Abstract
Objective
To determine whether positioning of the tibia affects the degree of tibial external rotation seen during a dial test in the posterior cruciate ligament (PCL)–posterolateral corner (PLC)‐deficient knee.
Design
Laboratory investigation.
Setting
Biomechanics laboratory.
Hypothesis
An anterior force applied to the tibia in the combined PCL–PLC‐deficient knee will yield increased tibial external rotation during a dial test.
Methods
The degree of tibial external rotation was measured with 5 N⋅m of external rotation torque applied to the tibia at both 30° and 90° of knee flexion. Before the torque was applied, an anterior force, a posterior force, or neutral (normal, reduced control) force was applied to the tibia. External rotation measurements were repeated after sequential sectioning of the PCL, the posterolateral structures and the fibular collateral ligament (FCL).
Results
Baseline testing of the intact specimens demonstrated a mean external rotation of 18.6° with the knee flexed to 30° (range 16.1–21.0°), and a mean external rotation of 17.3° with the knee flexed to 90° (range 13.8–20.0°). Sequential sectioning of the PCL, popliteus and popliteofibular ligament, and the FCL led to a significant increase in tibial external rotation compared with the intact knee for all testing scenarios. After sectioning of the popliteus and popliteofibular ligament, the application of an anterior force during testing led to a mean tibial external rotation that was 5° greater than during testing in the neutral position and 7.5° greater than during testing with a posterior force. In the PCL, popliteus/popliteofibular ligament and FCL‐deficient knee, external rotation was 9° and 12° greater with the application of an anterior force during testing compared with neutral positioning and the application of a posterior force, respectively.
Conclusion
An anterior force applied to the tibia during the dial test in a combined PCL–PLC‐injured knee increased the overall amount of observed tibial external rotation during the dial test. The anterior force reduced the posterior tibial subluxation associated with PCL injury, which is analogous to what is observed when the dial test is performed with the patient in the prone position. Reducing the tibia with either an anterior force when the patient is supine or performing the dial test with the patient in the prone position increases the ability of an examiner to detect a concomitant PLC injury in the setting of a PCL‐deficient knee.
Injuries to the posterolateral corner (PLC) of the knee have become increasingly appreciated as a source of significant morbidity, especially when combined with other ligamentous injuries in the knee.1 The posterolateral compartment of the knee is stabilised by two primary components, the fibular collateral ligament (FCL) and the popliteus complex. The popliteus complex consists of the popliteus tendon and its ligamentous connections (ie, the popliteofibular ligament). The fabellofibular ligament is also considered to be part of the PLC but its importance is believed to be relatively minor.2,3,4 The majority of PLC injuries have been found to occur in combination with other ligamentous pathology, most commonly with tears of the anterior cruciate ligament or posterior cruciate ligament (PCL).5 A failure to recognise and treat injury to the PLC in the presence of concomitant cruciate ligament injury has been demonstrated to add significant risk of failure to the reconstruction of the cruciate ligament.6,7,8,9,10
Several clinical and radiographic tests have been developed to assess injuries to the posterolateral structures. These include the reverse pivot‐shift test, external rotation recurvatum test, the posterolateral drawer test, the standing apprehension test, and PCL radiographic stress testing.5,11,12,13,14 With PCL stress x rays, >12 mm of side‐to‐side difference with respect to posterior tibial translation has been described to represent a combined PCL–PLC injury until proven otherwise.12,13 Another commonly used diagnostic test is the posterolateral rotation test, also known as the dial test.14 As first described by Noyes et al,14 the dial test was performed with the patient supine and the tibia positioned at both 30° and 90° of knee flexion, observing the extent of external tibial rotation with reference to the contralateral knee. This external rotation test has been shown to reliably assess PLC injuries in the laboratory,4,14,15,16 although some authors believe that it is more difficult to apply accurately in clinical situations.5,11 Currently, there is controversy within the orthopaedic literature as to whether the dial test should be performed with the patient in the prone position or in the supine position, and there are currently no recommendations as to whether any anterior or posterior force should be placed on the tibia during this provocative test.11 Potentially, if the knee is examined in a state of altered anatomical positioning, a PLC injury may be missed.
Commonly, in the setting of a PCL injury, posterior sag of the tibia is noted when the patient is in the supine position. The impact of this posterior tibial subluxation seen in the PCL‐deficient knee on the ability of the dial test to detect a concomitant PLC injury has not been evaluated previously. The purpose of the current study was to determine the effect of anterior or posterior tibial positioning on tibial external rotation in the PCL–PLC‐ deficient knee. We hypothesised that reducing the posterior tibial subluxation with an anterior force applied to the tibia in the PCL–PLC‐deficient knee would yield increased external rotation during the dial test.
Materials and methods
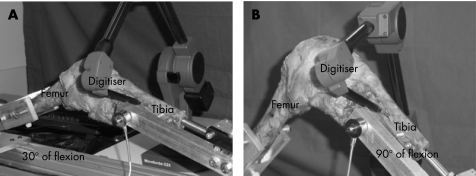
Ten fresh frozen human cadaveric knees with a mean (range) age of 67 (62–85) years underwent biomechanical testing. Each specimen was dissected, removing all muscles except the popliteus. The femur and tibia were cut using an oscillating saw to leave approximately 20 cm of bone above and below the joint line for specimen mounting. The intact knees were mounted on a custom‐built jig (fig 1), with the femur and tibia locked with intramedullary fixation. The jig enabled the knee to be positioned at any degree of flexion, while also allowing free rotation of the tibia. The testing apparatus was designed to allow testing in a neutral position (defined as a normal, reduced femorotibial articulation) and to apply a measured anterior or posterior force on the tibia via the intramedullary nail. A torque wrench was attached to the tibial intramedullary nail, which allowed application of a controlled 5 N⋅m external rotation torque.17 The 5 N⋅m torque was chosen to simulate the clinical application of the dial test in evaluating the posterolateral rotatory instability of the knee.14
Figure 1 Custom‐built jig with the femur and tibia locked with intramedullary fixation, enabling the knee to be positioned at any degree of flexion (30° of knee flexion (A) and 90° of knee flexion (B)), while also allowing free rotation of the tibia.
Biomechanical evaluation involved an initial assessment of the degree of tibial external rotation for each intact knee with an applied external rotation torque of 5 N⋅m. Measurements were made with the knee flexed to 30° and 90°, with 5 min duration between testing sessions to allow the viscoelastic structures to return to their baseline states. Rotational measurements were digitally recorded using a digitiser (MicroScribe G2X, High Accuracy Model–accurate to 0.009 inch (0.23 mm), Immersion Corporation, San Jose, California, USA). Subsequently, anterior and posterior loads of 50 and 100 N were applied to the tibia 10 cm distal to the knee joint line. A simultaneous 5 N⋅m external rotation torque was applied, and the amount of tibial external rotation was recorded for each loading scenario.
The PCL was then sectioned with a scalpel at the tibial insertion. The same anterior and posterior drawer forces of 50 and 100 N were placed on the tibia, and the 5 N⋅m external rotation torque was applied, measuring the extent of tibial external rotation with the knee at 30° and 90° of flexion. Next, the popliteus tendon and popliteofibular ligament were sectioned with a scalpel. Each specimen was similarly loaded and subjected to the external rotation torque, and tibial external rotation measurements recorded. Finally, the FCL was sectioned and the protocol repeated.
The data obtained consisted of the four scenarios (intact, PCL deficient, PCL and PLC deficient, and PCL, PLC and FCL deficient), with each specimen tested with 5 N⋅m of external rotation torque in neutral, with an applied anterior force and an applied posterior force. To test whether a trend in external rotation existed across the direction of force (anterior vs posterior vs neutral), we performed a quantile regression analysis, using the median as the quantile of choice. Data were stratified on the basis of degree of knee flexion (30° vs 90°) and applied force (50 N vs 100 N), which resulted in four models for each of the four specified knee specimen conditions (intact, PCL deficient, PCL and PLC deficient, and PCL, PLC and FCL deficient).
Results
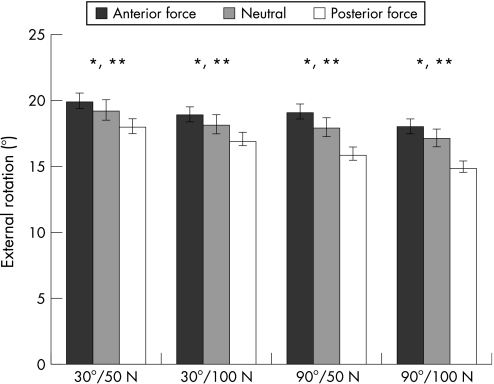
Testing of the intact specimens demonstrated a mean external rotation of 18.6°, with the knee flexed to 30° (range 16.1–21.0°), and a mean external rotation of 17.3°, with the knee flexed to 90° (range 13.8–20.0°). The application of an anterior force significantly increased the extent of external rotation observed in the intact specimens compared with that observed both in the neutral position and on the application of a posterior force (p<0.001 for both comparisons). With the knee positioned at both 30° and 90° of flexion, the application of a 50 N anterior force increased the mean external rotation by 2° compared with that seen with a 50 N posterior force. Similarly, a 100 N anterior force increased the mean external rotation by 2–3° compared with a 100 N posterior force at 30° and 90° of knee flexion (fig 2).
Figure 2 Observed external rotation during testing of intact knee specimens. *Significant difference observed between application of an anterior force and testing in the neutral position. **Significant difference observed between application of an anterior force and application of a posterior force.
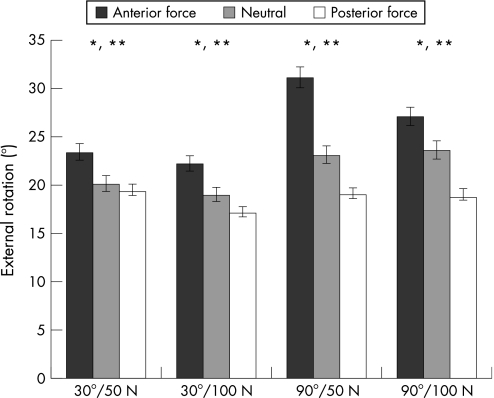
Sectioning of the PCL led to a significant increase in tibial external rotation compared with the intact knee for all testing scenarios (p<0.001). Knees tested with an application of an anterior force demonstrated a mean external rotation of 25.9°, which was significantly greater than that seen at neutral positioning (mean 21.4°) and with application of a posterior force (mean 18.7°; p<0.001 for both comparisons). The greatest extent of tibial external rotation was observed with a 50 N anterior force, with the knee at 90° of flexion (fig 3).
Figure 3 Observed external rotation during testing of posterior cruciate ligament‐deficient knee specimens. *Significant difference observed between application of an anterior force and testing in the neutral position. **Significant difference observed between application of an anterior force and application of a posterior force.
After sectioning of the popliteus and popliteofibular ligament, there was a further significant increase in the amount of tibial external rotation observed for all testing schema (p<0.001). The application of an anterior force during testing led to a mean tibial external rotation that was 5° greater than that for testing in the neutral position and 7.5° greater than that for testing with a posterior force (p<0.001 for both comparisons). Positioning the knee at 30° of flexion with the application of a 50 N anterior force led to the greatest amount of observed external rotation (fig 4).
Figure 4 Observed external rotation during testing of posterior cruciate ligament‐, popliteus‐ and popliteofibular ligament‐deficient knee specimens. *Significant difference observed between application of an anterior force and testing in the neutral position. **Significant difference observed between application of an anterior force and application of a posterior force.
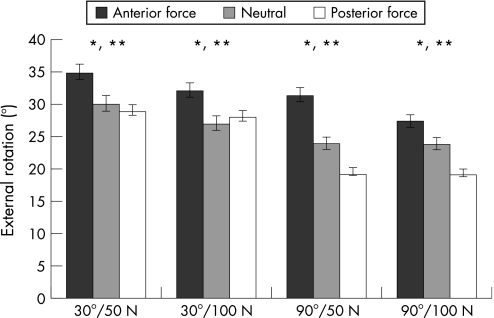
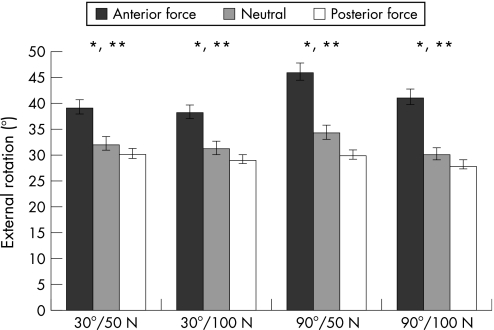
Tibial external rotation during testing was similarly increased with the sequential sectioning of the FCL (p<0.001). External rotation was 9° and 12° greater with the application of an anterior force during testing compared with that during neutral positioning and application of a posterior force, respectively (p<0.001 for both comparisons). With the PCL–PLC‐deficient knee flexed to 90° and application of a 50 N anterior force, the mean external rotation observed was 46°, a 250% increase compared with that seen under similar conditions with intact specimens (fig 5).
Figure 5 Observed external rotation during testing of posterior cruciate ligament‐, popliteus/popliteofibular‐ and fibular collateral ligament‐deficient knee specimens. *Significant difference observed between application of an anterior force and testing in the neutral position. **Significant difference observed between application of an anterior force and application of a posterior force.
Discussion
Although injuries to the posterolateral structures of the knee are relatively uncommon, when present, they can cause significant morbidity. Because of the convex opposing surfaces of the lateral femoral condyle and the lateral tibial plateau, patients with posterolateral knee injuries may have instability even with normal gait. The lack of static PLC structures at foot strike can lead to opening of the lateral compartment, and the resultant varus thrust gait can be disabling.2 Owing to the complex anatomy and biomechanics of the posterolateral structures of the knee, injuries in this region remain a diagnostic and therapeutic challenge to the orthopaedic surgeon.
The biomechanical role of the various components of the PLC of the knee has been elucidated in previous studies via selective ligament sectioning in fresh cadaveric knees.4,7,9,15,18,19 These studies have demonstrated that the posterolateral structures have a primary role in resisting excessive varus and external rotational forces. Of the components of the PLC, the FCL is the primary structure responsible for resisting varus force, although the popliteus complex acts as a primary restraint against external tibial rotation.15,19,20,21 In our biomechanical evaluation, we found that the FCL contributed significantly to the resistance of tibial external rotation as well. An additional 9–11° of tibial external rotation was noted after sectioning of the FCL subsequent to sectioning of the PCL, and popliteus and popliteofibular ligament. We did not section the FCL first in our testing protocol, which precluded us from determining whether the FCL or popliteus complex contributed more to resisting external rotation.
Prior cadaveric studies by Grood et al15 demonstrated that external rotation of the tibia increased with sectioning of the posterolateral structures, and that this was further increased with a concomitant PCL injury. The results of our evaluation confirm this finding. The amount of tibial external rotation observed during testing significantly increased with sequential sectioning of the PCL, popliteus and the FCL. This was true at both 30° and 90° of knee flexion, with the tibia in neutral position during testing and with both an anterior and a posterior applied force.
To our knowledge, there have been no prior studies evaluating the impact of application of an anterior or a posterior force to the tibia on the amount of tibial external rotation in a PLC‐deficient knee. Our results suggest that an increase of 4.5–12° of external rotation can be measured by applying an anterior force compared with a posterior force. Given that an increase of 10–15° of external rotation compared with the uninjured knee is considered significant to treat a PLC injury, the extra external rotation observed on application of an anterior force during testing may significantly improve the ability of an examiner to make the diagnosis.
PLC/FCL injuries in isolation are not common. More often, they are found as part of a combined injury pattern associated with cruciate ligament injury.5,22,23,24,25 For PCL injuries, the most common associated pathology is an injury to the PLC, occurring in up to 60% of cases.23 As a significant increase in force is seen on cruciate ligament reconstruction grafts when a concurrent PLC injury is present, it is recommended that PLC injuries be repaired or reconstructed during cruciate ligament reconstruction.5,26,27
Given the high association between these two injuries, it is important to know how the presence of a PCL tear can affect the physical diagnosis of the PLC injury. In the case of a grade 3 PCL injury, the tibia sags posteriorly compared with its normal position. If this posterior position decreases the amount of external rotation, then, theoretically, the chance of missing a PLC injury may be increased. Conversely, if the posterior tibial subluxation is reduced with an anteriorly directed force, which is analogous to prone positioning of the patient during testing, the amount of external rotation and therefore the sensitivity of the dial test may be increased.
What is already known on this topic
When combined with other ligamentous injuries in the knee, injury to the posterolateral corner (PLC) may be a source of significant morbidity.
Failure to recognise and treat injuries to the PLC in the presence of concomitant cruciate ligament injury may lead to poor outcomes following cruciate ligament reconstruction.
The posterolateral rotation test, also known as the dial test, is commonly used in the evaluation of suspected PLC injuries.
The goal of the dial test is to detect increased external tibial rotation relative to the contralateral side, at 30° and 90° of knee flexion, which would indicate injury to the structures of the PLC.
At present, there is no consensus on whether the dial test should be performed with the patient supine or prone or whether any anterior or posterior force should be applied during testing.
What this study adds
In a combined posterior cruciate ligament (PCL)–posterolateral corner (PLC)‐injured knee, an anterior force applied to the tibia increased the overall amount of observed tibial external rotation during the dial test.
The anterior force reduced the posterior tibial subluxation associated with PCL injury, which is analogous to what is observed when the dial test is performed with the patient in the prone position.
Reducing the tibia with either an anterior force when the patient is supine or performing the dial test with the patient prone increases the ability of an examiner to detect a concomitant PLC injury in the setting of a PCL‐deficient knee.
Although not evaluated in the current study, the competency of the medial collateral ligament (MCL) becomes important in the setting of a patient in the prone position during the dial test. Incompetence of the MCL may lead to tibial rotatory instability, mimicking a PLC injury with increased external rotation on the dial test.28,29 In a recent cadaveric study by Pritsch et al30, the authors found that the results of the dial test after transection of the MCL were similar to those seen from a solitary PLC injury, with significant increases in external rotation with the knee in both 30° and 90° of flexion. Although Pritsch's study did not investigate the effect of MCL incompetence on the PCL‐deficient knee, it seems appropriate to rule out an associated MCL injury with valgus stress testing at 0° and 30° of flexion during the physical examination for a suspected combined PCL/PLC injury.
Conclusion
PLC injuries of the knee are often accompanied by injuries to the PCL, making accurate diagnosis and treatment a challenge. The ability to accurately identify PLC injuries in a PCL‐deficient knee using a more sensitive diagnostic test would enable the surgeon to address this pathology at the time of reconstruction, thereby potentially limiting failures associated with the added stress of a missed PLC injury. In the setting of a combined PCL/PLC injury, an anteriorly directed reduction force applied to the tibia may increase the degree of external rotation observed during the dial test. The addition of the anterior force to the dial test manoeuvre, which is analogous to performing the test in the prone position, reduces the posterior tibial subluxation often seen in the PCL‐deficient knee, and may make the test more sensitive in detecting concomitant PLC injuries.
Abbreviations
FCL - fibular collateral ligament
MCL - medial collateral ligament
PCL - posterior cruciate ligament
PLC - posterolateral corner
Footnotes
Competing interests: None declared.
References
- 1.Chen F S, Rokito A S, Pitman M I. Acute and chronic posterolateral rotatory instability of the knee. J Am Acad Orthop Surg 2000897–110. [DOI] [PubMed] [Google Scholar]
- 2.Baker C L, Jr, Norwood L A, Hughston J C. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am 198365614–618. [PubMed] [Google Scholar]
- 3.Bleday R M, Fanelli G C, Giannotti B F.et al Instrumented measurement of the posterolateral corner. Arthroscopy 199814489–494. [DOI] [PubMed] [Google Scholar]
- 4.Gollehon D L, Torzilli P A, Warren R F. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am 198769233–242. [PubMed] [Google Scholar]
- 5.LaPrade R F, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res 2002402110–121. [DOI] [PubMed] [Google Scholar]
- 6.Harner C D, Janaushek M A, Ma C B.et al The effect of knee flexion angle and application of an anterior tibial load at the time of graft fixation on the biomechanics of a posterior cruciate ligament‐reconstructed knee. Am J Sports Med 200028460–465. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R F, Muench C, Wentorf F.et al The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med 200230233–238. [DOI] [PubMed] [Google Scholar]
- 8.Markolf K L, Slauterbeck J R, Armstrong K L.et al A biomechanical study of replacement of the posterior cruciate ligament with a graft. Part II: Forces in the graft compared with forces in the intact ligament. J Bone Joint Surg Am 199779381–386. [DOI] [PubMed] [Google Scholar]
- 9.Markolf K L, Wascher D C, Finerman G A. Direct in vitro measurement of forces in the cruciate ligaments. Part II: The effect of section of the posterolateral structures. J Bone Joint Surg Am 199375387–394. [DOI] [PubMed] [Google Scholar]
- 10.O'Brien S J, Warren R F, Pavlov H.et al Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am 199173278–286. [PubMed] [Google Scholar]
- 11.Larsen M W, Toth A. Examination of posterolateral corner injuries. J Knee Surg 200518146–150. [DOI] [PubMed] [Google Scholar]
- 12.Margheritini F, Mancini L, Mauro C S.et al Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy 200319706–711. [DOI] [PubMed] [Google Scholar]
- 13.Mariani P P, Margheritini F, Christel P.et al Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy 2005211354–1361. [DOI] [PubMed] [Google Scholar]
- 14.Noyes F R, Stowers S F, Grood E S.et al Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro ligament sectioning study in cadaveric knees. Am J Sports Med 199321407–414. [DOI] [PubMed] [Google Scholar]
- 15.Grood E S, Stowers S F, Noyes F R. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 19887088–97. [PubMed] [Google Scholar]
- 16.Tibone J E, Antich T J, Perry J.et al Functional analysis of untreated and reconstructed posterior cruciate ligament injuries. Am J Sports Med 198816217–223. [DOI] [PubMed] [Google Scholar]
- 17.Kaneda Y, Moriya H, Takahashi K.et al Experimental study on external tibial rotation of the knee. Am J Sports Med 199725796–800. [DOI] [PubMed] [Google Scholar]
- 18.Veltri D M, Warren R F. Posterolateral instability of the knee. Instr Course Lect 199544441–453. [PubMed] [Google Scholar]
- 19.Vogrin T M, Hoher J, Aroen A.et al Effects of sectioning the posterolateral structures on knee kinematics and in situ forces in the posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2000893–98. [DOI] [PubMed] [Google Scholar]
- 20.LaPrade R F, Bollom T S, Wentorf F A.et al Mechanical properties of the posterolateral structures of the knee. Am J Sports Med 2005331386–1391. [DOI] [PubMed] [Google Scholar]
- 21.Laprade R F, Wentorf F A, Olson E J.et al An in vivo injury model of posterolateral knee instability. Am J Sports Med 2006341313–1321. [DOI] [PubMed] [Google Scholar]
- 22.Fanelli G C. Surgical reconstruction for acute posterolateral injury of the knee. J Knee Surg 200518157–162. [DOI] [PubMed] [Google Scholar]
- 23.Fanelli G C, Larson R V. Practical management of posterolateral instability of the knee. Arthroscopy 200218(Suppl 1)1–8. [DOI] [PubMed] [Google Scholar]
- 24.LaPrade R F, Terry G C. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med 199725433–438. [DOI] [PubMed] [Google Scholar]
- 25.Terry G C, LaPrade R F. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med 199624732–739. [DOI] [PubMed] [Google Scholar]
- 26.Harner C D, Vogrin T M, Hoher J.et al Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med 20002832–39. [DOI] [PubMed] [Google Scholar]
- 27.LaPrade R F, Resig S, Wentorf F.et al The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med 199927469–475. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy J C, Fowler P J. Medial and anterior instability of the knee. An anatomical and clinical study using stress machines. J Bone Joint Surg Am 1971531257–1270. [PubMed] [Google Scholar]
- 29.Warren L A, Marshall J L, Girgis F. The prime static stabilizer of the medical side of the knee. J Bone Joint Surg Am 197456665–674. [PubMed] [Google Scholar]
- 30.Pritsch T, Blumberg N, Haim A.et al The importance of the valgus stress test in the diagnosis of posterolateral instability of the knee. Injury 2006371011–1014. [DOI] [PubMed] [Google Scholar]