Abstract
PURPOSE
To test the efficacy of resveratrol, a nontoxic plant product, in the treatment of uveal melanoma.
METHODS
The effect of oral administration and peritumor injection of resveratrol was tested on tumor growth in two animal models of uveal melanoma. The mechanism of resveratrol action on uveal melanoma cells was studied in vitro in a cell-viability assay: with JC-1 dye, to measure mitochondrial membrane potential; by Western blot analysis, to analyze the cellular redistribution of cytochrome c and Smac/diablo; and in a fluorescence assay with specific substrates, to measure activation of different caspases.
RESULTS
Resveratrol treatment inhibited tumor growth in animal models of uveal melanoma. Since oral administration resulted in relatively low bioavailability of resveratrol, the effect of increased local levels was tested by peritumor injection of the drug. This method resulted in tumor cell death and tumor regression. In vitro experiments with multiple uveal melanoma cell lines demonstrate that resveratrol causes a decrease in cell viability, resulting at least in part from an increase in apoptosis through a mitochondrial pathway. An early event in drug action is the direct targeting of mitochondria by resveratrol, which leads to a decrease in mitochondrial membrane potential and the eventual activation of caspase-3.
CONCLUSION
These data suggest that resveratrol can inhibit tumor growth and can induce apoptosis via the intrinsic mitochondrial pathway and that by further increasing bioavailability of resveratrol the potency of the drug can be increased, leading to tumor regression. The nontoxic nature of the drug at levels needed for therapy make resveratrol an attractive candidate for the treatment of uveal melanoma.
Uveal melanoma is the most common primary ocular tumor in adults with approximately 1300 to 2000 new cases occurring in the United States each year. Depending on size and other parameters, traditional treatment of the primary tumor has been enucleation. However, alternative treatments to preserve the eye have been devised, including cryotherapy, radioactive therapy, transpupillary thermotherapy, surgical resection, and photocoagulation. Despite these advances in treatment, mortality varies considerably, to more than 50% in high-risk patients, primarily due to metastasis to the liver.1 Although the incidence of overt metastases is low (2%–3%) at the time of presentation of the primary tumor,2,3 it is hypothesized that micrometastases already have been established.4 These may remain dormant for many years before enlargement occurs.5,6 Therefore, it is critical to develop drugs that are nontoxic and can be administered for potentially extended periods to patients who have received a diagnosis of primary uveal melanoma.
Resveratrol (3,5,4′-trihydroxy-trans-stilbene) is a nontoxic, plant-derived polyphenol found in grapes, berries, and peanuts. It has been found to be effective against a wide range of tumor cells in tissue culture as well as in certain animal models. 7 However, no studies have been conducted to show the effect of resveratrol on uveal melanoma cells in vitro or in vivo.
Resveratrol has pleiotropic effects, altering many different signaling pathways leading to suppression of tumor cell proliferation and metastasis, as well as reduced signs of inflammation and angiogenesis and induction of apoptosis and differentiation.7 Although numerous studies have described intracellular changes leading to cell cycle arrest or apoptosis in response to resveratrol treatment, the effects are often cell-type specific, and these studies have not yet identified the underlying mechanism of drug action.7,8
Mitochondrial involvement in resveratrol-induced cell death has been described.9–12 Mitochondrial dysfunction is a prominent signal for apoptosis as part of the intrinsic apoptosis pathway. Loss of membrane potential can signal apoptosis by a decrease in the Bcl-2–Bax ratio associated with mitochondria and the release of cytochrome c and Smac/Diablo from mitochondria, leading to the activation of caspase-9 via APAF-1 and to the activation of caspase-3 (for review see Ref. 13). Finally, the resultant induction of nucleases leads to DNA fragmentation and cell shrinkage, nuclear condensation, and membrane blebbing.
In the current study, resveratrol inhibited uveal melanoma cells by directly targeting the mitochondria, thereby activating the intrinsic mitochondrial pathway leading to release of cytochrome c and Smac/Diablo, activation of caspase-9 and -3, and, finally, tumor cell death. We also show that oral administration of resveratrol is effective at inhibiting tumor growth in two xenograft models of human uveal melanoma, using cells derived from a primary tumor and from a metastatic lesion. In addition, we find that direct injection of resveratrol adjacent to the tumor to elevate levels of the drug enhances tumor cell death. Therefore, resveratrol is a good candidate for therapeutic intervention in uveal melanoma, owing to its nontoxic characteristics and its potent antitumor effect.
METHODS
Cell Culture
Uveal melanoma cell lines were grown as adherent cells at 37°C, 5% CO2 in DMEM (M619, C918, Mum2b), RPMI medium supplemented with 10 mM HEPES (OCM-1, OCM-3, Mel290, and Mel270), and RPMI supplemented with 10 mM HEPES (Mediatech, Herndon, VA), 10 mM sodium pyruvate (Sigma-Aldrich, St Louis, MO), 1% nonessential amino acids (Hyclone, Logan, UT), and 1% MEM vitamin mixture (92.1). All media were supplemented with 10% vol/vol FBS (Atlanta Biologicals, Norcross, GA), and 1% penicillin-streptomycin-amphotericin B (Mediatech).
Inoculation of Mice
C918 and Mum2b cells (1 × 106) were mixed 1:1 with synthetic matrix (Matrigel; BD Bioscience, Bedford, MA) and injected subcutaneously (SC) into the flanks of athymic mice (Harlan, Indianapolis, IN), which were subsequently divided into groups of 15 animals each. Protocols were approved by the University of Wisconsin-Madison Research Animals Resources Center and adhered to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. Five days after inoculation, the resveratrol (Cayman Chemicals, Ann Arbor, MI) in triglyceride of Coconut Oil (Neobee M5 oil; Spectrum Chemical Mfg. Corp., Gardena, CA) or oil alone was administered to the experimental and vehicle groups, respectively, by oral gavage daily for 3 to 5 weeks, and the growth rate of SC tumors was monitored. Tumor size in the animals was measured as described.14 Tumor volume was analyzed by using a 1-way analysis of variance (ANOVA) test to detect statistical differences in tumor size among the groups. Tumor volume was transformed to the log scale before analysis to obtain approximately normal distribution residuals. Differences were considered significant at P < 0.05.
Peritumor Injections
C918 cells (3 × 106) were injected SC in 10 athymic mice and the tumors allowed to grow to approximately 200 mm3. The mice were divided into two groups of five animals each and administered three injections over 8 days of 20 mg resveratrol in 200 μL DMSO or DMSO alone. The animals were euthanatized, and tumor tissue was fixed in formalin, sectioned, and stained with hematoxylin-eosin (H&E).
Resveratrol Bioavailability
Resveratrol measurements in tissue homogenates or in sera by column chromatography were performed as described elsewhere.14
Tumor Cell Viability
Uveal melanoma cell viability was measured as described elsewhere.15
Apoptosis Determinations
The cells were treated with 100 μM resveratrol and then fixed, stained with Hoechst 33528 (Invitrogen-Molecular Probes, Eugene, OR), and analyzed according to a published method.16 The percentage of apoptotic cells was calculated as the number of apoptotic cells relative to the total number of cells in a viewing field and averaged over five different fields.
Isolation of Mitochondria
Mitochondria were isolated from 5 × 107 cells, as described elsewhere. 16
Mitochondrial Membrane Potential
Changes in mitochondrial membrane potential in whole cells and in isolated mitochondria were measured by fluorometry with JC-1 dye (Cell Technology, Mountain View, CA), as described elsewhere.16 The mitochondrial membrane potential drives the formation of red fluorescing JC-1 dimers (J aggregates). The ratio of red fluorescent dimers to green fluorescent monomers is a measure of the mitochondrial membrane potential.
Cytochrome c and Smac/Diablo Release
Cytochrome c and Smac/Diablo were compared by immunostaining cytosolic fractions prepared from 6 ×106 cells either treated with 100 μM resveratrol or left untreated. Cell fractionation was achieved as described earlier.16 Protein concentration was measured using a protein assay (BioRad, Hercules, CA). Western blot analysis was performed using 15% SDS-polyacrylamide gels followed by electrotransfer of proteins to PVDF membrane for immunodetection using either anti-cytochrome c (BD PharMingen, San Diego, CA) or anti-Smac/Diablo (Cell Signaling Technology, Danvers, MA) antibodies. Purity of the cytoplasmic and mitochondrial fractions was ascertained with anti-GAPDH and anti-cytochrome oxidase antibodies.
Caspase Activity
Cell lysates were prepared, and for caspase-9 activation, 50 μg of total protein, and for caspase-3 activation, 20 μg of total protein from each lysate was assayed by fluorometry using fluorogenic peptides, as described elsewhere.15 Caspase-8 activation was measured by Western blot analysis with an anti-caspase-8 antibody (Cell Signaling Technology).
RESULTS
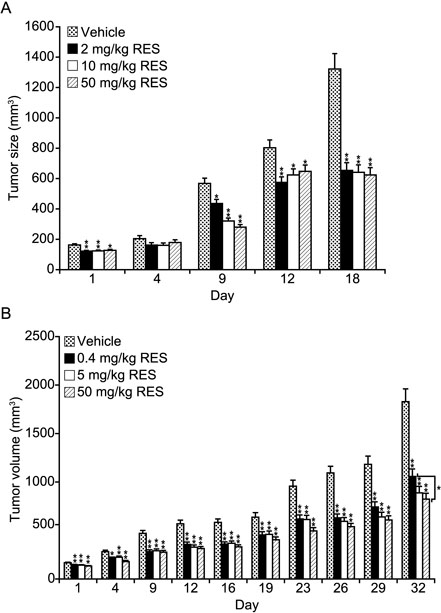
To determine whether resveratrol is effective in inhibiting uveal melanoma tumor growth, we tested mouse xenograft models of human uveal melanoma cell lines. Dose–response experiments were performed with C918 (originally derived from a primary uveal melanoma) and Mum2b (originally derived from a metastatic lesion) cells. The mice were treated daily with resveratrol, starting 5 days after inoculation when tumors were smaller than 50 mm3. After 3 to 5 weeks of oral drug treatment, tumor growth was strongly inhibited in the C918 xenograft model at the 2- to 50-mg/kg doses and at the 5- to 50-mg/kg doses in the Mum2b model (Table 1). Tumor growth was inhibited proportionately less at the lowest dose (0.4 mg/kg) compared with the control group that received vehicle alone (Table 1). Tumor volume was approximately 50% less at doses more than 2 mg/kg in both mouse models compared with the control group (P < 0.0001 for all groups). The 0.4-mg/kg group showed a significant decrease in response compared with the 50-mg/kg group in both mouse models (P = 0.03). Growth kinetic data show that significant differences between the treated and untreated tumors were apparent almost immediately after initiation of drug treatment (Fig. 1). However, no tumor regression was observed.
TABLE 1.
Inhibition of Uveal Melanoma Tumor Growth
| Tumor Size (mm3) |
Standard Error |
P* | ||
|---|---|---|---|---|
| C918 Vehicle | 1204.99 | 87.89 | ||
| 2 mg/kg RES | 610.02 | 44.50 | <0.0001 | |
| 10 mg/kg RES | 607.39 | 44.30 | <0.0001 | |
| 50 mg/kg RES | 599.39 | 43.72 | <0.0001 | |
| Mum2b Vehicle | 1700.05 | 160.35 | ||
| 0.4 mg/kg RES | 971.78 | 62.23 | <0.0001 | |
| 5 mg/kg RES | 835.92 | 56.49 | <0.0001 | |
| 50 mg/kg RES | 808.23 | 45.13 | <0.0001 | |
End tumor volumes after 3 and 5 weeks of oral resveratrol (RES) treatment in the xenograft models.
Compared with the control group.
Figure 1.
Inhibition of uveal melanoma tumor growth. Tumor growth kinetics during resveratrol treatment of C918 (A) and Mum2b (B) xenograft models by oral gavage. Data show the average tumor growth in resveratrol- and vehicle-treated groups of mice. *P < 0.05, **P < 0.0005.
Toxicity was assessed by survival, activity and, twice weekly, by body weight. All animals survived the treatment without evidence of toxic effects and animals gained 10% to 15% of weight compared with their pretreatment values. On autopsy, no changes were observed in the major organs after treatment with the highest dose of resveratrol. This is supported by toxicity studies of resveratrol (reviewed in Ref. 17).
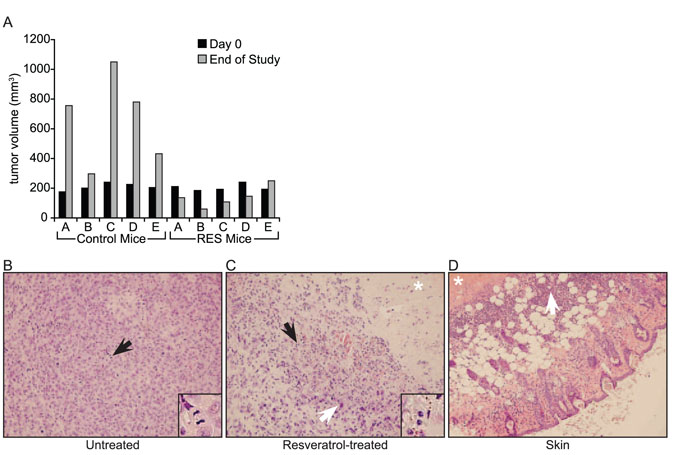
Bioavailability of resveratrol in serum was determined 30 minutes after oral administration of 0.4, 2, 10, and 50 mg/kg of resveratrol and found to be 0.6 ± 0.28, 1.4 ± 0.49, 1.3 ± 0.21, and 4.3 ± 0.14 μM, respectively. No accumulation of resveratrol was found in tumor tissue. Our experiments showed that these relatively low levels were nonetheless sufficient to inhibit tumor growth. To determine whether the inhibitory effects of resveratrol on tumors can be enhanced, especially given the proapoptotic effects of the drug observed on cells in vitro (described later), we assessed the effect of higher doses of resveratrol on tumor growth and viability. To this end, the drug was directly injected next to the tumor in a series of three injections. This resulted in a decrease in tumor volume in four of five mice compared with the vehicle-treated control animals, all of which increased in volume (Fig. 2A). Vehicle-treated tumor tissue showed the presence of healthy tumor cells with clear borders and the presence of many mitotic figures (Fig. 2B). In the resveratrol-treated tumors, there were areas of necrosis, increased presence of apoptotic cells interspersed with residual surviving tumor cells, and calcified tumor cells (Fig. 2C). Cell borders and nuclear detail were less clear, and, together with cytoplasmic swelling, these changes are consistent with cell damage. Adjacent normal tissue was relatively unaffected. Inflammatory cells were present in the subdermal fat layer and to a lesser degree in the epidermis (Fig. 2D).
Figure 2.
Tumor regression after peritumor injection of resveratrol in the C918 xenograft model. (A) Tumor size before and after three injections of vehicle or 20 mg resveratrol. H&E-stained sections of vehicle-treated tumor (B), 20 mg resveratrol-treated tumor (C), and adjacent normal skin tissue in the resveratrol-treated condition (D). Insets: detail of area around black arrows. (B, inset) Mitotic body; (C, inset) apoptotic cells. (C, D, *) Necrotic area. (C, white arrow) Calcified cell; (D, white arrow) inflammatory cells.
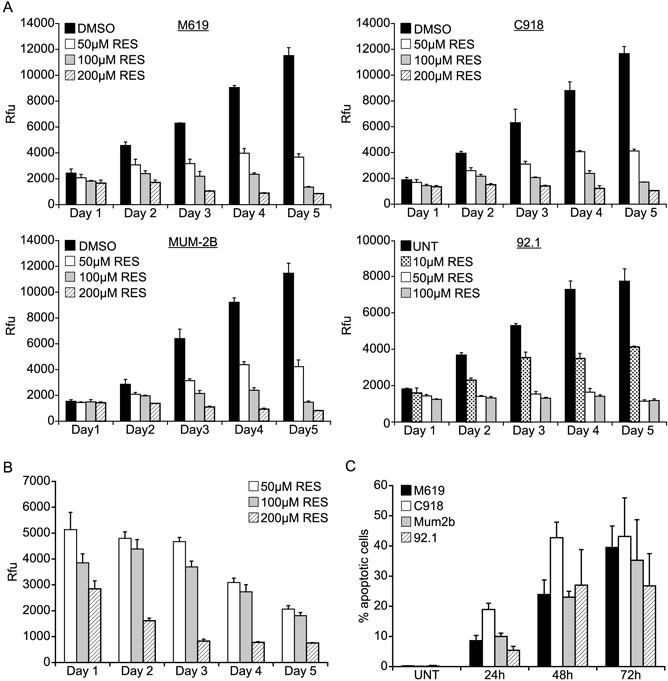
To understand the mechanism of the drug's antitumor activity, we performed in vitro studies on the uveal melanoma cell lines M619, C918, Mum2b, and 92.1. The viability of these cell lines was sharply decreased in response to resveratrol treatment in a time- and concentration-dependent manner (Fig. 3A). Additional cell lines (Ocm1, Ocm3, Mel270, and Mel290) showed similar effects (data not shown). At the highest drug concentration, cell viability decreased approximately 85% to 90% compared with untreated cells after 5 days of treatment. The IC50 of resveratrol after 48 hours of treatment was: M619, 80 μM; C918, 70 μM; Mum2b, 130 μM; and 92.1, 25 μM. If treatment was continued, all cells died after approximately 8 to 10 days. In addition, dense cultures of uveal melanoma cells (>90% confluent) were treated with resveratrol as a function of time and concentration and their viability measured. Under these conditions, cell viability decreased in a concentrationdependent manner over 5 days, further indicating the occurrence of cell death (Fig. 3B).
Figure 3.
Resveratrol decreased the cell viability of uveal melanoma cell lines by inducing apoptosis. (A) The cell viability of M619, C918, Mum2b, and 92.1 cells was measured as a function of resveratrol concentration and time after drug addition and plotted as relative fluorescence units (rfu). (B) Viability of dense (>90% confluent) 92.1 cells was measured similarly. Each experiment was performed in triplicate. (C) Apoptotic nuclei of M619, C918, Mum2b, and 92.1 cells were visualized in resveratrol time courses with Hoechst 33528 dye and plotted as the percentage of apoptotic cells relative to the total number of cells. The number of cells was counted in five different viewing areas by fluorescence microscope and averaged. Experiments were performed in duplicate.
To determine whether resveratrol treatment results in enhanced apoptosis, we treated uveal melanoma cells with 100 μM resveratrol for up to 72 hours, and then stained them with Hoechst 33528 dye, to visualize apoptotic nuclear morphology (Fig. 3C). The percentage of apoptotic M619 and Mum2b cells steadily increased over 72 hours, up to 39% and 36%, respectively. The fraction of apoptotic C918 and 92.1 cells reached a maximum at 48 hours and then leveled off. These results suggest that the decrease in cell viability is at least in part due to an increase in apoptosis.
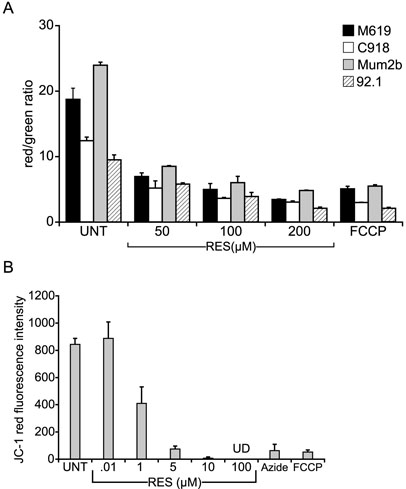
Since resveratrol treatment of tumor cells resulted in ultrastructural damage of the mitochondria before cell death, as indicated by disorganization of the cristae (Sareen D, unpublished observations, 2006), the intrinsic apoptosis pathway, in which the mitochondria play a key role, was studied in uveal melanoma cells. In this pathway, apoptotic stimuli induce mitochondrial dysfunction that in turn signals activation of downstream mediators of cell death. One of the parameters affected when mitochondria become dysfunctional is the mitochondrial transmembrane potential. Therefore, mitochondrial membrane potential was measured by using JC-1 in M619, C918, Mum2b, and 92.1 cells (Fig. 4A). These cell lines showed an early and sustained loss of mitochondrial membrane potential in response to resveratrol treatment. Increasing concentrations of the drug led to increased loss of membrane potential. Both resveratrol and the positive control carbonyl cyanide-p-(trifluoromethoxy)phenylhydrazone (FCCP), a protonophore, caused a collapse of the membrane potential, as indicated by the sharp decrease in the red-green JC-1 ratio. These results suggest a mechanism for resveratrol action involving mitochondrial function leading to apoptosis via the intrinsic pathway. Further, pretreatment with cyclosporin A did not prevent resveratrol-induced membrane potential collapse after 15 minutes of drug treatment. In the absence of cyclosporin A the red-green ratio of untreated and 100 μM resveratrol- treated samples was 112.4 ± 3.9 and 18.0 ± 1.4, respectively. Similarly, in the presence of cyclosporin A the red-green ratio of untreated and 100 μM resveratrol-treated samples was 84.0 ± 16.1 and 14.8 ± 0.6, respectively. Longer incubation of cells with resveratrol for 6 hours gave similar results, suggesting that, at least initially, resveratrol does not cause mitochondrial permeability transitional (MPT) pore opening.
Figure 4.
Resveratrol caused loss of mitochondrial membrane potential in uveal melanoma cells and in isolated mitochondria. Mitochondrial membrane potential in M619, C918, Mum2b, and 92.1 cells (A) and 92.1 mitochondria (B) was measured as a function of resveratrol concentration 15 minutes after drug addition, by using JC-1 dye. As a positive control, the cells were treated with FCCP or sodium azide. Data are plotted as the ratio of red to green fluorescence intensity at 530 and 590 nm, respectively, in cells and as the red fluorescence intensity in isolated mitochondria. Each experiment was performed in duplicate. UD, undetectable.
To test whether the mechanism of resveratrol action involves direct targeting of this organelle, we isolated mitochondria from 92.1 cells, treated with resveratrol and measured the mitochondrial membrane potential with JC-1 dye (Fig. 4B). Since no cytoplasmic compartment is present in these experiments, only the red fluorescence was measured. As an additional positive control, mitochondria were treated with sodium azide, a mitochondrial complex IV inhibitor. Membrane potential of isolated mitochondria was decreased after resveratrol treatment, suggesting that resveratrol causes mitochondrial dysfunction by directly targeting the mitochondria without the need to interact with cytosolic components. As expected, the drug concentration needed to attain these effects was less than needed for whole cells, probably due to the lack of diffusion barriers.
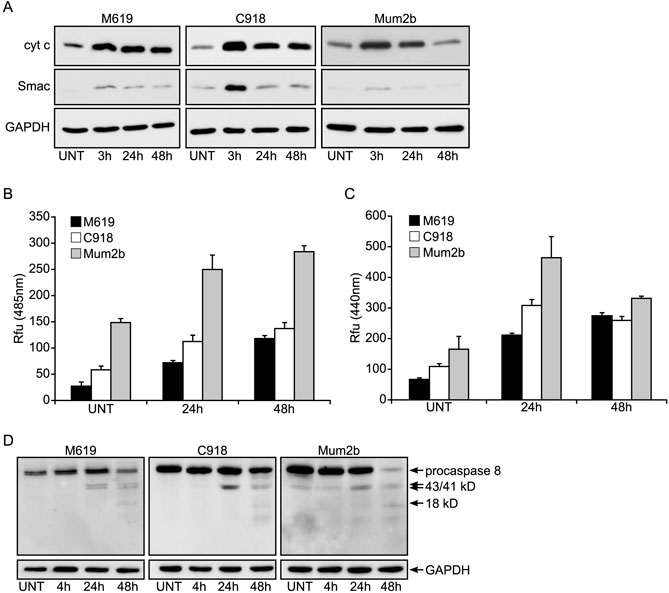
In other cell types, loss of mitochondrial membrane potential with resveratrol treatment is followed by release of cytochrome c and Smac/Diablo from the mitochondria.13 To determine whether this release occurs in uveal melanoma cells, we treated M619, C918, and Mum2b cells with resveratrol, lysed and fractionated the cells, and determined the amount of cytochrome c and Smac/Diablo found in the cytosolic fraction by Western blot analysis. Cytochrome c was released into the cytosol in all three cell types 3 hours after initiating drug treatment (Fig. 5A). Smac/Diablo was also released from the mitochondria in all three cell lines. The kinetics of Smac/Diablo release compared with cytochrome c release in response to resveratrol treatment were similar. In the C918 and Mum2b cells, the highest levels of these proteins in the cytoplasm were observed 3 hours after the addition of the drug, after which they tapered off (Fig. 5A). In contrast, cytochrome c and Smac/Diablo levels remained the same at 24 and 48 hours after treatment in the M619 cells (Fig. 5A).
Figure 5.
Resveratrol causes loss of cytochrome c and Smac/Diablo from the mitochondria and induces activation of caspase-9 and -3. (A) Cytochrome c and Smac/Diablo were measured by Western analysis in the cytoplasmic fractions of M619, C918, and Mum2b cells in a resveratrol time course. Each experiment was performed in duplicate. UNT, untreated cells. Caspase-9 (B) and -3 (C) activation was measured in M619, C918, and Mum2b cells with the substrates Ac-LEHD-AFC and Ac-DEVD-AMC, respectively, in a resveratrol-concentration course and plotted as relative fluorescence units (Rfu) after 48 hours of drug treatment. Each experiment was performed in triplicate. (D) Caspase-8 activation induced by resveratrol in M619, C918, and Mum2b cells was measured in whole cell lysates by Western analysis. The GAPDH level was measured as the loading control. Experiments were performed in duplicate.
To determine whether other components of the mitochondrial cell death pathway were activated, we measured caspase-9 and -3 activities in resveratrol-treated cells in a time-course experiment (Figs. 5B, 5C). These proteins act as executioner enzymes late in the apoptotic process. All three cell lines demonstrated increased activity of these enzymes after 24 hours, suggesting that these downstream components in the intrinsic apoptosis pathway are activated in response to resveratrol treatment.
In some instances, chemical-induced apoptosis can act via the mitochondria18 and involve caspase-8. To determine whether this pathway is activated in response to resveratrol treatment as well, processing of procaspase-8 was measured. Procaspase-8 was cleaved in the M619, C918, Mum2b, and 92.1 cells in a time-dependent manner indicated by the appearance of 43- and 41-kDa intermediate cleavage products and an 18- kDa active product (Fig. 5D).
DISCUSSION
Novel drug therapies are needed to treat uveal melanoma. We demonstrated that resveratrol, a nontoxic plant polyphenol, is very effective at inhibiting human uveal melanoma cells derived from primary and metastatic tumors in animal models of the disease. Both C918 cells and Mum2b cells have been shown to be highly invasive in assays in vitro.19 Furthermore, both cell lines form vascular loops and networks in vitro, further indicative of a more aggressive phenotype.20,21 Our data demonstrate that resveratrol caused a 50% inhibition of tumor growth over a 3- to 5-week period at drug doses from 2 to 50 mg/kg.
The bioavailability of resveratrol in serum was measured as a function of oral drug dose and was found to be between 0.8 and 4.4 μM at 0.4- to 50-mg/kg doses at 30 minutes and near undetectable amounts after 2 hours, in agreement with findings of others.22 This is also similar to preliminary results from a recently initiated human phase I trial of resveratrol where serum levels of approximately 3 μM were measured after an oral dose of 70 mg/kg. (Phase I repeat-dose clinical study of safety, pharmacokinetics, and pharmacodynamics of resveratrol. Available at http://www-personal.umich.edu/~monk/protocols.html.) We also find no accumulation of drug in serum or tumors during the treatment course. Despite these relatively low levels in serum, their presence is sufficient to cause significant inhibition of tumor growth. To enhance local levels of resveratrol, the drug was injected adjacent to the tumor, which resulted in regression in tumor size in four of five resveratrol-treated animals. Histologic examination of tumor sections of drug-treated animals showed an increase in tumor cell death, whereas neighboring tissue was relatively unaffected. These findings are consistent with our in vitro experiments in which resveratrol has a proapoptotic effect at higher concentrations of drug. This suggests that by increasing bioavailability of resveratrol or by tumor-specific targeting, a more potent antitumor effect can be obtained, leading to tumor regression by increased tumor cell death. We are currently pursuing several strategies to attain this goal through different drug delivery routes and the use of chemical analogues of resveratrol. Once this goal has been attained, these results may form the basis for initiation of clinical trials to test the efficacy of the drug in human patients either as a primary treatment or as an adjuvant therapy, especially to validate whether preclinical studies in mice are relevant to the human disease.
To understand the mechanism of resveratrol-induced growth inhibition, four uveal melanoma cell lines were studied in more detail. M619, like C918, is a cell line with high invasive potential derived from primary tumor23; Mum2b is a highly invasive clonal derivative from a metastatic lesion in the liver21; and 92.1 is derived from a primary tumor from a patient in whom liver metastasis later developed.24 Our data suggest that an early mechanism of resveratrol-mediated growth inhibition of uveal melanoma cells involves the mitochondria. We found that shortly after drug administration to cells, there was a collapse in mitochondrial membrane potential. However, this change in membrane potential did not lead to opening of the MPT pore, as indicated by the inability of cyclosporin A to prevent resveratrol-induced loss of membrane potential. Although MPT pore opening after the collapse of the mitochondrial membrane potential occurs in many apoptotic systems leading to loss of apoptogenic factors, such as cytochrome c and Smac/Diablo,25 a loss of membrane potential does not necessarily lead to MPT pore opening.26 In addition, cytochrome c release from the mitochondria can occur in the absence of MPT pores at a distinct Ca2+ threshold.27 Indeed, we have reported a resveratrol-induced increase in cytosolic Ca2+ in breast cancer cells.15 Since resveratrol also causes a decrease in membrane potential in isolated mitochondria, our data suggest that the drug directly targets this organelle. We are currently investigating the identity of the mitochondrial target. Mitochon-drial depolarization is followed later by loss of cytochrome c and Smac/Diablo, activation of caspase-9 and -3, and cell death. These data suggest that resveratrol causes cell death by activation of the intrinsic apoptosis pathway. In addition, we found activation of procaspase-8 in our cells. This caspase has been described as a component in chemical-induced apoptosis.18 It has been found to cleave Bid, which in turn leads to mitochondria-mediated apoptotic cell death. Therefore, resveratrol may act directly and indirectly on the mitochondria. Alternatively, caspase-8 activation may suggest that the extrinsic apoptosis pathway is also activated by resveratrol in uveal melanoma cells, as has been described in different tumor types.
In summary, the data presented herein suggest that resveratrol is effective at inhibiting uveal melanoma in animal models of the disease, despite its relatively low bioavailability after oral administration drug. In addition, we have shown that resveratrol has a more potent effect, leading to tumor cell death and tumor regression when local drug levels are increased, suggesting that strategies to increase bioavailability could enhance the antitumor action of the drug. Finally, the results of our in vitro studies suggest that tumor cell death occurs via a mitochondrial pathway.
Acknowledgments
The authors thank Joshua Harder for excellent technical assistance and June Kan-Mitchell (Ocm-1 and Ocm-3), Bruce Ksander (Mel290 and Mel270), Mary Hendrix (M619, C918, and Mum2b), and Martine Jager (92.1) for providing uveal melanoma cell lines.
Supported by National Cancer Institute Grant R01CA103653 (ASP) and grants from the Retina Research Foundation (ASP), the Mandelbaum Cancer Therapeutics Initiative (ASP, DMA), the American Institute for Cancer Research (PvG), and National Eye Institute Core Grant P30 EY016665-02.
Disclosure
P.R. van Ginkel, None; S.R. Darjatmoko, None; D. Sareen, None; L. Subramanian, None; S. Bhattacharya, None; M.J. Lindstrom, None; D.M. Albert, None; A.S. Polans, None
References
- 1.Collaborative Ocular Melanoma Study Group Assessment of metastatic disease status at death in 435 patients with large choroidal melanoma in the collaborative ocular melanoma study (COMS): COMS report no. 15. Arch Ophthalmol. 2001;119(5):670–676. doi: 10.1001/archopht.119.5.670. [DOI] [PubMed] [Google Scholar]
- 2.Pach JM, Robertson DM. Metastasis from untreated uveal melanomas. Arch Ophthalmol. 1986;104:1624–1625. doi: 10.1001/archopht.1986.01050230062032. [DOI] [PubMed] [Google Scholar]
- 3.Wagoner MD, Albert DM. The incidence of metastases from untreated ciliary body and choroidal melanoma. Arch Ophthalmol. 1982;100:939–940. doi: 10.1001/archopht.1982.01030030947009. [DOI] [PubMed] [Google Scholar]
- 4.Wang MX, Shields JA, Donoso LA. Subclinical metastasis of uveal melanoma. Int Ophthalmol Clin. 1993;33:119–127. doi: 10.1097/00004397-199303330-00017. [DOI] [PubMed] [Google Scholar]
- 5.Shields JA, Augsburger JJ, Donoso LA, Bernardino VB, Jr, Portenar M. Hepatic metastasis and orbital recurrence of uveal melanoma after 42 years. Am J Ophthalmol. 1985;100:666–668. doi: 10.1016/0002-9394(85)90621-x. [DOI] [PubMed] [Google Scholar]
- 6.Lorrigan JG, Wallace S, Mavligit GM. The prevalence and location of metastases from ocular melanoma: imaging study in 110 patients. Am J Radiol. 1991;157:279–281. doi: 10.2214/ajr.157.6.1950883. [DOI] [PubMed] [Google Scholar]
- 7.Aggarwal BB, Bhardwaj A, Aggarwal RS, Seeram NP, Shishodia S, Takada Y. Role of resveratrol in prevention and therapy of cancer: preclinical and clinical studies. Anticancer Res. 2004;24(5A):2783–2840. [PubMed] [Google Scholar]
- 8.Fulda S, Debatin KM. Resveratrol modulation of signal transduction in apoptosis and cell survival: a mini-review. Cancer Detect Prev. 2006;30(3):217–223. doi: 10.1016/j.cdp.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Tinhofer I, Bernhard D, Senfter M. Resveratrol, a tumorsuppressive compound from grapes, induces apoptosis via a novel mitochondrial pathway controlled by bcl-2. FASEB J. 2001;15(9):1613–1615. doi: 10.1096/fj.00-0675fje. [DOI] [PubMed] [Google Scholar]
- 10.Zini R, Morin C, Bertelli A, Bertelli AA, Tillement JP. Effects of resveratrol on the rat brain respiratory chain. Drugs Exp Clin Res. 1999;25(2–3):87–97. [PubMed] [Google Scholar]
- 11.Zheng J, Ramirez VD. Inhibition of mitochondrial proton F0F1- ATPase/ATP synthase by polyphenolic phytochemicals. Br J Pharmacol. 2000;130(5):1115–1123. doi: 10.1038/sj.bjp.0703397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma X, Tian X, Huang X, Yan F, Qiao D. Resveratrol-induced mitochondrial dysfunction and apoptosis are associated with ca(2+) and mCICR-mediated MPT activation in HepG2 cells. Mol Cell Biochem. 2007;302(1–2):99–109. doi: 10.1007/s11010-007-9431-8. [DOI] [PubMed] [Google Scholar]
- 13.Jiang X, Wang X. Cytochrome C-mediated apoptosis. Annu Rev Biochem. 2004;73:87–106. doi: 10.1146/annurev.biochem.73.011303.073706. [DOI] [PubMed] [Google Scholar]
- 14.van Ginkel PR, Sareen D, Subramanian L. Resveratrol inhibits tumor growth of human neuroblastoma and mediates apoptosis by directly targeting mitochondria. Clin Cancer Res. 2007;13(17):5162–5169. doi: 10.1158/1078-0432.CCR-07-0347. [DOI] [PubMed] [Google Scholar]
- 15.Sareen D, Darjatmoko SR, Albert DM, Polans AS. Mitochondria, calcium, and calpain are key mediators of resveratrol-induced apoptosis in breast cancer. Mol Pharmacol. 2007;72(6):1466–1475. doi: 10.1124/mol.107.039040. [DOI] [PubMed] [Google Scholar]
- 16.Sareen D, van Ginkel PR, Takach JC. Mitochondria as the primary target of resveratrol-induced apoptosis in human retinoblastoma cells. Invest Ophthalmol Vis Sci. 2006;47(9):3708–3716. doi: 10.1167/iovs.06-0119. [DOI] [PubMed] [Google Scholar]
- 17.Haneke K, Carson BL, Gregorio MA, Hardy R, Belue NS. trans-Resveratrol [501-36-0]: review of toxicological literature, Research Triangle Park, NC: Integrated Laboratory Systems; March 2002. Available at http://ntp.niehs.nih.gov/ntp/htdocs/chem_background/exsumpdf/resveratrol.pdf. Accessed September 26, 2005.
- 18.Anto RJ, Mukhopadhyay A, Denning K, Aggarwal BB. Curcumin (diferuloylmethane) induces apoptosis through activation of caspase-8, BID cleavage and cytochrome c release: its suppression by ectopic expression of bcl-2 and bcl-xl. Carcinogenesis. 2002;23(1):143–150. doi: 10.1093/carcin/23.1.143. [DOI] [PubMed] [Google Scholar]
- 19.Maniotis AJ, Folberg R, Hess A. Vascular channel formation by human melanoma cells in vivo and in vitro: vasculogenic mimicry. Am J Pathol. 1999;155(3):739–752. doi: 10.1016/S0002-9440(10)65173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maniotis AJ, Chen X, Garcia C, et al. Control of melanoma morphogenesis, endothelial survival, and perfusion by extracellular matrix. Lab Invest. 2002;82(8):1031–1043. doi: 10.1097/01.lab.0000024362.12721.67. [DOI] [PubMed] [Google Scholar]
- 21.Seftor EA, Meltzer PS, Kirschmann DA, et al. Molecular determinants of human uveal melanoma invasion and metastasis. Clin Exp Metastasis. 2002;19(3):233–246. doi: 10.1023/a:1015591624171. [DOI] [PubMed] [Google Scholar]
- 22.Asensi M, Medina I, Ortega A, et al. Inhibition of cancer growth by resveratrol is related to its low bioavailability. Free Radic Biol Med. 2002;33(3):387–398. doi: 10.1016/s0891-5849(02)00911-5. [DOI] [PubMed] [Google Scholar]
- 23.Hendrix MJC, Seftor EA, Seftor REB, et al. Biologic determinants of uveal melanoma metastatic phenotype: role of intermediate filaments as predictive markers. Lab Invest. 1998;78(2):153–163. [PubMed] [Google Scholar]
- 24.De Waard-Siebinga I, Blom D-R, Griffioen M, et al. Establishment and characterization of an uveal-melanoma cell line. Int J Cancer. 1995;62:155–161. doi: 10.1002/ijc.2910620208. [DOI] [PubMed] [Google Scholar]
- 25.Grimm S, Brdiczka D. The permeability transition pore in cell death. Apoptosis. 2007;12(5):841–855. doi: 10.1007/s10495-007-0747-3. [DOI] [PubMed] [Google Scholar]
- 26.Wieckowski MR, Wojtczak L. Fatty acid-induced uncoupling of oxidative phosphorylation is partly due to opening of the mitochondrial permeability transition pore. FEBS Lett. 1998;423(3):339–342. doi: 10.1016/s0014-5793(98)00118-5. [DOI] [PubMed] [Google Scholar]
- 27.Schild L, Keilhoff G, Augustin W, Reiser G, Striggow F. Distinct Ca2+ thresholds determine cytochrome c release or permeability transition pore opening in brain mitochondria. FASEB J. 2001;15(3):565–567. doi: 10.1096/fj.00-0551fje. [DOI] [PubMed] [Google Scholar]