Abstract
Objective
To compare the efficacy and safety of two eccentric rehabilitation protocols for patients with symptomatic patellar tendinopathy. A new eccentric overload training device was compared with the present standard eccentric rehabilitation programme on a decline board.
Design
Prospective, randomised clinical trial.
Setting
Sports rehabilitation clinic, university sports laboratory, supplemented with home exercises.
Patients
20 competitive and recreational athletes, all with clinical diagnosis of patellar tendinopathy, verified by MRI or ultrasound imaging.
Interventions
A 12‐week rehabilitation period, either with bilateral eccentric overload strength training using the Bromsman device twice a week or with unilateral eccentric body load training using a decline board twice a week, supplemented with daily home exercises.
Outcome measures
The primary outcome was pain and function, assessed by the Swedish Victorian Institute of Sport Assessment for Patella (VISA‐P) score. Secondary outcome measures were isokinetic muscle torque, dynamic function and muscle flexibility, as well as pain level estimations using visual analogue scale (VAS). Side effects were registered.
Results
Both treatment groups improved in the short term according to the VISA‐P scores during the 12‐week rehabilitation period. However, there were no significant differences between the groups in terms of pain and function. After a 3‐month rehabilitation period, most patients could be regarded as improved enough to be able to return to training and sports. No serious side effects were detected in either group.
Conclusion
In patients with patellar tendinopathy pain, two‐legged eccentric overload training twice per week, using the new device (Bromsman), was as efficient and safe as the present standard daily eccentric one‐legged rehabilitation‐training regimen using a decline board.
Proximal patellar tendon pain (patellar tendinopathy) occurs typically in sports characterised by high demands on force and power of the leg extensor muscles, such as basketball, volleyball, tennis and soccer. Controlled eccentric strengthening of the muscle–tendon complexes involved seems to be important for successful rehabilitation.1,2,3,4,5 Eccentric squat training on a decline board has been shown to have a superior therapeutic effect in reduction of pain compared with squatting on a flat surface.6 One‐legged squatting, using the decline board, resulted in encouraging results with, for example, earlier return to a functional level of sport.7,8 By contrast, Visnes et al9 showed no significant improvements of eccentric training on patellar tendinopathy among volleyball players when instituted during the playing season.
Previous research suggests that the efficacy of eccentric squatting rehabilitation may be correlated with the load applied to the quadriceps muscle. The aim of the present prospective randomised short‐term study was to evaluate and compare clinical outcomes in terms of knee pain and function after eccentric training, using either a novel eccentric overload training device (Bromsman, Lidingö, Sweden)10 or the current standard programme of one‐leg squatting exercises.11
Methods
The study design was a prospective randomised clinical trial with a 12‐week intervention and evaluation of either eccentric overload training using the Bromsman device (group I)10 or one‐legged eccentric quadriceps training using a 25° decline board (group II), as originally described by Stanish and Curwin.11
Patients and design
By contacting our colleague physicians and physiotherapists, we recruited 20 athletes (16 men, 4 women; table 1), all of whom had the clinical diagnosis of patellar tendinopathy. To be included in the study, the athletes had to present a characteristic history of patellar tendinopathy continuously for at least 3 months, or recurrent for at least 6 months, and with a verification of patellar tendinosis12 using either MRI or ultrasonography (US). Exclusion criteria were a history of a local corticosteroid injection during the past 3 months, previous anterior cruciate ligament injury or reconstruction, diabetes, chronic inflammatory or rheumatic joint disease, or back pain during the past 3 months. The Ethical Committee at the Karolinska Institutet, Stockholm, Sweden (no 00‐103), approved the study and the participants provided a written consent. The patients were allocated to either of the two treatment groups by random draw of a sealed, opaque envelope that contained the group assignment. All patients were examined, trained and tested by the principal investigator (AF), except for the range of motion examinations, which were assessed by two other physiotherapists.
Table 1 Baseline patient data for both treatment groups.
| Group I Eccentric overload training (n = 11) | Group II One‐legged standard eccentric training (n = 9) | |
|---|---|---|
| Age | 26 (±8) | 28 (±8) |
| Body weight (kg) | 78 (±9) | 78 (±5) |
| Length (cm) | 178 (±5) | 179 (±9) |
| BMI | 24.5 (±1.9) | 24.1 (±3.7) |
| Female/male ratio | 2/9 | 2/7 |
| Competitive/recreational athlete | 10/1 | 7/2 |
BMI, body mass index.
The values are given as mean (±SD).
Outcome measures
The Victorian Institute of Sports Assessment for Patella (VISA‐P) score,13 linguistically and culturally adapted into Swedish,14 was used as the primary outcome. The instrument consists of eight questions assessing pain, function and ability to participate in sports, confirmed to be valid and reliable for patients with patellar tendinopathy.13 The patients were instructed to complete a VISA‐P questionnaire every week.
For secondary outcome, isokinetic strength testing (IST) and dynamic function were performed, with a gap of 2 days between them in order to avoid muscle fatigue. The patients performed these tests at two occasions: at baseline (week 0) and at the end of the training period (ie, after 12 weeks). Before the IST and functional tests (see below), the patients warmed up for 15 min using a stationary bicycle (Monark Ergomedic 828 E, Varberg, Sweden). During the tests, they were given standardised instructions and oral encouragement.
Isokinetic strength tests
The isokinetic testing was performed using a Biodex dynamometer (Biodex Multi‐Joint System 2, Biodex Medical System, New York, USA). To evaluate repetitive strength, the test protocol included five maximal concentric quadriceps/hamstring contractions at 90°/s. A single series was tested, and the highest peak torque of the series was used for data analysis. All subjects were familiarised with the test procedure. The subjects were seated with an angle of 110° between the back support and the seat. The upper thigh was strapped onto the chair, while the lower thigh was strapped to the padded lever arm of a dynamometer. The non‐tested leg was hanging freely, and the upper body was secured and fastened with two diagonal straps and one horizontal strap over the trunk. The palpated centre at the knee joint was aligned with the axis of rotation of the lever arm.
Functional tests
Functional tests were performed to evaluate functional jumping performance.
1. Five‐repetition counter movement jumps (CMJ × 5): The starting position for CMJ × 5 was upright, with the arms extended towards the ceiling. At the sudden knee bending to approximately 90° of knee flexion followed by a maximal vertical jump, the swinging arms were used to help the jumping movements.15 The vertical jump tests were measured using a timer‐equipped infrared contact mat (IVAR IR‐Matta, LN Sport Konsult HB, Habo, Sweden). The time that the patients were in the air was measured with a precision of 0.001 s, which was converted to jump height.16 The set of five repetitions was performed three times, and the mean value of the best result in each of the three trials was registered.
2. One‐leg triple hop test: Allowing free arm swinging through the movement, the subjects were instructed to jump three repetitive long jumps straight forward as far as possible, using and landing on the same foot.17 The landing had to be steady for at least 2 s on the landing foot. The distance from the toe at the push‐off to the heel mark in the landing was measured, and the best of three technically approved jumps was used. The legs were tested alternatively, always with the uninjured leg tested first, and the best value of three trials was registered.
Visual analogue scale
At both testing sessions (0 and 12 weeks), as well as during all training sessions, the visual analogue scale (VAS) was used for the estimations of pain, where 0 is equal to no pain and 10 the worst pain imaginable.18 After each set of strength training during all training sessions, the patients were repeatedly asked to estimate their tendinopathy pain on the VAS. Using the pain‐handling model during rehabilitation exercises as described by Thomeé,19 they were instructed to squat at a lower load if they experienced pain at VAS >5.
Safety
Considering the risk of worsening the tendon injury, by significantly adding eccentric load (group I) to an abnormal tendon, the safety of the rehabilitation protocols were followed by recording any side effects (numbers of interrupted training session because of pain, suspicions of worsening the tendinopathy, back or hip pain and head ache).
Exercise protocols
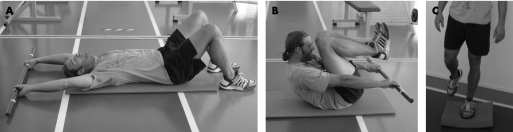
Supervised eccentric training was performed in both groups twice weekly, starting with a standardised warm‐up on a stationary bicycle for 15 min at 100 W. Each rehabilitation session included eccentric strength training (group I or II, as below), alternated with trunk and foot stability training (fig 1). The trunk training consisted of 3×15 sit‐up movements, and the foot stability exercises consisted of one‐legged stance at 3×1 min on each leg.
Figure 1 (A–C) Trunk and ankle stability exercises. Informed consent was obtained for publication of this figure.
This implied an active rest of 4 min between each eccentric strength series. Each training session lasted for about 70 min, and was rounded off with standardised stretching of the quadriceps and hamstring muscles, complemented with an ice pack over the painful patellar tendon for 20 min. All patients ceased participating in sports and other training activities for the first 6 weeks. During the last 6 weeks of the intervention, participants slowly resumed supervised jogging and plyometric jump training, guided by Thomeé's pain‐monitoring model,19 in order to keep pain <5 on the 10‐point scale.
Eccentric overload training group in Bromsman (group I)
The Bromsman eccentric overload training device (fig 2) consists of a barbell (320 kg) suspended from wires that can be moved up and down along a chosen distance and at a preset speed, by a hydraulic machine.10
Figure 2 Squat training in the Bromsman device (group I). Informed consent was obtained for publication of this figure.
The descending distance was individually set from a standing straight position to approximately 110° of knee flexion, and the speed was set to 0.11 m/s. Two industrial scales were used to register the vertical force under each foot, and the patients were given real‐time feedback of the forces by means of two bar graphs on a computer monitor. Another computer monitor facing the physiotherapist displayed time series of forces, which were recorded. The patients resisted the movement of the barbell using both legs during 4 sets × 4 repetitions, where the first set was for warm up and the remaining three for maximal effort. During the ascending phase, the patients followed the barbell without resisting the movement. Pain was assessed after each set using VAS.
One‐legged eccentric training according to Curwin (group II)
One‐legged eccentric training according to Curwin7,11 was carried out on a 25° decline board, with 3 sets×15 reps of unilateral squats on the injured leg, holding an extra weight in front of the chest (fig 3).
Figure 3 One‐legged squat training on a decline board (group II). Informed consent was obtained for publication of this figure.
Both legs were used during the ascending phase. At the start of the treatment no extra weights were added. At each following training session, the patients initially performed a set of 15 reps with the same weight as the previous time. The pain‐monitoring model19 was also used during the home training programme (group II, 3 sets×15 reps/day), and the extra load increase was accomplished by adding weights in a backpack or in their hands. If the VAS score was <3 for a set, the load was increased in 5 kg increments, and if VAS exceeded 5, the load was reduced.
The principal investigator (AF) supervised all the training sessions for all patients in both groups at the clinic.
Statistical analysis
Results were analysed using a three‐way analysis of variance, with group (I and II) as the between‐subjects factor, and time (before and after treatment) and side (affected leg and unaffected leg) as the within‐subjects factors. When an interaction was significant, simple main effects tests were performed—that is, effects of one factor, holding the other factor fixed. Due to the data level, the VISA‐P measurements were analysed by a generalised estimating equations (GEE) model with the GENMOD procedure in SASV.7.1. The GEE strategy is a useful approach for repeated measurements analysis of ordered categorical outcomes. The VISA‐P measurements were categorised into four categories: 0–50, >50–65, >65–75 and >75–100. This ordinal response ranged from 1 to 4, and was then analysed with a proportional odds model for repeated measurements with the GEE method. The model was set up with the within factor, time (0, 3, 6, 9 and 12 weeks), and the between factor, group (I and II). The group × time interaction refers to the statistical test of whether the response profile for one treatment group is the same as for the other group. Fisher's exact test was used to compare the two groups regarding the dichotomised VISA‐P score, ⩽75 and >75 (healthy), and the Sign test was used to analyse the effect within methods for the VAS measurements; p<0.05 was considered significant.20,21
Results
All 20 subjects completed the 12‐week intervention. There were no significant differences between the baseline characteristics of the groups (table 1).
Outcomes
Victorian Institute of Sport Assessment for Patella
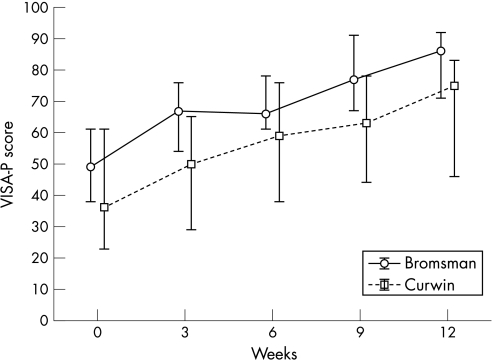
Both groups improved significantly during the treatment period of 12 weeks (p<0.001 for each group). Group I increased from a median of 49 (95% CI 38 to 61) to 86 (95% CI 71 to 92) points, whereas group II increased from a median of 36 (95% CI 23 to 61) to 75 (95% CI 46 to 83) points (fig 4). There were no significant differences between the study groups (fig 4) at any time during the treatment.
Figure 4 The Victorian Institute of Sport Assessment for Patella (VISA‐P) score development for the patients in the two groups of eccentric rehabilitation programmes: group I (eccentric overload training on Bromsman, n = 11) and group II (one‐legged standard eccentric training according to Curwin, n = 9). The median values (95% CI) are plotted.
Isokinetic strength testing
At 90°/s, there were no significant differences between the treatment groups (table 2). At baseline, the symptomatic leg in both groups was weaker than the asymptomatic one (F(1,16) = 6.92; p = 0.018). There was a significant increase in extensor torque after treatment for both legs in both groups (F(1,16) = 7.10; p = 0.017).
Table 2 Secondary outcome measures at baseline and after 12 weeks.
| Knee | Group I eccentric overload training (n = 11) | Group II one legged standard eccentric training (n = 9) | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 weeks | 12 weeks | Within group statistics | 0 weeks | 12 weeks | Within group statistics | Between group statistics | ||
| Isokinetic koncentric knee extension | ||||||||
| 90°/s (Nm) | Uninjured | 217 (181 to 253) | 219 (186 to 252) | p = 0.018 between legs, p = 0.017 with time | 197 (156 to 237) | 204 (167 to 241) | p = 0.018 between legs, p = 0.017 with time | NS |
| Injured | 185 (154 to 217) | 206 (173 to 239) | 178 (143 to 213) | 190 (152 to 227) | ||||
| Functional tests | ||||||||
| CMJ × 5 bilateral (cm) | 42 (38 to 46) | 43 (38 to 48) | NS | 35 (30 to 39) | 34 (29 to 40) | NS | p = 0.018 at both times | |
| One‐leg triple jump (cm) | Uninjured | 548 (501 to 596) | 582 (536 to 628) | p<0.001 for time | 505 (452 to 558) | 527 (476 to 578) | p<0.001 for time | NS |
| Injured | 555 (502 to 607) | 585 (531 to 638) | 496 (438 to 554) | 531 (471 to 590) | ||||
CMJ, counter movement jumps.
The results are expressed as mean (95% CI) values for the groups.
Functional tests
The time × group interaction was not significant in any of the functional tests (below).
1. Bilateral CMJ (× 5): Group I jumped higher at the start of the treatment (F(1,18) = 6.74; p = 0.018), as well as at the 12 week follow‐up, but this did not change over time (table 2).
2. One‐leg triple hop: Both groups improved over time (F(1,18) = 16.7; p<0.001), but there were no differences between the legs (F(1,18)<1; p = 0.90; table 2).
Visual analogue scale
Both groups showed a lower VAS after 12 weeks of treatment. Group I scored median 4 (Q25–Q75 4–6) at baseline and median 0 (Q25–Q75 0–1; p = 0.003) after 12 weeks. Group II decreased from VAS median 5 (Q25–Q75 4–5) at baseline to median 1 (Q25–Q75 1–2; p = 0.008) after 12 weeks.
Safety
At no training occasion, in either group, was the strength training at the clinic stopped due to unacceptable pain (VAS>5), or suspicions of any worsened injury. Also, neither incidents of sudden back or hip pain nor headaches were registered (data not shown).
Discussion
The present study showed that the knee function in athletes with patellar tendinopathy after 3 months was increased similarly after overload eccentric training in the Bromsman device as after eccentric training on the decline board. In a recent study, where eccentric squat training was compared with surgical intervention,22 a reduction of knee pain and an improvement in knee function, with an increase of the VISA‐P score from approximately 30 to 50 points, was observed for the eccentric treatment group after 12 weeks. This magnitude of improvement is in agreement with our results. Furthermore, Young et al8 observed a similar improvement in VISA‐P score from approximately 62 to 78 during a 12‐week period of eccentric treatment. Interestingly, the improvement in VISA‐P score is similar for all three studies, even though the baseline mean scores differ substantially. Considering a VISA‐P score of >75 points as non‐symptomatic,14 9 of 11 (82%) patients in group I and 4 of 9 (44%) patients in group II may be considered subjectively free of symptoms at the end point of the study at 12 weeks (p = 0.16). However, the long‐term outcome and possible recurrence rates are not yet available in our study.
What is already known on this topic
Eccentric training could be the primary treatment for patients with patellar tendinopathy, either on a decline board or with heavy eccentric resistance.
What this study adds
There is no risk of worsening an injured tendon with eccentric overload training under controlled circumstances.
The isokinetic strength tests illustrated that the injured leg was weaker at baseline. At 90°/s, both groups increased their quadriceps muscle torque after the treatment period (group I 9% in uninjured leg and 11% in injured leg; group II: 4% in uninjured leg and 7% in injured leg). Bahr et al22 observed strength improvements of similar magnitude at 6 months from start following a 12‐week period of eccentric treatment of patellar tendinopathy.
Among the jump tests, only the results of one‐leg triple jump showed improvements (group I: 6% in uninjured leg and 5% in injured leg; group II: 4% in uninjured leg and 7% in injured leg). This improvement may reflect the ankle stability training (see above) in both rehabilitation protocols, since the triple jump most likely puts higher demands on ankle stability and balance than, for example, the vertical jump test. The lack of improvement in the other jump test is also in agreement with the findings of Bahr et al.22
Considering the number of weekly maximal eccentric descents (24 two‐legged in group I, and 315 one‐legged in group II), and the total weekly mean load on the patellar tendon due to the eccentric training during both treatments, the weekly load in group II was approximately 10 times higher than in group I (group I ≈110 kN and group II ≈1130 kN). Despite this, both groups apparently improved equally, and hence the dosage of maximal eccentric challenge on the tendon may be quite different but may still produce similar subjective improvements. Also, the long‐term effect of exercise loading on tendons seems to be positive.23 Thus, the optimal dose of eccentric load required to decrease pain in rehabilitation of tendinopathy, when using eccentric exercises, remains unclear.24
The overload eccentric training descending phase in the Bromsman device (group I) resulted in higher peak force in the symptomatic injured patellar tendon when compared with the decline board. This may imply a risk of possible side effects, such as worsened tendon injury. Our attention during the study was directed towards worsening of the patellar tendinopathy in terms of pain with a theoretical possibility of partial or total ruptures, but also back and hip pain, or headaches. However, neither our own earlier clinical experience nor the present study has shown any such, or other, side effects. On the other hand, it has been asked whether it is the specific overload that may heal the injury. One explanation for the safety of this overload device may be that the maximal eccentric descent is two‐legged and thereby possibly better patient‐controlled. The pain‐monitoring model19 used in both groups of this study apparently seems to be a good method of controlling pain and thus guiding the eccentric rehabilitation exercises. Thus, we may conclude that the use of the new overload training device (Bromsman) seems to be safe and effective for rehabilitation of patients with patellar tendinopathy.
Even if eccentric muscle–tendon rehabilitation exercise remains one of the cornerstones in treatment of tendinopathies,19 a few novel treatment regimens for tendinopathies have been suggested recently. Alfredson and Öhberg have described a treatment regimen with sclerosing injections into the chronically hypervascular areas around a tendinopathy, which is apparently most successful for the mid‐portion Achilles tendinopathy,25 but is also promising for tendinopathies at the elbow26 and the knee.27 However, the latter study as well as a recent study comparing surgical treatment with eccentric training,22 showed short‐term (<3 months) improvements in the VISA‐P score at a similar pace as in the present study. Therefore, at present, eccentric exercise rehabilitation can be regarded as successful as different surgery techniques for short‐term outcome. We therefore agree with both Alfredson and Öhberg25 and Bahr et al22 that the need for surgery for patellar tendinopathy currently may be challenged. It therefore seems reasonable to recommend eccentric training before surgery is considered.
This study has shown successful results with both eccentric rehabilitation protocols. However, the outcome is short term (3 months), and long‐term results of return to preinjury levels of sport and activity, as well as possible recurrences, still have to be reported. The small sample sizes in each group limit the conclusions that can be drawn using heavy, overload eccentric training in the present or future experimental training equipment compared with body load. Therefore, the present investigations may be considered as an initial study to get more answers concerning the optimal treatment for patellar tendinopathy.
Acknowledgements
The extensive help from the statistical consultant, Mrs Elisabeth Berg, PhD (LIME, Karolinska Institutet, Stockholm, Sweden), is highly acknowledged. We also thank the Swedish Sports Research Council (CIF) for giving grants to support this project.
Abbreviations
CMJ - counter movement jumps
GEE - generalised estimating equations
IST - isokinetic strength testing
VAS - visual analogue scale
VISA‐P - Victorian Institute of Sport Assessment for Patella
US - ultrasonography
Footnotes
Competing interests: None.
Written consent was obtained from patients to publish their photos in this study.
References
- 1.Peers K H, Lysens R J. Patellar tendinopathy in athletes: current diagnostic and therapeutic recommendations. Sports Med 20053571–87. [DOI] [PubMed] [Google Scholar]
- 2.Lian O B, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross‐sectional study. Am J Sports Med 200533561–567. [DOI] [PubMed] [Google Scholar]
- 3.Blazina M E, Kerlan R K, Jobe F W.et al Jumper's knee. Orthop Clin North Am 19734665–678. [PubMed] [Google Scholar]
- 4.Jensen K, Di Fabio R P. Evaluation of eccentric exercise in treatment of patellar tendinitis. Phys Ther 198969211–216. [DOI] [PubMed] [Google Scholar]
- 5.Stanish W D, Rubinovich R M, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop 198620865–68. [PubMed] [Google Scholar]
- 6.Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: a prospective randomised study. Br J Sports Med 200539847–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Purdam C R, Jonsson P, Alfredson H.et al A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med 200438395–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young M A, Cook J L, Purdam C R.et al Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med 200539102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Visnes H, Hoksrud A, Cook J.et al No effect of eccentric training on jumper's knee in volleyball players during the competitive season: a randomized clinical trial. Clin J Sport Med 200515227–234. [DOI] [PubMed] [Google Scholar]
- 10.Frohm A, Halvorsen K, Thorstensson A. A new device for controlled eccentric overloading in training and rehabilitation. Eur J Appl Physiol 200594168–174. [DOI] [PubMed] [Google Scholar]
- 11.Stanish W D, Curwin S.Tendinitis: its etiology and treatment. Oxford, UK: Pergamon Press, 1984
- 12.Khan K M, Visentini P J, Kiss Z S.et al Correlation of ultrasound and magnetic resonance imaging with clinical outcome after patellar tenotomy: prospective and retrospective studies. Victorian Institute of Sport Tendon Study Group. Clin J Sport Med 19999129–137. [DOI] [PubMed] [Google Scholar]
- 13.Visentini P J, Khan K M, Cook J L.et al The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport 1998122–28. [DOI] [PubMed] [Google Scholar]
- 14.Frohm A, Saartok T, Edman G.et al Psychometric properties of a Swedish translation of the VISA–P outcome score for patellar tendinopathy. BMC Musculoskel Disord 2004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komi P V, Bosco C. Utilization of stored elastic energy in leg extensor muscles by men and women. Med Sci Sports 197810261–265. [PubMed] [Google Scholar]
- 16.Anderson F C, Pandy M G. Storage and utilization of elastic strain energy during jumping. J Biomech 1993261413–1427. [DOI] [PubMed] [Google Scholar]
- 17.Noyes F R, Barber S D, Mangine R E. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med 199119513–518. [DOI] [PubMed] [Google Scholar]
- 18.Price D D, McGrath P A, Rafii A.et al The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 19831745–56. [DOI] [PubMed] [Google Scholar]
- 19.Thomeé R. A comprehensive treatment approach for patellofemoral pain syndrome in young women. Phys Ther 1997771690–1703. [DOI] [PubMed] [Google Scholar]
- 20.Roger E.Experimental design: procedures for the behavioral sciences. Pacific Grove, USA: Brooks/Cole Publishing Company, 1995
- 21.Stokes M E, Davis C S, Koch G G.Categorical data analysis using the SAS system. 2nd edn. Cary, NC: SAS Institute, 2000
- 22.Bahr R, Fossan B, Loken S.et al Surgical treatment compared with eccentric training for patellar tendinopathy (Jumper's knee). A randomized, controlled trial. J Bone Joint Surg Am 2006881689–1698. [DOI] [PubMed] [Google Scholar]
- 23.Archambault J M, Wiley J P, Bray R C. Exercise loading of tendons and the development of overuse injuries. A review of current literature. Sports Med 19952077–89. [DOI] [PubMed] [Google Scholar]
- 24.Wang J H, Iosifidis M I, Fu F H. Biomechanical basis for tendinopathy. Clin Orthop Relat Res 2006443320–332. [DOI] [PubMed] [Google Scholar]
- 25.Alfredson H, Öhberg L. Sclerosing injections to areas of neo‐vascularisation reduce pain in chronic Achilles tendinopathy: a double‐blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 200513338–344. [DOI] [PubMed] [Google Scholar]
- 26.Zeisig E, Öhberg L, Alfredson H. Sclerosing polidocanol injections in chronic painful tennis elbow‐promising results in a pilot study. Knee Surg Sports Traumatol Arthrosc 2006141218–1224. [DOI] [PubMed] [Google Scholar]
- 27.Hoksrud A, Öhberg L, Alfredson H.et al Ultrasound‐guided sclerosis of neovessels in painful chronic patellar tendinopathy: a randomized controlled trial. Am J Sports Med 2006342013–2021. [DOI] [PubMed] [Google Scholar]