Abstract
Objectives
To examine the effects of ill health on selection into paid employment in European countries.
Methods
Five annual waves (1994–8) of the European Community Household Panel were used to select two populations: (1) 4446 subjects unemployed for at least 2 years, of which 1590 (36%) subjects found employment in the next year, and (2) 57 436 subjects employed for at least 2 years, of which 6191 (11%) subjects left the workforce in the next year because of unemployment, (early) retirement or having to take care of household. The influence of a perceived poor health and a chronic health problem on employment transitions was studied using logistic regression analysis.
Results
An interaction between health and sex was observed, with women in poor health (odds ratio (OR) 0.4), men in poor health (OR 0.6) and women (OR 0.6) having less chance to enter paid employment than men in good health. Subjects with a poor health and low/intermediate education had the highest risks of unemployment or (early) retirement. Taking care of the household was only influenced by health among unmarried women. In most European countries, a poor health or a chronic health problem predicted staying or becoming unemployed and the effects of health were stronger with a lower national unemployment level.
Conclusion
In most European countries, socioeconomic inequalities in ill health were an important determinant for entering and maintaining paid employment. In public health measures for health equity, it is of paramount importance to include people with poor health in the labour market.
The presence of socioeconomic inequalities in health has been widely acknowledged.1 Lower education, unskilled labour and low income are associated with higher mortality and morbidity.2 Labour force participation is an important determinant of health inequalities, as demonstrated by a higher prevalence of illness and disability3,4 and a higher mortality among unemployed people.5 The association between health and employment is bidirectional: unemployment may cause poor health (causation hypothesis) and poor health may increase the probability of becoming unemployed (selection hypothesis).6,7
The causation mechanism is illustrated among British households, where unemployment had a strong effect on the incidence of any limiting illness and employment was related to recovery from these illnesses.6 A review of longitudinal studies concluded that loss of employment affected mental health, but also that gaining employment improved mental health.8
There is also evidence for the selection hypothesis. Among long‐term unemployed Norwegians, mental morbidity was strongly associated with a reduction in obtaining a paid job.9 In a British study, healthier people were found more likely to gain employment than people with minor psychiatric morbidity.7 Ill health may also increase other forms of non‐employment, such as early retirement and having to stay home to take care of the family.7,10 In a Finnish cohort of men, self‐assessed poor health was a strong predictor of both disability as well as non‐illness‐based early retirement.11
The associations between health and employment will not be similar across all sociodemographic groups, as age, education, sex, marital status or household income may influence the social context of health and employment status.12,13 The consequences of ill health for the likelihood of becoming or staying unemployed also depend on social and labour market policies, which vary across European countries. For example, striking differences in access to benefits, such as early retirement or disability pension, for disabled people have been described in the European Union. In The Netherlands, <10% of disabled people have labour as their main source of income whereas in Sweden this proportion amounts to over 50%.14
Against this background, the aim of this study was to investigate the effects of ill health on the selection process into paid employment and whether these effects interacted with socioeconomic groups. The secondary aim of the study was to investigate whether observed associations between ill health and employment transitions differed among European countries.
Methods
Study population
The data were derived from the first five waves (1994–8) of the European Community Household Panel (ECHP).15 The ECHP is a social survey among member states of the European Union with a longitudinal design to describe the social dynamics in Europe. Data were collected by the National Institutes for Statistics or research centres, while data checks, weighings and imputations were done centrally by the Statistical Office of the European Communities (Eurostat). All surveys were based on a non‐stratified random sampling design among all national private households. All members of the household were individually interviewed. The data collection was carried out in most countries by paper‐and‐pencil interviewing, but in four countries (UK, The Netherlands, Portugal and Greece) by computer‐assisted personal interviewing. The overall household response rate in the first wave was 72%, but varied considerably among countries. The response rates in later waves of the ECHP study were higher. A detailed description of sampling procedures and response rates has been published elsewhere.16,17
For the purpose of this study, subjects aged between 16–65 years were selected, with available information on employment status and health status during at least three consecutive annual measurements, whereby the employment status remained unchanged in the first and second measurement and a possible employment transition had occurred in the third measurement. Although employment status was ascertained annually, we considered this status as representative for the whole year preceding the administration of the questionnaire. This procedure resulted in a cohort with 3 years of follow‐up, with two consecutive years before a possible employment transition. For a small part of the cohort, information was also available in the third and fourth annual measurements before the year of employment transition. Thus, for every subject, an employment transition was possible in a given year and labour status was regarded as constant in the 2–4 years before the possible employment transition.
Self‐defined employment status was classified into four mutually exclusive categories: employed (paid employment, paid apprenticeship or self‐employment), unemployed, retired or taking care of household.15 Employment was defined as working in a job for at least 15 h/week. Subjects working <15 h/week were automatically classified into the categories unemployed, retired, taking care of household, in military service, following education or economically inactive. Unemployed subjects were defined as those people who worked <15 h/week and who considered themselves as being unemployed. Subjects who classified themselves into the last three categories were not selected for analysis in this study, hence excluding economically inactive people who are without work and who do not wish to consider themselves as unemployed. Subjects with a disability pension as another form of non‐employment were also excluded from the analysis, as poor health is an essential requirement to qualify for a disability pension. However, disabled people with a paid job for >15 h/week were included in the category “employed”.
Two different populations were defined to study employment transitions. The first study population included 4446 people who were unemployed for at least two consecutive years, of which 1590 (36%) people entered the workforce during the last year of follow‐up. The second study population consisted of 57 436 workers who were employed for at least two consecutive years, of which 6191 (11%) people left the workforce in the last year of follow‐up due to unemployment (n = 3000), retirement (n = 2017) or having to take care of the household (n = 1174).
Questionnaire
The questionnaire comprised questions on individual and household characteristics, perceived general health, chronic health problems and employment status. Individual characteristics included age, sex, education and personal income. Household characteristics included marital status, the presence of children aged ⩽12 years and household income. Subjects were divided into three groups according to their level of educational attainment on the basis of the International Standard Classification of Education.18 Information on marital status was used to compare subjects married or living with others. Household and personal income were categorised into three centile groups (<25th centile, 25–75th centile and >75th centile), relative to the income distribution of the study sample in each country. If the personal income of a subject was ⩾75% of the household income, the subject was defined as breadwinner within the household.
Two measures of self‐reported health were used. First, subjects were asked to rate their own general health on a 5‐point scale, ranging from “very good”, “good”, “fair” and “bad” to “very bad”. Those reporting less than “good health” were defined as having a poor health.19 Second, subjects were asked whether they had any chronic physical or mental health problem, illness or disability (yes/no). An affirmative answer was classified as chronic health problem.15
Statistical methods
Logistic regression analysis was performed to study the impact of poor health and a chronic health problem on employment status, adjusted for country and personal and household characteristics. The first step in the analysis was to establish the associations between poor health and employment status, including country as a categorical variable (fixed factor) to adjust for the effect of country on the association between poor health and employment status. In the second step, other independent sociodemographic variables were included in the model by a step‐forward procedure. The variable with the strongest association with employment status was put in the model first, followed by the next strongest and so on. Variables with a significant reduction in the overall scaled deviance of the model were retained in the multivariate model. In the third step, interactions between poor health and significant sociodemographic variables were investigated for their influence on the overall fit of the model. The interaction with the strongest effect on the scaled deviance of the model was included in the final multivariate model. Thus, interaction terms without health were not considered, thereby excluding possible interactions among sociodemographic variables. For all analyses, four different time windows were applied, investigating the effects of the independent variables measured at 1, 2, 3 and 4 years before the employment transition. All statistical models were based on the (varying) number of people available for the three different measures of employment status, without weighing the regression coefficients according to attrition rate in the country sample or population size in each country.
For the analysis on transition from employment to (early) retirement, only subjects in the age group 55–65 years were used, as occurrence of retirement among those aged ⩽54 years was very low. Owing to this selection, age was not included in this analysis. Likewise, the analysis on transition from employment to household was restricted to women, as only very few men classified themselves as taking care of the household without having any paid job.
The variation among countries in the association between poor health and employment status was investigated by introduction of the interaction term of poor health and country in each multivariate model. This interaction term was used to estimate the country‐specific associations for poor health and employment status (expressed by odds ratios (ORs)), adjusted for relevant sociodemographic covariates. All analyses were repeated with the presence of a chronic health problem as outcome measure. The analyses were carried out with the statistical package SAS V.8.2.
Results
The background characteristics of both populations are presented in table 1. Both health measures were strongly associated with almost 50% of all people reporting a perceived poor health, also indicating the presence of a chronic physical or mental health problem, illness or disability. Ill health, sex, education, having young children in household and being a breadwinner were associated with employment transition.
Table 1 Background characteristics of subjects from the European Household Panel Survey in the year of an employment transition after at least two consecutive years of unemployment or employment.
| Characteristic | Subjects with at least 2 years of unemployment who remained unemployed (n = 2856) or entered employment (n = 1590) in the third year | Subjects with at least 2 years of employment who remained employed (n = 51 245) or left the workforce (n = 6191) in the third year | ||
|---|---|---|---|---|
| Unemployed | Became employed | Employed | Left workforce | |
| n (%) | n (%) | n (%) | n (%) | |
| Age (years) | ||||
| 16–24 | 758 (27) | 586 (38*) | 5610 (11) | 736 (13) |
| 25–44 | 1241 (45) | 785 (49) | 29 344 (60) | 2200 (38*) |
| 45–54 | 463 (17) | 170 (11) | 10 764 (22) | 1102 (19) |
| 55–65 | 291 (11) | 38 (2*) | 3240 (7) | 1805 (31*) |
| Sex (men) | 1315 (46) | 886 (56*) | 31 642 (62) | 3216 (52*) |
| Married (yes) | 1333 (47) | 700 (44) | 36 347 (71) | 4399 (71) |
| Educational level | ||||
| High | 263 (10) | 192 (13) | 13 297 (27) | 896 (15*) |
| Intermediate | 956 (35) | 595 (39) | 18 838 (38) | 2029 (34) |
| Low | 1507 (55) | 732 (48*) | 17 594 (35) | 2982 (51*) |
| Children <12 years | 800 (28) | 498 (31*) | 17 797 (35) | 1674 (27*) |
| Breadwinner | 481 (17) | 251 (16) | 16 341 (32) | 1585 (26*) |
| Perceived poor health | 968 (34) | 327 (21*) | 12 437 (24) | 2311 (37*) |
| Chronic health problem | 662 (23) | 200 (13*) | 8100 (16) | 1544 (25*) |
*χ2 test, p<0.05.
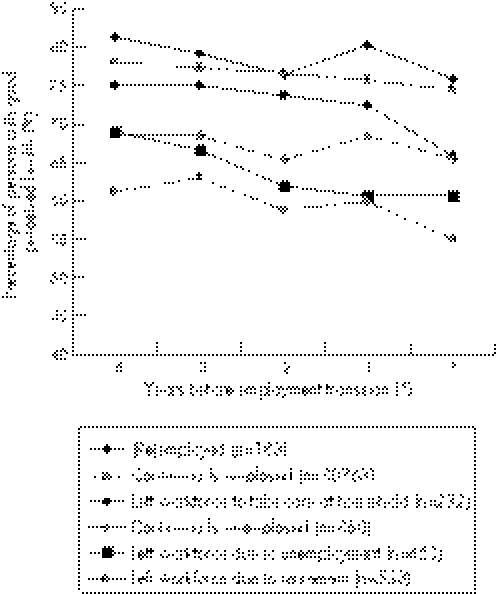
Figure 1 shows that in all groups the proportion of people in good health decreased in the period 1994–8. The proportion of people in good health was consistently higher among those who were employed or became employed than among people who were not employed or left the workforce.
Figure 1 Proportion of subjects with a perceived good health among respondents who completed all five waves of the European Household Panel Survey and an employment transition in the last year of the survey.
Table 2 shows that an interaction was observed between health status and sex. Women with poor health, men with poor health and women with good health were significantly more likely to remain unemployed in the next year than men with good health. This interaction was present up to 4 years before entering paid employment. A positive impact on (re)employment was observed for people being married, being of younger age, having higher education and having higher personal income. Being a breadwinner (OR 0.9, 95% CI 0.8 to 1.2) and having children <12 years in the household (OR 1.0, 95% CI 0.8 to 1.2) were not associated with entering employment. Chronic health problems showed very similar results for all time windows (results not shown).
Table 2 Multivariate models with different time windows of significant determinants of (re)employment among subjects from the European Household Panel Survey with at least two consecutive previous years of unemployment before entering paid employment.
| Determinant | Years before entering paid employment | |||
|---|---|---|---|---|
| 1 year | 2 years | 3 years | 4 years | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| n (stayed unemployed) | 2634 | 2646 | 1444 | 792 |
| n (entered employment) | 1481 | 1483 | 609 | 174 |
| Poor health–women† | 0.4 (0.3 to 0.5)* | 0.4 (0.3 to 0.5)* | 0.6 (0.4 to 0.8)* | 0.5 (0.3 to 0.9)* |
| Good health–women | 0.6 (0.5 to 0.7)* | 0.6 (0.5 to 0.7)* | 0.5 (0.4 to 0.7)* | 0.7 (0.5 to 1.0)* |
| Poor health–men | 0.6 (0.4 to 0.7)* | 0.6 (0.5 to 0.7)* | 0.6 (0.4 to 0.8)* | 0.6 (0.4 to 1.1) |
| Good health–men | 1 | 1 | 1 | 1 |
| Age (years) | ||||
| 16–24 | 8.1 (5.4 to 12.2)* | 9.0 (6.0 to 13.5)* | 11.0 (5.2 to 23.4)* | 4.7 (1.4 to 14.9)* |
| 25–44 | 5.7 (3.9 to 8.3)* | 6.0 (4.2 to 8.8)* | 8.3 (4.1 to 17.0)* | 3.6 (1.2 to 10.8)* |
| 45–54 | 3.3 (2.2 to 5.0)* | 3.4 (2.3 to 5.0)* | 4.7 (2.2 to 9.9)* | 1.7 (0.5 to 5.7) |
| 55–64 | 1 | 1 | 1 | 1 |
| Married | 1.4 (1.2 to 1.7)* | 1.4 (1.2 to 1.6)* | 1.4 (1.1 to 1.8)* | 1.6 (1.0 to 2.6)* |
| Educational level | ||||
| High | 1.7 (1.3 to 2.1)* | 1.6 (1.3 to 2.0)* | 2.1 (1.5 to 2.9)* | 2.6 (1.5 to 4.7)* |
| Intermediate | 1.6 (1.3 to 1.8)* | 1.5 (1.3 to 1.8)* | 1.6 (1.3 to 2.0)* | 1.9 (1.2 to 2.8)* |
| Low | 1 | 1 | 1 | 1 |
| Personal income | ||||
| >75th centile | 1.6 (1.3 to 1.9)* | 1.9 (1.6 to 2.3)* | 1.8 (1.4 to 2.5)* | 1.4 (0.9 to 2.3) |
| 25–75th centile | 1.5 (1.2 to 1.7)* | 1.4 (1.2 to 1.6)* | 1.4 (1.1 to 1.8)* | 1.0 (0.6 to 1.6) |
| <25th centile | 1 | 1 | 1 | 1 |
*Wald's χ2 test, p<0.05.
†Significant interaction.
Table 3 shows that poor health was more important among those with higher education than among those with lower education becoming unemployed. The effect of poor health within the strata of intermediate and higher education became less strong in more distant years. Job loss was also influenced by older age, not being married, having children <12 years (as per the previous year) and having lower personal income. Being a breadwinner (OR 1.0, 95% CI 0.9 to 1.1) or being male (OR 1.1, 95% CI 1.0 to 1.2) did not influence unemployment. The impact of chronic health problems was remarkably similar to a perceived poor health (results not shown).
Table 3 Multivariate models with different time windows of significant determinants of becoming unemployed among subjects from the European Household Panel Survey with at least two consecutive previous years of employment before becoming unemployed.
| Determinant | Years before becoming unemployed | |||
|---|---|---|---|---|
| 1 year | 2 years | 3 years | 4 years | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| n (stayed employed) | 47 378 | 36 610 | 30 706 | 28 780 |
| n (became unemployed) | 2700 | 1629 | 515 | 427 |
| Poor health–low education† | 2.2 (1.8 to 2.6)* | 2.5 (2.0 to 3.1)* | 2.3 (1.6 to 3.4)* | 2.5 (1.6 to 3.9)* |
| Good health–low education | 1.9 (1.7 to 2.2)* | 1.9 (1.6 to 2.3)* | 2.2 (1.6 to 3.1)* | 2.2 (1.5 to 3.1)* |
| Poor health–intermediate education | 2.4 (2.0 to 2.9)* | 2.1 (1.7 to 2.6)* | 2.5 (1.7 to 3.7)* | 2.3 (1.5 to 3.5)* |
| Good health–intermediate education | 1.4 (1.2 to 1.6)* | 1.5 (1.2 to 1.8)* | 1.6 (1.2 to 2.3)* | 1.8 (1.3 to 2.6)* |
| Poor health–high education | 2.1 (1.6 to 2.6)* | 1.6 (1.2 to 2.2)* | 1.4 (0.8 to 2.4)* | 1.2 (0.7 to 2.3) |
| Good health–high education | 1 | 1 | 1 | 1 |
| Age (years) | ||||
| 16–24 | 1.0 (0.9 to 1.3) | 1.0 (0.8 to 1.3) | 0.9 (0.6 to 1.4) | 0.9 (0.6 to 1.4) |
| 25–44 | 0.8 (0.7 to 0.9)* | 0.8 (0.6 to 1.0)* | 0.8 (0.5 to 1.1) | 0.7 (0.5 to 1.0) |
| 45–54 | 0.8 (0.7 to 0.9)* | 0.8 (0.6 to 1.0) | 0.9 (0.6 to 1.3) | 0.8 (0.5 to 1.2) |
| 55–64 | 1 | 1 | 1 | 1 |
| Married | 0.7 (0.6 to 0.7)* | 0.7 (0.6 to 0.8)* | 0.7 (0.6 to 0.9)* | 0.8 (0.6 to 0.9)* |
| Children <12 years | 1.2 (1.1 to 1.3)* | 1.1 (1.0 to 1.3) | 1.1 (0.9 to 1.4) | n/a |
| Personal income | ||||
| >75th centile | 0.2 (0.2 to 0.3)* | 0.2 (0.2 to 0.3)* | 0.3 (0.3 to 0.5)* | 0.4 (0.3 to 0.6)* |
| 25–75th centile | 0.5 (0.4 to 0.5)* | 0.4 (0.4 to 0.5)* | 0.5 (0.4 to 0.6)* | 0.5 (0.4 to 0.7)* |
| <25th centile | 1 | 1 | 1 | 1 |
n/a = not available in data collection.
*Wald's χ2 test, p<0.05.
†Significant interaction.
Among subjects aged ⩾55 years, those with a poor health had a higher chance of retiring the next year than those with a good health (table 4). Among highly educated subjects, this association was not observed for the health status 2, 3 and 4 years before the year of retirement. Being married reduced the likelihood of retirement. Being a breadwinner, sex and personal income all had ORs close to unity. The influence of a chronic health problem on (early) retirement closely mirrored the results of a perceived poor health.
Table 4 Multivariate models with different time windows of significant determinants of retirement among workers aged 55–65 years in the European Household Panel Survey with at least 2 consecutive previous years of employment before retirement.
| Determinant | Years before retirement | |||
|---|---|---|---|---|
| 1 year | 2 years | 3 years | 4 years | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| n (stayed employed) | 3140 | 3167 | 2097 | 1778 |
| n (became retired) | 1374 | 1384 | 806 | 345 |
| Poor health–low education† | 1.7 (1.4 to 2.2)* | 1.7 (1.3 to 2.1)* | 1.4 (1.0 to 1.9)* | 1.6 (1.0 to 2.4)* |
| Good health–low education | 1.3 (1.0 to 1.6)* | 1.2 (1.0 to 1.5) | 1.2 (0.9 to 1.5) | 1.2 (0.8 to 1.8) |
| Poor health–intermediate education | 2.0 (1.6 to 2.7)* | 1.8 (1.3 to 2.4)* | 1.7 (1.2 to 2.6)* | 1.7 (1.0 to 2.9)* |
| Good health–intermediate education | 1.4 (1.1 to 1.6)* | 1.3 (1.1 to 1.7)* | 1.2 (0.8 to 1.7) | 1.1 (0.7 to 1.7)* |
| Poor health–high education | 1.5 (1.0 to 2.2)* | 1.1 (0.8 to 1.6) | 0.8 (0.5 to 1.3) | 1.1 (0.6 to 2.1) |
| Good health–high education | 1 | 1 | 1 | 1 |
| Married | 0.8 (0.7 to 1.0)* | 0.8 (0.7 to 1.0)* | 0.8 (0.7 to 1.0) | 0.9 (0.6 to 1.2) |
n/a = not available in data collection.
*Wald's χ2 test, p<0.05.
†Significant interaction.
Table 5 demonstrates that taking care of the household was influenced by health among unmarried women (OR = 1.6) but not among married women. This interaction was not observed in earlier years. Leaving the workforce to take care of the household was consistently associated with older age, having young children, low personal income and low educational level.
Table 5 Multivariate models with different time windows of significant determinants of leaving employment for household care among women in the European Household Panel Survey with at least 2 consecutive previous years of employment before leaving the workforce to take care of household.
| Years before leaving the workforce to take care of household | ||||
|---|---|---|---|---|
| 1 year | 2 years | 3 years | 4 years | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| n (stayed employed) | 18 100 | 13 818 | 11 351 | 10 419 |
| n (household) | 1000 | 608 | 229 | 193 |
| Poor health–married | 2.6 (2.0 to 3.3)* | 2.1 (1.5 to 2.8)* | 1.7 (1.1 to 2.7)* | 1.3 (0.8 to 2.2) |
| Good health–married | 2.4 (2.0 to 3.0)* | 1.9 (1.4 to 2.4)* | 1.7 (1.1 to 2.6)* | 1.7 (1.1 to 2.5)* |
| Poor health–not married | 1.6 (1.1 to 2.3)* | 1.3 (0.9 to 2.0) | 0.7 (0.3 to 1.4) | 0.9 (0.4 to 1.7) |
| Good health–not married | 1 | 1 | 1 | 1 |
| Age (years) | ||||
| 16–24 | 0.5 (0.4 to 0.7)* | 0.4 (0.3 to 0.7)* | 0.6 (0.3 to 1.2) | 0.6 (0.3 to 1.2) |
| 25–44 | 0.4 (0.3 to 0.5)* | 0.4 (0.3 to 0.5)* | 0.4 (0.3 to 0.7)* | 0.4 (0.2 to 0.6)* |
| 45–54 | 0.4 (0.3 to 0.5)* | 0.4 (0.3 to 0.6)* | 0.5 (0.3 to 0.9)* | 0.4 (0.2 to 0.7)* |
| Educational level | ||||
| High | 0.6 (0.5 to 0.8)* | 0.7 (0.5 to 0.9)* | 0.8 (0.5 to 1.2) | 0.7 (0.5 to 1.2) |
| Intermediate | 0.8 (0.7 to 1.0)* | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.3) | 0.9 (0.6 to 1.3) |
| Low | 1 | 1 | 1 | 1 |
| Children <12 years | 1.9 (1.6 to 2.2)* | 1.6 (1.3 to 1.9)* | 1.1 (0.8 to 1.5) | n/a |
| Personal income | ||||
| >75th centile | 0.3 (0.2 to 0.4)* | 0.2 (0.2 to 0.4)* | 0.4 (0.2 to 0.6)* | 0.3 (0.2 to 0.6)* |
| 25–75th centile | 0.4 (0.3 to 0.4)* | 0.4 (0.3 to 0.5)* | 0.4 (0.3 to 0.6)* | 0.6 (0.4 to 0.8)* |
| <25th centile | 1 | 1 | 1 | 1 |
n/a = not available in data collection.
*Wald's χ2 test, p<0.05.
†Significant interaction.
In table 6, the country‐specific associations are presented for 11 countries (Luxembourg not included as associations were not estimable there because of very small numbers). In 9 of 11 European countries, a perceived poor health was a risk factor for staying unemployed, varying from OR = 0.2 in Denmark to OR = 0.7 in Germany and France, although this association reached the conventional level of statistical significance in only four countries. In 7 of 11 countries, a perceived poor health increased the risk of becoming unemployed, varying from OR = 1.2 in France to OR = 2.7 in The Netherlands. Among older workers, a perceived poor health raised the likelihood of retirement in nine countries, with small effects observed in France and the UK (OR = 1.1) and significantly large effects in Belgium (OR = 2.6) and Germany (OR = 2.6). For poor health and a chronic health problem, in general, comparable associations were found, with the exception of two countries. In Italy, a chronic health problem predicted remaining unemployed (OR = 0.4), but poor health had no discernable impact (OR = 1.0). In The Netherlands, a chronic health problem seemed to increase the likelihood of retirement among older workers (OR = 1.7), whereas a poor health decreased retirement (OR = 0.6), although both associations were not statistically significant.
Table 6 Influence of perceived poor health and chronic health problems in the previous year on employment transitions in the next year among subjects from the European Household Panel Survey in 11 European countries.
| Country | From unemployed to employed | From employed to unemployed | From employed to retired (>55 year) | |||
|---|---|---|---|---|---|---|
| n | OR | n | OR | n | OR | |
| Germany | 483 | 9530 | 796 | |||
| Perceived poor health | 0.7 (0.5 to 1.1) | 2.6 (2.1 to 3.8)* | 2.6 (1.8 to 3.8)* | |||
| Chronic health problem | 0.9 (0.5 to 1.3) | 2.2 (1.8 to 2.7)* | 2.4 (1.7 to 3.4)* | |||
| Denmark | 130 | 2564 | 223 | |||
| Perceived poor health | 0.2 (0.1 to 0.7)* | 2.0 (1.3 to 3.2)* | 1.6 (0.8 to 3.0) | |||
| Chronic health problem | 0.5 (0.2 to 1.2) | 1.2 (0.8 to 1.8) | 1.1 (0.7 to 2.0) | |||
| The Netherlands | 344 | 3804 | 130 | |||
| Perceived poor health | 0.3 (0.2 to 0.6)* | 2.7 (1.8 to 4.0)* | 0.6 (0.1 to 5.8) | |||
| Chronic health problem | 0.4 (0.3 to 0.8)* | 2.8 (198 to 4.3)* | 1.7 (0.3 to 10.8) | |||
| Belgium | 280 | 2699 | 134 | |||
| Perceived poor health | 0.6 (0.2 to 1.3) | 1.6 (1.0 to 2.6) | 2.6 (1.1 to 6.3)* | |||
| Chronic health problem | 0.3 (0.1 to 1.4) | 1.3 (0.6 to 2.5) | 1.5 (0.6 to 4.4) | |||
| France | 485 | 5609 | 370 | |||
| Perceived poor health | 0.7 (0.4 to 1.1) | 1.2 (1.0 to 1.6) | 1.1 (0.7 to 1.7) | |||
| Chronic health problem | 0.8 (0.5 to 1.4) | 1.2 (0.9 to 1.7) | 1.5 (0.9 to 2.6) | |||
| United Kingdom | 229 | 7109 | 605 | |||
| Perceived poor health | 0.4 (0.2 to 0.8)* | 1.8 (1.3 to 2.6)* | 1.1 (0.7 to 1.8) | |||
| Chronic health problem | 0.4 (0.2 to 0.8)* | 1.2 (0.9 to 1.8) | 1.5 (1.0 to 2.3) | |||
| Ireland | 260 | 2860 | 299 | |||
| Perceived poor health | 0.6 (0.3 to 1.3) | 0.6 (0.2 to 1.5) | 1.4 (0.7 to 2.7) | |||
| Chronic health problem | 0.7 (0.3 to 1.6) | 0.8 (0.4 to 1.7) | 1.4 (0.7 to 2.7) | |||
| Italy | 891 | 6238 | 554 | |||
| Perceived poor health | 1.0 (0.7 to 1.5) | 1.0 (0.7 to 1.3) | 0.8 (0.6to 1.1) | |||
| Chronic health problem | 0.4 (0.2 to 0.9)* | 0.9 (0.5 to 1.6) | 0.9 (0.5 to 1.5) | |||
| Greece | 385 | 3740 | 489 | |||
| Perceived poor health | 1.2 (0.5 to 2.5) | 1.3 (0.8 to 2.0) | 1.3 (0.9 to 2.0) | |||
| Chronic health problem | 0.7 (0.2 to 2.1) | 1.0 (0.6 to 1.8) | 0.9 (0.6 to 1.6) | |||
| Spain | 784 | 4897 | 410 | |||
| Perceived poor health | 0.6 (0.4 to 0.9)* | 0.9 (0.7 to 1.2) | 1.5 (1.0 to 2.4)* | |||
| Chronic health problem | 0.4 (0.3 to 0.7)* | 1.1 (0.8 to 1.4) | 1.3 (0.8 to 2.0) | |||
| Portugal | 191 | 4851 | 669 | |||
| Perceived poor health | 0.5 (0.3 to 1.0)* | 1.0 (0.7 to 1.2) | 1.5 (1.0 to 2.4) | |||
| Chronic health problem | 0.9 (0.4 to 2.1) | 1.5 (1.1 to 2.0)* | 1.8 (1.2 to 2.7)* | |||
*Wald's χ2 test, p<0.05, adjusted for age, sex, marital status, education and personal income.
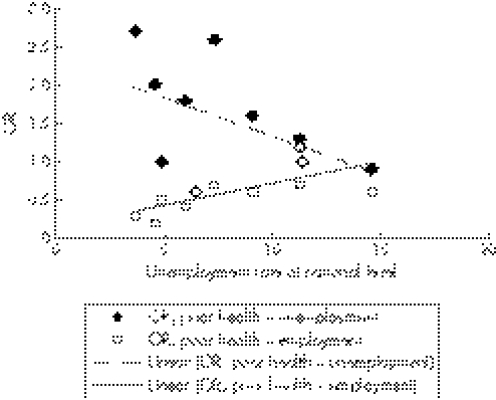
Figure 2 illustrates that a lower unemployment rate at national level in 1998 was associated with larger effects of poor health on not entering employment (regression coefficient = 0.06, R2 = 0.46, p = 0.02) and larger effects of poor health on becoming unemployed (regression coefficient = –0.10, R2 = 0.27, p = 0.10). This trend over countries was not observed for the effects of poor health on retirement or taking care of household.
Figure 2 The magnitude of the association between a perceived poor health and becoming unemployed or entering employment (OR) against the national unemployment rate in 1998 among 11 countries in the European Household Panel Survey.
Discussion
This study shows that the effects of health on transitions between paid employment and various forms of non‐employment were influenced by sociodemographic variables. A poor health was a risk factor for remaining unemployed among men, but had less effect among women. A poor health was also a risk factor for becoming unemployed or retiring, especially among highly educated workers. Finally, among women, the transition from employment into taking care of a household was influenced by poor health only among unmarried women. In most European countries, poor health and a chronic health problem were risk factors for not entering the workforce or becoming unemployed, but large differences among countries were observed that could partly be explained by the unemployment rate at national level.
These conclusions are based on the European Household Panel Survey. An obvious disadvantage of the current analysis is the restriction to two measures of self‐reported health. Both measures of health were strongly correlated, as one would expect. Unfortunately, no information was available on self‐reported or diagnosed specific diseases and, hence, it was not possible to evaluate which particular diseases largely explained the role of health in entering or leaving the workforce. The ordinal measurement and subsequent dichotomising of self‐perceived health may hamper comparability across countries and, indeed in our study populations, the prevalence of poor health varied from about 8% in Greece and Ireland to over 40% in Portugal and Germany. However, the magnitude of the prevalence was not associated with the observed ORs for poor health. In addition, when using a more stringent cut‐off point for a poor health (only including subjects with bad or very bad health), results remained largely similar, although the ORs for the effects of poor health and intermediate or high education on becoming unemployed or retiring were somewhat higher than those presented in tables 3 and 4. This suggests that the distributional differences among countries have not invalidated our findings.
A second drawback was the large variation in household responses, which in some countries were very low, most notably in Germany (48%) and Ireland (56%). In addition, among subjects lost to follow‐up between annual questionnaires (attrition rate), those with younger age, lower education, unmarried and male gender were over‐represented.16 The low household response in some countries could be influenced by health, but whether differential bias is present remains unknown. As the national attrition rate was not associated with the prevalence of perceived poor health at baseline, we do not expect a substantial bias in the non‐response during the follow‐up.
A third disadvantage was the use of self‐reported labour status, which may differ from official definitions. For example, a person may consider himself as unemployed only when he is actively looking for work, whereas others on unemployment benefit may have categorised themselves as economically inactive. Another example is the inability to distinguish illness‐based unemployment or retirement from non‐illness‐based unemployment or retirement. Subjects becoming or remaining unemployed may include a substantial proportion of subjects with (work‐related) disability. In the baseline survey, approximately 2% of the respondents classified as unemployed stated that the main reason for not seeking work was their own illness, injury or incapacitation. Hence, this will have only a small effect on the observed influence of poor health on the likelihood of entering paid employment.
The results of this study support the existence of a health selection in the workforce as healthier people are more likely to become or remain employed than less healthy people. Several studies have reported a similar impact of health on entering paid employment or leaving the workforce. Iversen and Sabroe20 showed that psychological health remained stable for those employed or unemployed during a 2‐year follow‐up, whereas for those losing or gaining employment, psychological health decreased or increased, respectively. The likelihood of finding paid work was negatively influenced by mental health problems in British workers7 and by health‐related difficulties in Finland.21 A Swedish longitudinal study showed that subjects with limiting longstanding illness had an increased risk of becoming unemployed10 and, among Finnish middle‐aged men, a poor health predicted non‐illness‐based early retirement.11 The influence of age, education, and marital status on employment status reflects well‐known labour market conditions—for example, in almost every European country, unemployment is highest among younger people and among those with a low level of educational attainment.22 The specific contribution of the current study is that it shows that poor health had a long‐term effect on entering paid employment, but a much more transient effect on leaving the workforce. Poor health was a risk factor for not entering paid employment already four years before the potential transition into the workforce. This suggests that the health status among unemployed subjects with poor health remains rather stable over time and, hence, has a long‐term effect on the probability of entering paid employment. In contrast, the effects of poor health on unemployment, retirement or taking care of household were less pronounced in more distant years, suggesting a more transient pattern, with a change in health being the risk factor rather than poor health.
Few studies have reported on interactions between health status and socioeconomic position. McDonough and Amick13 demonstrated that, in the USA, the effect of perceived ill health on labour market exit depended on sex, race and education. Poor health was a more important factor in leaving the workforce among men than among women, and the effect of poor health on labour force exit increased with education. Both findings were corroborated in our study (tables 2 and 3, respectively). The effect of health on employment status will differ across different socioeconomic positions as the consequences of poor health also depend on social and labour market circumstances. These latter circumstances vary across the 11 European countries in our study—for example, by the level of protection for workers with chronic diseases against workforce exclusion and rehabilitation policies, to include people with poor health in regular or sheltered employment.23 It may be hypothesised that countries wherein a poor health status was a strong predictor for labour force exit were less successful in retaining those with a poor health status in the labour force.14 An alternative explanation may be that in countries where this association was not observed, health is less important than other factors in determining employment status. Figure 2 suggests that, in countries with a low national unemployment rate, health will compete with other labour market factors in the process of entering or retaining paid employment, whereas in countries with a high national unemployment rate, the effect of health selection out of the workforce is relatively small compared with other factors that determine labour opportunities for people. However, this finding does not suggest that in these latter countries, health selection per sé is not important, but rather that it cannot be demonstrated in the current analysis.
An important question is what society should do with unhealthy job seekers and unhealthy workers. Preventive public health interventions should not only address the health selection out of the workforce, but also take into consideration that being unemployed can lead to further deterioration of the health status, long‐term unemployment and social exclusion.23 Ill health is an important determinant for entering and maintaining paid employment in many European countries. These consequences of ill health will increase socioeconomic inequalities in health. It has been reported before that unemployment, retirement and work disability explain a great deal of health inequalities across European countries.24 In policies for health equity, it is of paramount importance to develop public health measures, tailored to sociodemographic characteristics, that include people with a poor health in the labour market and prevent workers with ill health from dropping out of the workforce.
Key messages
In European countries, ill health is an important determinant for becoming and staying unemployed.
Ill health also increases the likelihood of voluntary early retirement.
The effect of ill health on labour force exit depends strongly on education, sex and family situation.
Policy implications
Preventive public health measures should prevent workers with ill health from dropping out of the workforce.
Socioeconomic inequalities in health can be reduced by increasing labour participation.
Abbreviations
ECHP - European Community Household Panel
Footnotes
Competing interests: None declared.
References
- 1.Acheson D. Independent inquiry into inequalities in health. London: The Stationary Office, 1998, http://www.archive.official‐documents.co.uk/document/doh/ih/ih.htm
- 2.Marmot M G, Smith G, Stansfield S.et al Health inequalities among British civil servants: the Whitehall II study. Lancet 19913371387–1393. [DOI] [PubMed] [Google Scholar]
- 3.Claussen B. Health and re‐employment in a five‐year follow up of long‐term unemployed. Scand J Public Health 19992794–100. [PubMed] [Google Scholar]
- 4.Janlert U. Unemployment as a disease and diseases of the unemployed. Scand J Work Environ Health 199723(Suppl 3)79–83. [PubMed] [Google Scholar]
- 5.Morris J K, Cook D G, Shaper A G. Loss of employment and mortality. BMJ 19943081135–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartley M, Sacker A, Clarke P. Employment status, employment conditions, and limiting illness: prospective evidence from the British household panel survey 1991–2001. J Epidemiol Community Health 200458501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas C, Benzeval M, Stansfeld S A. Employment transitions and mental health: an analysis from the British household panel survey. J Epidemiol Community Health 200559243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy G C, Athanasou J A. The effect of unemployment on mental health. J Occup Organ Psychol 19997283–99. [Google Scholar]
- 9.Claussen B, Bjorndal A, Hjort P F. Health and re‐employment in a two‐year follow up of long‐term unemployed. J Epidemiol Community Health 19934714–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindholm C, Burström, Diderichsen F. Class differences in the social consequences of illness? J Epidemiol Community Health 200256188–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karpansalo M, Manninen P, Kauhanen J.et al Perceived health as a predictor of early retirement. Scand J Work Environ Health 200430287–292. [DOI] [PubMed] [Google Scholar]
- 12.Loprest P, Davidoff A. How children with special health care needs affect the employment decisions of low‐income parents. Matern Child Health J 20048171–182. [DOI] [PubMed] [Google Scholar]
- 13.McDonough P, Amick B C., III The social context of health selection: a longitudinal study of health and employment. Soc Sci Med 200153135–145. [DOI] [PubMed] [Google Scholar]
- 14.OECD (Organisation for Economic Cooperation and Development) Transforming disability into ability. Policies to promote work and income security for disabled people. Paris: OECD, 2003
- 15.Eurostat European Community Household Panel, Users' Database Manual (Version of November 1999), Luxembourg 1999
- 16.Peracchi F. The European Community Household Panel: a review. Emp Econ 20022763–90. [Google Scholar]
- 17.Huisman M, Kunst A E, Mackenbach J P. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med 200540756–764. [DOI] [PubMed] [Google Scholar]
- 18.UNESCO International standard classification of education. Paris: UNESCO, 1997
- 19.Fayers P M, Sprangers M A G. Understanding self‐rated health. Lancet 2002359187–188. [DOI] [PubMed] [Google Scholar]
- 20.Iversen L, Sabroe S. Psychological well‐being among unemployed an employed people after a company closedown: a longitudinal study. J Soc Issues 198844141–152. [Google Scholar]
- 21.Pohjola A. Health problems and long‐term unemployment. Soc Work Health Care 200134101–112. [DOI] [PubMed] [Google Scholar]
- 22.Eurostat European union labour force study. http://forum.europa.eu.int/irc/dsis/employment/info/data/eu_lfs (accessed on 19 Feb 2007)
- 23.Grammenos S.Illness, disability and social inclusion. Longlinstown: European Foundation for the Improvement of Living and Working Conditions, 2003, (ISBN 92‐897‐022104)
- 24.Van Doorslaer E, Koolman X. Explaining the differences in income‐related health inequalities across European countries. Health Econ 200413609–628. [DOI] [PubMed] [Google Scholar]