Abstract
Objectives
To assess the risk of mortality from suicide among male veteran participants in a large population‐based health survey.
Design and setting
A prospective follow‐up study in the US. Data were obtained from the US National Health Interview Surveys 1986–94 and linked to the Multiple Cause of Death file (1986–97) through the National Death Index.
Participants
The sample comprised 320 890 men, aged ≥18 years at baseline. The participants were followed up with respect to mortality for 12 years.
Results
Cox proportional hazards analysis showed that veterans who were white, those with ≥12 years of education and those with activity limitations (after adjusting for medical and psychiatric morbidity) were at a greater risk for completing suicide. Veterans were twice as likely (adjusted hazard ratio 2.04, 95% CI 1.10 to 3.80) to die of suicide compared with non‐veterans in the general population. The risk of death from “natural” causes (diseases) and the risk of death from “external” causes did not differ between the veterans and the non‐veterans. Interestingly, male veterans who were overweight had a significantly lower risk of completing suicide than those who were of normal weight.
Conclusions
Veterans in the general US population, whether or not they are affiliated with the Department of Veterans Affairs (VA), are at an increased risk of suicide. With a projected rise in the incidence of functional impairment and psychiatric morbidity among veterans of the conflicts in Afghanistan and Iraq, clinical and community interventions that are directed towards patients in both VA and non‐VA healthcare facilities are needed.
Suicide is a major cause of death in the US; approximately 30 000 people commit suicide every year, and nearly 650 000 people are seen in emergency departments after they have attempted suicide.1 The suicide rate for men (17.6/100 000 in 2003) is four times that for women (4.3/100 000 in 2003).2 Compared with the general adult population, US veterans may have an increased risk of suicide.3 Studies conducted among US veterans have focused on samples derived from patient populations in the Department of Veterans Affairs (VA) system.1,4,5,6,7 Risk factors for suicide common in patients of VA include the male sex, the elderly, those with diminished social support, medical and psychiatric conditions associated with suicide, and the availability and knowledge of firearms.4 Equally important is that much of the research on suicide has been based on Vietnam‐era veterans.3,7,8 Many studies have also focused on suicidal ideation and attempts (morbidity) of veterans, rather than on mortality from suicide.9,10,11
The reliance on VA clinical samples is particularly limiting from a population‐based perspective because three‐quarters of veterans do not receive healthcare through VA facilities.12 Consequently, little is known about the risk factors for suicide among veterans in the general US population. Estimates of the risk of suicide may be biased, to the extent that the characteristics of veterans who use the VA system differ from those of the larger population of veterans. In light of the high incidence of physical and mental disabilities among veterans of the conflicts in Iraq and Afghanistan,13,14,15 it is important to examine the risk of suicide among veterans in the general population.
The purpose of this paper was to examine risk factors for suicide among veterans in the general population. In pursuing this goal, we used a large, nationally representative, prospective dataset (with 653 deaths from suicide during the follow‐up period) to: (1) assess the relative risk of suicide for male veterans in the general population; (2) compare male veteran suicide decedents with those who died of natural and external causes; and (3) examine the effects of baseline sociodemographic circumstances and health status on the subsequent risk of suicide.
Methods
Data sources
This study used data from the 1986–94 National Health Interview Survey (NHIS).16 In the NHIS, which was conducted by the National Center for Health Statistics, people from the 50 states and the District of Columbia who were not institutionalized were sampled. NHIS uses a multistage probability sampling design. In the first stage, 198 primary sampling units were selected out of 1900 geographical areas (a county, a small group of contiguous counties, or a metropolitan statistical area). The second stage sampled households within each geographical area. Personal (face‐to‐face) household interviews were conducted, with response rates ranging from 94% to 98%.
The total sample of male veterans for the combined NHIS used in the analyses was 104 026. The demographic profile for the NHIS veteran sample closely matched that of other surveys, including the National Survey of Veterans12 and the Current Population Survey for September 1989.17
The NHIS 1986–94 data file was linked to the Multiple Cause of Death file (1986–97) through the National Death Index (NDI). NHIS participants aged ≥18 years were matched from the date of interview through December 1997 using 12 weighted criteria: social security number, first and last names, middle initial, race, sex, marital status, birth date (day, month and year), and state of birth and residence.18 We used the recommended National Center for Health Statistics scoring cut‐off, which corresponds to an estimate of 97% correctly classified deaths.19
Measures
The main outcome variable was death by suicide. Suicide cases were identified using the International classification of diseases, ninth revision, clinical modification (ICD‐9 E950–E959). Respondents were identified as veterans if they answered in the affirmative to “did you ever serve on active duty in the Armed Forces of the United States?” Covariates, from the baseline interview, included age (18–44, 45–64, or ≥65 years), marital status (married, widow/divorced/separated, or single), living arrangement (alone or with others), race (white or non‐white), education (<12 or ≥12 years), employment status (employed, unemployed, or not in the labour force—that is, retired, disabled or not looking for a job), region of residence (northeast, midwest, south, or west), place of residence (rural or urban), body mass index (BMI), number of chronic non‐psychiatric medical conditions (ICD‐9 001–289 and 320–779), number of psychiatric conditions (ICD‐9 290–316), self‐rated health, and activity limitations. In the analyses, a dichotomous variable was constructed from self‐rated health, with “good health” (excellent, very good, or good) opposed to “poor health” (fair or poor). Following Adams et al,20 activity limitations were ascertained with the question: “does any health problem now keep you from working at a job or business, keeping house, going to school, or something else?”, with the reply options (1) “unable to perform major activities”, (2) “limited in kind/amount of major activities”, (3) “limited in other activities” and (4) “not limited”. The first three categories were collapsed and henceforth are referred to as “limited”.
Statistical analyses
The Cox proportional hazards model was used to estimate the relative hazard of suicide adjusting for demographic characteristics, socioeconomic factors and health. Cox regression coefficients (b) measure the impact of predictors on time to death.21 All the variables were entered simultaneously into the Cox model. Time to death was measured from the month of the interview to the month of suicide completion. The reference group consisted of individuals who were censored at the time of their death due to other causes or, if they survived through the entire period, in December 1997.
In addition, competing risk analyses were performed to compare the relative risk of suicide to other causes of death among veterans versus non‐veterans. This procedure allowed us to compare coefficients from two Cox proportional hazards models (b1 and b2) using the Wald χ2 statistic with the following formula22:
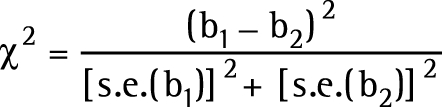 |
Analyses were weighted to adjust for differential response rates and variation in probabilities of selection into the sample. The Taylor series linearisation procedure using SUDAAN (Release 9.0.1; Research Triangle Institute, Research Triangle Park, North Carolina, USA.) was used to adjust significance tests for the complex sample design. Because there were too few female veterans in the sample who completed suicide (n = 6), we did not include women in the analyses. However, separate analyses with both men and women showed that the results were virtually identical to those in the model with men only (data not shown).
Results
Table 1 shows the baseline characteristics of the veterans and non‐veterans in the NHIS‐NDI. Veterans were proportionally more likely than were non‐veterans to be older, white, married and overweight.
Table 1 Characteristics of male veterans and non‐veterans in the NHIS‐NDI, National Health Interview Survey‐National Death Index.
| Veterans (n = 104 026) | Non‐veterans (n = 216 864) | |
|---|---|---|
| %* | %* | |
| Sex | ||
| Female | 4.77 | 62.48 |
| Male | 95.23 | 37.52 |
| Age (years) | ||
| 18–44 | 24.82 | 70.28 |
| 45–64 | 44.98 | 20.40 |
| ⩾65 | 30.20 | 9.32 |
| Race/ethnicity | ||
| White | 85.72 | 73.50 |
| Non‐white | 14.28 | 22.65 |
| Marital status | ||
| Married | 79.15 | 63.63 |
| Widowed/divorced/separated | 13.49 | 8.79 |
| Never married | 7.36 | 21.20 |
| Living arrangements | ||
| With others | 87.43 | 87.65 |
| Alone | 12.57 | 12.35 |
| Education | ||
| <12 years | 17.41 | 22.51 |
| ⩾12 years | 82.59 | 77.49 |
| Employment status | ||
| Employed | 62.13 | 77.34 |
| Unemployed | 2.47 | 3.74 |
| Not in labour force | 35.40 | 18.92 |
| Region of residence | ||
| Northeast | 19.72 | 20.51 |
| Midwest | 25.36 | 25.08 |
| South | 33.17 | 32.55 |
| West | 21.76 | 21.86 |
| Place of residence | ||
| Rural | 25.00 | 23.40 |
| Urban | 75.00 | 77.33 |
| Self‐rated health | ||
| Good | 93.70 | 96.14 |
| Poor | 6.30 | 3.86 |
| Body mass index | ||
| Underweight (0.0–19.9 kg/m2) | 2.50 | 4.46 |
| Normal weight (20.0–24.9 kg/m2) | 34.25 | 40.80 |
| Overweight (25.0–29.9 kg/m2) | 46.99 | 40.41 |
| Obese (⩾30.0 kg/m2) | 16.26 | 14.33 |
| Has at least one chronic non‐psychiatric condition | 51.75 | 38.02 |
| Has at least one psychiatric condition | 1.53 | 2.03 |
| Activity limitations | ||
| Not limited | 76.30 | 85.03 |
| Limited | 23.70 | 14.97 |
| Military service era | ||
| World War I | 0.32 | — |
| World War II | 28.01 | — |
| Korean conflict | 15.95 | — |
| Vietnam era | 29.02 | — |
| Post‐Vietnam | 9.91 | — |
| Other service | 16.79 | — |
—, not applicable.
*Weighted percentages.
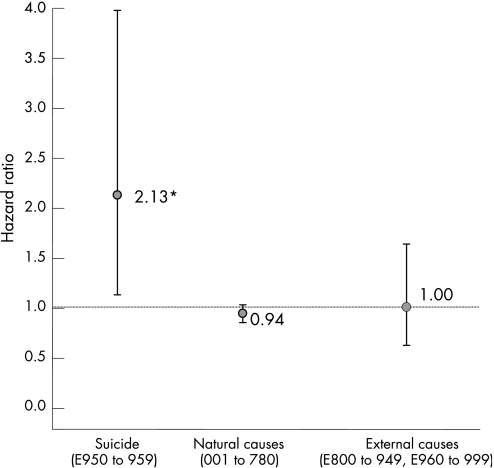
Veterans represented 15.7% of the NHIS sample but accounted for 31.1% of the suicide decedents. Figure 1 shows that over time veterans were twice as likely (adjusted HR 2.13, 95% CI 1.14 to 3.99) to die of suicide compared with male non‐veterans in the general population. Conversely, the risk of death from natural (diseases) and the risk of death from external (accidents and homicides) causes did not differ between the veterans and the non‐veterans after we adjusted for confounding factors.
Figure 1 Comparison of cause‐specific risk of mortality among veterans versus non‐veterans. Risk adjusted for age, marital status, living arrangement, race, education, family income, employment status, region, interval since last visit to doctor, self‐rated health, and body mass index. Reference group was non‐veterans. Error bars indicate 95% CI. For each model, survivors and decedents from other causes of death were considered censored. International classification of diseases, ninth revision codes appear in parentheses.*Significant difference (p<0.05) between suicide and other causes of death using competing risk comparisons.
Table 2 provides descriptive information on the predictor variables for those who committed suicide. At baseline, veteran suicide decedents were significantly (p<0.05) more likely than were non‐veteran decedents to be older, white, and high‐school graduates, and less likely to never be married. Veteran suicide decedents had more activity limitations at baseline than non‐veteran decedents. Furthermore, at the time of death, veterans were more likely to have committed suicide using a firearm than their non‐veteran counterparts.
Table 2 Characteristics of male veteran and non‐veteran suicide decedents in the National Health Interview Survey‐National Death Index.
| Veteran suicide (n = 197) | Non‐veteran suicide (n = 311) | p Value | ||||
|---|---|---|---|---|---|---|
| N (%)§ | n (%)§ | |||||
| Age (years) | ||||||
| 18–44 | 45 (22.38) | 230 (69.65) | ||||
| 45–64 | 76 (37.23) | 35 (11.72) | ‡ | |||
| ⩾65 | 76 (40.39) | 46 (18.63) | † | |||
| Race/ethnicity | ||||||
| White | 175 (95.53) | 248 (72.35) | ‡ | |||
| Non‐white | 21 (4.47) | 60 (27.65) | ||||
| Marital status | ||||||
| Married | 139 (72.09) | 155 (50.86) | ||||
| Widowed/divorced/separated | 45 (18.73) | 40 (8.40) | ||||
| Never married | 13 (9.19) | 116 (40.74) | * | |||
| Living arrangements | ||||||
| With others | 152 (75.71) | 258 (88.12) | ||||
| Alone | 45 (24.29) | 53 (11.88) | ||||
| Education (years) | ||||||
| <12 | 52 (12.30) | 91 (26.11) | ||||
| ⩾12 | 145 (87.70) | 217 (73.89) | * | |||
| Employment status | ||||||
| Employed | 96 (52.92) | 214 (68.41) | ||||
| Unemployed | 6 (1.88) | 17 (6.28) | ||||
| Not in labour force | 95 (45.19) | 80 (25.31) | ||||
| Region of residence | ||||||
| Northeast | 26 (12.14) | 52 (11.46) | ||||
| Midwest | 42 (17.92) | 81 (33.14) | ||||
| South | 86 (42.63) | 107 (29.89) | ||||
| West | 43 (27.31) | 71 (25.51) | ||||
| Place of residence | ||||||
| Rural | 62 (43.43) | 90 (76.96) | ||||
| Urban | 135 (56.57) | 221 (23.04) | ||||
| Self‐rated health | ||||||
| Good | 142 (90.92) | 269 (90.08) | ||||
| Poor | 24 (9.08) | 17 (9.92) | ||||
| Body mass index | ||||||
| Underweight (0.0–19.9 kg/m2) | 13 (8.70) | 27 (13.25) | ||||
| Normal weight (20.0–24.9 kg/m2) | 88 (51.77) | 135 (44.41) | ||||
| Overweight (25.0–29.9 kg/m2) | 71 (30.32) | 109 (31.33) | ||||
| Obese (⩾ 30.0 kg/m2) | 22 (9.21) | 27 (11.02) | ||||
| Has at least one chronic non‐psychiatric condition | 115 (68.53) | 137 (50.95) | ||||
| Has at least one psychiatric condition | 7 (3.03) | 16 (1.61) | ||||
| Activity limitations | ||||||
| Not limited | 134 (45.99) | 238 (76.88) | ||||
| Limited | 63 (50.98) | 73 (23.12) | * | |||
| Suicide method | ||||||
| Firearm (ICD‐9 E955.0–E955.4) | 152 (83.51) | 185 (55.11) | † | |||
| Non‐firearm (ICD‐9 E950.0–E953.0 and E955.5–E959.0) | 45 (16.49) | 126 (44.89) | ||||
| Military service era | ||||||
| World War I | 1 (0.23) | — | ||||
| World War II | 88 (47.06) | — | ||||
| Korean conflict | 21 (5.29) | — | ||||
| Vietnam era | 43 (25.77) | — | ||||
| Post‐Vietnam | 14 (7.53) | — | ||||
| Other service | 25 (14.12) | — | ||||
—, not applicable.
ICD‐9, International classification of diseases, ninth revision, clinical modification.
*p<.05; †p<0.01; ‡p<0.001.
§Unweighted N and weighted percentage with bivariate logistic tests.
Table 3 shows the predictors of suicide risk among veterans. The results indicate that whites, those with >12 years of education and those with activity limitations (after adjusting for medical and psychiatric morbidity) were at a greater risk for suicide completion. An interesting result was that relative to those with normal weight (BMI 20.0–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2) male veterans were at lower risk of completing suicide.
Table 3 Risk factors for suicide among male veterans in the National Health Interview Survey‐National Death Index 1986–97.
| Adjusted HR (95% CI)§ | |
|---|---|
| Age (years) | |
| 18–44 | 1.00 |
| 45–64 | 0.90 (0.31 to 2.65) |
| ⩾65 | 1.46 (0.51 to 4.15) |
| Race/ethnicity | |
| White | 3.23 (1.75 to 5.88)‡ |
| Non‐white | 1.00 |
| Marital status | |
| Married | 1.00 |
| Widowed/divorced/separated | 0.58 (0.03 to 10.77) |
| Never married | 0.72 (0.02 to 26.41) |
| Living arrangements | |
| With others | 1.00 |
| Alone | 3.48 (0.14 to 87.97) |
| Education (years) | |
| <12 | 1.00 |
| ⩾12 | 2.67 (1.38 to 5.17)† |
| Employment status | |
| Employed | 1.00 |
| Unemployed | 0.56 (0.10 to 3.10) |
| Not in labour force | 1.03 (0.44 to 2.41) |
| Region of residence | |
| Northeast | 1.00 |
| Midwest | 1.02 (0.24 to 4.43) |
| South | 2.02 (0.46 to 8.78) |
| West | 1.87 (0.40 to 8.63) |
| Place of residence | |
| Rural | 1.00 |
| Urban | 0.44 (0.17 to 1.18) |
| Self‐rated health | |
| Good | 1.00 |
| Poor | 0.54 (0.15 to 1.98) |
| Body mass index | |
| Underweight (0.0–19.9 kg/m2) | 2.44 (0.46 to 12.84) |
| Normal weight (20.0–24.9 kg/m2) | 1.00 |
| Overweight (25.0–29.9 kg/m2) | 0.45 (0.22 to 0.92)* |
| Obese (⩾30.0 kg/m2) | 0.41 (0.14 to 1.17) |
| Number of chronic non‐psychiatric conditions | 1.08 (0.68 to 1.72) |
| Number of psychiatric conditions | 0.41 (0.14 to 1.26) |
| Activity limitations | |
| Not limited | 1.00 |
| Limited | 4.44 (1.33 to 14.80)* |
*p<0.05. †p<0.01. ‡p<0.001.
§Model comparing suicide death to alive or other cause of death.
Discussion
Using prospective (NHIS‐NDI) population‐based health and mortality data, we examined risk of suicide among male veterans of military service. The results revealed that male veterans are at increased risk of suicide relative to non‐veterans. Contrary to studies conducted in the UK,23,24 the findings showed that veterans were at greater risk of dying from suicide compared with a non‐veteran cohort. The results of this study are particularly noteworthy because they were derived from a sample representative of all veterans in the US general population, whether or not they sought care in the VA system. Conversely, nearly all previous studies have examined suicide in VA‐based samples and such studies may over‐ or underestimate risk of suicide because the VA serves only a fraction of veterans.12
A surprising finding was that veterans who were overweight had a lower risk for suicide. This finding is consistent with a recent longitudinal study. In a 31‐year analysis of more than one million Swedish male military conscripts, Magnusson et al25 concluded that the risk of suicide decreased with increasing BMI. Other studies that examined the association between overweight and obesity and depression—a critical psychiatric condition preceding suicide—yielded conflicting results.26,27,28,29 According to Magnusson and colleagues, rather than directly reducing the risk of suicidal behaviour, a growing body of research suggests that raised BMI may be negatively associated with depression and suicidal behaviour through biological pathways. Two recent studies suggest that insulin resistance influences free fatty acids in the blood, tryptophan metabolism and serotonin levels in the brain.30,31 Serotonin deficiency in turn is implicated in suicidal behaviour.32
Our results also show that activity limitation is an important risk factor for suicide among veterans. Healthcare providers are well positioned to intervene with at‐risk veterans who have physical and/or mental disabilities. Primary care physicians, as gatekeepers of the healthcare system, along with other specialists, have important roles in the assessment and management of depression and suicidality among veterans in clinical settings.33
Another important finding was the higher probability that US veterans used firearms as a mode of suicide compared with non‐veterans. Supplementary analyses with data from the National Mortality Followback Survey (NMFS)34 showed that veteran suicide decedents were 58% (OR 1.58, 95% CI 1.08 to 2.33) more likely than non‐veterans to use firearms than other suicide methods, after adjusting for sex, age, marital status, race, education, region, metropolitan status, psychiatric visit in the last year of life, number of half‐days in bed for illness or injury in the last year of life, and alcohol use (data not shown). Furthermore, an analysis of veteran suicide decedents in the NMFS revealed that those who owned guns were 21.1 times more likely to use firearms than were those who did not own guns (OR 21.10, 95% CI 9.12 to 48.83), after adjusting for sex, age, marital status, race, education, region, and metropolitan status. Other data show that military personnel on active duty are more likely to own and use firearms to commit suicide than the non‐military population.35 According to recent data from the Behavioral Risk Factor Surveillance System,36 veterans are substantially more likely to own guns than are individuals in the general population (45.7% vs 32.3%, p<0.001).
Although there is a debate among suicidologists and policy makers about the association between the availability of firearms and risk of suicide, the preponderance of evidence suggests that a gun in the house, even if unloaded, increases the risk for suicide in adults.37 Case–control studies on the prevalence of guns and risk of suicide have shown significant increases in suicides in homes with guns, even when adjustments were made for other factors, such as education, arrests, and drug misuse.38 Because veterans are familiar with and have greater access to firearms, healthcare providers need to be more attentive to the critical role that firearms play in suicidal behaviour among veterans. Unfortunately, some doctors find it difficult to ask patients directly about suicide.39 Kaplan et al40 also found that only half of the primary care physicians who identified patients as suicidal would inquire about their access to firearms.
This study has several potential limitations. The first limitation concerns the reliability of suicide data derived from death certificates. In this regard, Fuse41 reported that “there is general agreement that suicides are likely under‐reported for such reasons as the beyond‐a‐reasonable‐doubt criterion used and for some socio‐cultural reasons that may bias the reporting. There is not, however, much agreement as to the degree to which true suicides are undercounted.” Fuse concluded that errors in collective suicide statistics are usually random and should not bias the present findings. Second, a further constraint of the NHIS‐NDI design was the absence of time‐varying covariates. However, most suicides occurred shortly after the interview (ie, 75% died within 3 years) so there was a limited opportunity for baseline measures to change (eg, marital status). Third, data were unavailable on important measures such as suicide attempts, source of healthcare coverage, or combat experience—all of which are associated with suicide risk. Fourth, psychiatric conditions are critical risk factors in suicide. One would expect over 90% of suicide decedents to have psychiatric illness.1,42 However, little information about baseline psychiatric morbidity was available in the NHIS. Therefore, we were unable to examine the role of well‐established risk factors such as major depressive disorders or post‐traumatic stress disorder because of the small number of suicide decedents and because major depressive disorders and post‐traumatic stress disorder were not available as separate psychiatric conditions in the NHIS‐NDI dataset. Finally, we could not address cohort and period effects associated with suicide rates. For example, there have been major developments in suicide prevention since the NHIS was conducted, particularly the enormous changes in rates of antidepressant prescriptions and reduced suicide rates in the last 10 years.
Despite these limitations, the results have substantial clinical and public health implications. Clinicians outside the VA system need to be alert for signs of suicidal intent among veterans, as well as their access to firearms. Similarly, healthcare facilities that serve veterans outside the VA system should also recognise the increased risk of suicide in this population. With the projected rise in functional impairments13 and psychiatric morbidity14,15 among veterans of the conflicts in Afghanistan and Iraq, clinical and community interventions directed towards patients in both VA and non‐VA healthcare facilities are needed.
Policy implications
With the projected rise in functional impairments and psychiatric morbidity among veterans of the conflicts in Afghanistan and Iraq, clinical and community interventions directed towards patients in both Veterans Affairs and non‐Veterans Affairs healthcare facilities are needed.
What is already known
Veteran suicide decedents are more likely to be men, older, to have diminished social support, medical and psychiatric conditions, and the availability and knowledge of firearms.
Most, if not all, previous studies on veteran suicide focused on patients of the US Department of Veterans Affairs and/or on those who served during the Vietnam War era.
Little is known about the risk of suicide among veterans in the general population.
What this paper adds
Compared with non‐veterans in the general population, male veterans are more likely to die of suicide but are not more likely to die of external causes or diseases.
Impaired functional status increased the risk for mortality from suicide among male veterans.
Acknowledgements
Data for this study were made available through the Inter‐University Consortium for Political and Social Research and the National Center for Health Statistics.
Abbreviations
BMI - body mass index
HR - hazard ratio
ICD‐9 - International Classification of Diseases, ninth revision
NHIS - National Health Interview Survey
NHIS‐NDI - National Health Interview Survey‐National Death Index
VA - Veterans Affairs
Footnotes
Funding: This research was undertaken with a grant from the National Institute of Mental Health (MH070520).
Competing interests: None.
References
- 1.Goldsmith S K, Pellmar T C, Kleinman A M.et alReducing suicide: a national imperative. Washington, DC: National Academy Press, 2002, http://www.nap.edu/catalog/10398.html (accessed 26 Mar 2006) [PubMed]
- 2.Centers for Disease Control and Prevention, National Centers for Injury Prevention and Control Web‐based Injury Statistics Query and Reporting System (WISQARS) 2005. www.cdc.gov/ncipc/wisqars (accessed 26 Jan 2006)
- 3.Desai R, Dausey D, Rosenheck R A. Mental health service delivery and suicide risk: the role of individual patient and facility factors. Am J Psychiatry 2005162311–318. [DOI] [PubMed] [Google Scholar]
- 4.Lambert M T, Fowler D R. Suicide risk factors among veterans: risk management in the changing culture of the Department of Veterans Affairs. J Ment Health Adm 199724350–358. [DOI] [PubMed] [Google Scholar]
- 5.Rosenheck R. Mental and substance use health services for veterans: experience with performance evaluation in the Department of Veterans Affairs. In: Institute of Medicine, ed. Improving the quality of health care for mental and substance‐use conditions: Quality Chasm Series. Washington, DC: National Academy Press, 2006;382–448, http://darwin.nap.edu/books/0309100445/html (accessed 26 Mar 2006)
- 6.Thompson R, Kane V R, Sayers S L.et al An assessment of suicide in an urban VA medical center. Psychiatry 200265327–337. [DOI] [PubMed] [Google Scholar]
- 7.Bullman T A, Kang H K. The risk of suicide among wounded Vietnam veterans. Am J Public Health 199686662–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boehmer T K, Flanders W D, McGeehin M A.et al Postservice mortality in Vietnam veterans: 30‐year follow‐up. Arch Intern Med 20041641908–1916. [DOI] [PubMed] [Google Scholar]
- 9.Brenda B B. Gender differences in predictors of suicidal thoughts and attempts among homeless veterans that abuse substance. Suicide Life Threat Behav 200535106–116. [DOI] [PubMed] [Google Scholar]
- 10.Reich J. The relationship of suicide attempts, borderline personality traits, and major depressive disorder in a veteran outpatient population. J Affect Disord 199849151–156. [DOI] [PubMed] [Google Scholar]
- 11.Fonatana A, Rosenheck R. Attempted suicide among Vietnam veterans: a model of etiology in a community sample. Am J Psychiatry 1995152102–109. [DOI] [PubMed] [Google Scholar]
- 12.Department of Veterans Affairs 2001 National Survey of Veterans final report. http://www.va.gov/vetdata/SurveyResults/index.htm (accessed 26 Jan 2006)
- 13.Gawande, A Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med 20043512471–2475. [DOI] [PubMed] [Google Scholar]
- 14.Kang H K, Hyams K C. Mental health care needs among recent war veterans. N Engl J Med 20043521289. [DOI] [PubMed] [Google Scholar]
- 15.Hoge C W, Auchterlonie J L, Milliken C S. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 20062951023–1032. [DOI] [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services, National Center for Health Statistics. National Health Interview Survey, 1986–1994 (computer file). 2nd ICPSR release. Washington, DC: US Department, of Health and Human Services, National Center for Health Statistics (producer), 1986–1995. Ann Arbor, MI: Inter‐university Consortium for Political and Social Research (distributor), 1989– 1996
- 17.US Department of Commerce, Bureau of the Census. Current population survey, September 1989: Veterans and cardiovascular disease risk factor supplements (Computer file), Washington, DC: US Department. of Commerce, Bureau of the Census (producer), 1989. Ann Arbor, MI: Inter‐university Consortium for Political and Social Research (distributor) 1992
- 18.Rogot E, Sorlie P, Johnson N J. Probabilistic methods in matching census samples to the National Death Index. J Chronic Dis 198639719–734. [DOI] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics National Health Interview Survey. Data and documentation. Hyattsville, MD: Public Health Service, 2000
- 20.Adams P F, Hendershot G E, Marano M A. Current estimates from the National Health Interview Survey, 1996. National Center for Health Statistics. Vital Health Stat 199910, 2001–203. [PubMed] [Google Scholar]
- 21.Lee E T, Go O T. Survival analysis in public health research. Annu Rev Health 199718105–134. [DOI] [PubMed] [Google Scholar]
- 22.Lagakos S W. A covariate model for partially censored data subject to competing causes of failure. Appl Stat 197827235–241. [Google Scholar]
- 23.Macfarlane G J, Thomas E, Cherry N. Mortality among UK Gulf War veterans. Lancet 200035617–21. [DOI] [PubMed] [Google Scholar]
- 24.Macfarlane G J, Hotop M, Maconochi N.et al Long‐term mortality amongst Gulf War veterans: is there a relationship with experiences during deployment and subsequent morbidity? Int J Epidemiol 2005341403–1408. [DOI] [PubMed] [Google Scholar]
- 25.Magnusson P K, Rasmussen F, Lawlor D A.et al Association of body mass index with suicide mortality: a prospective cohort study of more than one million men. Am J Epidemiol 20061631–8. [DOI] [PubMed] [Google Scholar]
- 26.Simon G E, Von Korff M, Saunders K.et al Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry 200663824–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onyike C U, Crum R M, Lee H B.et al Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 20031581139–1147. [DOI] [PubMed] [Google Scholar]
- 28.Roberts R E, Deleger S, Strawbridge W J.et al Prospective association between obesity and depression: evidence from the Alameda County study. Int J Obes Relat Metab Disord 200327514–521. [DOI] [PubMed] [Google Scholar]
- 29.Stunkard A J, Faith M S, Allison K C. Depression and obesity. Biol Psychiatry 200354330–337. [DOI] [PubMed] [Google Scholar]
- 30.Golomb B A, Tenkanen L, Alikoski T.et al Insulin sensitivity markers: predictors of accidents and suicides in Helsinki Heart Study screenees. J Clin Epidemiol 200255767–773. [DOI] [PubMed] [Google Scholar]
- 31.Lawlor D A, Smith G D, Ebrahim S. British Women's Heart and Health Study. Association of insulin resistance with depression: cross sectional findings from the British Women's Heart and Health Study, BMJ 20033271383–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lester D. The concentration of neurotransmitter metabolites in the cerebrospinal fluid of suicidal individuals: a meta‐analysis. Pharmacopsychiatry 19952845–50. [DOI] [PubMed] [Google Scholar]
- 33.Goldman L S, Nielsen N H, Champion H C. Awareness, diagnosis, and treatment of depression. J Gen Intern Med 199914569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Health and Human Services, National Center for Health Statistics. National mortality followback survey, 1993 computer file). ICPSR version. Hyattsville, MD: U, S. Dept. of Health and Human Services, National Center for Health Statistics (producer), 1999. Ann Arbor, MI: Inter‐university Consortium for Political and Social Research (distributor) 2000
- 35.Mahon M J, Tobin J P, Cusack D A.et al Suicide among regular‐duty military personnel: a retrospective case‐control study of occupation‐specific risk factors for workplace suicide. Am J Psychiatry 20051621688–1696. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control, Prevention (CDC) Behavioral risk factor surveillance system survey data. Atlanta, GA: US Department of Health and Human Services, CDC, 2003
- 37.Mann J J. A current perspective of suicide and attempted suicide. Ann Intern Med 2002136302–311. [DOI] [PubMed] [Google Scholar]
- 38.Wellford C F, Pepper J V, Petrie C V.Firearms and violence: a critical review. Washington, DC: National Academy Press, 2004, http://darwin.nap.edu/books/0309091241/html (accessed 26 Mar 2006)
- 39.Schulberg H C. Treating depression in primary care practice: applications of research findings. J Fam Pract 200150535–537. [PubMed] [Google Scholar]
- 40.Kaplan M S, Adamek M E, Calderon A. Managing depressed and suicidal geriatric patients: differences among primary care physicians. Gerontologist 199939417–425. [DOI] [PubMed] [Google Scholar]
- 41.Fuse T.Suicide, individual and society. Toronto: Canadian Scholars' Press, 1997
- 42.Gibbons R D, Hur K, Bhaumik D K.et al The relationship between antidepressant medication use and rate of suicide. Arch Gen Psychiatry 200562165–172. [DOI] [PubMed] [Google Scholar]