Abstract
Background
Community‐care networks are a partnership between the local police force, housing corporations, general social services, specialised home care and mental healthcare services. The networks were set up to improve the healthcare for patients with (chronic) psychiatric problems through local cooperation between different agencies operating in underprivileged areas.
Objective
To evaluate the effects of community‐care networks on psychiatric emergency contacts, hospitalisation and involuntary admission.
Design
An ecological intervention design was used, comparing neighbourhoods with and without a community‐care network. Mean numbers and standardised ratios of psychiatric emergency contacts, hospitalisation rates and involuntary admissions were assessed over a 10‐year period, covering the early stages and the years in which community‐care networks were fully operational.
Setting
Underprivileged neighbourhoods in the city of Rotterdam, The Netherlands.
Patients
Inhabitants aged 20–64 years living in these neighbourhoods.
Results
Standardised ratios for contact with psychiatric emergency services were higher in the neighbourhoods where community‐care networks were set up (standardised ratios = 137, 95% CI 121 to 145 in the network neighbourhoods vs standardised ratios = 107, 95% CI 96 to 119 in the control neighbourhoods). Number of admissions and standardised ratios for involuntary admissions were lower in the community‐care network neighbourhoods than in the control neighbourhoods (standardised ratios = 123, 95% CI 95 to 157 vs standardised ratios = 152, 95% CI 120 to 191).
Conclusions
Community‐care networks have a significant impact on the use of mental healthcare services. These networks may be an important tool in the prevention of involuntary admissions.
In recent years, the number of patients receiving mental healthcare in The Netherlands has grown.1,2 Even so, there are patients in need of care for a range of problems, such as severe mental illness, addiction, somatic problems, and financial and social problems, who have no contact with mental healthcare services or who actively avoid mental healthcare.3 According to the Health Council of The Netherlands, the number of people with multiple problems is increasing because of the marginalisation of vulnerable people in the job and housing markets, and because of a lack of specific and appropriate interventions to help underprivileged patients who have mental illnesses. The Dutch Health Council states that coordinating the efforts of different agencies may help bridge the gulf between supply and demand for healthcare resources among patients with multiple problems.4
In many healthcare projects, a coordinator or case manager is responsible for arranging and coordinating the necessary care for a patient. The role of the coordinator can range from a “care broker's function” to a role in which the coordinator is primarily responsible for treatment or supervision.5,6,7 In The Netherlands, healthcare projects for patients with chronic psychiatric problems are in the form of outreach programmes or assertive community treatment programmes.8,9,10,11
The City Council of Rotterdam, the second largest city in The Netherlands, adopted a more front‐end approach and has set up community‐care networks in underprivileged neighbourhoods.12,13 These networks distinguish themselves from other coordinated care interventions in that, in addition to healthcare agencies, they also include welfare services, housing corporations and the local police force. The participants of such a network bear joint responsibility for the (coordination of) care for people with multiple problems living in the area, with emphasis on the detection and prevention of new problems rather than on supporting patients already in contact with specialist services. Process evaluations of community‐care networks have shown that the feeling of being supported, not having to face problematic situations alone, makes network participants more tenacious in establishing contact with patients who refuse help.14,15 In an earlier study, we found a decrease in the number of eviction orders and in the number of notifications of problematic situations to the local health authority in areas with a community‐care network.16 In addition, patients benefited from the supervision provided by the community‐care network, showing improvements in health and social functioning as measured by the Goal Attainment Functioning Score and the Health of the Nation Outcome Scales.17,18 In particular, improvements have been achieved in areas such as living conditions, social contacts, depression, and other mental and behavioural problems.13,16
To evaluate the effectiveness of community‐care networks, we monitored the use of mental health services, both inpatient and outpatient services, over 10 years. We hypothesised that:
neighbourhoods with community‐care networks make more use of emergency psychiatric services because early detection of problematic situations might increase the need for immediate action;
the number of patients admitted to a psychiatric hospital decreases as the health situation and social functioning of patients improve under community‐care network supervision; and
the rate of acute involuntary admissions is lower in neighbourhoods with community‐care networks as a result of early involvement of emergency psychiatric services and community support systems.
Methods
Type of intervention
Dutch healthcare consists of a mix of public and private services in connection with a mixed system of insurance and healthcare funding. Apart from public university hospitals, Dutch hospitals are managed on a private non‐profit basis. Most of the specialist care is organised by hospitals. General practitioners mainly work in private practices and play an important gate‐keeping role in access to specialist services, including mental health services, and alcohol and drug clinics. Social insurance covers a statutory package and is mandatory for those earning below an income threshold (about €30 000, US$38 000, £20 000). In addition, the Exceptional Medical Expenses Act provides cover for exceptional care and uninsurable risks (eg, involuntary admission or medical expenses for handicapped people). Social welfare services constitute an adjoining set of arrangements to support people who have social or financial problems. Although there have been many changes in the Dutch healthcare system in recent years, medical and social welfare services on the whole have been free from charge at point of use and readily available in underprivileged areas also. However, despite the availability of healthcare and social welfare services, there is a “multiple‐problem group” that does not use these facilities. Instead of adding yet another service, community‐care networks combine and reinforce the activities of different agencies operating in the same neighbourhood.
Community‐care networks are a partnership between the local police force, housing corporations, general social services, specialised home care and mental healthcare services. The backbone of the community‐care network is a network coordinator, who is often a community psychiatric nurse. When a patient is reported by one of the network partners, the network participants gather relevant information and (if necessary) the coordinator starts intensive outreach to contact the person. Next, a plan of action is drawn up, if possible in consultation with the patient. The coordinator monitors the implementation of the plan and ensures that everyone adheres to the agreed strategy. As soon as possible, community‐care network involvement is scaled down or the responsibility is transferred to the most appropriate agency, usually a welfare agency or a mental healthcare service.
The first community‐care network was set up in 1992 and after a first wave in the mid‐1990s the number has grown to >25 networks at present. In the starting period, the City Council of Rotterdam reserved a budget to develop the network approach in underprivileged neighbourhoods. On the Municipal Health Department's advice, the financial support was allocated to neighbourhoods where relevant partners submitted an application showing commitment to adopt the community‐network approach. This study focused on the first series of seven networks.
Study design
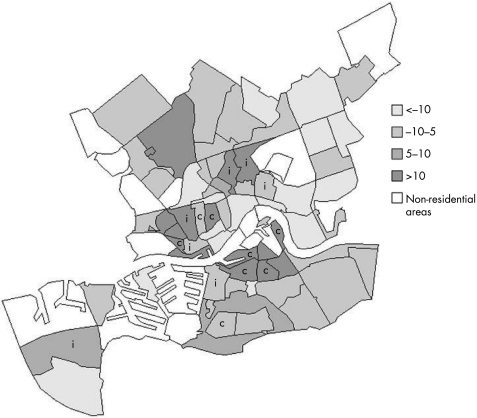
The study was set up as an ecological intervention comparing neighbourhoods with and without a community‐care network. The seven neighbourhoods with intervention (intervention neighbourhood) were matched with eight control neighbourhood regarding geographical location (in case of potential differences in primary healthcare and social welfare services) and socioeconomic position (because more mental health problems are reported in underprivileged areas).19,20 For every intervention neighbourhood, we inspected the socioeconomic position of adjoining areas. These areas had to be within the catchment area of the local departments of community services for the neighbourhood with a community‐care network. To match neighbourhoods by socioeconomic position we used the Jarman index or “underprivileged area score”.21 This score is a weighted average of eight census variables that were considered by a poll of British general practitioners to be important factors in creating high workloads—high positive scores indicate high relative demand. Some of the items were adjusted because they were not relevant in the Dutch context (eg, percentage of households headed by a person born in the New Commonwealth or in Pakistan). The index for the year 1995 was calculated on the basis of the items and values shown in table 1; index scores for different years are highly correlated (for the years 1993 and 1997, the mean (SD) change was 2.6 (2.4); Spearman's r = 0.91). Because the combination of matching criteria could not always strictly be applied, practical considerations led to the selection of eight control areas (fig 1). This procedure in part accounts for differences in mean scores and standard deviations for some of the items listed in table 1. The mean (SD) Jarman score was 9.8 (4.74) for the intervention areas and 12.2 (7.37) for the control areas. Although these scores differed slightly, they were 3–4 times higher than the overall score for the other residential areas (2.8), showing that the targeted neighbourhoods were underprivileged areas.
Table 1 Underprivileged area score items, weighted z score and number of inhabitants for the intervention and control areas (demographic data 1995, Rotterdam is the reference area).
| Subjects | Reference area | Weight | Intervention areas (n = 7) | Control areas (n = 8) | ||
|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | |||
| Elderly living alone (%) | 8.3 | 6.62 | 5.2 | 3.4–8.5 | 5.8 | 3.4–13.1 |
| Children <5 years (%) | 6.3 | 4.64 | 7.5 | 5.9–9.0 | 7.2 | 4.7–9.3 |
| Unskilled socioeconomic groups (%)* | 20.9 | 3.74 | 23.4 | 19.0–32.8 | 27.2 | 17.8–36.1 |
| Unemployed (%) † | 17.3 | 3.34 | 24.1 | 20.5–27.4 | 23.9 | 15.9–28.9 |
| One‐parent families (%) | 10.9 | 3.01 | 15.1 | 10.6–17.7 | 14.3 | 10.4–21.2 |
| Dwellings without bath (%) | 11.8 | 2.88 | 17.7 | 1.0–29.6 | 19.5 | 1.0–40.0 |
| Change of address ‡ | 38.1 | 2.68 | 62.4 | 39.7–95.5 | 68.8 | 59.1–92.5 |
| Ethnic groups (%) § | 40.1 | 2.5 | 53.6 | 38.7–66.8 | 59.1 | 33.8–75.9 |
| UPA score (weighted z score) | 2.8 | 9.8 | 3.7–16.7 | 12.2 | −2.2–20.9 | |
| Inhabitants (aged 20–64 years), n | 369824 | 9718 | 7967 | |||
UPA, underprivileged.
*Primary school is the highest education level.
†Percentage of the working population.
±Mobility score combines number of births, deaths, establishments, number of people leaving the area and change of address within the area.
§People born outside The Netherlands, the rich, western European and North‐American countries not included.
Figure 1 Neighbourhood variation in underprivileged area score (Jarman index) for Rotterdam 1995, i, intervention; c, control area.
Use of mental healthcare was monitored at the neighbourhood level for the years 1992–2001, covering the period from the introduction of community‐care networks to their being fully operative. Owing to the practical setting of the study, it proved difficult to pinpoint the exact start and degree of implementation for each community‐care network. In practice, some degree of cooperation between relevant partners at the neighbourhood level was a precondition for funding. At the end of 1995 four networks had started, and in early 1998 all seven community‐care networks were fully operational. Therefore, we expected differences in the average use of emergency psychiatric services, hospitalisation and involuntary admissions to start to show in 1999.
Data
The size and nature of the use of mental health services and the flow of patients between services were monitored by the psychiatric case register for the Rotterdam region.22,23 This case register covers all contacts of the Rotterdam inhabitants with mental health services, with the exclusion of private psychiatry or psychotherapy practices; however, this is unlikely to affect findings since private practices form only a small part of the outpatient care and play no role in emergency psychiatry or hospital admissions. We restricted analyses to people aged 20–64 years because in The Netherlands, child psychiatry and psychogeriatric care are closely interwoven with other youth services and facilities for elderly people, including emergency services and inpatient care, and thus could bias the mental healthcare indicators. For similar reasons, we excluded data on the use of alcohol and drug (outpatient) services. We also excluded the data on long‐stay patients or those with previous psychiatric problems living in sheltered or other community accommodation, because service use is higher in these facilities and this would inflate care indicators at the neighbourhood level. Demographic and other administrative data were obtained from the Centre for Research and Statistics of the municipality of Rotterdam. Ethical approval was secured from a review board representing all participating services.23
Standardised service use ratios
Detailed demographic information enabled us to correct for the geographic variation in the use of mental health services that is the result of the size and differences in age and sex of the neighbourhood population. In addition to rates per 1000 of the population, we used indirect standardisation relating the actual number of patients in an area to the expected number, if the age‐and sex‐specific patterns of service use were that of the reference population. The reference values were calculated for the wider area (Rotterdam) for three broad sex and age groups (20–34, 35–54 and 55–64 years). In this way, we obtained the selected measures of service use as standardised hospitalisation ratios and standardised contact ratios. To focus on the effects of the community‐care network approach, we also calculated standardised service use ratios over the last 3 years of the study period (1999–2001). Confidence intervals (CI) were estimated using the Poisson process approximation.24
Results
Use of emergency psychiatric services
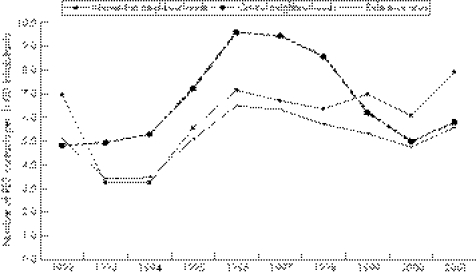
The number of patients in contact with emergency services was fairly constant in the region as a whole (about 3.0 per 1000 population). There was a small increase in the contact rate: from 5.1 contacts per 1000 in 1992 to 5.6 contacts per 1000 population in 2001. Figure 2 shows the differences in contact rates in the intervention neighbourhoods and in the control neighbourhoods. From 1995 onward the contact rates both for intervention and control neighbourhoods were higher than the overall contact rate. In the beginning of the observation period, the number of patients and the number of contacts per 1000 were higher in the control areas than in the intervention areas, but this reversed in 1999.
Figure 2 Number of contacts with psychiatric emergency services (PES) per 1000 inhabitants aged 20–64 years in neighbourhoods with and without a community‐care network in Rotterdam (reference area), 1992–2001.
The standardised contact ratio over the years 1999–2001 was significantly higher than the reference area for the intervention neighbourhoods: 137 (95% CI 121 to 145) vs 107 (95% CI 96 to 119) for the control neighbourhoods.
Hospitalisation rates
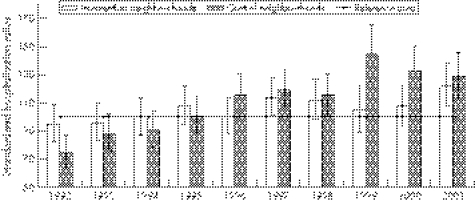
The number of patients per 1000 in the region decreased from 3.9 per 1000 inhabitants hospitalised in 1997 to 3.1 in 2001. The average hospitalisation rate in the period 1997–2001 was 3.5 per 1000 inhabitants in the intervention areas, and 4.0 per 1000 inhabitants in the control areas. The mean number of hospital days per patient was lower than the regional average in the intervention areas, and higher in the control areas (93 and 108, respectively, in 2001).
Figure 3 shows the standardised hospitalisation ratios over the years 1992–2001. Except at the start of the observation period, the hospitalisation ratios were lower in the intervention neighbourhoods than in the control neighbourhoods. Over the years 1999–2001, the standardised hospitalisation ratio was not higher for the intervention areas (standardised ratios = 108, 95% CI 100 to 118), whereas it was significantly higher in the control areas (standardised ratios = 135, 95% CI 125 to 145).
Figure 3 Standardised hospitalisation ratios and confidence intervals for neighbourhoods with and without a community‐care network (Rotterdam is the reference area, patients aged 20–64 years), 1992–2001.
Acute involuntary admissions
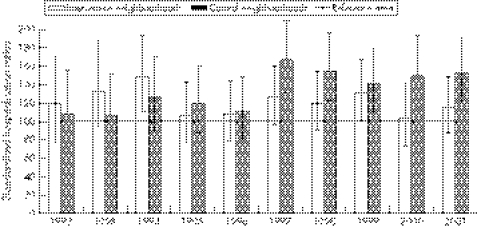
The rate of involuntary admissions among people aged 20–64 years almost doubled during the observation period, rising from 0.43 admissions per 1000 inhabitants in 1992 to 0.82 admissions per 1000 in 2001 (95% increase). The rate of involuntary admissions increased in this period by about 65% in the intervention areas and by 171% in the control areas. Although the rate of involuntary admission was initially higher in the intervention areas, after some years this pattern reversed.
Figure 4 shows the number of involuntary admissions as standardised ratios in relation to the reference area (Rotterdam = 100). From 1996 onwards, the number of involuntary admissions in the intervention areas was often that expected according to the age and sex distribution of the population, whereas it was higher in the control areas. The standardised involuntary admission ratio over the years 1999–2001 was significantly higher for the control areas: 148 (95% CI 128 to 169) vs 115 (95% CI 99 to 133) for the intervention areas.
Figure 4 Standardised involuntary admission ratios and confidence intervals for neighbourhoods with and without a community‐care network (Rotterdam is the reference area, patients aged 20–64 years), 1992–2001.
Discussion
Main results
After the implementation of community‐care networks, we found marked differences between intervention areas and matched control areas in trends and outcomes at the end of a 10‐year study period: more contacts with emergency psychiatric services and less (involuntary) admissions in the intervention neighbourhoods as compared with the control neighbourhoods.
Despite the fact that within the area the same procedures concerning involuntary admission were effective and the same alternative services were at hand, the rate of acute involuntary admissions was significantly higher in the neighbourhoods without a community‐care network.
What is already known
Although the number of patients with mental health problems is growing steadily, there is still a group of patients who have no contact with mental health services or who actively avoid care.
Many initiatives have been set up to reach these patients using assertive outreach and models of cooperation between various agencies.
Little is known about the effects of community‐care networks that use assertive outreach and coordinate care for people with complex problems.
Strengths and limitations of the study
Ecological intervention studies are difficult to implement because the practice of healthcare services and local policy change the research setting constantly. Because the initial development of community‐care networks in the mid‐1990s was bound by a fixed budget, we could analyse use of mental health services in a quasi‐experimental design. Geographical variation as a result of the size and differences in age and sex of the neighbourhood population could be corrected using detailed demographical information.
An important limitation of this study is that we did not include more recently established community‐care networks, and so we cannot exclude the possibility that the results were linked to the first batch of networks and their pioneering coordinators. Also, the difficulties we had in matching intervention areas with relevant control areas cannot be ignored. This may be accompanied by a different use of mental health services at a neighbourhood level. However, the mean underprivileged area scores for both intervention and control areas were much higher than the regional average. In addition, Jarman Index Scores were stable, and correlation coefficients for different years were high. This implies that it is unlikely that the results can be explained by increasing socioeconomic differences between intervention and control neighbourhoods.
What this paper adds
Community‐care networks seem to have a significant beneficial effect on psychiatric emergency service use, hospitalisation and involuntary admission.
Such community‐care networks may be particularly important in underprivileged neighbourhoods, improving the early identification of individuals with psychiatric problems.
Implications
The introduction of local community‐care networks seems to have a significant impact on the use of mental health services. This is consistent with the findings of the ACCESS Program (Access to Community Care and Effective Services and Support) in the US, which promoted service integration in nine experimental sites, along with funds to support assertive community treatment in both experimental sites and nine comparison community sites. The ACCESS study demonstrated that integration strategies are likely to improve collaboration and cooperation between a mental health agency and other agencies in the same community. However, compared with the results of assertive community treatment, the integration strategies did not improve patient outcomes, except for independent housing.25 Our study suggests that collaboration and cooperation between agencies may also help to prevent problems from escalating and to reduce the “need” for admission, especially involuntary admission.
The potential of coordinating the efforts of different agencies in local community‐care networks was acknowledged by the Dutch Commission on Socio‐Economic Differences in Health. The commission recommended that the government facilitate the spread of community‐care networks.26 The City Council of Rotterdam followed through on the community network initiative, and from 2001 this approach was expanded to all neighbourhoods.
Policy implications
Community‐care networks, in close cooperation with emergency psychiatric services, prevent problems from escalating and reduce the “need” for involuntary admission.
It may be that community‐care networks are effective because participants closely monitored the situation of the patient. Our study also suggests that close cooperation between the community‐care network and emergency psychiatric services is important. Possibly, this is the result of improved detection of problems through assertive outreach and a better communication between the community‐care network coordinators and staff of emergency services. The upward trend of emergency psychiatric service contacts in the areas with a community‐care network was mirrored by a downward trend in the control areas, which may be explained by the limited growth in the capacity of emergency psychiatric services over the years. At the end of the study period, there was a decline in the differences between the intervention and control neighbourhoods in the number of hospital admissions, both voluntary and involuntary. Perhaps more patients with chronic psychiatric problems who have been avoiding mental health care were contacted, inevitably leading to more hospital admissions. Moreover, community networks might evoke earlier hospital discharge and, consequently, more readmissions and emergency admissions (the mean number of hospital days per patients was lower in the intervention areas).
Additional research
Further studies should identify the key elements in this community‐network approach, because existing networks differ (eg, in coordinator training and full‐ or part‐time appointments). Cost–benefit analysis can contribute to public support for sufficient funding and a better understanding of possible cost‐reducing mechanisms. A preliminary cost analysis, in which we weighed the increase in use of psychiatric emergency services against the decrease in (involuntary) admissions, showed that it makes financial sense to invest in community‐care networks.
Acknowledgements
The research was funded by a grant from the Dutch Socio‐Economic Differences in Health Programme Commission. Data collection was in part funded by the Department of Health and the Municipal Health Service for the Rotterdam region.
Footnotes
Competing interests: None.
Ethical approval: Ethical approval was secured from a review board representing all participating services.
References
- 1.Pijl Y J, Kluiter H, Wiersma D. Increasing use of Dutch mental health care: an investigation. Soc Psychiatry Psychiatr Epidemiol 200035564–568. [DOI] [PubMed] [Google Scholar]
- 2.Kooi L, Sytema S, Wiersma D.et al GGZ onder druk? Verkenning met behulp van drie Nederlandse psychiatrische casusregisters [Mental health care under pressure? An exploration on the basis of three Dutch psychiatric case registers]. Maandblad Geestelijke Volksgezondheid 200055223–230. [Google Scholar]
- 3.Lourens J, Scholten C, Werf C van der, et al Verkommerden en verloederden. Een onderzoek naar de omvang en aard van de groep in Nederland [The withered and degenerated. An investigation into the size and nature of the group in The Netherlands]. Leiden: Research voor Beleid, 2002
- 4.Health Council of the Netherlands Care for nonhospitalized psychiatric patients in acute need. The Hague: Health Council of The Netherlands, 2004
- 5.Roovers S V, Wilken J P. Van zorgcoordinatie naar integrale zorg. De ontwikkeling van casemanagement [From coordinating care to integrated care. The development of casemanagement]. Passage 1997135–15. [Google Scholar]
- 6.Kroon H. Groeiende zorg. Ontwikkeling van casemanagement in de zorg voor chronisch psychiatrische patienten [Growing care. Development of case management in mental health care for chronic psychiatric patients]. Utrecht: Nationaal centrum Geestelijke volksgezondheid, 1996
- 7.Wolf J. Zorgvernieuwing in de GGZ: evaluatie van achttien zorgvernieuwingsprojecten [Modernization of mental health care: evaluation of eighteen modernization of care projects]. Utrecht: Trimbos‐instituut, 1995
- 8.Henselmans H. Bemoeizorg, ongevraagde hulp voor psychotische patienten [Assertive outreach, unsolicited help for psychotic patients]. Delft: Eburon, 1993
- 9.Stein L I, Santos A B.Assertive community treatment of persons with severe mental illness. New York: Norton, 1998
- 10.Allness D J, Knoedler W H.The pact model of community‐based treatment for persons with severe and persistent mental illnesses: a manual for pact start‐up. Arlington, VA: National Alliance For The Mentally ill, Anti‐Stigma Foundation, 1998
- 11.Mulder C L, Kroon H. eds. Assertive community treatment. Wageningen: Wetenschappelijke Uitgeverij Cure & Care Publishers, 2005
- 12.Poodt H D, Hijden E van der, Torn P van der Werken aan samenhang. Handboek voor het bevorderen van de samenhang in de sociaal‐psychiatrische zorg op wijkniveau. [Working at connections.A guide to improve cooperation in the community mental health care at the neighnouhood level]. Rotterdam: Municipal Health Service, 1997
- 13.Poodt H D, Wierdsma A I. Verleiden tot vertrouwen J. De resultaten van de inzet van lokale zorgnetwerken [Tempting to trust. Effects of the efforts of community‐care networks]. In: Stronks K, ed, Sociaal‐economische gezondheidsverschillen:van verklaren naar verkleinen (Socio‐economic inequalities in health:from explaining to reducing). Den Haag: ZON 199931–47.
- 14.Poodt H D. Het lokale zorgnetwerk Hoogvliet: een tussentijdse balans. [The community‐care network Hoogvliet: an interim audit report], Rotterdam: Municipal Health Service 1997
- 15.Hijden E van der Meneer, ik heb geen probleem en ben dus zeker niet gek. Een jaar openbare geestelijke gezondheidszorg in Crooswijk: een voortgangsrapportage. [Sir, I have no problem and therefore certainly not mentally ill.One year public mental health care in the neighbourhood Crooswijk:progress report]. Rotterdam: Municipal Health Service, 1993
- 16.Poodt H D, Wierdsma A I. Lokale zorgnetwerken: een kwestie van bemoeizorg? [Community‐care networks: a matter of assertive outreach] Tijdschr Gezondheidswetenschappen, 200179275–281. [Google Scholar]
- 17.Goldman H H, Skodol A E, Lave T R. Revising axis V for DSM IV: a review of measures of social functioning. Am J Psychiatry 19921491148–1156. [DOI] [PubMed] [Google Scholar]
- 18.Wing J K, Curtis R H, Beever A S. HoNOS. Health Of Nations Outcome Scales. Report on research and development. London: College Research, 1996
- 19.Thornicroft G. Social deprivation and rates of treated mental disorder. Developing statistical models to predict psychiatric service utilisation. Br J Psychiatry 1991158475–484. [DOI] [PubMed] [Google Scholar]
- 20.Reijneveld S A, Schene A H. Higher prevalence of mental disorders in socioeconomically deprived urban areas in The Netherlands: community or personal disadvantage? J Epidemiol Community Health 1998522–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarman B. Underprivileged areas: validation and distribution of scores. BMJ 19842891587–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horn GHMM ten. Giel R, Gulbinat W H.et al, eds. Psychiatric case registers in public health: a worldwide inventory 1960–1985 Amsterdam: Elsevier, 1986
- 23.Wierdsma A I, Dieperink C J, Koopmans G T. Regional mental health care information—the psychiatric case register Rotterdam region. In: Dekker WA, ed. Health Information Developments in The Netherlands. Amsterdam: The Dutch Association for Medical Records Administration, 1999
- 24.Liddell F D. Simple exact analysis of the standardised mortality ratio. J Epidemiol Community Health 19843885–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldman H H, Morrissey J P, Rosenheck R A. eds. Lessons from the evaluation of the ACCESS Program. Psychiatr Serv 200253967–969. [DOI] [PubMed] [Google Scholar]
- 26.Stronks K, Hulshof J. De kloof verkleinen. Theorie en praktijk van de strijd tegen sociaal‐economische gezondheidsverschillen. [Reducing Socio‐Economic Inequalities in Health. Final report and policy recommendations from the Dutch Programme Committee on Socio‐economic Inequalities in Health—second phase. Health Research and Development Council of The Netherlands]. Assen: Koninklijke Van Gorcum, 2001