Summary
OBJECTIVE
To determine the cost of rotavirus and all-cause diarrhoea in Vellore, India.
METHODS
Parents of children <5 years of age accessing clinics, emergency rooms, or hospitals for acute diarrhoea completed a questionnaire detailing healthcare utilisation, medical and non-medical expenditures, and lost income. Faecal samples were screened for rotavirus and medical records were examined. Costs were estimated for inpatient and outpatient resource consumption, stratified by facility.
RESULTS
Total societal costs of a hospitalised diarrhoeal episode were Rs 3278.50 (US$ 80.80) at a large referral hospital and Rs 1648.60 (US$ 40.60) at a smaller community hospital. Costs for rotavirus positive or negative gastroenteritis were similar. Median household expenditures per diarrhoeal episode at the referral and the community hospitals equalled 5.8% and 2.2% of the annual household income, respectively.
CONCLUSIONS
Diarrhoeal disease in children constitutes a considerable economic burden. An appropriately priced and effective rotavirus vaccine may provide significant economic savings for the Indian household and healthcare system.
Keywords: rotavirus, vaccine, cost, India, health economics, diarrhoea, paediatrics
Introduction
As the leading cause of severe acute gastroenteritis in children worldwide, rotavirus is responsible for more than 600 000 deaths, 2 million hospitalisations and 25 million outpatient visits annually (Parashar et al. 2003, 2006). It was estimated in 1998 that approximately 100 000 of those deaths occurred in India alone, a number that has likely increased in the past decade given the increasing incidence of rotavirus hospitalisations (Jain et al. 2000). Unlike bacterial gastroenteritis, improved water quality, hygiene and sanitation do not significantly reduce the burden of rotavirus infection (Bresee et al. 1999). Therefore, immunisation may offer the best hope for reducing morbidity and mortality associated with rotavirus diarrhoea.
Two rotavirus vaccines were recently introduced into the global market (Ruiz-Palacios et al. 2006; Vesikari et al. 2006). In clinical trials, these vaccines demonstrated 74–85% efficacy against any rotavirus gastroenteritis and up to 100% efficacy against the most severe forms of disease. The vaccines reduced rotavirus-associated hospitalisation by 86–94.5% and diarrhoeal hospitalisations of any cause by 42–59% (Ruiz-Palacios et al. 2006; Vesikari et al. 2006). However, when deciding whether to incorporate a rotavirus vaccine into national immunization programs, governments must consider the economic burden of disease and the cost-effectiveness of a vaccine as well as the expected health benefits.
Ongoing surveillance in Vellore, India, has detected rotavirus in 7.1% of community episodes of acute diarrhoea and approximately 40.0% of hospitalisations for acute gastroenteritis in the past year (G. Kang, unpublished data); a previously reported rate in hospitalised children was 27.1% (Banerjee et al. 2006). These data suggest that rotavirus is responsible for a significant proportion of diarrhoeal disease in India and its associated costs. In order to consider the cost-effectiveness of a rotavirus vaccine, the baseline cost of rotavirus disease to the healthcare system and society must be established. Costing studies of rota-virus have been previously conducted in other countries in Asia, Europe, and America, but their outcomes may not be applicable to India because of the diversity of healthcare systems and economies (Zimmerman et al. 2001; Fischer et al. 2005; Nelson et al. 2005; Podewils et al. 2005; Lu et al. 2006; Giaquinto et al. 2007; Isakbaeva et al. 2007). No country-specific economic analysis of rotavirus is currently available for India. The purpose of this study was to estimate the economic burden of all cause and rotavirus-associated paediatric diarrhoea in India using Vellore as a model.
Methods
The study is based on the World Health Organization (WHO) generic protocol for estimating the economic burden of diarrhoeal disease with a focus on assessing the cost of rotavirus-associated diarrhoea (WHO 2005). $1 (US) is equivalent to Rs 40.6 (India).
Study population
Study site
Healthcare costs were gathered from a convenience sample of three healthcare facilities located in Vellore, India. The first, Christian Medical College (CMC), is a 2200-bed, not-for-profit, urban referral hospital that provides discounted or free care to about 30% of its patients, while the remainder receive fee-for-service care. The second, CMC's Community Health and Development Hospital (CHAD), is a 100-bed, not-for-profit community hospital that provides discounted care for a rural population of approximately 100 000 residents of 78 villages. The Kasba Urban Health Center (UHC), the final site, serves an urban slum population of approximately 40 000, who are provided free outpatient care supported by the government healthcare system. Patients were recruited from inpatient paediatric wards, outpatient clinics and emergency rooms.
Inclusion criteria
Children who were <5 years of age and resident in Vellore and presented to the outpatient clinic or emergency room with a complaint of loose stool or who were hospitalised for a primary diagnosis of acute diarrhoea were eligible to participate.
Laboratory methods
All faecal samples collected from the community and hospital were processed immediately after collection for the detection of rotavirus by enzyme-linked immunosorbent assays as described by Banerjee et al. (2006).
Healthcare costs of rotavirus-associated and all-cause diarrhoea
Patient enrolment
Patients were recruited prospectively from CMC, CHAD and the UHC for a period of 12 months at each facility, from November 2005 to December 2006. Field workers screened all clinic inpatients, outpatients and new admissions daily for their chief complaint and primary diagnosis, recruiting eligible patients whose parents gave written informed consent. Emergency room recruitment was conducted by home visits to patients who had been treated and discharged during the previous week. Informed consent was obtained from the parents of all enrolled children, and the study was approved by the Research Committee of CMC.
At recruitment, parents completed a questionnaire detailing patient demographics and the cost of all expenses incurred since the start of the diarrhoeal episode – including prior healthcare visits, transportation, food, hotels and missed work days. Ten to fourteen days after the initial survey, all parents were telephoned or visited at home if there were no telephone available. During the follow-up interview, the end of the diarrhoeal episode and all related additional expenses were recorded. Patients were phoned twice and visited once before they were considered lost to follow-up.
Medical direct costs to the healthcare system
For all patients from CMC, medical and pharmacy bills, as well as medical charts, were reviewed in order to document all visits, medications and diagnostic tests associated with the diarrhoeal episode. At CHAD, only medical charts were reviewed for the same purpose, because of a lack of computerised billing. At the UHC field workers recorded all medications given by the physician at recruitment, because no charts are maintained. Information on medications and visits related to the diarrhoeal episode prior to or after the initial questionnaire was collected based on patient recall during follow-up interviews.
Unit costs were calculated for medications and diagnostics associated with the episodes, as well as for hospital bed-days, outpatient clinic visits and emergency room visits at each facility as appropriate. Medications were assigned wholesale drug costs per unit, based on CMC's purchasing prices, while the accounting departments at CMC and CHAD provided pre-calculated costs for each diagnostic test. The cost of rotavirus diagnostic testing was not included, because it was conducted only for the purpose of the study. No diagnostic tests are ordered at the UHC. The total medication and diagnostic costs to the healthcare system equalled the sum of the individual unit costs times the quantity of medication and diagnostic tests ordered, respectively.
Visit and bed-day costing included personnel salaries, electricity, linens, water supplies, building and equipment depreciation, maintenance and medical record expenses incurred by the healthcare facility, with inpatient expenses calculated at an 80% occupancy rate. The total visit cost to the healthcare system equalled the sum of the individual unit cost per visit or bed-day multiplied by the total number of visits or days admitted, respectively. Follow-up visits to confirm that the child's health had returned to normal after discharge and the actual charge of any prior or subsequent private practitioner visits were included in the total visit cost.
Medical direct costs to the healthcare system equalled the sum of all medication, diagnostic and visit costs.
Medical direct costs to the patient
Actual charges to each patient for all medications, diagnostic tests and visits associated with the diarrhoeal episode were recorded from reviews of medical bills and charts. Patient-reported costs of outside private practitioner visits were included. Medical direct costs to the patient equalled the sum of all visit, medication, and diagnostic costs. All visits and medications at the UHC are free to the patient and were therefore not included.
Direct non-medical and indirect costs
The direct non-medical costs equalled the sum of all transportation, food and hotel expenses incurred during the diarrhoeal episode. The indirect costs of the diarrhoeal episode per household equalled the sum of each worker's estimated daily salary multiplied by lost work days.
Data analysis
Data were analyzed with SPSS v12.0. Data were stratified by facility type, because CMC, CHAD and the UHC each serve different populations. Because the data were skewed, differences in medians were calculated using Mann–Whitney U and Kruskal–Wallis H tests. Data are presented as median values (inter-quartile range, IQR).
Results
Enrolment of study participants
A total of 439 patients were enrolled in this study – 283 from CMC, 54 from CHAD, and 102 from the UHC outpatient clinic (Table 1). Participants included 188 outpatient clinic cases, 119 emergency room cases, and 132 hospitalisations. At outpatient clinics, 188 of 202 (93.1%) eligible patients were recruited. For emergency room cases, where addresses were frequently incomplete, the homes of 90 of 289 (31.1%) potential cases were located, all of whom participated in the study (100% enrolment rate). The family of only one hospitalised child declined to participate, but 35 patients were discharged before the field worker visited the ward. Therefore, of the eligible hospitalised children, 133 of 167 (79.6%) were located and 132 of 133 (99.2%) were recruited. The follow-up rate, 10–14 days after the initial survey, was 90.7% (398/439) for all cases.
Table 1.
Baseline demographic and costing data for three healthcare facilities in Vellore, South India
| CMC | CHAD | UHC | |
|---|---|---|---|
| Number of patients surveyed | |||
| Outpatient clinic | 79 | 7 | 102 |
| Emergency room | 90 | 29 | |
| Hospitalisation | 114 | 18 | |
| Total | 283 | 54 | 102 |
| Sex (n %) | |||
| Male | 162 (57.2%) | 33 (61.1%) | 56 (54.9%) |
| Female | 121 (42.8%) | 21 (38.9%) | 46 (45.1%) |
| Age (months) | |||
| Median (IQ1, IQ3) | 11 (7, 17) | 11 (7.8, 14) | 12 (6, 24) |
| Mother's education (n %) | |||
| None | 12 (4.2%) | 1 (1.9%) | 25 (24.5%) |
| Primary school | 26 (9.2%) | 14 (25.9%) | 50 (49.0%) |
| Secondary school | 142 (50.2%) | 34 (63.0%) | 24 (23.5%) |
| University/college | 103 (36.4%) | 5 (9.3%) | 3 (2.9%) |
| Annual household income (Rs) | |||
| Median (IQ1, IQ3) | 48 000 (24 000, 1 14 000) | 31 800 (24 000, 55 440) | 38 400 (30 000, 58 050) |
| Cost to healthcare system | |||
| Inpatient cost per bed-day (Rs) | Ward = 628 PICU = 1355 |
443 | |
| Emergency room cost per visit (Rs) | 264 | 58 | |
| Outpatient cost per visit (Rs) | 53 | 61 | 27 |
| Charge to patient | |||
| Inpatient cost per bed-day (Rs) | Ward = 470† PICU = 1040† |
40 | |
| Emergency room cost per visit (Rs) | Visit = 150 Admit = 285‡ |
35 | |
| Outpatient cost per visit (Rs) | 45 | 25 | 0 |
CMC, Christian Medical College; CHAD, Community Health and Development Hospital; UHC, Urban Health Centre.
The patient is also charged a one-time Rs 275 registration fee for each hospitalisation.
Emergency room admit = patient stayed for observation but was not admitted to the ward.
Case description and baseline costing data
Patient's age, sex, median household income and maternal education are shown in Table 1. The calculated unit cost per visit or bed-day to the healthcare system and the actual patient charges per visit are also shown. Duration of illness, visits to other private healthcare facilities and the total number of healthcare visits per episode are reported in Table 2. Patients with a documented second diagnosis were not excluded, although 83.4% of participants had a single diagnosis of acute gastroenteritis. An additional diagnosis was made for 16.6% of participants (Table 2), and included both acute and chronic conditions. The most common second diagnoses were upper and lower respiratory tract infections (31.5% and 24.6%, respectively).
Table 2.
Gastrointestinal illness and visits at each healthcare facility
| CMC | CHAD | UHC | Total | |
|---|---|---|---|---|
| Number of diagnoses | ||||
| Diarrhoea only | 220 (77.7%) | 44 (81.5%) | 102 (100%)† | 366 (83.4%) |
| Diarrhoea and other diagnosis | 63 (22.3%) | 10 (18.5%) | 0 | 73 (16.6%) |
| Duration of illness (days)‡ | ||||
| Median (IQR) | 6 (4, 14) | 3 (1, 6) | 6 (4, 11) | 6 (3, 12) |
| Vesikari score (mean + SD)§ | ||||
| Inpatient | 10.6 ± 2.9 | 10.6 ± 2.4 | Data not available | |
| Emergency room visit | 6.4 ± 2.9 | 5.7 ± 2.2 | ||
| Outpatient visit | 6.1 ± 2.4 | 8.1 ± 3.4 | ||
| Additional private clinic visit during episode?¶ | ||||
| Yes | 127 (44.9%) | 15 (27.8%) | 29 (28.4%) | 171 (39%) |
| No | 156 (55.1%) | 39 (72.2%) | 73 (71.6%) | 268 (61%) |
| Mean (SD) visits | 0.7 (1.0) | 0.3 (0.5) | 0.3 (0.6) | 0.5 (0.9) |
| Median (IQ1, IQ3) number of visits/episode | ||||
| Hospitalisations | ||||
| Inpatient (range in days) | 2 (1.75, 4) | 3 (1, 3) | ||
| Emergency room (IQR) visits | 1 (1, 2) | 1 (1, 1) | ||
| Outpatient clinic (IQR) visit | 2 (1, 3) | 1 (0, 2) | ||
| Emergency room | ||||
| Emergency room (IQR) visit | 1 (1, 2) | 1 (1, 1) | ||
| Outpatient clinic (IQR) visit | 1 (0, 2) | 0 (0, 0.5) | ||
| Outpatient clinic | ||||
| Outpatient clinic (IQR) visit | 2 (1, 2) | 1 (1, 2) | 1 (1, 2) | |
CMC, Christian Medical College; CHAD, Community Health and Development Hospital; UHC, Urban Health Centre; IQR, inter-quartile range.
UHC had no charts for documentation of a second diagnosis.
Patient reported.
Data from 263 children (78%) seen at CMC or CHAD.
A visit to a private clinic not associated with CMC, CHAD, or the UHC.
Cost per episode to the patient
Direct costs incurred by patients were over four times greater at CMC than at CHAD for both hospitalisations (Rs 2773.8 vs. Rs 663.7, P < 0.001) and emergency room visits (Rs 497.8 vs. Rs 116.9, P < 0.001) (Table 3). For outpatient visits, direct costs at CMC were almost 1.5 times greater than at CHAD, although the difference was not significant (Rs 152.9 vs. Rs 109.1, P = 0.068). Patients incurred no direct costs when accessing the government healthcare system (Table 3).
Table 3.
Median and inter-quartile range of cost in Indian rupees to the patient per diarrhoeal episode
| Hospitalisations |
Emergency room |
Outpatient clinic |
|||||
|---|---|---|---|---|---|---|---|
| CMC (n = 114) | CHAD (n = 18) | CMC (n = 90) | CHAD (n = 29) | CMC (n = 79) | CHAD (n = 7) | UHC (n = 102) | |
| Non-medical direct costs† | 40 (13.9, 82.5) | 39.5 (19.8, 124.8) | 62.5 (28.5, 120) | 16 (8, 63) | 12.8 (4.8, 40) | 21 (0, 46.3) | 0 (0, 16) |
| Private visit cost‡ | 20 (0, 88.5) | 0 (0, 41.3) | 0 (0, 130) | 0 (0, 38.5) | 0 (0, 50) | 0 (0, 75) | 0 (0, 46.3) |
| Medical direct costs§ | 2745.3 (1944.9, 4210.1) | 537.9 (393.9, 745.4) | 384.8 (223.1, 806.3) | 77.8 (56.9, 152.3) | 133.4 (82.1, 195.4) | 75.5 (46.9, 126.9) | 0 (0, 46.3) |
| Total direct costs¶ | 2773.8 (1985.2, 4257.7) | 663.7 (426.7, 824.0) | 497.8 (281.7, 917.4) | 116.9 (77.0, 158.3) | 152.9 (104, 234.4) | 109.1 (46.9, 137.9) | 1.0 (0, 71.3) |
| Annual income | 51 000 (24 000, 1 20 000) | 26 700 (17 100, 49 680) | 66 000 (48 000, 1 21 500) | 36 000 (24 960, 77 400) | 24 000 (15 360, 48 000) | 28 800 (24 000, 36 000) | 38 400 (30 000, 58 050) |
| % of annual income†† | 5.8 (2.1, 12.9) | 2.2 (0.9, 4.8) | 0.6 (0.3, 1.6) | 0.3 (0.1, 0.6) | 0.6 (0.3, 1.1) | 0.4 (0.2, 0.5) | 0 (0, 0.2) |
CMC, Christian Medical College; CHAD, Community Health and Development Hospital; UHC, Urban Health Centre.
Non-Medical direct cost = cost of transportation + food + hotel.
Private visit cost = out-of-pocket expenses incurred at an additional private clinic visit not associated with CMC, CHAD, or UHC.
Medical direct costs = private visit cost + visit cost + medication cost + diagnostic cost.
Total direct costs = direct medical + direct non-medical costs.
% Annual income = total direct costs/(annual household income) × 100.
Financial impact of a diarrhoeal episode on the household
Amongst CMC and CHAD hospitalisation cases, the median household spent 5.8% (2.1, 12.9) and 2.2% (0.9, 4.8), respectively, of its annual income treating the diarrhoeal episode (Table 3). While the total direct costs to the patient of a CMC hospitalisation were 4.2 times greater than those at CHAD, the median percentage of annual income spent in treating a CMC hospitalisation was only 2.6 times greater than the corresponding percentage at CHAD because of the higher household income of CMC patients. Households at both CMC and CHAD spent about half a per cent of their annual income (0.3–0.6%) treating outpatient or emergency room cases.
When asked about the cost of the diarrhoeal treatment, 37.7% of CMC and CHAD mothers (110/292) stated that it was difficult to pay for their child's treatment, while 41.5% (120/289) reported borrowing money. Mothers who reported borrowing money spent 1.6% (0.6, 8.8) of their annual income paying for the treatment, a significantly larger percentage of annual income than the 0.7% (0.3, 2.1) spent by those who used savings to pay for the treatment (P < 0.001). The median annual income of households which borrowed money to pay for the diarrhoeal episodes was Rs 24 000 (15 540, 36 000), significantly less than the median Rs 72 000 (48 000, 144 000) annual income of households who paid for the treatment with savings (P < 0.001). More than 80% of households with an annual income of less than Rs 36 000 reported borrowing money to pay for treatment (Figure 1). Borrowing dropped drastically in households earning more than Rs 36 000: only 35.7% of households in the Rs 36–48 000 income category borrowed money.
Figure 1.
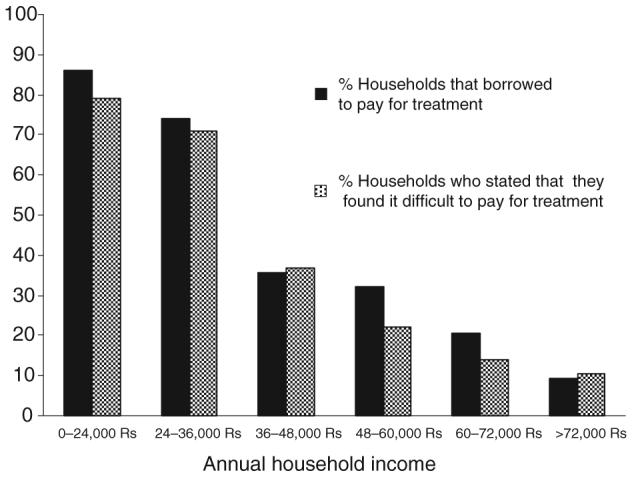
Financial burden of treatment of diarrhoea: percentage of households borrowing money to pay for a diarrhoeal hospitalisation stratified by annual income.
Cost per episode to the healthcare system
Median costs per diarrhoeal episode to the healthcare system are reported in Table 4. The median total direct costs of a CMC hospitalisation were nearly twice those at CHAD (Rs 3056.9 vs. Rs 1648.6, P < 0.001). At CMC, visit costs comprised 59%, diagnostic costs 25%, and medication costs 9% of the total direct costs per hospitalised episode, while at CHAD, the corresponding costs were 81%, 0%, 12%, respectively.
Table 4.
Median and inter-quartile range of cost in Indian rupees per diarrhoeal episode to the healthcare system and society
| Hospitalisations |
Emergency room |
Outpatient clinic |
|||||
|---|---|---|---|---|---|---|---|
| CMC (n = 114) | CHAD (n = 18) | CMC (n = 90) | CHAD (n = 29) | CMC (n = 79) | CHAD (n = 7) | UHC (n = 102) | |
| Non-medical direct costs1 | 40 (13.9, 82.5) | 39.5 (19.8, 124.8) | 62.5 (28.5, 120) | 16 (8, 63) | 12.8 (4.8, 40) | 21 (0, 46.3) | 0 (0, 16) |
| Private visit cost2 | 20 (0, 88.5) | 0 (0, 41.3) | 0 (0, 130) | 0 (0, 38.5) | 0 (0, 50) | 0 (0, 75) | 0 (0, 46.3) |
| Visit cost | 1804.6 (1299.9, 2914.2) | 1342 (547, 1372.3) | 317 (264, 528) | 58 (58, 58) | 53 (53, 53) | 61 (61, 61) | 26.5 (26.5, 26.5) |
| Medication cost | 288.9 (186.7, 419.8) | 203.8 (139.9, 308.5) | 57.6 (23.7, 137.3) | 31.0 (14.2, 40.7) | 33.5 (18, 58.7) | 23.7 (9, 40.0) | 17.6 (13.1, 29.9) |
| Diagnostic cost | 790 (248.8, 1282.5) | 0 (0, 81) | 45 (0, 290) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Medical direct costs3 | 3036.2 (2093.1, 4728.6) | 1576.6 (1054.1, 1781.9) | 612.0 (365.0, 1022.8) | 98.0 (76, 182.8) | 137.0 (84.9, 243.9) | 109.7 (79, 150) | 59.9 (41.3, 98.0) |
| Health care subsidy4 | 68.3 (−147.4, 630.3) | 956.4 (518.5, 1162.3) | 113.5 (97.8, 244.2) | 21.1 (19.1, 30.9) | 4.1 (−11.7, 8.0) | 32.1 (29.0, 34.1) | 45.4 (39.7, 59.7) |
| Total direct costs5 | 3056.9 (2102.9, 4889.5) | 1648.6 (1117.5, 1905.6) | 696.5 (411.6, 1132.5) | 149.0 (97.5, 190.3) | 159.1 (107.1, 256.7) | 142.0 (80.8, 161) | 63.6 (42.3, 121.7) |
| Indirect costs (lost wages) | 0 (0, 7.2) | 0 (0, 69.8) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 76.9 (0, 200) | 0 (0, 0) |
| Societal cost6 | 3278.5 (2272.8, 5072.3) | 1648.6 (1130.7, 2050.4) | 760.3 (417.6, 1132.5) | 167 (103.4, 216.3) | 164.8 (108.2, 293.6) | 253.5 (130.7, 342.4) | 66.8 (42.4, 121.7) |
| Societal cost in US $ (Rs 40.6: 1$) | 80.8 | 40.6 | 18.7 | 4.1 | 4.1 | 6.2 | 1.6 |
CMC, Christian Medical College; CHAD, Community Health and Development Hospital; UHC, Urban Health Centre.
Non-medical direct cost = cost of transportation + food + hotel.
Private visit cost = out-of-pocket expenses incurred at an additional private clinic visit not associated with CMC, CHAD, or UHC.
Medical direct costs = private visit cost + visit cost + medication cost + diagnostic cost.
Healthcare system subsidy = medical direct cost to healthcare system – medical direct cost to patient.
Total direct costs = direct medical + direct non-medical costs.
Societal cost = indirect cost + total direct costs.
The median direct costs to the healthcare system of a diarrhoeal episode that resulted in an emergency room visit at CMC were over four times those at CHAD (Rs 696.5 vs. Rs 149.0, P < 0.001). Difference in CMC and CHAD visit costs (Rs 317 vs. Rs 58, P < 0.001) and diagnostics costs (Rs 45 vs. Rs 0, P < 0.001) were major contributors to the higher cost at CMC. In contrast, the median direct costs for an outpatient episode at CMC and CHAD were nearly equal (Rs 159.1 vs. Rs 142.0, P = 0.364), while the UHC was over 50% less (Rs 63.6, P < 0.001).
In all the cases, patients paid less than the total direct medical cost of treatment provided by the healthcare facility (Table 4). At CMC, the hospital paid less than 5% of direct medical costs for the median hospitalised and outpatient diarrhoeal episode, but nearly 20% of the cost of the median emergency room episode. CHAD subsidised a large part of patient care by paying approximately 60% of hospitalisation, 20% of emergency room, and 30% of outpatient direct medical costs for the median episode. The UHC subsidised more than 75% of the direct medical costs for an outpatient episode.
Non-medical direct and indirect costs
Non-medical direct costs made up less than 3% of the total direct cost for hospitalisations at both facilities and up to 14% of total direct costs for outpatient and emergency room cases (Table 4). There were no indirect costs because of time lost from work for the majority of cases (Table 4), because most households had single incomes.
Rotavirus-positive vs. rotavirus-negative hospitalisations
Faecal samples were obtained from 62% of the CMC hospitalisation cases (71/114) and 67% of the hospitalisation cases at CHAD (12/18). At CMC, 47% of samples (34/71) were rotavirus-positive, while at CHAD, 41.7% of samples (5/12) tested positively for rotavirus (Table 5).
Table 5.
Median and inter-quartile range of medical direct cost in Indian rupees of rotavirus positive and rotavirus negative hospitalisations
| CMC hospitalisations |
CHAD hospitalisations |
|||||
|---|---|---|---|---|---|---|
| RV+ (n = 34) | RV− (n = 37) | P-value | RV+ (n = 5) | RV− (n = 7) | P-value | |
| Length of stay (days) | 2 (2, 4) | 2 (2, 4) | 0.717 | 3 (1.5, 3) | 3 (2, 4) | 0.432 |
| Visit cost | 1576.6 (1468.1, 3095.6) | 2110.6 (1575.6, 3417.6) | 0.489 | 1133.4 (729.0, 1433.5) | 1342.0 (1033.0, 1770.0) | 0.530 |
| Medication cost† | 211.3 (154.6, 403.1) | 320.8 (267.6, 441.7) | 0.021 | 0 (0, 61.5) | 0 (0, 175) | 0.268 |
| Diagnostic cost‡ | 425.0 (180.0, 1070.0) | 1040.0 (342.5, 1630.0) | 0.024 | 193.1 (105.3, 283.7) | 255.4 (190.5, 303.4) | 0.639 |
| Medical direct costs | 3128.0 (1899.6, 4224.1) | 3420.3 (2616.9, 5467.9) | 0.164 | 1529.4 (918.9, 1756.2) | 1651.5 (1502.7, 2159.5) | 0.202 |
CMC, Christian Medical College; CHAD, Community Health and Development Hospital; UHC, Urban Health Centre; RV, rotavirus.
Costs calculated from the healthcare system perspective.
Cost of Rotavirus testing not included in diagnostic cost.
The difference between the median medical direct costs of CMC's rotavirus-positive vs. rotavirus-negative cases was not significant (Rs 3128.0 vs. Rs 3420.3, P = 0.164, Table 5). The length of stays did not significantly differ (P = 0.717), nor did the visit costs (P = 0.489). However, rotavirus-negative episodes had significantly higher medication and diagnostic costs (P = 0.021 and 0.024, respectively). Amongst CHAD hospitalisations, median medical direct costs for rotavirus-positive vs. rotavirus-negative hospitalisations did not differ significantly (Rs 1529.4 vs. Rs 1651.5, P = 0.202), nor did the visit, medication or diagnostic costs.
Discussion
The costs per episode of all-cause and rotavirus-associated diarrhoea were examined from the perspectives of both the patient and the healthcare system in order to estimate the economic burden of all-cause and rotavirus diarrhoea in Vellore, India. Data were collected from three types of facilities – a tertiary care centre, a community hospital and a government clinic – under the premise that these facilities serve different populations and would incur different costs. The patterns of illness were similar to earlier reports, with the mean (±SD) of inpatients at CMC and CHAD 10.6 + 2.9 and 10.6 + 2.4, respectively, in this study, compared with 11 + 2.5 (Table 3, Banerjee et al. 2006). The severity of diarrhoeal episodes by Vesikari score (mean + SD) presenting to the outpatient clinic (CMC 6.1 + 2.4, CHAD 8.1 + 3.4) and the emergency rooms (CMC 6.4 + 2.9, CHAD 5.7 + 2.2) was similar to community-based data (7.6 + 3.4) from the same area (Banerjee et al. 2006). Income was higher among patients accessing healthcare at CMC than those who sought care at CHAD or UHC (Table 1).
Although direct costs incurred by patient at CMC were higher, both CMC and CHAD patients used a striking percentage of their annual household income to treat just one hospitalisation because of diarrhoea, 5.8% at CMC and 2.2% at CHAD. These data indicate that the treatment of diarrhoea places a large financial burden on Indian households, as an estimated 80% of Indian healthcare expenditures are met out-of-pocket by individuals and families (WHO 2007).
The economic burden of diarrhoeal treatment was confirmed by mothers, particularly those with lower household incomes who borrowed money to pay for the treatment. Borrowing was reported when household income was a median of Rs 24 000 per year ($591) or diarrhoeal treatment costs were a median of 1.6% of annual income.
Although outpatient costs at CHAD and CMC were similar, inpatient and emergency room costs at CMC were higher, mainly because of the inclusion of laboratory testing and inherently higher facility costs. Outpatient costs at the UHC were lower than CMC and CHAD because of lower facility costs. These differences in costs indicate that use of a higher level facility results in greater costs to the healthcare system. At all levels of the healthcare system, however, children received at least partially subsidised treatment. The subsidies were greatest at CHAD and the UHC, suggesting that although lower-level facilities provide less-expensive care, they must pay a larger portion of the care themselves because they are accessed by populations that find it difficult to pay for even low-cost treatment. At CMC, the highest level of healthcare and most expensive facility, nearly 45% of patients accessed an additional healthcare facility prior to admission (Table 2), most often a private medical practitioner. This may reflect severity of illness, which could not be managed outside a hospital and would require referral from the private practitioner.
Comparisons of rotavirus-positive and rotavirus-negative hospitalisation showed no difference in total direct medical costs, suggesting that any severe diarrhoeal episode requiring hospitalisation would be managed similarly and therefore result in comparable costs. Although an individual episode of rotavirus diarrhoea is not more expensive than other causes of diarrhoea, because rotavirus accounts for nearly 40% of diarrhoeal hospitalisations, it is likely that its total cost to society is significant. A rotavirus vaccine could therefore potentially result in significant savings to the Indian healthcare system depending on the cost of the vaccine. Furthermore, as poorer families pay a greater percentage of their income to treat diarrhoea, a vaccine could provide greater economic relief to poorer families while equally benefiting the health of all children.
Two previous studies have examined the cost of rotavirus in developing Asian countries (Fischer et al. 2005; Isakbaeva et al. 2007). Although these and our studies used the WHO generic diarrhoeal costing protocol (WHO 2005), our study examined a significantly larger group, analyzed the medical records of each patient and conducted follow-up interviews to ascertain whether additional treatment was obtained after hospital discharge. In Vietnam, Fischer et al. (2005) reported that the societal cost of a rotavirus hospitalisation ranged between $31.00 and $36.16, while in Uzbekistan, Isakbaeva et al. (2007) estimated the societal cost per hospitalised rotavirus episode to be $77.8 ± 13.5. The range of estimates in our study (societal costs of 40.6 US$ at CHAD to 80.8 US$ at CMC) points to the stratified nature of the Indian healthcare system, where costs cannot be adequately represented by data from a single type of facility or another developing country.
There are some limitations to this study. First, the data were collected in Tamil Nadu, a state which has a relatively high healthcare profile therefore may not be generalised to the whole country. However, it must be pointed out that data from states with less well-developed infrastructure can be difficult to collect, and also may not be generalised to all of India. Second, although our costing studies are more detailed than required by the WHO recommendations, we used a convenient sample of healthcare facilities in Vellore. Healthcare costs in corporate hospitals and some private practices in India, particularly in larger cities, are likely to be higher. It is also possible that we overestimated the cost of a diarrhoeal episode by not excluding cases with a second diagnosis. However, only 16% of all cases had a second diagnosis; the most common was upper respiratory tract infection, known to be associated with diarrhoeal diseases, particularly those of viral origin.
There is a critical need to estimate the potential cost-effectiveness of a rotavirus vaccine using local Indian data, so that appropriate decisions can be made regarding the incorporation of a vaccine into state immunisation strategies. When estimating the cost effectiveness of the vaccine, it would be expected that herd immunity would play a role in preventing rotavirus diarrhoea, but our recent report of a lack of protection from natural infection with G10 rotaviruses (Banerjee et al. 2007) raises questions about potential differences in protective efficacy of vaccines in this setting. However, it is also possible that immunity to G10 rotaviruses is different from the immunity induced by the vaccine strains, because G10P[11] is a neonatal infection, and the currently available vaccines do not include neonatal strains. We next plan to extrapolate estimates of the cost-effectiveness of a rotavirus vaccine in India from these and other community-based data on rotavirus infection in India.
In conclusion, we found that the costs resulting from diarrhoea were substantial, posing a high economic burden for both the individual family as well as society. Costs were highest when the diarrhoeal episode resulted in hospitalisation, but there was little difference in rotavirus positive and negative episodes of diarrhoea. Nevertheless, because of the high burden of rotavirus infection, an affordably priced rotavirus vaccine may result in cost savings in India and positively impact the ability of the Indian family to manage personal healthcare costs.
Acknowledgements
This research was supported by the Fogarty International Clinical Research Scholars Program, 2005 Overseas Fellowship in Global Health and Clinical Research and Wellcome Trust Grant No. 063144. These data were presented at the Annual Meeting of the American Public Health Association, 5 November 2007, Washington, DC.
References
- Banerjee I, Ramani S, Primrose B, et al. Comparative study of the epidemiology of rotavirus in children from a community-based cohort and a hospital in South India. Journal of Clinical Microbiology. 2006;44:2468–2474. doi: 10.1128/JCM.01882-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee I, Gladstone BP, LeFevre AM, et al. Neonatal infection with G10P[11] rotavirus does not confer protection against subsequent rotavirus infection in a community cohort in Vellore, South India. Journal of Infectious Diseases. 2007;195:625–632. doi: 10.1086/510853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresee JS, Glass RI, Ivanoff B, Gentsch J. Current status and future priorities for rotavirus vaccine development, evaluation, and implementation in developing countries. Vaccine. 1999;17:2207–2222. doi: 10.1016/s0264-410x(98)00376-4. [DOI] [PubMed] [Google Scholar]
- Fischer TK, Anh DD, Antil L, et al. Health care costs of diarrhoeal disease and estimates of the cost-effectiveness of rotavirus vaccination in Vietnam. Journal of Infectious Diseases. 2005;192:1720–1726. doi: 10.1086/497339. [DOI] [PubMed] [Google Scholar]
- Giaquinto C, Van Damme P, Huet F, Gothefors L, Van der Wielen M. Cost of community-acquired pediatric rotavirus gastroenteritis in 7 European countries: the reveal study. Journal of Infectious Diseases. 2007;195:S36–S44. doi: 10.1086/516716. [DOI] [PubMed] [Google Scholar]
- Isakbaeva ET, Musabaev E, Antil L, et al. Rotavirus disease in Uzbekistan: cost-effectiveness of a new vaccine. Vaccine. 2007;25:373–380. doi: 10.1016/j.vaccine.2006.07.029. [DOI] [PubMed] [Google Scholar]
- Jain V, Parashar UD, Glass RI, Bhan MK. Epidemiology of rotavirus in India. Indian Journal of Pediatrics. 2000;68:855–862. doi: 10.1007/BF02762113. [DOI] [PubMed] [Google Scholar]
- Lu CY, Lauderdale TL, Fang YH, et al. Disease burden and related medical costs of rotavirus infections in Taiwan. BMC Infectious Diseases. 2006;6:176–184. doi: 10.1186/1471-2334-6-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EA, Tam JS, Yu LM, et al. Hospital-based study of the economic burden associated with rotavirus diarrhoea in Hong Kong. Journal of Infectious Diseases. 2005;192:S64–S70. doi: 10.1086/431493. [DOI] [PubMed] [Google Scholar]
- Parashar UD, Hummelman EJ, Bresee JS, Miller MA, Glass RI. The global illness and deaths caused by rotavirus disease in children. Emerging Infectious Diseases. 2003;9:565–572. doi: 10.3201/eid0905.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parashar UD, Gibson CJ, Bresee JS, Glass RI. Rotavirus and severe childhood diarrhea. Emerging Infectious Diseases. 2006;12:304–306. doi: 10.3201/eid1202.050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podewils LJ, Antil L, Hummelman E, et al. Projected cost-effectiveness of rotavirus vaccination for children in Asia. Journal of Infectious Diseases. 2005;192:S133–S145. doi: 10.1086/431513. [DOI] [PubMed] [Google Scholar]
- Ruiz-Palacios GM, Pérez-Schael I, Velázquez FR, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. New England Journal of Medicine. 2006;354:11–22. doi: 10.1056/NEJMoa052434. [DOI] [PubMed] [Google Scholar]
- Vesikari T, Matson DO, Dennehy P, et al. Safety and efficacy of a pentavalent human–bovine (WC3) reassortant rotavirus vaccine. New England Journal of Medicine. 2006;354:23–33. doi: 10.1056/NEJMoa052664. [DOI] [PubMed] [Google Scholar]
- WHO . Guidelines for Estimating the Economic Burden of Diarrhoeal Disease with Focus on Assessing the Costs of Rotavirus Diarrhoea. Geneva: WHO; 2005. WHO/IVB/05.10. [Google Scholar]
- WHO Health financing. World Health Statistics 2007. 2007. http://www.who.int/whosis/database/core/core_select_process.cfm?countries=all&indicators=nha. Accessed: 25 June 2007.
- Zimmerman CM, Bresee JS, Parashar UD, Riggs TL, Holman RC, Glass RI. Cost of diarrhoea-associated hospitalisations and outpatient visits in an insured population of young children in the United States. Pediatric Infectious Diseases Journal. 2001;20:14–19. doi: 10.1097/00006454-200101000-00004. [DOI] [PubMed] [Google Scholar]


