Abstract
Paget‐Schroetter syndrome is the spontaneous thrombosis of the axillary/subclavian vein. A 16‐year‐old male presented with acute onset of right upper limb swelling after vigorous weight training. A venogram confirmed the diagnosis of Paget–Schroetter syndrome. He was started on intravenous thrombolytics followed by oral anticoagulation therapy. His symptoms resolved and he was symptom free at six‐month follow‐up. Thrombolytics and anticoagulation is the most widely accepted first‐line therapy for this syndrome. Defining any anatomical anomaly as the predisposing factor in this condition is essential in the selection of which patients will benefit from thoracic outlet decompression.
Primary subclavian vein thrombosis is relatively an uncommon condition. It was first described by Paget in 1875, and then independently by Schroetter in 1884. Hughes, while reviewing his 320 cases of subclavian vein thrombosis, gave its name as Paget–Schroetter syndrome.1 In this paper we describe a case of Paget–Schroetter syndrome.
Case report
A 16‐year‐old male, who had been intensively weight training in preparation for the upcoming rugby season, presented with a two‐week history of discomfort in the right axilla. Following continued physical activity, there was progressive swelling of his right arm with associated engorged veins in his right upper limb, axilla and anterior‐lateral chest wall. The patient denied any trauma or past injuries to his upper extremities or trunk. He was not on any medications, although he was on protein supplements and creatine. The patient's family history was negative for any coagulopathies or venous thrombosis.
On physical examination, there was prominent superficial veins visible over the right subclavian area and a palpable cord over the basilic and axillary veins. The right upper extremity had oedema with homogeneous erythema that blanched to palpation. His radial and brachial pulses were normal. The remainder of the physical examination was normal.
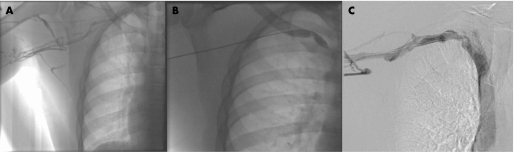
An upper extremity Doppler ultrasound showed complete thrombosis of the right subclavian axillary vein. The patient was admitted for treatment with intravenous unfractionated heparin. A 4‐F micropuncture sheath was placed into the right basilic vein; right subclavian venography was performed, which confirmed occlusion of right subclavian, axillary, and upper brachial branches with thrombus (fig 1A). A multisidehole infusion system (Craig‐McNamara, Micro Therapeutics Inc., Irvine, California, USA) was introduced through the 5Fr vascular sheath and its infusion length was embedded in the entire thrombus burden. After 10 mg bolus of recombinant tissue plasminogen activator (rt‐PA), an infusion was instituted at 1 mg/h, with heparin infusing via the side arm of the sheath at 42 U/h. Intravenous heparin was delivered by an infusion at 500 U/h. Subsequent venography performed revealed full resolution of the thrombus. The underlying subclavian vein lesion was treated with angioplasty (fig 1B) with good venographic result (fig 1C).
Figure 1 (A) Right upper limb venogram via right brachial access showing multiple right upper limb collaterals secondary to right subclavian occlusive thrombus. (B) 10 mm angioplasty balloon inflated in the right subclavian vein and distal right brachiocephalic vein with central stenosis of the right subclavian vein. (C) Venogram post‐angioplasty balloon dilation, intravenous TPA and heparin infusion. Patent right subclavian vein lumen with flow of contrast to the superior vena cava.
On discharge, the patient's symptoms were resolved and a decision was made to anticoagulate the patient for six months.
Discussion
Upper extremity deep venous thrombosis (UEDVT) is also known as thrombosis of the axillary‐subclavian vein, or Paget–Schroetter syndrome. It is a relatively infrequent disorder that occurs predominantly in young, otherwise healthy people who participate in repetitive upper extremity activity.2,3 The underlying mechanisms of thrombosis are thought to be a venous compressive anomaly at the thoracic outlet or intimal damage due to a strain of the subclavian and axillary veins by retroversion or hyperabduction of the arm. These movements are usually done during sport activities.
From an epidemiological perspective, the general incidence of UEDVT remains low (approximately 2/100 000 people per year), even though it is regarded as the most common vascular condition among athletes.4,5 Although early clinical recognition of UEDVT is important, diagnosis can be difficult because of its indeterminate cause and indistinct pathophysiology.
Symptoms are non‐specific, range in severity, may be position‐dependent and occasionally, patients may be entirely asymptomatic.5 Most commonly, however, patient complaints include initial “heaviness” in the affected arm, as well as a dull ache and pain of the involved limb. Other more dramatic signs may include swelling of the shoulder and arm; discolouration and mottled skin; and, distention of the cutaneous veins of the involved upper extremity.5 Acute symptoms can include pulmonary embolism in 7% to 20% of cases.6,7 Duplex ultrasound is the initial imaging test of choice as it is non‐invasive and demonstrates a high sensitivity and specificity for peripheral deep vein thrombosis.7
Anticoagulation is the cornerstone of therapy, to prevent further propagation of thrombus and maintain patency of collateral veins. Catheter‐directed thrombolysis restores venous patency early, minimises damage to the vessel endothelium, and reduces the risk of long‐term complications, especially post‐thrombotic syndrome, which is characterised by chronic arm and hand aching and swelling.8 Percutaneous mechanical thrombectomy is often used in combination with thrombolytics. If extrinsic venous compression is diagnosed, many surgeons are in favour of early correction of anatomy (rib or clavicle resection).8,9 However, others recommend a trial of conservative therapy after thrombolysis, rather than aggressive early surgical decompression.5,10
In conclusion, this case study serves as a reminder for sports trainers that athletes can develop UEDVT, a rare venous condition with atypical presentations. Although this diagnosis is infrequently reported in sports medicine publications, the condition has potential for significant morbidity and can cause a potentially fatal complication. Timely, accurate clinical recognition of the signs and symptoms of UEDVT is necessary to facilitate appropriate medical referral and treatment. A staged, multimodal approach to Paget–Schroetter syndrome can effectively restore venous patency, reduce the risk of rethrombosis, and return the person to normal function.
What is already known on this topic
It is a relatively infrequent disorder that occurs predominantly in young, otherwise healthy people who participate in repetitive upper extremity activity.
What this study adds
This report serves as a reminder for sports trainers that athletes can develop upper extremity deep vein thrombosis, a rare venous condition with atypical presentations. Although this diagnosis is infrequently reported in sports medicine publications, the condition has potential for significant morbidity and can cause a potentially fatal complication.
Abbreviations
UEDVT - upper extremity deep vein thrombosis
Footnotes
Competing interests: None declared.
References
- 1.Hughes E S R. Venous obstruction in upper extremity. Br J Surg 194936155–163. [DOI] [PubMed] [Google Scholar]
- 2.Medler R G, McQueen D A. Effort thrombosis in a young wrestler: a case report. J Bone Joint Surg Am 1993751071–1073. [DOI] [PubMed] [Google Scholar]
- 3.Filis K A, Nguyen T Q, Olcott C., 4th Subclavian vein thrombosis caused by an unusual congenital clavicular anomaly in an atypical anatomic position. J Vasc Surg 200236629–631. [DOI] [PubMed] [Google Scholar]
- 4.Feugier P, Aleksic I, Salari R.et al Long‐term results of venous revascularization for Paget‐Schroetter syndrome in athletes. Ann Vasc Surg 200115212–218. [DOI] [PubMed] [Google Scholar]
- 5.Joffe H V, Goldhaber S Z. Upper‐extremity deep vein thrombosis. Circulation 20021061874–1880. [DOI] [PubMed] [Google Scholar]
- 6.Gloviczki P, Kazmier F J, Hollier L H. Axillary subclavian venous occlusion: the morbidity of a nonlethal disease. J Vasc Surg 19864333–337. [DOI] [PubMed] [Google Scholar]
- 7.Prandoni P, Polistena P, Bernardi E.et al Upper extremity deep vein thrombosis. Risk factors, diagnosis, and complications. Arch Intern Med 199715757–62. [PubMed] [Google Scholar]
- 8.Urschel H C, Jr, Razzuk M A. Paget‐Schroetter syndrome: what is the best management? Ann Thorac Surg 2000691663–1668. [DOI] [PubMed] [Google Scholar]
- 9.Lee M C, Grassi C J, Belkin M.et al Early operative intervention after thrombolytic therapy for primary subclavian vein thrombosis: an effective treatment approach. J Vasc Surg 1998271101–1108. [DOI] [PubMed] [Google Scholar]
- 10.Khan S N, Stansby G. Current management of Paget‐Schroetter syndrome in the UK. Ann R Coll Surg Engl 20048629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]