Abstract
Aim
To assess whether the use of a night splint is of added benefit on functional outcome in treating chronic midportion Achilles tendinopathy.
Methods
This was a single‐blind, prospective, single centre, randomised controlled trial set in the Sports Medical Department, The Hague Medical Centre, The Netherlands. Inclusion criteria were: age 18–70 years, active participation in sports, and tendon pain localised at 2–7 cm from distal insertion. Exclusion criteria were: insertional disorders, partial or complete ruptures, or systemic illness. 70 tendons were included and randomised into one of two treatment groups: eccentric exercises with a night splint (night splint group, n = 36) or eccentric exercises only (eccentric group, n = 34).
Interventions
Both groups completed a 12‐week heavy‐load eccentric training programme. One group received a night splint in addition to eccentric exercises. At baseline and follow‐up at 12 weeks, patient satisfaction, Victorian Institute of Sport Assessment–Achilles questionnaire (VISA‐A) score and reported compliance were recorded by a single‐blind trained researcher who was blinded to the treatment.
Results
After 12 weeks, patient satisfaction in the eccentric group was 63% compared with 48% in the night splint group. The VISA‐A score significantly improved in both groups; in the eccentric group from 50.1 to 68.8 (p = 0.001) and in the night splint group from 49.4 to 67.0 (p<0.001). There was no significant difference between the two groups in VISA‐A score (p = 0.815) and patient satisfaction (p = 0.261).
Conclusion
A night splint is not beneficial in addition to eccentric exercises in the treatment of chronic midportion Achilles tendinopathy.
Overuse injury of the Achilles tendon is a common entity in athletes and older athletes are at an increased risk. When the exact origin of tendon pain is unclear, the term tendinopathy is preferred.1,2
Scientific evidence for many proposed aetiological factors (biomechanical abnormalities, alteration of vascularity, certain systemic diseases, use of certain medications, genetic predisposition and excessive load in sports) is scarce.3,4 Consequently, there is no consensus as to which treatment should be used. Many differing treatments have been proposed, but none of these treatments have shown reproducible promising results in randomised trials.5,6,7
Alfredson et al8 described a heavy‐load eccentric exercise programme for 15 athletes with chronic Achilles tendinosis. It consisted of 180 repetitions daily, which were allowed to be painful. The results were excellent in all athletes. In subsequent studies, comparable results were reported.9,10,11,12
A recent systematic review on the effect of eccentric overload training, in which nine studies satisfied the methodological criteria, showed that the effects on pain are promising.13 They stated, however, that the weakness of all these publications is that only pain is used when scoring the outcomes. Besides pain, the functional status and (sports) activity should be scored to determine the magnitude of the effect, and they suggest using the validated Victorian Institute of Sport Assessment–Achilles questionnaire (VISA‐A) score.
The basic mechanisms underlying the effectiveness of eccentric exercises are unknown to date. Alfredson14 suggests a few possible theories. The first theory is that an alteration of pain perception, due to the painful exercises, reduces the symptoms.14 The second theory is based on the ingrowth of neovessels with accompanying nerves around the tendon, which are supposed to be the source of pain. Eccentric exercises should destroy these neovessels.5,14 The third theory is that loading improves the tensile strength of the tendons. It may also induce lengthening of the musculotendinous junction and, therefore, put less strain on the Achilles tendon during movement.14
The use of a night splint has been shown to be effective in cases of chronic plantar fasciitis.15,16,17 There are several hypotheses supporting the use of a night splint, which provides passive dorsiflexion, in cases of Achilles tendinopathy. One hypothesis is that a night splint would work for Achilles tendinopathy owing to lengthening of muscle and tendon, and the concomitant reduction in strain on the tendon.11 It has been stated that passive dorsiflexion may be helpful in chronic Achilles tendon injury.2
The effect of splinting has been studied twice with differing results. Dijkstra and Van Enst18 found clinical benefit using splinting alone. Roos et al11 reported no difference between the three groups: eccentric exercises, use of a night splint and combination of splinting and eccentric exercises.
The aim of this single‐blinded prospective study is to compare the short‐term effects on pain and functional outcome of a heavy‐load eccentric exercise programme, with a heavy‐load eccentric programme in combination with the use of a night splint.
Materials and methods
Patients
The location for the study was an outpatient sports medicine department in a large district general hospital (The Hague Medical Centre, The Netherlands). We included patients who were referred by a general practitioner, physical therapist or a medical specialist. Most of the patients had already received another conservative treatment, but none had undergone surgical treatment, a heavy‐load eccentric training programme or used a night splint before.
Inclusion criteria were patients aged between 18 and 70 years, presence of symptoms for >2 months, active participation in sporting activities before the onset of symptoms and the patients' wish to return to their original level of sports. All patients had a tendon that was tender on palpation and painful during or after sport. The tendon thickening was located approximately 2–7 cm proximal to the distal insertion. The diagnosis was made based on clinical examination. Exclusion criteria were the previous performance of an intensive programme of heavy‐load eccentric exercises and inability to perform heavy‐load exercises. Insertional disorders, tendon ruptures and patients with systemic illness were also excluded.
Study design
The study design was a single‐blinded randomised controlled trial. Patients were randomised after initial standardised assessment to one of two treatment groups: eccentric exercises or eccentric exercises in combination with a night splint. The researcher was blinded to the treatment groups. An appointment was made after 4 weeks to evaluate possible problems. Patients were followed‐up after 12 weeks.
Patient evaluation
After the patients were informed about the aims and possible risks of the study, they signed the informed consent form. The study protocol was approved by the Medical Ethics Committee, The Hague Medical Centre, The Netherlands.
All patients were examined by the same single researcher using a standard protocol consisting of standardised outcome measures: the VISA‐A19 was completed with minimum assistance from the researcher, and patient satisfaction was rated subjectively as poor, fair, good or excellent. A good or excellent result was considered as successful.
After completing the history and examination, all patients received detailed instruction about how to perform the eccentric exercises. The patient was then sent to the secretary, where they chose an envelope from a box that contained 80 envelopes for randomisation of the treatment. Patients who were randomised to the night splint received further instruction from a different clinician to ensure adequate blinding.
Outcome was evaluated by the researcher at baseline and at 12 weeks.
The Wilcoxon signed rank test was used to assess changes over time in the variables within groups and the Mann Whitney U test was used to detect changes over time between the two groups. The χ2 test was used to evaluate patient satisfaction and compliance between groups. Statistical significance was assumed when p<0.05.
Eccentric exercises
The eccentric calf muscle exercises were performed with straight knee and with bent knee as described by Alfredson et al.8
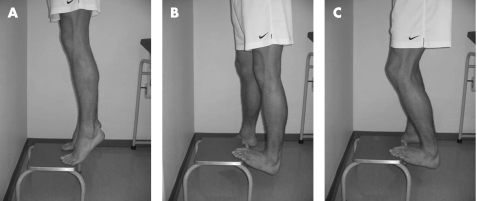
The researcher explained and demonstrated the exercise programme and patients were also shown a video of the exercises (fig 1). Finally, the patients had to perform a series of supervised eccentric drops, until the technique was correct.
Figure 1 Instruction of eccentric exercises to patients started with a heel lift (A), after that the eccentric drop was performed with the injured leg with straight knees (B) and flexed knees (C). Informed consent was obtained for the publication of this figure.
The patients were instructed to perform 180 repetitions a day, beginning on the first day without a period of gradual increase. Patients were instructed that these exercises commonly cause pain and that they should ignore this pain. They were also instructed to increase the load when the exercises could be performed without any discomfort. Increasing load was done using a backpack, with added weights, or a weight machine. When pain during or after exercises was unbearable or disabling, the patient had to contact the clinician, not the researcher. The patients were informed that they could expect muscle soreness, besides experiencing pain. All patients were instructed to avoid weight‐bearing sporting activities for the first 4 weeks. After 4 weeks, gradual return to sports activities was encouraged if the pain allowed.
Night splint (additional to eccentric exercises)
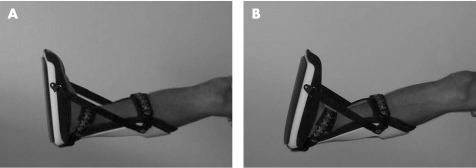
Patients had a 50% chance of being randomised to receive a night splint (UFO night splint, Somas Industries, Sint Anthonis, The Netherlands) besides the eccentric exercises. In this case, the patient was sent to a different clinician for consultation to ensure blinding. The clinician decided which size was suitable for the patient. After that, the ankle positions of 0° and 5° dorsiflexion were marked on the night splint. The patient could easily adjust the splint between these two positions. For the first 4 weeks, patients had to maintain the neutral position of 0°, and after this period, the position of at least 5° dorsiflexion was used. Patients were told that the night splint should be positioned beyond these 5° dorsiflexion if pain could be tolerated (fig 2). Pain and the extent of sleep disturbances were the main guidelines when positioning the night splint.
Figure 2 Night splint fitted in a patient. In the first 4 weeks, a neutral position of 0° dorsiflexion was maintained (A). After 4 weeks of treatment, a position of 5° dorsiflexion was advised. Dorsiflexion of more degrees was recommended, when tolerated (B). Informed consent was obtained for the publication of this figure.
Compliance
Patient compliance was measured by daily registration in the form of a diary. The patients had to note their number of repetitive exercises performed. Items on the night splint diary were number of hours the splint was worn and degrees in which the splint was positioned. Compliance was divided into four categories. When <25% of the exercises were performed, patient compliance was scored as poor. Between 25% and 50% it was scored as moderate, between 50% and 75% as good, and >75% was scored as an excellent compliance.
Results
Patients
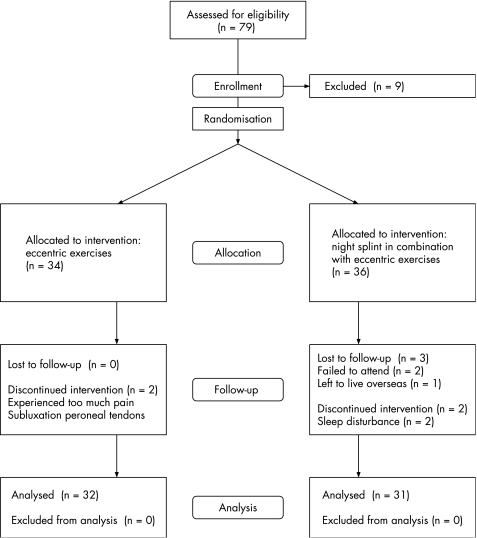
Between March 2005 and December 2005, 67 patients (79 tendons) visited the Hague Medical Centre for the study. Nine tendons were excluded. Four patients had an insertional disorder, two patients already performed a heavy‐load eccentric exercise programme, one patient had a partial rupture, one patient had a total rupture and one patient was unable to carry out the eccentric exercises.
In all, 58 patients (70 tendons, 46 unilateral and 12 bilateral) met the inclusion criteria. The mean (range) age was 44.6 (26–59) years, mean (range) duration of symptoms 30.7 (2–221) months and the mean (range) body mass index was 25.1 (20.2–34.5) kg/m2. All patients participated actively and most of them had to stop their sporting activities (mean (range) 13 (0–104) weeks).
A total of 70 tendons were randomised into two groups: 34 in the eccentric excersises only (eccentric group) and 36 in the eccentric excersises with the night splint (night splint group). At baseline, there were no statistical differences in patient characteristics between the groups (table 1).
Table 1 Patient characteristics at baseline.
| Variable | Eccentric group | Night splint group |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Patient's age (years) | 44.1 (7.0) | 45.1 (8.9) |
| Male/female | 20/12 | 17/14 |
| Body mass index | 25.4 (3.1) | 24.9 (3.2) |
| Duration of symptoms (months) | 33.7 (55.6) | 27.7 (45.9) |
| Duration of sports neglect (weeks) | 12.6 (24.4) | 13.4 (25.1) |
No significant differences in patient characteristics were found between the eccentric group and night splint group (night splint in combination with eccentric exercises).
There was a significant higher patient satisfaction in the group of patients (n = 9, patient satisfaction 89%) with a duration of symptoms of <5.5 months when compared to the group of patients (n = 54, patient satisfaction 50%) with a duration of symptoms of >5.5 months (p = 0.03).
There was a significant higher VISA‐A score after 12 weeks in the group of patients (n = 9, VISA‐A score 87) with a duration of symptoms of <5.5 months when compared to the group of patients (n = 54, VISA‐A score 65) with a duration of symptoms of >5.5 months (p = 0.019). The VISA‐A score at baseline did not differ significantly between these groups (p = 0.232).
In the night splint group, there were four patients (five tendons) who could not be included in the analysis. One patient (two tendons) was poorly motivated and failed to attend the follow‐up appointments, one patient (one tendon) left to live overseas and two patients (two tendons) stopped using the night splint because of sleep disturbance.
Results within groups
Patient satisfaction in the eccentric group after 12 weeks was excellent or good in 20 (63%) tendons and moderate or poor in 12 (37%) tendons. Patient satisfaction in the night splint group after 12 weeks was excellent or good in 15 (48%) tendons and moderate or poor in 16 (52%) tendons.
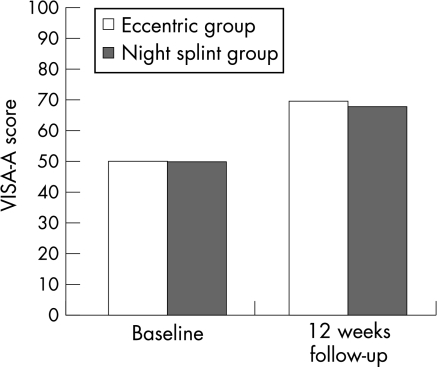
Figure 3 shows the change in VISA‐A score within each treatment group.
Figure 3 VISA‐A score in the two treatment groups. In both treatment groups, VISA‐A score improved significantly. There was no significant difference at baseline and at 12 weeks follow‐up between these two groups after 12 weeks.
The VISA‐A score in the eccentric group increased significantly from 50.1 at baseline to 68.8 after 12 weeks (p = 0.001). In the night splint group, the VISA‐A score also increased significantly from 49.4 at baseline to 67 after 12 weeks (p<0.001).
In the eccentric group, there was an increase in VISA‐A score in 78% of the tendons after 12 weeks, compared with baseline. In the night splint group, 71% of the tendons had a higher VISA‐A score after 12 weeks.
Results between groups
No significant differences were found in VISA‐A score between the treatment groups after 12 weeks treatment (p = 0.815).
There was no statistically significant difference in patient satisfaction between the two treatment groups at 12 weeks follow‐up (p = 0.261).
Compliance
Table 2 shows reported patient compliance after 12 weeks therapy in the two treatment groups.
Table 2 Good/excellent patient satisfaction in the two treatment groups after 12 weeks.
| Patient satisfaction | ||
|---|---|---|
| Eccentric group (n = 32) | Night splint group (n = 31) | |
| Overall | 20 (63) | 15 (48) |
| Good/excellent compliance | 16 (70) | 9 (50) |
| Moderate/poor compliance | 4 (44) | 1 (0) |
Values are n (%). Besides the overall results (2nd row), good/excellent patient satisfaction was calculated for good/excellent compliance (3rd row) and moderate/poor compliance (4th row). Better patient compliance in the eccentric group tends to lead to a higher patient satisfaction than patients with a low reported compliance for the eccentric exercises in the eccentric group. However, the differences were not statistically significant.
In all, 17 of 63 (27%) subjects reported a moderate or poor compliance after a 12‐week programme of eccentric exercises (in eccentric and night splint group).
Compliance in the eccentric group
Compliance reported after 12 weeks in the eccentric group was excellent or good in 23 of 32 (72%) patients; patient satisfaction in this group was excellent or good in 16 (70%) patients and moderate or poor in 7 (30%) patients (table 2).
Compliance was moderate or poor in 9 (28%) patients; patient satisfaction in this group was excellent or good in 4 (44%) patients and moderate or poor in 5 (56%) patients. There were no statistically significant differences between these groups (p = 0.194).
Compliance in the night splint group
Eccentric exercises
In the night splint group, reported compliance of the eccentric exercises after 12 weeks was good or excellent in 23 of 31 (74%) patients; patient satisfaction in this group was excellent or good in 13 (57%) patients and moderate or poor in 10 (43%) patients.
Compliance was moderate or poor in 8 (26%) patients; patient satisfaction in this group was excellent or good in 2 (25%) patients and moderate or poor in 6 (75%) patients. There were no statistically significant differences between these groups (p = 0.131).
Night splint
Compliance of the night splint after 12 weeks was excellent or good in 25 of 31 (81%) patients; patient satisfaction in this group was excellent or good in 11 (44%) patients and moderate or poor in 14 (56%) patients.
Compliance was moderate or poor in 6 (19%) patients; patient satisfaction in this group was excellent or good in 4 (67%) patients and moderate or poor in 2 (33%) patients. There were no statistically significant differences between these groups (p = 0.931).
Eccentric exercises and night splint
In the night splint group, reported compliance of both the eccentric exercises and the night splint after 12 weeks was good or excellent in 18 of 31 (58%) patients; patient satisfaction in this group was excellent or good in 9 (50%) patients and moderate or poor in 9 (50%) patients. Compliance was moderate or poor for both the eccentric exercises and the night splint in 1 of 31 patients; patient satisfaction was rated as poor (table 2).
Complications and dropouts
Figure 4 shows the progress of patients through the study. Two patients (two tendons) did not complete the treatment in the eccentric group. One patient experienced too much pain and one patient developed a subluxation of the peroneal tendon during the study, which prevented him from performing the exercises.
Figure 4 Progress of patients through the study.
In a few cases, the night splint caused minor symptoms, which did not prevent further treatment. Two patients experienced painful pressure areas and one patient could not increase dorsiflexion of the night splint >0° because of paraesthesia of the foot.
Discussion
This prospective study shows that splinting in addition to eccentric exercises did not lead to a significantly better outcome for patient satisfaction and VISA‐A score.
The effect size of eccentric training is still uncertain and few studies have a sound method.13 The early studies showed promising results of eccentric training on pain and/or patient satisfaction,9,10,11,12 but functional outcome scores are required.13 The VISA‐A questionnaire is a validated score for Achilles tendinopathy, which measures pain, and also function in daily living and sporting activity. In a recent study in non‐athletes, Sayana and Maffulli20 have shown VISA‐A scores of approximately 50 after a 12‐week heavy‐load eccentric exercise programme. In their population, improvement was scored in 19 of 34 (56%) patients, which is comparable with our results. Brown et al21 found that only 13% of the patients treated with heavy‐load eccentric training and placebo injections had returned to sports after 3 months.
The patient satisfaction after a heavy‐load eccentric exercise programme (63%) is lower than previously reported Scandinavian studies; overall satisfaction in these trials is around 80–90%.8,9,10,11,12 An explanation for this result could be that our population had a longer duration of symptoms. The mean duration of symptoms in previous studies ranged from 5.5 to 21 months. Mean duration of symptoms in our population was 31.6 months. A longer duration of symptoms is generally thought to be associated with a worse prognosis and we found that patients who had symptoms for <5.5 months had a better outcome. Another explanation could be the shorter follow‐up time used in our study. The follow‐up time ranged from 12 weeks to 3.8 years in previously published Scandinavian studies. In this study, a follow‐up time of 12 weeks was used. This was found to be the case in the study of Brown et al,21 who showed that although only 13% had returned to sport after 3 months, 85% had returned at 1 year.
Dijkstra and Van Enst18 retrospectively studied nine patients with Achilles tendinopathy and concluded that a night splint reduced pain after a mean duration of 9.4 months. The mean visual analogue score decreased from 7.3 to 2.7. In a prospective randomised controlled trial, Roos et al11 reported that effects of eccentric exercises alone were comparable to a night splint or a combination of eccentric exercises with a night splint. A gradual onset of the exercises was used during the first week and when the patient could perform the exercises without discomfort, an increased load was prescribed. In all, 44 patients were included in this study. After 6 weeks, pain reduction in the eccentric group was 27%, in the night splint‐only group 19% and in the night splint combined with eccentric group 18%. These differences were not statistically significant between the groups. After 1 year, there were no differences between groups and there was significant improvement in pain reduction (35–42%) in all groups compared to baseline. Roos et al11 proposed that a night splint may negatively influence the positive effect of eccentric exercises to the muscle tendon unit. To our knowledge, Roos et al11 are the only other researchers to have compared the eccentric exercise model with the addition of a night splint; a night splint with 0° dorsiflexion was used. In this study, the patients were instructed to increase dorsiflexion as much as they could tolerate. This was done to maximise the hypothesised beneficial effects of splinting. Another difference was the instruction of the eccentric exercises. Roos et al11 used a gradual onset during the first week. In this study, the abrupt loading as described by Alfredson et al8 was used.
What is already known on this topic
Eccentric training is effective in pain reduction in the treatment of Achilles tendinopathy. The magnitude of the effect is uncertain
The use of a night splint has been previously studied with differing outcomes and the studies did not use validated methods of assessing outcome specifically in Achilles tendinopathy.
What this study adds
The use of a night splint is of no added value in treating Achilles tendinopathy when used in addition to eccentric exercises.
The magnitude of effect on pain after an eccentric exercise programme was found to be less than recently reported in a systematic review.
Reported patient compliance for the eccentric exercises was excellent or good in the majority of the patients in both treatment groups, although it should be mentioned that still more than a quarter of the patients in both groups reported performing the exercises at <50% of the prescribed intensity. Of the nine studies in the recent systematic review of Kingma et al,13 only Roos et al11 report the compliance rate in their findings. In their study, a good compliance (75% of the recommended exercises) for eccentric exercises in the first weeks was reported. At 12 weeks, however, only half still reported a good compliance. Compliance for the night splint was good for most of the study period.
Roos et al11 did not calculate the association between outcome and compliance. To our knowledge, there are no other studies in which this relationship is described. In both treatment groups, there was a tendency that a better patient compliance for eccentric exercises lead to better results (table 2). However, the differences were not statistically significant. A possible way to increase patient compliance in future studies can probably be through more frequent patient contact by telephone or email.
Although we strictly adhered to our inclusion criteria, we cannot exclude the occurrence of selection bias. We used a checklist for objective inclusion and exclusion of patients, and we always discussed with several clinicians when there was doubt whether a patient could be included.
The researcher gave minimal assistance to patients on the first occasion they completed the VISA‐A questionnaire. Robinson et al19 also always administered the questionnaire once with an investigator and stated that this would avoid some but not all potential for observer bias.
Conclusion
In this study, eccentric exercises and eccentric exercises in combination with a night splint reduced pain and improved functional outcome in patients with Achilles tendinopathy. The results on pain reduction are less promising than previously reported. Further trials including functional outcome measures are necessary to evaluate the effect of eccentric exercises. It can be stated that a night splint in addition to eccentric exercises is not beneficial at short‐term follow‐up. There was a tendency that higher reported patient compliance for eccentric exercises was correlated with a higher patient satisfaction. Outcome in patients with a shorter duration of the symptoms (<5.5 months) was significantly better than in patients with longer duration of symptoms.
Acknowledgements
We are grateful for the help and advice of S Willemsen (Biostatistics, Erasmus Medical Centre, Rotterdam, The Netherlands) in the statistical evaluation of the data.
Abbreviations
VISA‐A - Victorian Institute of Sport Assessment–Achilles questionnaire
Footnotes
Competing interests: None declared.
Informed consent was obtained for publication of all photographs in this paper.
References
- 1.Maffulli N, Wong J, Almekinders L C. Types and epidemiology of tendinopathy. Clin Sports Med 200322675–692. [DOI] [PubMed] [Google Scholar]
- 2.Schepsis A A, Jones H, Haas A L. Achilles tendon disorders in athletes. Am J Sports Med 200230287–305. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N, Khan K M, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy 199814840–843. [DOI] [PubMed] [Google Scholar]
- 4.Vora A M, Myerson M S, Oliva F.et al Tendinopathy of the main body of the Achilles tendon. Foot Ankle Clin 200510293–308. [DOI] [PubMed] [Google Scholar]
- 5.Alfredson H. Conservative management of achilles tendinopathy: new ideas. Foot Ankle Clin 200510321–329. [DOI] [PubMed] [Google Scholar]
- 6.Kader D, Saxena A, Movin T.et al Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med 200236239–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maffulli N, Sharma P, Luscombe K L. Achilles tendinopathy: aetiology and management. J R Soc Med 200497472–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alfredson H, Pietila T, Jonsson P.et al Heavy‐load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 199826360–366. [DOI] [PubMed] [Google Scholar]
- 9.Mafi N, Lorentzon R, Alfredson H. Superior short‐term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc 2001942–47. [DOI] [PubMed] [Google Scholar]
- 10.Fahlstrom M, Jonsson P, Lorentzon R.et al Chronic Achilles tendon pain treated with eccentric calf‐muscle training. Knee Surg Sports Traumatol Arthrosc 200311327–333. [DOI] [PubMed] [Google Scholar]
- 11.Roos E M, Engstrom M, Lagerquist A.et al Clinical improvement after 6 weeks of eccentric exercise in patients with mid‐portion Achilles tendinopathy—a randomized trial with 1‐year follow‐up. Scand J Med Sci Sports 200414286–295. [DOI] [PubMed] [Google Scholar]
- 12.Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up [Discussion 11]. Br J Sports Med 2004388–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kingma J J, de Knikker R, Wittink H W.et al Eccentric overload training in patients with a chronic Achilles tedinopathy: a systematic review. Br J Sports Med 200741e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med 200322727–741. [DOI] [PubMed] [Google Scholar]
- 15.Wapner K L, Sharkey P F. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle 199112135–137. [DOI] [PubMed] [Google Scholar]
- 16.Batt M E, Tanji J L, Skattum N. Plantar fasciitis: a prospective randomized clinical trial of the tension night splint. Clin J Sport Med 19966158–162. [PubMed] [Google Scholar]
- 17.Powell M, Post W R, Keener J.et al Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int 19981910–18. [DOI] [PubMed] [Google Scholar]
- 18.Dijkstra H J W, Van Enst G C. The therapeutic value of a G‐brace in the management of chronic achilles tendinosis: a pilot study. Geneeskunde en Sport 200336137–140. [Google Scholar]
- 19.Robinson J M, Cook J L, Purdam C.et al The VISA‐A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med 200135335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sayana M K, Maffulli N. Eccentric calf muscle training in non‐athletic patients with Achilles tendinopathy. J Sci Med Sport 20071052–58. [DOI] [PubMed] [Google Scholar]
- 21.Brown R, Orchard J, Kinchington M.et al Aprotinin in the management of Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 200640275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]