Abstract
Background
The use of natural openings for abdominal surgery started at the beginning of the 21th century. A trans-Douglas endoscopic device has been designed to perform most of the intra-abdominal operations in women through the pouch of Douglas. The posterior vaginal vault is limited in size and could be damaged by an oversized instrument. This study investigates the optimal dimensions of the instrument by measuring the limiting factor in the passage.
Methods
In ten female embalmed bodies the transversal and sagittal diameter of the fornix posterior vaginalis was measured by two observers. The pouch of Douglas was filled to its maximal capacity with mouldable latex through an open abdomen. By internal vaginal examination the connective tissue borders of the fornix posterior were palpated and the impression in the cast was measured. The mean value of these two diameters was evaluated in this study. The level of agreement between the observers was calculated.
Results
The mean fornix posterior diameter was 2.6 cm (standard deviation, SD 0.5 cm) with a range of 2.0–3.4 cm. The mean difference between the two observers of all measurements was 0.08 cm (not significant). Both observers had an acceptable intraobserver variation. The interobserver agreement was excellent.
Conclusion
Instruments with dimensions within the measured limits can be used safely for intra-abdominal operations via the natural orifice of the vagina.
Keywords: Fornix vaginalis, Pouch of Douglas, Natural orifice surgery
The 19th century was the era of the laparotomy. Endoscopy was developed in the 20th century. The use of the natural openings for abdominal surgery started at the beginning of the 21st century. Instruments have been designed in order to perform most of the intra-abdominal operations in women through the pouch of Douglas. In order to find the optimal dimensions of this instrument, the limiting factor in the passage through the vagina into the abdominal cavity, the fornix vaginalis, has to be measured.
Anatomy
The fornix vaginalis is formed anatomically by the vagina around the cervix uteri. It is most spacious dorsally, where it is separated from the recto-uterine pouch of Douglas only by vaginal wall and peritoneum. The fornix to Douglas relation is not end-to-end. Douglas continues for a shorter or longer distance along the posterior vaginal wall [1, 2]. The background of this is that, in the embryological phase, Douglas’ pouch is deeper, reaching the perineum. It condensates later into the recto-vaginal septum as the cul de sac moves upward, just short of the full length of the posterior vaginal wall. The recto-vaginal septum then extends from the caudal margin of the recto-uterine peritoneal pouch to the proximal border of the perineal body. It forms a fixation point for the perineal body and stiffens the anterior rectal wall during defecation [1].
Surgical techniques
The posterior fornix of the vagina has been used as an entrance and as an exit to the pelvic and abdominal cavity in several surgical developments in the last 100 years [3, 4].
In the first half of the 20th century the fornix posterior was used as a passage for the 1.2-cm-diameter culdoscopes. In culdoscopy the pelvic organs were visualized without insufflation and with the patient in knee–elbow position. The technique was used to search for causes of pelvic pain and infertility, and for diagnosing adnexal masses [5].
Later this changed into transvaginal endoscopy with insufflation of the abdominal cavity with CO2 or fluid [6]. The fornix posterior here served as a gateway for a Veress needle–trocar system for insufflation as well as for access. The trocar had a diameter of 3.9 mm and the patient was lying on her back. Complications of the transvaginal route in culdoscopy and transvaginal endoscopy were damage to the surrounding tissues, mostly bleeding of the entry site, and puncture of the retroperitoneal rectum. These complications were rarely of a serious nature [7].
The posterior fornix can also serve as an exit for laparoscopically removed specimen like fibroids, gallbladder or fallopian tube that cannot be removed through the abdominal wall without extension of the abdominal incision.
Materials and methods
In ten embalmed female human bodies, that had not undergone any previous pelvic surgery, the transversal and sagittal diameter of the fornix posterior was measured. In case of obesity the vulva was removed in order to obtain better access.
The pouch of Douglas was filled to its maximal capacity with moldable latex through the open abdomen (Fig. 1). Glycerin was used to reduce the adhesiveness of the cast. By internal vaginal examination the connective tissue borders of the fornix posterior were palpated and an impression was made in the cast (Fig. 2). The imprint was measured in the transversal and sagittal direction with a marking gauge. Independently two observers conducted five separate measurements in each specimen. A coefficient of variation to assess the intraobserver variety was calculated. The mean values of the five measurements were used to calculate the intraclass correlation coefficient as a measure of interobserver agreement. A Bland and Altman plot, a statistical method to look for systematic bias, was used.
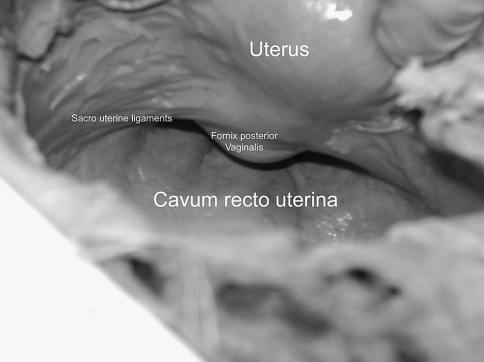
Fig. 1.
Posterior aspect of the uterus with protruding finger through the vagina and the posterior fornix into the pouch of Douglas
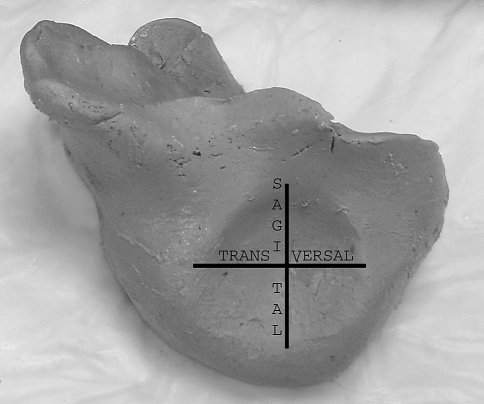
Fig. 2.
Impression of the fornix vaginalis in a Douglas pouch cast. The horizontal and vertical lines represent the transversal and sagittal measurement diameters
Results
The mean fornix posterior diameter in ten embalmed specimen was 2.6 cm (SD 0.5 cm) with a range of 2.0–3.4 cm.
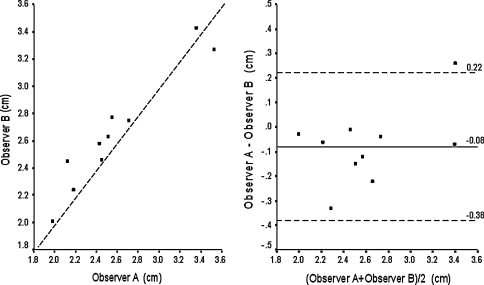
Both observers had an acceptable intraobserver variation with a mean coefficient of variation of 8.0% and 6.9%. These values did not differ significantly from each other (p = 0.85, Wilcoxon test). Comparing the two observers, the intraclass coefficient was 0.94 (Fig. 3, left panel). An intraclass coefficient of more than 0.9 is generally considered to represent excellent agreement.
Fig. 3.
Left panel: scatterplot of differences of both observers. The dotted line represents the line of identity. Right panel: Bland and Altman plot. The horizontal line represents the mean difference; the two dotted lines represent the limits of agreement (mean ± 2SD)
The mean difference between both observers in all measurements of 0.08 cm was not significant (p = 0.15, paired t-test). The Bland and Altman plot showed acceptable limits of agreement (Fig. 3, right panel).
Discussion
The full surgical potential of the vagina will be realized in the one-entry one-instrument principle of this kind of the natural orifice surgery [8]. The posterior fornix is the bottleneck of the entrance as the rest of the vagina and the pouch of Douglas is wider. The diameter measured gives an idea of the potential diameter of the instrument. The diameters in embalmed human bodies can be seen as minimal diameters. Rigor mortis and the effect of embalming have a significant influence upon these diameters. It is not improbable that in patients undergoing surgery the natural elasticity of the fibromuscular layers around the posterior vaginal vault will allow the introduction of wider instruments. Damage by an oversized instrument to the nearby proximal fixation point of the recto-vaginal fascia has a considerable clinical significance. If this attachment is avulsed and the fascia only fixated to the perineal body, the anterior rectal wall may bulge during straining for defecation, resulting in functional disturbances of bowel movement with possible chronic retention of faeces.
Acknowledgement
The authors thank Dr. P. C. Struijk for assistance with the statistical analysis.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Nichols D. Vaginal surgery. London: Williams & Wilkins; 1983. [Google Scholar]
- 2.Baessler K, Schuessler B. Anatomy of the sigmoid colon, rectum, and the rectovaginal pouch in women with enterocele and anterior rectal wall procidentia. Clin Anat. 2006;19(2):125–129. doi: 10.1002/ca.20232. [DOI] [PubMed] [Google Scholar]
- 3.McGowan L. Incidental appendectomy during vaginal surgery. Am J Obstet Gynecol. 1966;95(4):588. doi: 10.1016/0002-9378(66)90157-8. [DOI] [PubMed] [Google Scholar]
- 4.Delvaux G, De Waele B, Willems G. Transvaginal removal of gallbladders with large stones after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1993;3(4):307–309. [PubMed] [Google Scholar]
- 5.Lane E. Culdoscopy—useful or useless. Int J Gynaecol Obstet. 1980;17(4):372–374. doi: 10.1002/j.1879-3479.1980.tb00303.x. [DOI] [PubMed] [Google Scholar]
- 6.Brosens I, Campo R, Puttemans P, Gordts S. Transvaginal laparoscopy. Clin Obstet Gynecol. 2003;46(1):117–122. doi: 10.1097/00003081-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Gordts S, Watrelot A, Campo R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76(6):1238–1241. doi: 10.1016/S0015-0282(01)02887-4. [DOI] [PubMed] [Google Scholar]
- 8.Benhidjeb T, Witzel K, Barlehner E, Stark M. The natural orifice surgery concept. Chirurg. 2007;78(6):537–542. doi: 10.1007/s00104-007-1346-0. [DOI] [PubMed] [Google Scholar]