Abstract
Hypertension is a risk factor for heart failure and stroke. However, the effect of hypertension in patients with heart failure has not been well studied. In the Digitalis Investigation Group trial, 3674 (47%) of the 7788 patients had a history of hypertension. Probability or propensity scores for a history of hypertension were calculated for each patient using a multivariable logistic regression model, and were then used to match 2386 pairs of patients without and with a history of hypertension. Kaplan-Meier and matched Cox regression analyses were used to estimate associations of a history of hypertension hospitalization due to stroke during 37 months of median follow up. After matching, patients without and with a history of hypertension had a mean systolic blood pressure of 127 mm Hg. Hospitalization due to stroke occurred in 90 patients (rate, 129/10,000 person-years of follow-up) without a history of hypertension and 121 patients (rate, 178/10,000 person-years of follow-up) with a history of hypertension (hazard ratio {HR} =1.52; 95% confidence interval {CI} =1.11–2.08; P=0.010). This association was also observed among patients with baseline systolic blood pressure <140 mm Hg (HR =1.35; 95% CI =1.01–1.81; P=0.044). A history of hypertension was associated with increased risk of hospitalization due to stroke among heart failure patients balanced in all measured baseline covariates including blood pressure.
Keywords: heart failure, NYHA class, natural history, outcomes, stroke, mortality
High blood pressure is a risk factor for stroke and normalization of blood pressure has been shown to reduce incident stroke.1–3 Hypertension is also a risk factor for heart failure (HF) and the prevalence of hypertension is high in patients with HF. The prevalence of stroke is also high in patients with HF.4 However, to what extent a history of hypertension, regardless of the level of blood pressure control, may be associated with incident stroke in HF is unknown. We studied the effect of a history of hypertension on hospitalizations due to stroke in a propensity-matched population of ambulatory chronic systolic and diastolic HF patients in normal sinus rhythm who were well balanced in all measured baseline covariates including blood pressure.
Methods
We used a public-use copy of the Digitalis Investigation Group (DIG) trial dataset obtained from the National Heart, Lung and Blood Institute. The design of the DIG trial has been previously described.5 Of the 7788 ambulatory patients with chronic HF enrolled in the DIG trial, 3674 (47%) had a history of hypertension and no baseline history of stroke was reported. Most patients were receiving angiotensin-converting enzyme inhibitor and diuretics. The presence of baseline hypertension was ascertained by investigators based on chart documentation of past medical history. For the purpose of the current analysis, hospitalization due to stroke was the primary outcome. Data on type of stroke were not available. Hospitalization due to stroke was a pre-specified secondary outcome in the DIG trial. The diagnosis leading to hospitalization was classified by DIG investigators, who were blinded to the patient’s study-drug assignment. However, these diagnoses were not centrally adjudicated. Patients were followed up for a median duration of 38 months and follow up was 99% complete.6
Due to the significant imbalance in baseline covariates between patients with and without hypertension (Table 1), we used propensity score matching to assemble a balanced cohort of patients. The propensity score is the conditional probability of receiving an exposure (e.g. hypertension) given a set of measured covariates.7–9 We estimated propensity scores for hypertension for each of the 7788 patients, using a non-parsimonious multivariable logistic regression model (c statistic=0.76) and used that to match 2386 pairs of patients with and without hypertension.10–14 We assessed the effectiveness of matching and bias reduction by estimating standardized differences, expressed as a percentage of the pooled standard deviations. We also provide paired-sample t- and McNemar tests to describe the baseline characteristics of patients with and without hypertension.
Table 1.
Baseline patient characteristics in patients with and without a history of hypertension, before and after propensity score matching
| Before matching
|
After matching
|
|||||
|---|---|---|---|---|---|---|
| History of hypertension | History of hypertension | |||||
| Variables | No (N =4114) | Yes (N =3674) | P value | No (N =2386) | Yes (N =2386) | P value |
| Age (years) | 63.4 (±11.2) | 64.5 (±10.5) | <0.0001 | 64.3 (±11.2) | 64.4 (±10.2) | 0.776 |
| Women | 836 (20%) | 1090 (30%) | <0.0001 | 589 (25%) | 560 (24%) | 0.334 |
| Non-whites | 316 (8%) | 812 (22%) | <0.0001 | 283 (12%) | 294 (12%) | 0.628 |
| Body mass index (kg/m2) | 26.5 (±4.8) | 28.2 (±5.8) | <0.0001 | 27.3 (±5.1) | 27.1 (±4.9) | 0.394 |
| Heart failure duration (months) | 30.5 (±36.5) | 29.0 (±36.2) | 0.088 | 29.8 (±35.6) | 29.1 (±36.2) | 0.510 |
| Ischemic cause of heart failure | 3054 (74%) | 2306 (63%) | <0.0001 | 1677 (70%) | 1671 (70%) | 0.873 |
| Prior myocardial infarction | 2790 (68%) | 2118 (58%) | <0.0001 | 1516 (64%) | 1517 (64%) | 1.000 |
| Current angina pectoris | 1104 (27%) | 1011 (28%) | 0.499 | 647 (27%) | 661 (28%) | 0.667 |
| Diabetes mellitus | 903 (22%) | 1315 (36%) | <0.0001 | 679 (29%) | 692 (29%) | 0.688 |
| Chronic kidney disease | 1740 (42%) | 1787 (49%) | <0.0001 | 1130 (47%) | 1120 (47%) | 0.794 |
| Medications | ||||||
| Digoxin (pre-trial use) | 1875 (46%) | 1490 (41%) | <0.0001 | 1070 (45%) | 1035 (43%) | 0.324 |
| Digoxin (by randomization) | 2057 (50%) | 1832 (50%) | 0.905 | 1181 (50%) | 1190 (50%) | 0.814 |
| Angiotensin-converting enzyme inhibitors | 3829 (93%) | 3445 (94%) | 0.218 | 2234 (94%) | 2238 (94%) | 0.859 |
| Hydralazine and Nitrates | 29 (1%) | 82 (2%) | <0.0001 | 25 (1%) | 26 (1%) | 1.000 |
| Non-potassium-sparing diuretics | 3067 (75%) | 3009 (82%) | <0.0001 | 1891 (79%) | 1890 (79%) | 1.000 |
| Potassium-sparing diuretics | 329 (8%) | 267 (7%) | 0.227 | 200 (8%) | 191 (8%) | 0.673 |
| Potassium supplement | 1048 (26%) | 1151 (31%) | <0.0001 | 699 (29%) | 698 (29%) | 1.000 |
| Symptoms and signs of heart failure | ||||||
| Dyspnea at rest | 755 (18%) | 950 (26%) | <0.0001 | 505 (21%) | 506 (21%) | 1.000 |
| Dyspnea on exertion | 3092 (75%) | 2770 (75%) | 0.809 | 1785 (75%) | 1809 (76%) | 0.436 |
| Jugular venous distension | 488 (12%) | 532 (15%) | 0.001 | 316 (13%) | 318 (13%) | 0.966 |
| Third heart sound | 1006 (25%) | 840 (23%) | 0.100 | 574 (24%) | 560 (24%) | 0.661 |
| Pulmonary râles | 624 (15%) | 677 (18%) | <0.0001 | 377 (16%) | 396 (17%) | 0.478 |
| Lower extremity edema | 670 (16%) | 963 (26%) | <0.0001 | 486 (20%) | 470 (20%) | 0.586 |
| New York Heart Association functional class | ||||||
| I | 580 (14%) | 523 (14%) | 348 (15%) | 334 (14%) | ||
| II | 2245 (55%) | 1999 (54%) | 0.907 | 1317 (55%) | 1302 (55%) | 0.496 |
| III | 1212 (30%) | 1075 (29%) | 674 (28%) | 701 (29%) | ||
| IV | 77 (2%) | 77 (2%) | 47 (2%) | 49 (2%) | ||
| Heart rate (beats per minute) | 78 (±12) | 79 (±13) | <0.0001 | 78 (±13) | 78 (±13) | 0.986 |
| Systolic blood pressure (mm Hg) | 121 (±17) | 135 (±21) | <0.0001 | 127 (±17) | 127 (±18) | 0.735 |
| Diastolic blood pressure (mm Hg) | 72 (±10) | 78 (±12) | <0.0001 | 75 (±10) | 75 (±11) | 0.677 |
| Chest radiograph findings | ||||||
| Pulmonary congestion | 538 (13%) | 571 (16%) | 0.002 | 319 (13%) | 336 (14%) | 0.502 |
| Cardiothoracic ratio > 0.5 | 2306 (56%) | 2384 (65%) | <0.0001 | 1446 (61%) | 1447 (61%) | 1.000 |
| Serum concentrations | ||||||
| Creatinine (mg/dL) | 1.3 (±0.3) | 1.3 (±0.4) | <0.0001 | 1.3 (±0.4) | 1.3 (±0.4) | 0.826 |
| Potassium (mEq/L) | 4.4 (±0.4) | 4.3 (±0.5) | 0.002 | 4.3 (±0.5) | 4.3 (±0.4) | 0.761 |
| Estimated glomerular filtration rate (ml/min per 1.73 m2) | 65 (±21) | 62 (±24) | <0.0001 | 63 (±20) | 63 (±25) | 0.322 |
| Ejection fraction >45 % | 398 (10%) | 590 (16%) | <0.0001 | 289 (12%) | 288 (12%) | 1.000 |
| Ejection fraction (%) | 31 (±12) | 34 (±13) | <0.0001 | 32 (±12) | 32 (±12) | 0.792 |
We used Kaplan-Meier and matched Cox regression analyses to determine the effect of baseline hypertension on outcome. Even though our matched cohort was well-balanced in all measured baseline covariates, we cannot rule out hidden bias due to imbalances in unmeasured covariates. Therefore, we conducted a formal sensitivity analysis to quantify the degree of a hidden bias that would need to be present to invalidate our main conclusions.15
To determine if the effect of a history of hypertension on incident stroke was modified by baseline blood pressure control, we conducted a subgroup analysis among patients with normal (<140 mm Hg) and above-normal (≥140 mm Hg) baseline systolic blood pressure using the pre-match cohort and adjusting for propensity scores. All data analyses were performed using SPSS-15 for Windows.16 All P values were 2-sided and P < 0.05 was regarded as statistically significant.
Results
The mean (±SD) age of the 4772 matched patients was 64 (±11) years (range 21–94), 24% were women, and 12% were non-whites. There were no significant imbalances in any measured baseline covariates between patients with and without hypertension after matching (Table 1). Before matching, mean systolic and diastolic blood pressures were higher in those with a history of hypertension but was similar after matching. After matching, absolute standardized differences for all baseline covariates were less than 10% and most were <5%, suggesting substantial bias reduction (Figure 1).
Figure 1.

Absolute standardized differences before and after propensity score matching comparing covariate values for patients with and without a history of hypertension
Hospitalizations due to stroke occurred in 90 (rate, 129/10,000 person-years) patients without a history of hypertension and 121 (rate, 178/10,000 person-years) patients with a history of hypertension (hazard ratio {HR}=1.52; 95% confidence interval {CI}=1.11–2.08; P=0.001; Figure 2 and Table 2). Extrapolated to an estimated 5 million HF patients in the United States, a history of hypertension would be responsible for an additional 40422 hospitalizations due to stroke. The rates of hospitalizations due to stroke before matching are also displayed in Table 2. Our sensitivity analysis reveals that an unmeasured binary covariate would need to increase the odds of “not having hypertension” by more than 10.6% to explain away this association (z-statistic=2.61; two-tailed p = 0.0093), suggesting that these results are insensitive to modest hidden biases.
Figure 2.
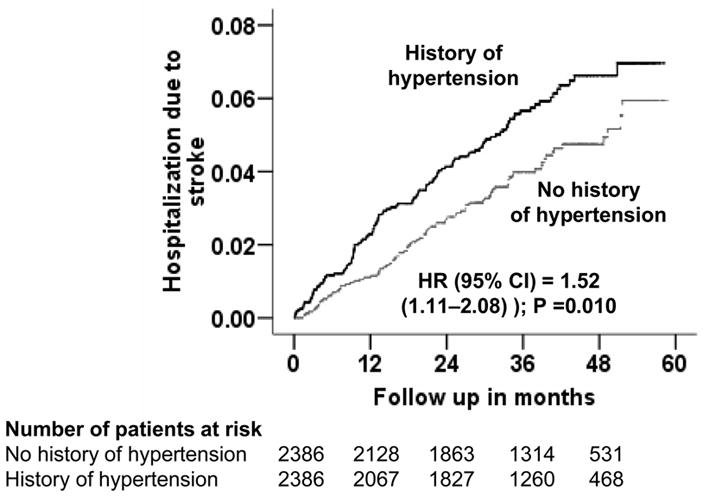
Kaplan-Meier plots for hospitalization due to stroke for patients with and without a history of hypertension
Table 2.
History of hypertension and hospitalization due to stroke, before and after propensity score matching
| Outcomes | Rate/10,000 person-years (events/total follow up years)
|
Absolute increase in rate/10000 person-years* | Increase in the number of stroke hospitalizations in the US** | Hazard ratio (95% confidence interval) | P value | |
|---|---|---|---|---|---|---|
| No history of hypertension | History of hypertension | |||||
| Before matching | (n =4,114) | (n =3,674) | ||||
| Hospitalization due to stroke | 126 (151/11,978) | 207 (215/10,391) | + 80 | + 40,422 (103,454 – 63,032) | 1.63 (1.33–2.01) | <0.0001 |
| After matching | (n =2,386) | (n =2,386) | ||||
| Hospitalization due to stroke | 129 (90/6,996) | 178 (121/6,789) | + 49 | + 24,792 (89,115 – 64,322) | 1.52 (1.11–2.08) | 0.010 |
Absolute rate differences were calculated by subtracting the rates of hospitalizations due to stroke in the no hypertension group from the rate in the hypertension group (before values were rounded).
Number of hospitalizations for stroke for an estimated 5 million heart failure patients in the US was calculated by subtracting the number of hospitalizations due to stroke in the no hypertension group from that in the hypertension group (before values were rounded).
Of the 7788 pre-match patients, 2363 (30.3%) had baseline systolic blood pressure ≥140 mmHg. Among patients with normal baseline systolic blood pressure (<140 mm Hg), stroke hospitalization occurred in 3.4% (115/3360) and 4.8% (99/2065) of patients without and with a history of hypertension (HR=1.35; 95% CI =1.01–1.81; P=0.044). Among patients with above-normal baseline systolic blood pressure (≥140 mm Hg), stroke hospitalization occurred in 4.8% (36/754) and 7.2% (116/1609) of patients without and with a history of hypertension (HR =1.35; 95% CI =0.91–2.02; P=0.139). There was no interaction between a history of hypertension and baseline systolic blood pressure. The effect of a history of hypertension on stroke hospitalization was similar in both genders and regardless of ejection fraction (data not shown). A history of hypertension was also associated with all-cause hospitalization (HR=1.13; 95% CI=1.03–1.23; P=0.009) and cardiovascular hospitalization (HR =1.13; 95% CI =1.03–1.23; P=0.009) but had no association with all-cause mortality (HR =1.02; 95% CI =0.92–1.15; P=0.689).
Discussion
These findings of the current analysis suggest that in ambulatory patients with chronic mild to moderate HF, a history of hypertension was common and was associated with increased risk of incident hospitalization due to stroke despite similar baseline blood pressure. Further, a history of hypertension was associated with increased risk of stroke among those with normal baseline blood pressure.
The findings of our study are consistent with those in the literature suggesting a positive association between hypertension and stroke. Though the effect of blood pressure and hypertension on stroke has been well studied in the general population, less is known about the effect of a history of hypertension regardless of the level of blood pressure control on stroke in those with HF.17,18 To the best of our knowledge this is the first report of the effect of a history of hypertension on stroke in a propensity-matched cohort of HF patients who were well balanced in all measured covariates including baseline blood pressure.
Despite the increased risk for stroke in HF, currently there is no evidence that antiplatelet or anticoagulation therapy is effective in preventing stroke in these patients and current guidelines do not recommend the routine use of anticoagulants in HF patients with normal sinus rhythm.19–21 This highlights the importance of identifying HF patients at high risk for stroke such as those with a history of hypertension. The effect of hypertension on stroke may be attenuated with the reduction of blood pressure.1,2,22–24 However, it is unlikely to fully explain the reduction in the risk of stroke in patients receiving anti-hypertensive therapy.25,26 Activation of the renin-angiotensin-aldosterone system in stroke is believed to play a major role in causing ischemic vascular injury to vital organs including the brain and their inhibitors may provide benefit beyond blood pressure control.27–29 However, differences in the use of ACE inhibitors may not explain the results of our analysis as over 90% of patients in the DIG trial were receiving ACE inhibitors and patients were balanced in all measured baseline covariates including use of ACE inhibitors.
The risk of stroke in HF patients with controlled hypertension was similar to those with new-onset hypertension (baseline high systolic blood pressure in those without a history of hypertension). This suggests that factors other than the level of blood pressure control may be associated with the pathogenesis of stroke in these patients.30 However, this also suggests that lower baseline blood pressure was associated with fewer strokes, highlighting the importance of monitoring and controlling blood pressure in HF.
Our study has several limitations. In the DIG trial, the incidence of hospitalization due to stroke was not a major endpoint and was not centrally adjudicated. Therefore, misclassification is possible. However, because this was likely a random misclassification, it may have underestimated the association observed in the current analysis. Imbalances in unmeasured covariates, may explain our findings, if such covariates are strongly correlated with a history of hypertension and incident stroke, and not strongly correlated with covariates used to estimate propensity scores (Table 1). We had no data on duration and control of hypertension and other anti-hypertensive drugs used. It is possible that some patients without baseline history of hypertension may have developed hypertension during follow up. However, this regression dilution may have underestimated the association observed in our analysis. Finally, patients in our analysis are relatively young male HF patients in normal sinus rhythm from the early 1990s and their relevance to contemporary HF patients is unknown.
In conclusion, a history of hypertension was associated with increased risk of hospitalizations due to stroke in HF patients with normal sinus rhythm who were well-balanced in all measured baseline covariates including blood pressure and that this association persisted in the subgroup with normal blood pressure. Future studies are needed to better understand factors associated with increased risk of stroke in HF patients with a history of hypertension and normal blood pressure.
Acknowledgments
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants from the National Heart, Lung, and Blood Institute (1-R01-HL085561-01 and P-50-HL077100).
“The Digitalis Investigation Group (DIG) study was conducted and supported by the NHLBI in collaboration with the DIG Investigators. This Manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the DIG Study or the NHLBI.”
Footnotes
Conflict of Interest Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hypertension-Stroke Cooperative Study Group. Effect of antihypertensive treatment on stroke recurrence. JAMA. 1974;229:409–418. doi: 10.1001/jama.1974.03230420021019. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Wolf PA, McGee DL, Dawber TR, McNamara P, Castelli WP. Systolic blood pressure, arterial rigidity, and risk of stroke. The Framingham study. JAMA. 1981;245:1225–1229. [PubMed] [Google Scholar]
- 3.Alla F, Zannad F, Filippatos G. Epidemiology of acute heart failure syndromes. Heart Fail Rev. 2007;12:91–95. doi: 10.1007/s10741-007-9009-2. [DOI] [PubMed] [Google Scholar]
- 4.Wolf PA, Kannel WB, McNamara PM. Occult impaired cardiac function, congestive heart failure, and risk of thrombotic stroke: the Framingham Study. Neurology. 1970;20:373. [PubMed] [Google Scholar]
- 5.The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–533. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 6.Collins JF, Howell CL, Horney RA. Determination of vital status at the end of the DIG trial. Control Clin Trials. 2003;24:726–730. doi: 10.1016/j.cct.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 8.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 9.Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- 10.Ahmed A. A propensity matched study of New York Heart Association class and natural history end points in heart failure. Am J Cardiol. 2007;99:549–553. doi: 10.1016/j.amjcard.2006.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed A, Husain A, Love TE, Gambassi G, Dell'Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed A, Perry GJ, Fleg JL, Love TE, Goff DC, Jr, Kitzman DW. Outcomes in ambulatory chronic systolic and diastolic heart failure: a propensity score analysis. Am Heart J. 2006;152:956–966. doi: 10.1016/j.ahj.2006.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed A, Rich MW, Sanders PW, Perry GJ, Bakris GL, Zile MR, Love TE, Aban IB, Shlipak MG. Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol. 2007;99:393–398. doi: 10.1016/j.amjcard.2006.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed A, Zannad F, Love TE, Tallaj J, Gheorghiade M, Ekundayo OJ, Pitt B. A propensity-matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J. 2007;28:1334–1343. doi: 10.1093/eurheartj/ehm091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenbaum PR. Observational Studies. New York: Springer-Verlag; 2002. [Google Scholar]
- 16.SPSS. SPSS for Windows, Rel. 15. Chicago, IL: SPSS Inc., Chicago, IL; 2007. [Google Scholar]
- 17.Pullicino PM, Halperin JL, Thompson JL. Stroke in patients with heart failure and reduced left ventricular ejection fraction. Neurology. 2000;54:288–294. doi: 10.1212/wnl.54.2.288. [DOI] [PubMed] [Google Scholar]
- 18.Dries DL, Rosenberg YD, Waclawiw MA, Domanski MJ. Ejection fraction and risk of thromboembolic events in patients with systolic dysfunction and sinus rhythm: evidence for gender differences in the studies of left ventricular dysfunction trials. J Am Coll Cardiol. 1997;29:1074–1080. doi: 10.1016/s0735-1097(97)00019-3. [DOI] [PubMed] [Google Scholar]
- 19.Cleland JG, Ghosh J, Freemantle N, Kaye GC, Nasir M, Clark AL, Coletta AP. Clinical trials update and cumulative meta-analyses from the American College of Cardiology: WATCH, SCD-HeFT, DINAMIT, CASINO, INSPIRE, STRATUS-US, RIO-Lipids and cardiac resynchronisation therapy in heart failure. Eur J Heart Fail. 2004;6:501–508. doi: 10.1016/j.ejheart.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 20.Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich A, Hoes A, Jaarsma T, Korewicki J, Levy S, Linde C, Lopez-Sendon JL, Nieminen MS, Pierard L, Remme WJ. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26:1115–1140. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 21.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 22.Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. III. Reduction in stroke incidence among persons with high blood pressure. JAMA. 1982;247:633–638. [PubMed] [Google Scholar]
- 23.Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension) Lancet. 1991;338:1281–1285. doi: 10.1016/0140-6736(91)92589-t. [DOI] [PubMed] [Google Scholar]
- 24.Hansson L, Lindholm LH, Ekbom T, Dahlof B, Lanke J, Schersten B, Wester PO, Hedner T, de Faire U. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354:1751–1756. doi: 10.1016/s0140-6736(99)10327-1. [DOI] [PubMed] [Google Scholar]
- 25.Lubsen J, Voko Z, Poole-Wilson PA, Kirwan BA, de Brouwer S. Blood pressure reduction in stable angina by nifedipine was related to stroke and heart failure reduction but not to coronary interventions. J Clin Epidemiol. 2007;60:720–726. doi: 10.1016/j.jclinepi.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 26.Ekbom T, Dahlof B, Hansson L, Lindholm LH, Oden A, Schersten B, Wester PO. The stroke preventive effect in elderly hypertensives cannot fully be explained by the reduction in office blood pressure--insights from the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension) Blood Press. 1992;1:168–172. doi: 10.3109/08037059209077513. [DOI] [PubMed] [Google Scholar]
- 27.Laragh JH. Renin-angiotensin-aldosterone system for blood pressure and electrolyte homeostasis and its involvement in hypertension, in congestive heart failure and in associated cardiovascular damage (myocardial infarction and stroke) J Hum Hypertens. 1995;9:385–390. [PubMed] [Google Scholar]
- 28.Papademetriou V, Farsang C, Elmfeldt D, Hofman A, Lithell H, Olofsson B, Skoog I, Trenkwalder P, Zanchetti A. Stroke prevention with the angiotensin II type 1-receptor blocker candesartan in elderly patients with isolated systolic hypertension: the Study on Cognition and Prognosis in the Elderly (SCOPE) J Am Coll Cardiol. 2004;44:1175–1180. doi: 10.1016/j.jacc.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 29.Iadecola C, Gorelick PB. Hypertension, angiotensin, and stroke: beyond blood pressure. Stroke. 2004;35:348–350. doi: 10.1161/01.STR.0000115162.16321.AA. [DOI] [PubMed] [Google Scholar]
- 30.Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, Thomas F, Pannier B, Asmar R, Zureik M, Safar M, Guize L. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation. 2002;105:1202–1207. doi: 10.1161/hc1002.105135. [DOI] [PubMed] [Google Scholar]


