Abstract
Objective
Data are scarce regarding the sociodemographic predictors of antenatal and postpartum depression. This study investigated whether race/ethnicity, age, finances, and partnership status were associated with antenatal and postpartum depressive symptoms.
Setting
1662 participants in Project Viva, a US cohort study.
Design
Mothers indicated mid‐pregnancy and six month postpartum depressive symptoms on the Edinburgh postpartum depression scale (EPDS). Associations of sociodemographic factors with odds of scoring >12 on the EPDS were estimated.
Main results
The prevalence of depressive symptoms was 9% at mid‐pregnancy and 8% postpartum. Black and Hispanic mothers had a higher prevalence of depressive symptoms compared with non‐Hispanic white mothers. These associations were explained by lower income, financial hardship, and higher incidence of poor pregnancy outcome among minority women. Young maternal age was associated with greater risk of antenatal and postpartum depressive symptoms, largely attributable to the prevalence of financial hardship, unwanted pregnancy, and lack of a partner. The strongest risk factor for antenatal depressive symptoms was a history of depression (OR = 4.07; 95% CI 3.76, 4.40), and the strongest risk for postpartum depressive symptoms was depressive symptoms during pregnancy (6.78; 4.07, 11.31) or a history of depression before pregnancy (3.82; 2.31, 6.31).
Conclusions
Financial hardship and unwanted pregnancy are associated with antenatal and postpartum depressive symptoms. Women with a history of depression and those with poor pregnancy outcomes are especially vulnerable to depressive symptoms during the childbearing year. Once these factors are taken in account, minority mothers have the same risk of antenatal and postpartum depressive symptoms as white mothers.
Keywords: depression, pregnancy, socioeconomic factors, women, minority groups
Major depressive disorder affects more than 20% of women during their lifetime, and is a leading cause of morbidity among women.5 Pregnancy and the postpartum months may be windows of heightened vulnerability to depression. Antenatal and postpartum depression are associated with marital discord and low social, emotional, and cognitive competence among offspring.2,3,4,5
Despite advances in understanding the causes of major depression, the predictors of antenatal and postpartum depressive symptoms remain poorly understood. Major depression in women is associated with poor social support, marital conflict, adverse life events, and low maternal education.6 Poverty is a powerful predictor of major depression, with incidence rates two to three times higher among lowest socioeconomic groups.7,8 Several stressors associated with major depression also predict depression during the childbearing year. Primary among these are adverse life events and poor social support.9,10,11,12
There is more debate, and less data, with regard to sociodemographic risk factors for antenatal and postpartum depression. Although several studies report no association of socioeconomic position with antenatal and postpartum depression,13,14,15,16,17,18 others conducted in impoverished areas report depression rates as high as 25% during pregnancy and 20% or more postpartum.11,19,20 Large epidemiological surveys have shown that white persons and Hispanics may be more vulnerable to major depression uncomplicated by other illness, while black persons are especially prone to comorbid depression.21,22,23 Almost no studies, however, have examined how antenatal and postpartum depression vary across racial and ethnic groups, and the extent to which such variation is explained by socioeconomic position. We determined to investigate sociodemographic predictors of antenatal and postpartum depressive symptoms in a large obstetrics practice.
Methods
Project Viva is a prospective cohort study of pregnancy outcomes and maternal and child health.24,25 Participants were recruited at their first prenatal visit to one of eight obstetric practices associated with Harvard Vanguard Medical Associates, a large group practice in urban and suburban Boston. This analysis used data collected at enrolment (at a mean 10 weeks' gestation), mid‐pregnancy (28 weeks' gestation), and at six months postpartum.
Of 2128 Project Viva participants who delivered a live infant, 1662 (78%) completed a mid‐pregnancy questionnaire that assessed history of depression as well as current depressive symptoms with a 10 item Edinburgh postpartum depressive symptoms scale (EPDS).26 At six months postpartum, 1278 respondents (77% of the cohort that completed the mid‐pregnancy questionnaire) completed a second EPDS.
We chose the EPDS because it has been validated for both antenatal and postpartum use.26,27,28 The EPDS focuses on cognitive and affective symptoms, avoiding the inflation of prevalence by physical symptoms (such as fatigue and physical discomfort) typical of normal pregnancy and the postpartum.9,29 An EPDS score above 12 indicates probable depression.29,30,31 Validation of the EPDS against diagnostic clinical interviews indicated a specificity of 78% and a sensitivity of 86%.26 While a score of more than 12 on the EPDS does not confirm depression, factors that predict an EPDS score above this threshold probably predict clinically significant depression.
We measured history of depressive symptoms before pregnancy with the question, “Before this pregnancy, was there ever a period of time when you were feeling depressed or down or when you lost interest in pleasurable activities most of the day, nearly every day, for at least 2 weeks?” There were 309 women (19%) who endorsed this question. A history of depression required an endorsement of the symptom question plus either an indication that she saw a health care professional who said she was depressed or an indication that a health care professional had prescribed her a medication for depression. By this definition, 185 (11%) women had a history of depression. Concerned that women with lower socioeconomic status might be less likely to receive professional diagnosis or treatment of depression, we also considered history of depressive symptoms without treatment or diagnosis.
We measured by interview and questionnaire risk factors for depression. Maternal age, race/ethnicity, immigrant status, household income, education, maternal employment status, cigarette smoking, pre‐pregnant body mass index (kg/m2), partnership status, and pregnancy intention/wantedness were recorded at enrolment, typically in the first trimester. Pregnancy intention/wantedness was assessed with the question: “Regarding this pregnancy: (a) I was actively trying to become pregnant; (b) I was not actively trying, but I was glad to become pregnant; (c) I wanted to be pregnant someday, but not now; or (d) I did not want to be pregnant now or at any time in the future”. Because of small numbers, we collapsed both “not now” responses into one category that represented 5% of respondents. As teen motherhood and childbearing before the typical age of college graduation were rare in this cohort, we considered as the youngest age group mothers under the age of 23 years (74 participants, or 4% of the cohort). We chose this age cut off point because it represented the age at which a woman might bear a child after having completed four years of post‐high school education. Social support was recorded at mid‐pregnancy, using short questionnaire scales that measured emotional and material support from a partner and, separately, from family or friends.32 Offspring birth weight was extracted from hospital delivery records. At six months postpartum, when the EPDS was readministered, we again recorded partnership status, body mass index, cigarette smoking, household income, financial hardship, maternal employment, as well as resumption of menstrual cycles, breast feeding, social support, postpartum physical symptoms, and quantity of maternal and infant sleep. Postpartum financial hardship was defined as a “no” response to any of the following items, “Since your baby was born, have you always had enough money to: (a) buy infant formula; (b) buy baby food; (c) buy nappies (diapers); (d) buy food; (e) pay rent or mortgage.” We used multiple imputation to account for missing independent variables.33 This study was approved by the human subjects committee of Harvard Pilgrim Health Care.
Statistical analysis
We built logistic regression models to account for the independent and confounding effects of many variables. We sought to include only variables that were either (1) a main exposure under investigation (age, race/ethnicity, immigrant status, household income, financial hardship, partnership status) or (2) theoretical or empirical confounders of the main exposures (such as parity or delivery of a low birthweight infant). Where information is lacking on the exact timing of the “exposures” relative to onset of depressive symptoms, it can be murky to discover if the “exposures” might in fact be the result of a history of depressive symptoms. For example, could current partnership status be a result of previous depressive symptoms? Did depressive symptoms start before or after the conception of an unintended pregnancy? We therefore performed secondary analyses to test whether exposure‐outcome relations were similar among women without a history of depression or depressive symptoms.
Results
Prevalence of depressive symptoms
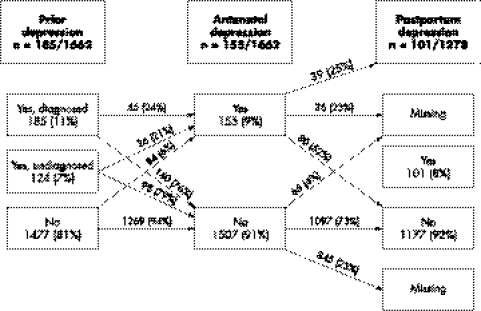
Figure 1 shows the prevalence of depressive symptoms before, during, and after pregnancy. Overall, 9% of participants had an EPDS score >12 during pregnancy. At six months postpartum, 8% of participants scored >12 on the EPDS. There were 1278 participants who responded to both the antenatal and postpartum questionnaires: among these women, 31% of women with antenatal depressive symptoms also suffered from postpartum depressive symptoms. In contrast, only 6% without antenatal depressive symptoms experienced postpartum depressive symptoms.
Figure 1 Prevalence of depression before, during, and after pregnancy, Project Viva.
Risk factors for depressive symptoms
Table 1 shows the prevalence of risk factors. These unadjusted statistics show higher prevalence of depressive symptoms among mothers who were younger, less educated, with fewer financial resources, without a spouse or cohabitating partner, and those who delivered low birthweight infants. Before adjusting for other factors associated with minority status, it seemed that there was a higher prevalence of depressive symptoms among black and Hispanic mothers. The remaining analysis focused on identifying which of these were independent risk factors for depressive symptoms.
Table 1 Characteristics of participants and prevalence of depressive symptoms, Project Viva.
| Antenatal Number (% of antenatal respondents with characteristic) | History of depression before index pregnancy Number (% of antenatal respondents with history of depression) | Antenatal EPDS >12 Number (% of antenatal respondents with antenatal depressive symptoms) | Postpartum Number | Postpartum EPDS >12 Number (% of postpartum respondents with postpartum depressive symptoms) | |
|---|---|---|---|---|---|
| 1662 | 185 (11) | 155 (9) | 1278 | 101 (8) | |
| Maternal age | |||||
| <23 | 74 (4) | 12 (16) | 17 (23) | 49 | 11 (22) |
| 23–29 | 376 (23) | 35 (9) | 38 (10) | 268 | 19 (7) |
| 30–34 | 739 (44) | 73 (10) | 64 (9) | 581 | 45 (8) |
| 35–39 | 406 (24) | 53 (13) | 32 (8) | 329 | 23 (7) |
| >40 | 67 (4) | 12 (18) | 4 (6) | 51 | 3 (6) |
| Race/ethnicity | |||||
| White | 1199 (72) | 144 (12) | 89 (7) | 974 | 68 (7) |
| Black | 207 (12) | 14 (7) | 31 (15) | 120 | 14 (12) |
| Hispanic | 91 (5) | 14 (15) | 15 (16) | 66 | 8 (12) |
| Asian | 97 (6) | 7 (7) | 12 (12) | 74 | 3 (4) |
| Other | 60 (4) | 6 (10) | 8 (13) | 42 | 8 (19) |
| Missing | 8 (<1) | 0 (0) | 0 (0) | 2 | 0 (0) |
| Immigrant status | |||||
| US born | 1299 (78) | 162 (12) | 110 (8) | 1029 | 83 (8) |
| Foreign born | 335 (20) | 20 (6) | 43 (13) | 233 | 17 (7) |
| Missing | 28 (2) | 3 (11) | 2 (7) | 16 | 1 (6) |
| Parity | |||||
| 0 | 838 (50) | 112 (13) | 75 (9) | 657 | 55 (8) |
| ⩾1 | 824 (50) | 73 (9) | 80 (10) | 621 | 46 (7) |
| Annual household income | |||||
| ⩽$20000 | 49 (3) | 8 (16) | 12 (24) | 24 | 3 (13) |
| 20001–40000 | 137 (8) | 17 (12) | 24 (18) | 91 | 15 (16) |
| 40001–70000 | 361 (22) | 42 (12) | 35 (10) | 266 | 27 (10) |
| >$70000 | 998 (60) | 105 (11) | 66 (7) | 822 | 48 (6) |
| Missing | 117 (7) | 13 (11) | 18 (15) | 75 | 8 (11) |
| Financial hardship at six months postpartum | |||||
| Yes | 68 (5) | 19 (28) | |||
| No | 1184 (93) | 78 (7) | |||
| Missing | 26 (2) | 4 (15) | |||
| Maternal education | |||||
| HS or less | 139 (8) | 23 (17) | 25 (18) | 73 | 11 (15) |
| Some college | 342 (21) | 34 (10) | 39 (11) | 252 | 26 (10) |
| BA or BS | 628 (38) | 61 (10) | 46 (7) | 495 | 29 (6) |
| Graduate degree | 545 (33) | 67 (12) | 45 (8) | 456 | 35 (8) |
| Missing | 8 (<1) | 0 (0) | 0 (0) | 2 | 0 (0) |
| Marital status | Early pregnancy status | Postpartum status | |||
| Married | 1426 (86) | 150 (11) | 110 (8) | 1152 | 82 (7) |
| Cohabitating | 126 (8) | 17 (13) | 18 (14) | 68 | 6 (9) |
| Unpartnered | 101 (6) | 18 (18) | 27 (27) | 42 | 11 (26) |
| Missing | 9 (<1) | 0 (0) | 0 (0) | 16 | 2 (13) |
| Pregnancy intention | |||||
| Trying | 1036 (62) | 114 (11) | 73 (7) | 833 | 55 (7) |
| Not trying but glad | 487 (29) | 54 (11) | 54 (11) | 348 | 32 (9) |
| Not now/never | 84 (5) | 13 (15) | 22 (26) | 63 | 12 (19) |
| Missing | 55 (3) | 4 (7) | 6 (11) | 34 | 2 (6) |
| Low birth weight | |||||
| Yes | 68 (4) | 10 (15) | 9 (13) | 56 | 11 (20) |
| No | 1594 (96) | 175 (11) | 146 (9) | 1222 | 90 (7) |
Predictors of antenatal depressive symptoms
Table 2 shows models built to investigate predictors of antenatal depressive symptoms. In a basic model including maternal age, race/ethnicity, immigrant status, and parity (model 1), we found decreasing risks of antenatal depressive symptoms with increasing maternal age, with the youngest mothers (<23 years) at two or more times the risk of depressive symptoms compared with older mothers. In this naive model, black and Hispanic mothers seemed to be at increased risk of antenatal depressive symptoms. However, further adjustment for household income (model 2) dampened the associations of maternal age and race/ethnicity with antenatal depressive symptoms.
Table 2 Odds ratios (95% confidence intervals) for risk factors for antenatal depressive symptoms in mid‐pregnancy, Project Viva.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Maternal age | ||||
| <23 | 2.71 (1.40,5.24) | 1.87 (0.93,3.74) | 1.21 (.057,2.56) | 1.10 (0.51,2.39) |
| 23–29 | 1.15 (.075,1.78) | 1.02 (0.66,1.59) | 0.95 (0.60,1.49) | 0.96 (0.61,1.52) |
| 30–34 | 1.00 | 1.00 | 1.00 | 1.00 |
| 35–39 | 0.88 (0.56,1.39) | 0.93 (0.59,1.45) | 0.92 (.058,1.44) | 0.88 (0.56,1.39) |
| 40+ | 0.65 (0.23,1.85) | 0.67 (0.23,1.94) | 0.66 (0.23,1.91) | 0.65 (0.22,1.88) |
| Race/ethnicity | ||||
| White | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 1.67 (1.02,2.72) | 1.31 (0.78,2.17) | 1.02 (0.60,1.74) | 0.89 (0.52,1.54) |
| Hispanic | 1.97 (1.06,3.68) | 1.69 (0.89,3.20) | 1.37 (0.71,2.65) | 1.29 (0.66,2.54) |
| Asian | 1.35 (0.66,2.77) | 1.25 (0.61,2.59) | 1.23 (0.59,2.54) | 1.16 (0.55,2.43) |
| Other | 1.33 (0.59,2.98) | 1.18 (0.52,2.67) | 0.95 (0.41,2.19) | 0.88 (0.37,2.08) |
| Immigrant | 0.75 (0.49,1.16) | 0.78 (0.50,1.21) | 0.70 (0.45,1.09) | 0.72 (0.46,1.13) |
| Parous | 1.22 (0.86,1.73) | 1.12 (0.78,1.59) | 1.14 (0.79,1.64) | 1.05 (0.72,1.51) |
| Household income, mid‐pregnancy | ||||
| ⩽20000 | 1.57 (0.90,2.77) | 1.33 (0.74,2.37) | 1.25 (0.69,2.26) | |
| 20001–40000 | 1.63 (0.91,2.93) | 1.38 (0.76,2.52) | 1.37 (0.75,2.52) | |
| 40001–70000 | 0.71 (0.46,1.10) | 0.76 (0.49,1.19) | 0.81 (0.51,1.37) | |
| >70000 | 1.00 | 1.00 | 1.00 | |
| Partnership status, early pregnancy | ||||
| Married | 1.00 | 1.00 | ||
| Cohabitating | 1.43 (0.77,2.65) | 1.29 (0.69,2.41) | ||
| Not married or cohabitating | 2.34 (1.26,4.35) | 2.16 (1.13,4.12) | ||
| Pregnancy intention, early pregnancy | ||||
| Trying | 1.00 | 1.00 | ||
| Not trying, but glad | 1.16 (0.77,1.73) | 1.13 (0.75,1.71) | ||
| Not wanted | 2.31 (1.29,4.16) | 2.05 (1.12,3.75) | ||
| Family/friends support , mid‐pregnancy (per unit, 7 unit range) | 0.86 (0.79,0.94) | |||
| Partner support, mid‐pregnancy (per unit, 7 unit range) | 0.91 (0.82,1.02) | |||
We further adjusted for partnership status and pregnancy intention in model 3. Lack of a spouse or cohabitating partner and unwanted pregnancy doubled the risk of second trimester depressive symptoms. Accounting for these factors in model 3 reduced the risk associated with young motherhood and minority status. Further adjustment for maternal education, cigarette smoking, maternal prepregnancy body mass index, or a history of depressive symptoms or history of depression did not materially change the associations of race/ethnicity, immigrant status, age, or household income with antenatal depressive symptoms. Antenatal maternal employment status was not a predictor of antenatal depressive symptoms as employed women, whether they were seeking work (OR = 1.12, 95% CI 0.64, 1.95) or not (OR = 0.90, 95% CI 0.47, 1.72).
We considered first trimester social support from family/friends and from partner (model 4), both of which were associated with reduced risk of antenatal depressive symptoms in the second trimester, although only support from family and friends was statistically significantly related to antenatal depressive symptoms. Adjustment for social support dampened, but did not eliminate, the risk of antenatal depressive symptoms associated with being unpartnered or carrying an unwanted pregnancy. There was little evidence of race or age associations in model 4.
A history of any depressive symptoms before pregnancy (age adjusted OR = 4.51, 95% CI 4.24, 4.80) and of diagnosed or treated depression (age adjusted OR = 4.07, 95% CI 3.76, 4.40) were potent risk factors for antenatal depressive symptoms. We reasoned that a history of depression or depressive symptoms before pregnancy might adversely influence partnership status or pregnancy intention, each of which was associated with antenatal depressive symptoms in this cohort. To examine whether these factors affected risk of antenatal depressive symptoms independent of any association with prepregnancy depression, we reran model 3 among the group of 1353 women who reported no history of depression or depressive symptoms before pregnancy, among whom 84 (6%) reported a first onset of depressive symptoms during pregnancy. We found slightly weaker associations of partnership status (OR = 2.08; 0.90, 4.84) and unwanted pregnancy (1.89; 0.88, 4.09) with risk of antenatal depressive symptoms among women with no history of depression before pregnancy, compared with the full cohort (ORs of 2.34 and 2.31, respectively, in model 3 in table 2).
Predictors of postpartum depressive symptoms
Table 3 shows models built to identify sociodemographic predictors of depressive symptoms at six months postpartum. As with antenatal depression, we again found increased risk of postpartum depressive symptoms among the youngest mothers (model 5). While black and Hispanic mothers seemed to be at higher risk of postpartum depressive symptoms, these associations lacked statistical significance. Having delivered a low birthweight infant conferred a nearly threefold higher risk of postpartum depressive symptoms; this explained a small portion of the increased risk associated with young maternal age and minority status (model 6). In model 7, we added a measure of financial hardship that more than tripled the risk of postpartum depressive symptoms. Household income (model 7) had an inconsistent association with postpartum depressive symptoms (whether or not the financial hardship term was in the model). These financial factors explained all of the apparent higher risk among black mothers and much of the higher risk seen among Hispanic mothers, and a portion of the risk associated with young motherhood. Partnership status and pregnancy intention were not associated with postpartum depressive symptoms. Further adjustment for cigarette smoking, breast feeding, return of menses, infant sleeping hours, postpartum physical symptoms (haemorrhoids, incontinence, varicose veins, pain during sex, sciatica, sore breasts, or back pain), postpartum body mass index, or history of depression of depressive symptoms before or during the pregnancy did not materially change these findings. While mothers who were not working outside the home and mothers on maternity leave were at the same risk of postpartum depressive symptoms as employed mothers, those who were looking for work were more likely to have postpartum depressive symptoms (OR = 2.35; 1.00, 5.49, compared with employed mothers).
Table 3 Odds ratios (95% confidence intervals) for risk factors for depressive symptoms at six months postpartum, Project Viva.
| Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | |
|---|---|---|---|---|---|
| Maternal age | |||||
| <23 | 2.37 (1.05,5.38) | 2.27 (0.99,5.18) | 1.43 (0.57,3.57) | 1.45 (0.54,3.92) | 1.47 (0.52,4.22) |
| 23–29 | 0.86 (0.49,1.52) | 0.85 (0.48,1.51) | 0.71 (0.39,1.27) | 0.69 (0.38,1.26) | 0.69 (0.37,1.27) |
| 30–34 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 35–39 | 0.93 (0.55,1.59) | 0.95 (0.56,1.62) | 1.02 (0.59,1.74) | 1.06 (0.61,1.81) | 0.92 (0.53,1.60) |
| 40+ | 0.75 (0.22,2.53) | 0.80 (0.24,2.68) | 0.85 (0.25,2.87) | 0.88 (0.26,3.01) | 0.93 (0.27,3.22) |
| Race/ethnicity | |||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 1.62 (0.83,3.15) | 1.58 (0.81,3.08) | 1.01 (0.50,2.06) | 0.92 (0.44,1.91) | 0.78 (0.37,1.63) |
| Hispanic | 1.74 (0.78,3.89) | 1.62 (0.72,3.66) | 1.26 (0.54,2.93) | 1.17 (0.50,2.76) | 1.05 (0.44,2.51) |
| Asian | 0.61 (0.17,2.15) | 0.54 (0.15,1.96) | 0.54 (0.15,1.95) | 0.51 (0.14,1.88) | 0.43 (0.11,1.61) |
| Other | 2.32 (0.96,5.62) | 2.17 (0.88,5.36) | 1.79 (0.69,4.64) | 1.64 (0.62,4.32) | 1.88 (0.69,5.14) |
| Immigrant | 1.15 (0.63,2.11) | 1.17 (0.63,2.15) | 1.17 (0.63,2.19) | 1.14 (0.61,2.12) | 1.11 (0.58,2.09) |
| Parous | 0.91 (0.59,1.41) | 0.93 (0.60,1.45) | 0.84 (0.54,1.31) | 0.80 (0.51,1.27) | 0.79 (0.50,1.26) |
| Low birth weight | 2.75 (1.33,5.66) | 3.19 (1.50,6.76) | 3.29 (1.55,7.00) | 2.88 (1.44,5.46) | |
| Household income postpartum | |||||
| ⩽20000 | 0.82 (0.35,1.87) | 0.82 (0.35,1.90) | 0.76 (0.31,1.82) | ||
| 20001–400000 | 1.49 (0.72,3.09) | 1.40 (0.67,2.95) | 1.42 (0.66,3.06) | ||
| 40001–70000 | 0.61 (0.36,1.03) | 0.62 (0.37,1.04) | 0.67 (0.39,1.14) | ||
| >70000 | 1.00 | 1.00 | 1.00 | ||
| Financial hardship postpartum | 3.59 (1.92,6.72) | 3.54 (1.87,6.72) | 2.80 (1.44,5.46) | ||
| Partnership status, postpartum | |||||
| Married | 1.00 | 1.00 | |||
| Cohabitating | 0.56 (0.21,1.53) | 0.44 (0.16,1.20) | |||
| Not married or cohabitating | 1.46 (0.63,3.38) | 1.11 (0.45,2.71) | |||
| Pregnancy intention, early pregnancy | |||||
| Trying | 1.00 | 1.00 | |||
| Not trying, but glad | 1.16 (0.70,1.90) | 1.12 (0.67,1.86) | |||
| Not wanted | 1.89 (0.85,4.20) | 1.55 (0.68,3.53) | |||
| Family/friends support, postpartum (per unit, 7 unit range) | 0.81 (0.73,0.90) | ||||
| Partner support, postpartum (per unit, 7 unit range) | 0.85 (0.75,0.96) | ||||
Although partnership status did not seem to determine postpartum depressive symptoms, social support from a partner had a strong protective association with postpartum depressive symptoms, as did social support from family and friends (model 8). When these social support factors were added to the model (model 9), the risk associated with hardship decreased considerably, suggesting that the impact of financial hardship on postpartum depressive symptoms may be partly explained by low social support that may accompany or predate hardship.
A history of undiagnosed depressive symptoms before pregnancy (OR = 3.37; 2.14, 5.29), diagnosed or treated pre‐pregnancy depression (OR = 3.82; 2.31, 6.31) or antenatal depressive symptoms (OR = 6.78; 4.07, 11.31) conferred a several‐fold higher risk of postpartum depressive symptoms. When we ran model 8 among the 1051 mothers with no history of depressive symptoms before or during pregnancy, financial hardship remained a risk factor (OR = 4.05; 1.6, 9.83) for postpartum depressive symptoms, but low birthweight did not (OR = 1.45; 0.40,5.28).
Discussion
We saw a 9% prevalence of antenatal depressive symptoms, which is on the lower side of the 9% to 15% prevalence of antenatal depressive symptoms reported by other studies using the EPDS.31,34 Other studies, using a variety of depression assessment tools, have reported antenatal depression prevalences of 9%–28% for predominantly middle class samples11,19,35 and 25%–50%11,19,36 for low income populations. The somewhat lower prevalence in our population probably reflects both the specificity of the EPDS and the comparatively high socioeconomic position of our cohort.
Although our study is one of the first to report a higher prevalence of antenatal depressive symptoms among minority and young mothers, these associations were largely explained by differences in income, partnership status, and pregnancy intention. We saw a roughly 30% higher prevalence of antenatal depressive symptoms among women with household incomes below $40 000, although this did not reach statistical significance. However, the higher risk is consistent with several studies20,35,37 that have reported high prevalence of antenatal depression among women of lower socioeconomic position. We also found a twofold increased risk of antenatal depressive symptoms with unwanted pregnancy, which we believe has not been previously examined. By far the most powerful risk factor for depressive symptoms during pregnancy was a history of prior depression, which conferred a fourfold increased risk of antenatal depressive symptoms, similar to that reported in a small study of Norwegian mothers.1
Few studies have examined race/ethnicity as a risk factor for postpartum depression. As with antenatal depression, the higher prevalence of postpartum depressive symptoms that we saw among minority mothers was explained by financial hardship. Although some studies report no associations of postpartum depression with socioeconomic position,11,39 others have found that financial difficulties,19,29 unemployment,11,38 or low education36 are more prevalent among women with postpartum depression. We saw a nearly threefold increased risk of postpartum depression among mothers who had low birthweight infants. One study reported increased risk of postpartum depression with poor infant health,36 but another found reduced risk of depression among women who had delivered before term.29 The single strongest risk factor for postpartum depressive symptoms was depressive symptoms during pregnancy, as has been seen consistently.34,40
What is known on this topic
Although major depression is associated with low socioeconomic position, available data are contradictory regarding the association of sociodemographic factors with antenatal and postpartum depression.
What this paper adds
Our report confirms that women living in disadvantage are at higher risk of depressive symptoms during the childbearing year. Maternal minority status does not confer risk independent of its socioeconomic correlates, a question that had never been satisfactorily addressed.
To the extent that depressive symptoms before, during, and after pregnancy represent a consistent underlying depressive syndrome, it is possible that depressive symptoms preceding pregnancy might increase social and economic risk (such as unemployment or lack of a partner); if this were the case, these social and economic risks might seem as spurious “predictors” of antenatal and postpartum depression. To our knowledge, no study has examined whether these risk factors predict depressive symptoms among women with no history of depressive symptoms. Lack of a partner and unwanted pregnancy remained associated with antenatal depressive symptoms among women with no history of depressive symptoms, suggesting that the risks associated with partnership status and pregnancy intention are not spurious artefacts of an antecedent depressive symptoms. For postpartum depressive symptoms, financial hardship was a risk factor whether or not women had experienced prior depressive symptoms, suggesting that poverty precedes postpartum depression, rather than the alternative that depression leads to poverty.
This study had several limitations. Chief among these is our reliance on a self reported screen of depressive symptoms, rather than clinician diagnosis. Although the EPDS has been validated in a broad range of populations,41 it remains possible that cultural and/or economic factors may have caused women to over‐report or under‐report depressive symptoms. Social desirability bias may particularly affect minority42 and lower socioeconomic participants,43 leading them to under‐report symptoms of depression,42 and us to underestimate associations between these factors and depressive symptoms. The timing of exposures and the onset of depressive symptoms is not established for every exposure; in particular, the examination of social support and depression is effectively cross sectional and should be interpreted with caution (as in most other studies). While 23% of the cohort who responded to the mid‐pregnancy questionnaire did not return the postpartum questionnaire, the proportion responding was similar among those with (75%) and without (77%) depression mid‐pregnancy. This suggests that non‐response neither substantially reduced our estimate of the prevalence of depression, nor created bias in ascertaining predictors of depression. If anything, the higher loss to follow up among minority and disadvantaged mothers might have caused us to slightly underestimate associations between lower socioeconomic status and depressive symptoms.
Policy implications
Because of their increased risk of antenatal and postpartum depression, women facing socioeconomic hardship and those with poor pregnancy outcomes should be targeted for depression screening, prevention, and treatment.
In summary, we found that maternal race/ethnicity is not an independent predictor of antenatal or postpartum depressive symptoms. Instead, the apparently higher risk among minority women seems to result from financial hardship and, for postpartum depressive symptoms, poor pregnancy outcome. The higher risk of antenatal and postpartum depressive symptoms associated with young maternal age is largely explained by financial hardship, unwanted pregnancy, and lack of a partner. The fact that financial hardship and partnership status predicted depressive symptoms among women with no history of depressive symptoms suggests that these factors are likely to predate, and perhaps cause, depression during pregnancy and the postpartum.
Acknowledgements
We thank the participants of Project Viva and the clinicians at Harvard Vanguard Medical Associates who made this study possible.
Footnotes
Funding: this work is supported by the National Institute of Mental Health grants MH068596 (Rich‐Edwards), MH 56217 (McLaughlin), and K24 HL68041 (Gillman).
Competing interests: none declared.
This study was approved by the Human Studies Committee of Harvard Pilgrim Health Care, Boston, MA, USA.
References
- 1.Depression Guideline Panel Depression in primary care. Vol 1. Detection and diagnosis. Clinical practice guideline, number 5. Rockville, MD: US Department of Health and Human Services, Agency for Health Care Policy and Research, 1993
- 2.Weinberg M K, Tronick E Z. The impact of maternal psychiatric illness on infant development. J Clin Psychiatry 19985953–61. [PubMed] [Google Scholar]
- 3.Murray L, Sinclair D, Cooper P.et al The socioemotional development of 5‐year‐old children of postnatally depressed mothers. J Child Psychol Psychiatry 1999401259–1271. [PubMed] [Google Scholar]
- 4.Luomo I, Tamminen T, Kaukonen P.et al Longitudinal study of maternal depressive symptoms and child well‐being. J Am Acad Child Adolesc Psychiatry 2001101367–1374. [DOI] [PubMed] [Google Scholar]
- 5.Sinclair D, Murray M L. Effects of postnatal depression on children's adjustment to school. Br J Psychiatry 199817258–63. [DOI] [PubMed] [Google Scholar]
- 6.Yonkers K A, Chantilis S J. Recognition of depression in obstetric/gynecology practices. Am J Obstet Gynecol 1995173632–638. [DOI] [PubMed] [Google Scholar]
- 7.Kessler R C. Stress, social status, and psychological distress. J Health Soc Behav 197920259–272. [PubMed] [Google Scholar]
- 8.Weissman M M, Leaf P J, Tischler G L.et al Affective disorders in five United States communities. Psychol Med 198818141–153. [DOI] [PubMed] [Google Scholar]
- 9.O'Hara M W, Neunaber D, Zeboski E M. Prospective study of postpartum depression: prevalence, course and predictive factors. J Abnorm Psychol 198493158–171. [DOI] [PubMed] [Google Scholar]
- 10.Gotlib I H, Whitten V E, Wallace P M.et al Prospective investigation of postpartum depression: factors involved in onset and recovery. J Abnorm Psychol 1991100122–132. [DOI] [PubMed] [Google Scholar]
- 11.Hobfoll S E, Ritter C, Lavin J.et al Depression prevalence and incidence among inner‐city pregnant and postpartum women. J Consult Clin Psychol 199563445–453. [DOI] [PubMed] [Google Scholar]
- 12.Stowe Z N, Nemeroff C B. Women at risk for postpartum‐onset major depression. Am J Obstet Gynecol 1995143639–645. [DOI] [PubMed] [Google Scholar]
- 13.O'Hara M W. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 198646569–573. [DOI] [PubMed] [Google Scholar]
- 14.O'Hara M W, Zeboski E M, Phillips L H. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 1990993–15. [DOI] [PubMed] [Google Scholar]
- 15.Gotlib I H, Whiffen V, Mount J.et al Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol 198957269–274. [DOI] [PubMed] [Google Scholar]
- 16.Watson J P, Elliott S A, Rugg A J.et al Psychiatric disorder in pregnancy and the first postnatal year. Br J Psychiatry 1994144453–462. [DOI] [PubMed] [Google Scholar]
- 17.Cutrona C E. Social support and stress in the transition to parenthood. J Aborm Psychol 19849378–90. [DOI] [PubMed] [Google Scholar]
- 18.Campbell S B, Cohn J F. Prevalence and correlates of postpartum depression in first time mothers. J Abnorm Psychol 1991100594–599. [DOI] [PubMed] [Google Scholar]
- 19.Seguin L, Potvin L, St‐Dennis M.et al Depressive symptoms in the late postpartum among low socioeconomic women. Birth 199926157–163. [DOI] [PubMed] [Google Scholar]
- 20.Seguin L, Potvin L, St‐Dennis M.et al Chronic stressors, social support, and depression during pregnancy. Obstet Gynecol 199585583–589. [DOI] [PubMed] [Google Scholar]
- 21.Williams D R, Yu Y, Jackson J.et al Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol 19972335–351. [DOI] [PubMed] [Google Scholar]
- 22.Williams D R, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol 199521349–386. [Google Scholar]
- 23.Blazer D G, Kessler R C, McGonagle K A.et al The prevalence and distribution of major depression in a national community sample: the national comorbidity survey. Am J Psychiatry 1994151979–986. [DOI] [PubMed] [Google Scholar]
- 24.Rich‐Edwards J W, Krieger N, Majzoub J.et al Maternal experiences of racism and violence as predictors of preterm birth: rationale and study design. Paediatr Perinat Epidemiol 200115124–135. [DOI] [PubMed] [Google Scholar]
- 25.Gillman M W, Rich‐Edwards J, Rifas‐Shiman S L.et al Maternal age and other predictors of newborn blood pressure. J Pediatr 2004144240–245. [DOI] [PubMed] [Google Scholar]
- 26.Cox J L, Holden J M, Sagovsky R. Detection of postnatal depression. Br J Psychiatry 1987150782–786. [DOI] [PubMed] [Google Scholar]
- 27.Murray D M, Cox J L. Screening for depression during pregnancy with the Edinburgh depression scale. J Reprod Infant Psychol 199011119–125. [Google Scholar]
- 28.Thorpe K. A study of the Endinburgh postnatal depression scale for use with parent groups outside the postpartum period. J Reprod Infant Psychol 199311119–125. [Google Scholar]
- 29.Righetti‐Veltema M, Conne‐Perreard E, Bousquet A.et al Risk factors and predictive signs of postpartum depression. J Affective Disord 199849167–180. [DOI] [PubMed] [Google Scholar]
- 30.Warner R, Appleby L, Whitton A. Demographic and obstetric risk factors for postnatal pyschiatric morbidity. Br J Psychiatry 1996168605–611. [DOI] [PubMed] [Google Scholar]
- 31.Evans J, Heron J, Francomb H.et al Cohort study of depressed mood during pregnancy and after childbirth. BMJ 2001323257–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Turner R J, Grindstaff C F, Phillips N. Social support and outcome in teenage pregnancy. J Health Soc Behav 19903143–57. [PubMed] [Google Scholar]
- 33.Little R, Rubin D B.Statistical analysis with missing data. New York: Wiley, 2005209–222.
- 34.Heron J, O'Connor T G, Evans J.et al The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affective Disord 20048065–73. [DOI] [PubMed] [Google Scholar]
- 35.Marcus S E, Drury T F, Brown L J.et al Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988–1991. J Dent Res 199675684–695. [DOI] [PubMed] [Google Scholar]
- 36.Chung E K, McCollum K F, Elo I T.et al Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics 2004113e523–e529. [DOI] [PubMed] [Google Scholar]
- 37.Bolton H L, Hughes P M, Turton P.et al Incidence and demographic correlates of depressive symptoms during pregnancy in an inner London population. J Psychosom Obstet Gynaecol 199819202–209. [DOI] [PubMed] [Google Scholar]
- 38.Eberhard‐Gran M, Tambs K, Opjordsmoen S.et al Depression during pregnancy and after delivery: a repeated measurement study. J Psychosom Obstet Gynaecol 20042515–21. [DOI] [PubMed] [Google Scholar]
- 39.Josefsson A, Angelsioo L, Berg G.et al Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet Gynecol 200299223–228. [DOI] [PubMed] [Google Scholar]
- 40.O'Hara M W, Swain A M. Rates and risk of postpartum depression—a meta‐analysis. Int Rev Psychiatry 1996837–54. [Google Scholar]
- 41.Cox J, Holden J M.Perinatal mental health: a guide to the Edinburgh postnatal scale. London: Gaskell, 2003
- 42.Bardwell W A, Dimsdale J E. The impact of ethnicity and response bias on the self‐report of negative affects. Journal of Applied Biobehavioral Research 2001627–38. [Google Scholar]
- 43.Welte J W, Russel M. Influence of socially desirable responding in a study of stress and substance abuse. Alcohol Clin Exp Res 199317758–761. [DOI] [PubMed] [Google Scholar]