Abstract
Background
Chronic ankle instability (CAI) is a common orthopaedic entity in sport. Although other risk factors have been studied extensively, little is known about how it is influenced by the osseous joint configuration.
Aim
To study the effect of osseous ankle configuration on CAI.
Design
Case–control study, level III.
Setting
Radiological examination with measurement of lateral x rays by an independent radiologist using a digital DICOM/PACS system.
Patients
A group of 52 patients who had had at least three recurrent sprains was compared with an age‐matched and sex‐matched control group of 52 healthy subjects.
Main outcome measures
The radius of the talar surface, the tibial coverage of the talus (tibiotalar sector) and the height of the talar body were measured.
Results
The talar radius was found to be larger in patients with CAI (21.2 (2.4) mm) than in controls (17.7 (1.9) mm; p<0.001, power >95%). The tibiotalar sector, representing the tibial coverage of the talus, was smaller in patients with CAI (80° (5.1°)) than in controls (88.4° (7.2°); p<0.001, power >95%). No significant difference was observed in the height of the talar body between patients with CAI (28.8 (2.6) mm) and controls (27.5 (4.0) mm; p = 0.055).
Conclusion
CAI is associated with an unstable osseous joint configuration characterised by a larger radius of the talus and a smaller tibiotalar sector. There is evidence that a higher talus might also play some part, particularly in women.
Ankle ligament injuries are the most common injuries in sport and recreational activities.1 The anterior talar‐fibular ligament is affected in 85% of ankle sprains.2,3,4 This type of injury represents a sprain with a major component in the sagittal plane.5,6 This kind of injury is therefore best investigated using lateral views of the ankle, where the osseous containment of the talus in the tibia can be assessed. Although most of these ligamentous ankle injuries can be successfully treated with physical rehabilitation and non‐operative treatment, 20–40% of patients with ankle injuries develop chronic ankle instability (CAI) and experience recurrent sprains.7,8,9,10 Many of these patients with CAI can be satisfactorily treated with reconstruction of the injured ligaments.3,11,12,13,14,15,16 However, good results of surgery and physical rehabilitation notwithstanding, some patients keep experiencing persistent symptomatic ankle instability10,17 and have the propensity to develop post‐traumatic ligamentous ankle osteoarthritis.18
The risk of spraining an ankle depends on both intrinsic factors (hindfoot alignment, ligament laxity, muscular force, neuromuscular control and so on) and extrinsic factors (shoes worn, type and intensity of sport, warm up and so on).19,20,21 The shoulder, a rather unstable joint, is characterised by a humeral head that is large compared with the glenoid, whereas in the hip, a stable joint, the femoral head and the acetabulum are of equal size. This suggests that there is a relationship between joint stability and osseous joint configuration, but to date, the effect of the osseous configuration on the predisposition to develop CAI has not been investigated.
The current study examines whether the osseous joint configuration of the ankle joint plays a role in the development of CAI. The hypotheses of this study were that (a) a flat talus, characterised in terms of a large radius, contributes to CAI; (b) a lack of restraint of the talus in the tibia, characterised in terms of a small tibiotalar coverage, contributes to CAI; and (c) a higher talar body with consequently more torque forces contributes to CAI.
Methods
Study design
This study is a comparative case–control study of patients with symptomatic CAI and healthy controls with a stable and normal ankle. The study was approved by the Medical Sciences Ethical Review Board, University of Basel, Basel, Switzerland, and the subjects gave informed consent to participate in the study. The study was carried out in accordance with the World Medical Association Declaration of Helsinki.
Inclusion/exclusion criteria for patients with CAI
The inclusion criteria for patients with CAI were that they had had at least three recurrent ankle sprains, with symptomatic instability requiring surgical ligament reconstruction. Patients were excluded if they had experienced trauma to the lower extremity, had previously had foot surgery, had hindfoot deformity or ankle osteoarthritis, posterior tibial dysfunction, limited dorsiflexion (<10°), neurological disorders, or any other systemic disease such as rheumatoid arthritis or diabetes.
During the course of the study, a total of 80 patients were assessed, 17 of whom were excluded because they did not meet the selection criteria. Of the remaining patients, 11 had to be excluded because their lateral x ray was not taken strictly laterally (see radiological criteria below), which made it impossible to measure the relevant parameters with the required accuracy. This resulted in a final group of 52 patients with CAI meeting the selection criteria (18 men and 34 women, mean (SD) age 39 (13.9) years; table 1).
Table 1 Subject groups.
| Patients with CAI | Controls | |
|---|---|---|
| Number of subjects | 52 | 52 |
| Sex (male:female) | 18:34 | 18:34 |
| Mean (SD, range) age (years) | 39 (13.9, 16–66) | 37 (16.5, 16–71) |
CAI, chronic ankle instability.
Inclusion/exclusion criteria for controls
Patients for the control group were recruited from those who were admitted to our emergency department for reasons other than ankle sprains or CAI and had x rays of their ankles taken. The purpose of these x rays was to rule out the possibility of ankle fractures caused by external forces—for example, a car accident, a motorcycle crash, a cycling accident or falling off a wall (n = 86)—or due to direct trauma (n = 6). Patients were excluded if they had one (or more) of the following conditions: acute ankle fracture, acute or previous ankle sprain, any history of ankle instability, previous surgery of the foot, hindfoot deformity, ankle osteoarthritis, posterior tibial dysfunction, systemic disease such as rheumatoid arthritis or diabetes, or neurological disorders. For comparison with the patients with CAI, the control group was matched for age and sex resulting in 52 consecutive controls (18 men and 34 women, mean (SD) age 37 (16.5) years; table 1).
Radiological measurement
A DICOM/PACS application was used to carry out standardised measurements of the ankle joints on digital x rays. All ankle radiographs were taken at the Radiological Department, University of Basel, on a digital flat panel system with flat detector technology (Aristos FX, Siemens Erlangen, Erlangen, Germany). Weight‐bearing standard anterior–posterior and lateral (exposure medially, film laterally) radiographs were taken by focusing the x ray exactly on the centre of the ankle joint. Only strictly lateral views were accepted, which were characterised by superimposition of the lateral and medial malleoli, whereas the distal fibula was projected on to the posterior third of the distal tibia, and exact superimposition of the medial and lateral surfaces of the talus (fig 1). All x rays were analysed by an independent blinded radiologist in a radiology workstation with a high‐resolution monitor using the DICOM/PACS review application E‐Film (Department of Medical Imaging, University Health Network and Mount Sinai Hospital, Toronto, Ontario, Canada). All measurements were carried out in digital zoom without radiological magnification.
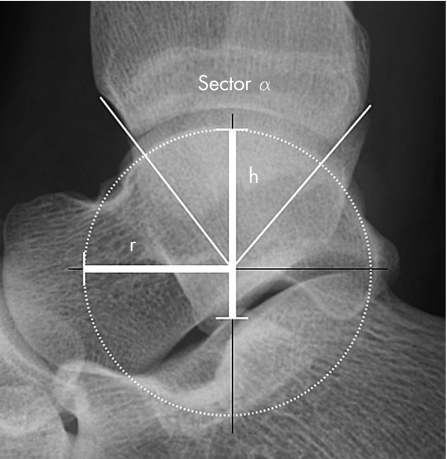
Figure 1 Osseous parameters of the ankle. This x ray shows the radius (r), sector (α) and height (h) of the talus.
The following validated parameters were measured (fig 1)22:
Radius of the talus (r): A circle was digitally fitted to the talar joint surface and then used to determine the centre of the talus. The distance between the centre of the talus and the circle is the radius of the talus (measured in mm).
Tibiotalar sector (α): A line was drawn from the centre of the talus to both the anterior and posterior margins of the distal tibia. These two lines enclose the angle α, which, by definition, is the tibiotalar sector, indicating the size of the tibial coverage of the talus (measured in degrees).
Height of the talus (h): A line was drawn perpendicular to the ground through the centre of the talus. The talar height is defined as the length of the segment of this line between the talar surface and the inferior border of the talus (measured in mm).
Statistical methods and data analysis
Statistical differences among groups were determined by the unpaired Student's t test. Significance was considered at p⩽0.05. All statistical calculations were performed using the STATISTICA statistical package V.6.1. Minimal sample size was calculated using power analysis for a minimal power of 0.95: talar radius r (n = 13), tibiotalar sector α (n = 20) and talar height h (n = 247).
Results
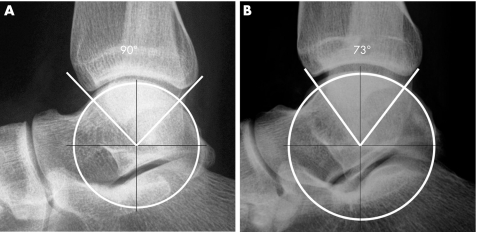
Talar radius
Patients with CAI had a significantly larger talar radius (21.2 (2.4) mm) than controls (17.7 (1.9) mm; p<0.001, power >95%; table 2, fig 2). Separated by sex, men with CAI had a significantly larger talar radius (22.8 (2.3) mm) than men in the control group (18.4 (1.9) mm; p<0.001, power >95%; table 3). Women with CAI had a significantly larger talar radius (20.3 (1.9) mm) than women in the control group (17.3 (2.0) mm; p<0.001, power >95%; table 3).
Table 2 Radiological results.
| Patients with CAI | Controls | p Value (power, %) | |
|---|---|---|---|
| Mean (SD, range) radius (mm) | 21.2 (2.4, 17–26) | 17.7 (1.9, 13–23) | <0.001 (>95) |
| Mean (SD, range) sector (deg) | 80.0 (5.1, 72–95) | 88.4 (7.2, 79–111) | <0.001 (>95) |
| Mean (SD, range) talar height (mm) | 28.8 (2.6, 24–34) | 27.5 (4.0, 20–37) | 0.055 (38) |
CAI, chronic ankle instability.
Figure 2 Lateral x ray of a normal and an unstable ankle joint. Radiographs of (A) a typical stable joint configuration with a larger sector and smaller radius, and (B) a typical unstable configuration with a smaller sector and larger radius.
Table 3 Radiological results dependent on sex.
| Patients with CAI | Controls | p Value (power, %) | |
|---|---|---|---|
| Men (n = 18) | |||
| Mean (SD, range) radius (mm) | 22.8 (2.3, 19–26) | 18.4 (1.9, 15–23) | <0.001 (>95) |
| Mean (SD, range) sector (deg) | 80.3 (6.1, 72–95) | 91.4 (7.2, 81–102) | <0.001 (>95) |
| Mean (SD, range) height (mm) | 30.9 (1.6, 28–34) | 30.3 (3.9, 24–37) | 0.051 (7) |
| Women (n = 34) | |||
| Mean (SD, range) radius (mm) | 20.3 (1.9, 17–25) | 17.3 (2.0, 13–21) | <0.001 (>95) |
| Mean (SD, range) sector (deg) | 79.8 (4.6, 72–93) | 86.8 (6.7, 79–111) | <0.001 (>95) |
| Mean (SD, range) height (mm) | 27.6 (2.2, 24–33) | 26.0 (3.3, 20–33) | 0.02 (53) |
CAI, chronic ankle instability.
Tibiotalar sector
Patients with CAI had a significantly smaller tibiotalar sector (80° (5.11°)) than normal subjects (88.4° (7.2°); p<0.001, power >95%; table 2, fig 2). Separated by sex, men with CAI had a significantly smaller tibiotalar sector (80.3° (6.1°)) than men in the control group (91.4° (7.2°); p<0.001, power >95%; table 3). Women with CAI had a significantly smaller tibiotalar sector (79.8° (4.6°)) than women in the control group (86.8° (6.7°); p<0.001, power >95%; table 3).
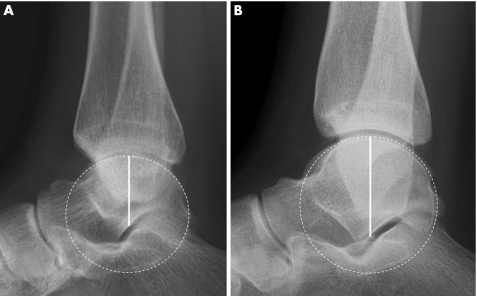
Talar height
Patients with CAI had a higher talus (28.8 (2.6) mm) than controls (27.5 (4.0) mm; p = 0.055; table 2, fig 3), but this difference was not significant. Separated by sex, women with CAI had a significantly higher talus (27.6 (2.2) mm) than women in the control group (26.0 (3.3) mm; p<0.05; table 3). Men with CAI had a higher talus (30.9 (1.6) mm) than men in the control group (30.3 (3.9) mm; p = 0.51; table 3), but this, again, was not significant.
Figure 3 Lateral x rays of the ankle joint with different talar heights. Radiographs of (A) a stable ankle with a flat talus and (B) an unstable ankle with increased height of the talus.
Discussion
This study shows that the stability of the ankle joint could be influenced by its osseous configuration. A larger radius, corresponding to a flatter talus, and a smaller tibiotalar sector, reflecting less restraint of the talus in the tibia, are significantly correlated with CAI and could, therefore, be considered intrinsic risk factors for CAI. Further, there is also evidence that a higher talus plays some part, particularly in women.
What is already known on this topic
The risk of spraining an ankle depends on both intrinsic factors (hindfoot alignment, ligament laxity, muscular force, neuromuscular control, etc) and extrinsic factors (shoes worn, type and intensity of sport, warm up, and so on).
The shoulder, a rather unstable joint, is characterised by a humeral head that is large compared with the glenoid, whereas in the hip, a stable joint, the femoral head and the acetabulum are of equal size.
This suggests that there is a relationship between joint stability and osseous joint configuration, but to date, the effect of the osseous configuration on the predisposition to develop chronic ankle instability has not been investigated.
What this study adds
This study shows that the osseous configuration of the ankle joint contributes to the stability of the joint.
A larger radius, corresponding to a flatter talus, and a smaller tibiotalar sector, reflecting less restraint of the talus in the tibia, are significantly correlated with chronic ankle instability (CAI).
There is also evidence that a higher talus plays some part, particularly in women.
These intrinsic risk factors might help doctors and surgeons dealing with patients with CAI to choose a treatment that is appropriate in each individual case.
The present study could help doctors and surgeons to decide on the appropriate treatment for a particular patient with CAI. Surgical ankle ligament stabilisation might be recommended in patients with an unstable osseous configuration (characterised by a larger radius of the talus and a smaller tibiotalar sector), as such patients have a disposition to recurrent sprains. Such a treatment seems particularly apt in these cases because long‐term ankle instability might lead to post‐traumatic ligamentous ankle instability.18 Further, the osseous configuration might explain why some patients with CAI have recurrent sprains although they have previously undergone surgical ligament repair. We hope that future biomechanical and clinical studies will clearly reveal the possibility of a clinical application for our findings.
Another question in connection with treating patients with CAI is whether osteophytes on the anterior border of the tibia should be removed in the presence of impingement symptoms.23,24 Theoretical considerations suggest such a treatment, in particular in the presence of hypertrophic synovial thickening.25 However, removing the osteophytes, as widely recommended in the orthopaedic literature,23,24 would, in turn, decrease the tibial coverage of the talus and thus dispose the talus to dislocate anteriorly out of the ankle mortise. Such surgery should therefore be performed with caution, particularly in the case of unstable ankles and in patients who have previously experienced ankle sprains. According to this radiological–biomechanical study, cheilectomy in unstable ankles might be better performed on the talus neck than in the anterior tibial border as this leaves the tibial coverage unchanged.
Given that ankle sprains are the most common injury in sport, this study might be of great importance for the prevention of ankle ligament injuries. People engaging in activities with high risk of ankle sprains (eg, basketball, football and soccer) and who have an unstable ankle configuration could be recommended to wear ankle‐protecting sports equipment.26,27 Future prospective studies might analyse this CAI‐preventive aspect in people with such radiological intrinsic risk factors for CAI.
The question arises of whether ankle instability can be adequately assessed using radiographs in a two‐dimensional plane only. The ankle joint is a three‐dimensionally complex joint with wider anterior talus, larger lateral radius, a larger posterior talar radius and a larger tibial radius than talar radius and consists of three bones, which leads to a three‐dimensional movement.5,28,29,30 A total of 85% of ankle sprains affect the anterior talar‐fibular ligament and therefore the ligamentous stability in the sagittal plane.2,3,4 From experimental and mathematical studies, Leardini et al31 have deduced that the human ankle joint can be modelled in the sagittal plane. Approximating the ankle joint as a simple hinge joint is now widely accepted and many models are based on this approximation.5,6 For example, Tochigi et al,32 focusing solely on the sagittal plane, found that anterior or a posterior positioning of the talus in the mortise increases mechanical stress and therefore leads to osteoarthritis or failure of total ankle replacement. LeBrun and Krause33 found that a posterior position of the fibula predisposes to ankle instability. On the basis of these facts, the present study focused on stability in the sagittal plane only to suggest osseous risk factors for CAI.
To eliminate the effect of joint load on ankle stability in the present study, all x rays were taken in a standard weight‐bearing set‐up. Fraser and Ahmed34 studied the passive rotational stability of the loaded ankle and found that the rotation decreased with increasing load. McCullough and Burge35 also found that increasing the axial load decreased the axial rotation in both conditions in an ankle with intact ligaments, as well as after ligament release. Stormont et al,36 in a preloaded model, found that the articular surfaces supplied 30% of the stability in rotation and 100% of the stability in inversion testing.
The present study has certain limitations. First, there were more women than men in the group with CAI. On the basis of this distribution, one could argue that ankle instability is more common in women. This assumption is, in fact, supported by the finding of Hosea et al,37 who showed in a prospective study of 11 780 basketball players that women have a 25% higher risk of ankle sprains. In cross‐country running, the incidence of sprains was higher for women (2.2/1000 h of sport) than for men (0.7/1000 h of sport).38 Women are also more likely to have hypermobility, which is associated with an increased prevalence of sports injuries.39
Second, one may suspect that the measured values depend on body height. However, Leardini et al5 have found no correlation between the patient's height and anatomical measurements of the ankle joint. In addition, the tibiotalar sector as the main factor determining the osseous ankle stability is not dependent on absolute anatomical values and therefore is independent of the patient's height.
Third, the role of ligaments has been neglected in this study. The motion of the articular surfaces on each other is well guided by the ligaments and the ankle joint stabilised.5 However, in the case of an unstable joint configuration, there will be more stress on the ligaments.
Fourth, the risk of sustaining an ankle sprain might depend on the activity level of the patient. According to Halasi et al40, the activity level is characterised by the type and amount of time spent in sport. The precise activity level of each patient was not recorded, as this was not the aim of this radiological–biomechanical study. However, the two groups were age and sex matched as both these factors might influence activity level.
Conclusions
This study shows that the osseous configuration of the ankle joint contributes to its stability. A larger radius, corresponding to a flatter talus, and a smaller tibiotalar sector, corresponding to less restraint of the talus in the tibia, are significantly correlated with CAI. There is also evidence that a higher talus plays some part, particularly in women. These intrinsic risk factors might help doctors and surgeons dealing with patients with CAI to choose a treatment that is appropriate in each individual case.
Abbreviations
CAI - chronic ankle instability
Footnotes
Competing interests: None declared.
References
- 1.Garrick J G. The frequency of injury mechanism of injury and epidemiology of ankle sprains. Am J Sports Med 19775241–242. [DOI] [PubMed] [Google Scholar]
- 2.Baumhauer J F, Alosa D M, Renstroem P A. A prospective study of ankle injury risk factors. Am J Sports Med 199523564–570. [DOI] [PubMed] [Google Scholar]
- 3.Giza E, Fuller C, Junge A.et al Mechanisms of foot and ankle injuries in soccer. Am J Sports Med 200331550–554. [DOI] [PubMed] [Google Scholar]
- 4.Wright I C, Neptune R R, van den Bogert A J.et al The influence on foot positioning on ankle sprains. J Biomech 200033513–519. [DOI] [PubMed] [Google Scholar]
- 5.Leardini A, O'Connor J J, Catani F.et al Kinematics of the human ankle complex in passive flexion; a single degree of freedom system. J Biomechanics 199932111–118. [DOI] [PubMed] [Google Scholar]
- 6.Stagni R, Leardnini A, Ensini A.et al Ankle morphometry evaluated using a new semi‐automated techinque based on X‐ray pictures. Clin Biomech 200520307–311. [DOI] [PubMed] [Google Scholar]
- 7.Brand R L, Collins M D, Templeton T. Surgical repair of ruptured lateral ankle ligaments. Am J Sports Med 1981940–44. [DOI] [PubMed] [Google Scholar]
- 8.Brostroem L. Sprained ankle V—treatment and prognosis. Acta Chir Scand 1966132537–550. [PubMed] [Google Scholar]
- 9.Freeman M A. Instability of the foot after injuries to the lateral liagment of the ankle. J Bone Joint Surg Br 196547B669–677. [PubMed] [Google Scholar]
- 10.Karlsson J, Bergstern T, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am 198870A581–588. [PubMed] [Google Scholar]
- 11.Brostroem L. Sprained ankles VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand 1966132551–565. [PubMed] [Google Scholar]
- 12.Czaja S, Müller W. Surgical treatment of ankle instability secondary to chronic tear of the lateral ligaments. Orthop Traumatol 19986245–256. [Google Scholar]
- 13.Karlsson J, Eriksson B I, Bergsten T.et al Comparison of two anatomic reconstructions for chronic lateral instability of the ankle joint. Am J Sports Med 19972548–53. [DOI] [PubMed] [Google Scholar]
- 14.Rudert M, Wülker N, Wirth C J. Reconstruction of the lateral ligaments of the ankle using a regional periosteal flap. J Bone Joint Surg Br 199779B446–451. [DOI] [PubMed] [Google Scholar]
- 15.Sammarco G J, DiRaimondo C V. Surgical treatment of lateral ankle instability syndrome. Am J Sports Med 198816501–511. [DOI] [PubMed] [Google Scholar]
- 16.St Pierre R K, Allman F, Bassett F H.et al A review of ankle ligamentous reconstructions. Foot Ankle 19823114–123. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum D, Becker H P, Sterk J.et al Functional evaluation of the 10‐year outcome after modified Evans repair for chronic ankle instability. Foot Ankle Int 199718765–771. [DOI] [PubMed] [Google Scholar]
- 18.Valderrabano V, Hintermann B, Horisberger M.et al Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med 200634612–620. [DOI] [PubMed] [Google Scholar]
- 19.Beynnon B D. Predictive factors for lateral ankle sprains: a literature review. J Athl Train 200237376–380. [PMC free article] [PubMed] [Google Scholar]
- 20.Hartsell H D, Spaulding S J. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med 199933255–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaminski T W, Buckley B D, Powers M E.et al Effect of strenghth and propioception on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br J Sports Med 200337410–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magerkurth O, Knupp M, Ledermann H.et al Evaluation of hindfoot dimensions: a radiological study. Foot Ankle Int 200627612–616. [DOI] [PubMed] [Google Scholar]
- 23.Biedert R. Anterior ankle pain in sport medicine: etiology and indications for arthroscopy. Arch Orthop Trauma Surg 1991110293–297. [DOI] [PubMed] [Google Scholar]
- 24.Van Dijk C N, Tol J L, Verheyen C C. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med 199725737–745. [DOI] [PubMed] [Google Scholar]
- 25.Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 200230402–409. [DOI] [PubMed] [Google Scholar]
- 26.Müller C C, Hintermann B. Die Wirkung von äusseren Stabilisierungshilfen auf die Rotationsinstabilität des Sprunggelenks. Sportverletz Sportschaden 19962084–87. [DOI] [PubMed] [Google Scholar]
- 27.Nigg B M, Nurse M A, Stefanyshyn D J. Shoe inserts and orthotics for sport and physical activities. Med Sci Sports Exerc 199931421–428. [DOI] [PubMed] [Google Scholar]
- 28.Hintermann B, Nigg B M. In vitro kinematics of the axially loaded ankle complex in response to dorsiflexion and plantarflexion. Foot Ankle Int 199516514–518. [DOI] [PubMed] [Google Scholar]
- 29.Lundberg A, Svennson O K, Nemeth G.et al The axis of rotation of the ankle joint. J Bone Joint Surg Br 198971B94–99. [DOI] [PubMed] [Google Scholar]
- 30.Macko V W, Matthews L S, Zwirkoski P. The joint‐contact area of the ankle. J Bone Joint Surg Br 199173347–351. [PubMed] [Google Scholar]
- 31.Leardini A, O'Connor J J, Catani F.et al A geometric model of the human ankle joint. J Biomech 199932585–591. [DOI] [PubMed] [Google Scholar]
- 32.Tochigi Y, Suh J S, Amendola A.et al Ankle alignment on lateral radiographs. Part 2: reliability and validity of measures. Foot Ankle Int 20062788–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LeBrun C T, Krause J O. Variations in mortise anatomy. Am J Sports Med 200533852–855. [DOI] [PubMed] [Google Scholar]
- 34.Fraser G A, Ahmed A M. Passive rotational stability of the weight‐bearing talocrural joint: an in vitro biomechanical study. Orthop Trans 19837248 [Google Scholar]
- 35.McCullough C J, Burge P D. Rotatory stability of the load‐bearing ankle. An experimental study. J Bone Joint Surg Br 198062B460–464. [DOI] [PubMed] [Google Scholar]
- 36.Stormont D M, Morrey B F, An K N.et al Stability of the loaded ankle. Am J Sports Med 198513295–300. [DOI] [PubMed] [Google Scholar]
- 37.Hosea T M, Carey C C, Harrer M F. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop 200037245–49. [DOI] [PubMed] [Google Scholar]
- 38.Johansson C. Training, injury and disease in senior and junior elite orienteers. Sci J Orienteer 198843–13. [Google Scholar]
- 39.Smith R, Damodaran A K, Swaminathan S.et al Hypermobility and sport injuries in junior netball players. Br J Sports Med 200539628–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Halasi T, Kynsburg A, Tallay A. Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 200432899–908. [DOI] [PubMed] [Google Scholar]