | 37 (10) vs 33 (10) | −11 | 0.312 | 54 (20) vs 48 (14) | −11 | 0.336 |
| Proximal mid‐portion | 45 (16) vs 48 (14) | 7 | 0.348 | 54 (19) vs 63 (27) | 17 | 0.169 |
Foot and Ankle Outcome Score
The eccentric training could significantly increase the FAOS regarding symptoms (93 (16) vs 94 (16), p = 0.01), pain (98 (18) vs 99 (19), p = 0.023), sport (95 (23) vs 97 (20), p = 0.002) and quality of life (88 (17) vs 92 (24), p = 0.0001).
Pain on Visual Analogue Scale
The eccentric training reduced the overall pain in Achilles tendinopathy significantly from 5.5 (2.1) to 3.6 (2.4; p = 0.0001). At a follow‐up of 12 months, no Achilles tendon rupture occurred. Pain was reduced from 5.4 (2.1) to 3.6 (2.4; p = 0.001) in the mid‐portion and from 6 (2.5) to 3.2 (2.7; p = 0.002) in the insertional tendinopathy group (fig 4).
Figure 4 Pain on Visual Analogue Scale (VAS) for mid‐portion tendinopathy (49 patients with 54 symptomatic tendons) and insertional tendinopathy (10 patients with 10 symptomatic tendons) after 12 weeks of daily eccentric training.
Discussion
A 12‐week eccentric training regimen is not harmful for altered Achilles tendon microcirculation in insertional and mid‐portion Achilles tendinopathy. Increased tendon capillary blood flow is decreased significantly at the insertion and the distal mid‐portion area in symptomatic tendons, which is in line with the published data regarding the disappearance of neovessels following eccentric training.6,7 Interestingly, patients with both mid‐portion and insertional tendinopathy could reduce their pain level following 12 weeks of painful eccentric training. The patients with insertional pain included in this study had pure tendinopathy without any bony abnormality such as Haglund exostosis or spurs, which might have caused impingement with limited success for the patients.
This paper shows for the first time that Achilles tendon oxygenation is not impaired by painful 12‐week eccentric training throughout the entire symptomatic tendon. A decreased tissue oxygenation is associated with local acidosis and impaired cell function owing to relative ischaemia, as shown in case of vessel removal.13 An increased tendon oxygen saturation might enhance the local metabolism, which can be achieved by intermittent cryotherapy and compression using the Cryo/Cuff device (Aircast) on the mid‐portion Achilles tendon14 or in case of preconditioning such as in cardiac surgery, to prepare the myocardium against ischaemia in beating heart surgery.
The post‐capillary Achilles tendon venous filling pressures indicate the capillary outflow out of the tendon. Increased post‐capillary tendon pressures cause venous congestion and deteriorate local metabolic function.15 This is encountered in disease states such as post‐thrombotic syndromes. We found that decreased pressures after 12 weeks of eccentric training thus facilitate capillary venous outflow and are therefore beneficial for the local clearance of metabolic end products, which might decrease pain in addition to reduced capillary tendon blood flow. Eccentric training reduces post‐capillary venous filling pressures throughout the tendon with maximal effects at the tendon insertion.
In conclusion, we found that 12‐week eccentric training is not harmful with regard to the microcirculatory Achilles tendon level. It is beneficial, easy to apply and should be promoted broadly among patients with mid‐portion as well as insertional tendinopathy without bony abnormalities, as the microcirculatory changes and the pain level reduction indicate that both groups may benefit from painful eccentric training.
What is already known on this topic
Neovascularisation plays an important role in Achilles tendinopathy. Capillary blood flow is quantitatively increased at the point of pain in both insertional and mid‐portion Achilles tendinopathy.
Daily painful eccentric training over 12 weeks can reduce pain in mid‐portion tendinopathy.
What this study adds
Daily painful eccentric training does not compromise insertional or mid‐portion microcirculation.
It is a safe and easy measure with beneficial effects on the microcirculatory tendon levels without any evident adverse effects in both mid‐portion and insertional Achilles tendinopathy.
Pain is reduced significantly in patients with mid‐portion and pure insertional tendinopathy.
Abbreviations
FAOS - Foot and Ankle Outcome Score
Footnotes
Competing interests: None declared.
References
- 1.Stanish W, Rubinovich M, Curvin S. Eccentric exercise in chronic tendonitis. Clin Orthop 198620865–68. [PubMed] [Google Scholar]
- 2.Alfredson H, Pietila T, Lorentzon R. Chronic Achilles tendinitis and calf muscle strength. Am J Sports Med 199624829–833. [DOI] [PubMed] [Google Scholar]
- 3.Alfredson H, Pietila T, Jonsson P.et al Heavy‐load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 199826360–366. [DOI] [PubMed] [Google Scholar]
- 4.Sayana M K, Maffulli N. Eccentric calf muscle training in non‐athletic patients with Achilles tendinopathy. J Sci Med Sport 20071052–58. [DOI] [PubMed] [Google Scholar]
- 5.Roos E M, Engstrom M, Lagerquist A.et al Clinical improvement after 6 weeks of eccentric exercise in patients with mid‐portion Achilles tendinopathy—a randomized trial with 1‐year follow‐up. Scand J Med Sci Sports 200414286–295. [DOI] [PubMed] [Google Scholar]
- 6.Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. Br J Sports Med 2004388–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid‐portion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc 200412465–470. [DOI] [PubMed] [Google Scholar]
- 8.Langberg H, Ellingsgaard H, Madsen T.et al Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports 20071761. [DOI] [PubMed] [Google Scholar]
- 9.Knobloch K, Kraemer R, Lichtenberg A.et al Achilles tendon and paratendon microcirculation in mid‐portion and insertional tendinopathy in sportsmen. Am J Sports Med 20063492–97. [DOI] [PubMed] [Google Scholar]
- 10.Roos E M, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int 200122788–794. [DOI] [PubMed] [Google Scholar]
- 11.Knobloch K, Kraemer R, Gössling T.et al Microcirculation of the ankle after Cryo/Cuff application in healthy volunteers. Int J Sport Med 200627250–255. [DOI] [PubMed] [Google Scholar]
- 12.Ghazanfari M, Vogt L, Banzer W.et al Reproducibility of non‐invasive blood flow measurements using laser Doppler spectroscopy. Phys Med Rehab Kuror 200212330–336. [Google Scholar]
- 13.Knobloch K, Lichtenberg A, Pichlmaier M.et al Palmar microcirculation following harvesting of the radial artery in coronary revascularisation. Ann Thorac Surg 2004791026–1030. [DOI] [PubMed] [Google Scholar]
- 14.Knobloch K, Grasemann R, Jagodzinski M.et al Changes of Achilles mid‐portion tendon microcirculation after repetitive simultaneous cryotherapy and compression using standardized cryo‐compression device (Cryo/Cuff™). Am J Sports Med 2006341953–1959. [DOI] [PubMed] [Google Scholar]
- 15.Knobloch K, Lichtenberg A, Pichlmaier M.et al Sternal microcirculation after harvesting of the left internal thoracic artery in cardiac surgery. Thorac Cardiovasc Surg 200351255–259. [DOI] [PubMed] [Google Scholar]