Abstract
The hygiene hypothesis postulates that the increase in atopic diseases may in part be due to diminished exposure to microorganisms. But it is unknown which type of infection does render protection. An epidemiological study was conducted in Leipzig, Germany, and its rural county, involving 3347 school starters. Two types of infection were considered: (1) gastrointestinal colonisation (Helicobacter pylori detection using in vivo [13C] urea breath test) and (2) respiratory infections (physician‐diagnosed lower (bronchitis) and upper (common cold) respiratory infections). H pylori colonisation was selected because it is very common and plays an important role in gastrointestinal disorders. Atopic eczema was selected as the (allergic) target variable because of its high frequency in the age of the study participants. The results, adjusted for relevant confounders, showed a significant inverse association between H pylori infection and eczema (adjusted odds ratio (aOR) = 0.31, p = 0.006) in children not predisposed to atopy. In contrast, bronchitis increased the risk of eczema (aOR = 1.98, p<0.001). Bacterial digestive tract colonisation (infection) seems to protect against eczema in comparison with the effect of respiratory tract infections. The hygiene hypothesis may be better explained when gastrointestinal and respiratory infections are subtly differentiated.
The increasing prevalence of allergic disorders could be explained if they were prevented by microbial colonisation in early childhood.1 This so‐called hygiene hypothesis suggests that the allergy protective effect may be mediated by microbial agents2 associated with the presence of older siblings and the attendance at day care, but focused on airway infections.3,4,5,6,7,8 In other words, infections may have a protective effect on the development of allergic disorders. Others report on a protective effect following gastrointestinal infections.9,10,11,12,13 These facts lead to the question as to which pathway of infection (colonisation) has a greater effect on the protection of allergic disorders—the inhalative or the ingestive one. Determining this is of major importance in view of possible preventive measures. Until now, such comparative studies are very rare.
Methods
This study considered gastrointestinal and upper/lower respiratory tract infections. The study population (Leipzig Infection Study of School Starters study) is described elsewhere in detail.14 All preschool children eligible to enter grade one were included. The H pylori test (in vivo [13C] urea breath test) was administered at the time of the mandatory medical examinations and carried out by the medical staff of the respective local public health departments. The presented results base on 2487 participants including a parent completed questionnaire considering upper and lower respiratory tract infections and a UBT result.
The target variable was lifetime physician‐diagnosed eczema. The following questions were entered into the analyses: has a physician ever diagnosed (allergic) eczema, bronchitis, tendency to have frequent colds? For each diagnosis it was asked “At what age did the physician make this diagnosis for the first time?”
The infection status was defined by a positive H pylori–urea breath test result for gastrointestinal colonisation14 and a positive answer to the questions on physician‐diagnosed upper (common cold) and lower (bronchitis) respiratory infections (signifying an inhalative/respiratory pathway).
The estimated odds ratios (ORs; logistic regression analyses using STATISTICA V.6) were controlled for confounding factors: sex, parental atopy status (mother or father have at least one of a physician‐diagnosed eczema, asthma and/or hay fever), number of older/younger siblings, age of entry into day care, duration of breast feeding, cats in the household and smoking habits (smoking during pregnancy and passive smoking).
The socioeconomic status was also considered, characterised by parental educational level, employment/unemployment and single parenthood. Previous work has shown that socioeconomic status affects the prevalence of H pylori15 as well as atopic disease.1
The study was approved by the ethics committee of the University of Leipzig (Leipzig, Germany). Authorities of the City of Leipzig gave permission for the participation of preschool children in the study.
Results
The prevalences related to 2487 children in this age group (mean age 6.3 years) were for eczema 16.9%, for H pylori colonisation 6.1%, for bronchitis 30.2% and for (frequent) colds 23.4%. In all, 33.5% of the parents had allergic disorders, 16.4% were unemployed and 15.4% were single parents. Also, 11.3% of the mothers smoked during pregnancy, 40.3% in the presence of the child. In total, 6.3% of the children entered day care before age 1 year, and 38.6% had a cat currently and in the past.
The logistic regression shows significant associations between eczema and H pylori colonisation (adjusted OR (aOR) = 0.37; p = 0.002) and bronchitis (aOR = 1.99; p<0.001) but not for frequent colds (aOR = 1.09; p = 0.493). Significant effects on eczema were also found for parental disposition to atopy (aOR = 1.56; p<0.001) and the number of older siblings (aOR = 0.88; p = 0.049).
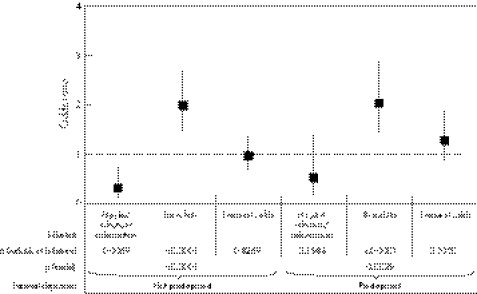
A comparison was made between children of parents with a reported allergy and the children of parents without an allergy (fig 1). This division was made to exclude a masking effect due to parental predisposition. The data indicate that the most significant H pylori‐mediated protection against eczema is observed in children not predisposed to atopy (aOR = 0.31; p = 0.006). Bronchitis, on the other hand, increased significantly the odds of eczema, independent of the children's predispositions (predisposed aOR = 2.02; p<0.001/not predisposed aOR = 1.98; p = 0.001).
Figure 1 aOR (95% CI) for eczema and infectious diseases/colonisation status, depending on parents' disposition to atopy (adjusted for sex, smoking during pregnancy, smoking in the presence of the child, having pets such as cats, number of older siblings, entry into day care before age 1 year, duration of breast feeding and socioeconomic status).
Discussion
Gastrointestinal colonisations showed a significant inverse association with eczema in children without a parental disposition to atopy (fig 1), indicating a protective effect against eczema in children not predisposed to atopy. The effect seems to be masked in children predisposed to atopy.
Other findings support these Hpylori‐associated results, suggesting that pathogens may stimulate the gut‐associated immune responses.2,3,4,5,6,7,8,9
The association between H pylori infections and eczema also seems to be mediated by the presence of older children.1,4,5 The protective sibling effect could possibly also be explained by the positive association between the number of siblings and H pylori infections. Depending on the number of older siblings (0, 1, 2 and >2), the frequency of H pylori infection increased (4.6%, 5.5%, 9.4% and 9.5%) in this population.
Both lower and upper respiratory infections increased the risk for eczema as well as for upper respiratory tract infections in childhood and for atopic diseases in later life.16
What this paper adds
The paper clearly shows an inverse association between bacterial colonisation and eczema (protective effect) in children without parental disposition to atopic diseases.
Furthermore, it could be shown that the ingestive pathway is of more importance compared with the respiratory ones.
Policy implications
Further research is required to clear up the role of bacterial colonisation of the gut compared with inhalative ones in protection against allergies. The aim should be a “vaccination” against allergies.
The results indicate that the gut plays a key role in such an active protective measure.
Under no circumstances should hygiene measures be diminished.
Summarising, this investigation showed in a preschool population that a bacterial infection/colonisation of the gastrointestinal tract may have a protective effect against eczema up to the age of school entry (6–7 years). Common respiratory infections (early in life), on the other hand, seem to enhance the risk of eczema later in life. A sibling effect does seem to exist, but may be better understood when both gastrointestinal infections/colonisations and respiratory infections are taken into account.
Methodological limitations might possibly have contributed to biases. The retrospective nature of the evaluation of this study and its reliance on parent‐administered, questionnaire‐based information may have weakened the reliability of the memory‐dependent information obtained. Another point of weakness is lack of knowledge of the time of the first H pylori colonisation. Usually H pylori colonisation is acquired in early childhood and persists throughout life.10 The question is, should the colonisation take place before an atopic disease breaks out (to avoid it via stamping of the immune system) or is it that colonisation can be used to restrain and/or suppress an allergic disorder? An answer to this question cannot be given at this time.
Footnotes
Funding: This study was supported by the BMBF Federal Ministry of Education and Research (Germany), the UFZ (Grant No. UFZ‐20/97), and State Ministry of Family and Health Saxony (Grant No. WVSMS/2001).
Competing interests: None declared.
References
- 1.Strachan D P. Hay fever, hygiene, and household size. BMJ 19992991259–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tantisira K, Weiss S T. Childhood infections and asthma: at the crossroads of the hygiene and Barker hypotheses. Respir Res 20012324–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ball T M, Castro‐Rodriguez J A, Griffith K A.et al Siblings, day‐care attendance, and the risk of asthma and wheezing during childhood. N Engl J Med 2000343538–543. [DOI] [PubMed] [Google Scholar]
- 4.Ponsonby A ‐ L, Couper D, Dwyer T.et al Cross sectional study of the relation between sibling number and asthma, hay fever, and eczema. Arch Dis Child 199879328–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. v. Mutius E, Martinez FD, Fritzsch C, et al. Skin test reactivity and number of siblings. BMJ 1994308692–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Infant‐Rivard C, Amre D, Gautrin D.et al Family size, day‐care attendance, and breastfeeding in relation to the incidence of childhood asthma. Am J Epidemiol 2001153653–658. [DOI] [PubMed] [Google Scholar]
- 7.Haby M M, Peat J K, Marks G B.et al Asthma in preschool children: prevalence and risk factors. Thorax 200156589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Illi S, v Mutius E, Lau S.et al Early childhood infectious diseases and the development of asthma up to school age: a birth cohort study. BMJ 2001322390–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matricardi P M, Rosmini F, Riondino S.et al Exposure to foodborne and orofecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ 2000320412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCune A, Lane A, Murray L.et al Reduced risk of atopic disorders in adults with Helicobacter pylori infection. Eur J Gastroenterol Hepatol 200315637–640. [DOI] [PubMed] [Google Scholar]
- 11.Cremonini F, Gasbarrini A. Atopy, Helicobacter pylori and the hygiene hypothesis. Eur J Gastroenterol Hepatol 200315635–636. [DOI] [PubMed] [Google Scholar]
- 12.Kosunen T U, Hook‐Nikanne J, Salomaa A.et al Increase of allergen‐specific immunoglobulin E antibodies from 1973 to 1994 in a Finnish population and a possible relationship to Helicobacter pylori infections. Clin Exp allergy 200232373–378. [DOI] [PubMed] [Google Scholar]
- 13.Pessi T, Virta M, Adjers K.et al Genetic and environmental factors in the immunopathogenesis of atopy: interaction of Helicobacter pylori infection and IL4 genetics. Int Arch Allergy Immunol 2005137282–288. [DOI] [PubMed] [Google Scholar]
- 14.Herbarth O, Krumbiegel P, Fritz G J.et al Helicobacter pylori prevalences and risk factors among school beginners in a German urban centre and its rural county. Environ Health Perspect 2001109573–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dominici P, Bellentani S, Di Biase A R.et al Familial clustering of Helicobacter pylori infection: population‐based study. BMJ 1999319537–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balemans W A, Rovers M M, Schilder A G.et al Recurrent childhood upper respiratory tract infections do not reduce the risk of adult atopic disease. Clin Exp Allergy 200636198–203. [DOI] [PubMed] [Google Scholar]