Abstract
Objective:
To examine and summarize previous retrospective and observational studies assessing noncontact anterior cruciate ligament (ACL) injury mechanisms and to examine such reported ACL injury mechanisms based on ACL loading patterns due to knee loadings reported in in vivo, in vitro, and computer simulation studies.
Data Sources:
We searched MEDLINE from 1950 through 2007 using the key words anterior cruciate ligament + injury + mechanisms; anterior cruciate ligament + injury + mechanisms + retrospective; and anterior cruciate ligament + injury + mechanisms + video analysis.
Study Selection:
We selected retrospective studies and observational studies that specifically examined the noncontact ACL injury mechanisms (n = 7) and assessed ACL loading patterns in vivo, in vitro, and using computer simulations (n = 33).
Data Extraction:
The motion patterns reported as noncontact ACL injury mechanisms in retrospective and observational studies were assessed and critically compared with ACL loading patterns measured during applied external or internal (or both) forces or moments to the knee.
Data Synthesis:
Noncontact ACL injuries are likely to happen during deceleration and acceleration motions with excessive quadriceps contraction and reduced hamstrings co-contraction at or near full knee extension. Higher ACL loading during the application of a quadriceps force when combined with a knee internal rotation moment compared with an external rotation moment was noted. The ACL loading was also higher when a valgus load was combined with internal rotation as compared with external rotation. However, because the combination of knee valgus and external rotation motions may lead to ACL impingement, these combined motions cannot be excluded from the noncontact ACL injury mechanisms. Further, excessive valgus knee loads applied during weight-bearing, decelerating activities also increased ACL loading.
Conclusions:
The findings from this review lend support to ACL injury prevention programs designed to prevent unopposed excessive quadriceps force and frontal-plane or transverse-plane (or both) moments to the knee and to encourage increased knee flexion angle during sudden deceleration and acceleration tasks.
Keywords: injury mechanism, injury prevention, lower extremity injury, knee
An estimated 80 000 anterior cruciate ligament (ACL) injuries occur annually in the United States,1 and ACL-injured people often suffer long-term complications, such as meniscal lesions, impairment of normal knee function, and arthrofibrosis.2–4 These complications and the extended time loss from sport participation can be major setbacks for athletes. Although several injury prevention programs have been designed and shown to reduce the injury rate to some extent,5,6 information is lacking about how and which components of these training programs are effective in modifying movement patterns or neuromuscular control during dynamic activities. Understanding the mechanisms of noncontact ACL injury may help us better design and focus our neuromuscular training programs to more effectively prevent at-risk motions that may lead to ACL injury.
Mechanisms of ACL injury have been investigated using a variety of research models, including retrospective interviews, chart reviews, and observational video analyses. However, as a result of limitations in these studies, it is not possible to directly determine how the ACL is injured. Therefore, in vivo and in vitro biomechanical studies of ACL loading patterns and mathematical modeling such as computer simulations have also been used to examine the loads (ie, force, moment) stressing the ACL. Thus, our first objective was to examine and summarize previous retrospective and observational studies that described noncontact ACL injury mechanisms. Our second objective was to further examine the described ACL injury mechanisms based on in vivo, in vitro, and computer simulation studies of ACL loading patterns in response to combined directional loads.
Study Selection/data Extraction
A literature search was done using MEDLINE; we reviewed literature from 1950 through 2007. For our first purpose, we searched the literature using a combination of the following key words: anterior cruciate ligament + injury + mechanisms, anterior cruciate ligament + injury + mechanisms + retrospective, and anterior cruciate ligament + injury + mechanisms + video analysis. Studies that we included in addressing our first purpose were those in which the authors (1) retrospectively reviewed medical charts for ACL-injured patients and/or interviewed ACL-injured patients using questionnaires, etc, (2) described specific motions (eg, knee internal-external, valgus-varus motions) at the time at which the noncontact ACL injury happened based on video observations, and (3) assessed noncontact ACL injuries that were not equipment related (eg, skiing injuries). We also included studies that reported the activities observed at the time of noncontact ACL injuries to further examine the knee loading that possibly occurred at the time of injury. When the patient injured the ACL during functional activities in the absence of any external forces other than the ground reaction force, we defined such ACL injuries as noncontact injuries.
For our second purpose, we used a combination of anterior cruciate ligament and the following key words: loading in vivo, loading in vitro, force in vivo, strain in vivo, force in vitro, strain in vitro, forward dynamics, computer simulation, quadriceps loading, quadriceps force, quadriceps strain, hamstring loading, hamstring force, hamstring strain, gastrocnemius loading, gastrocnemius force, gastrocnemius strain, loading closed kinetic chain, force closed kinetic chain, and strain closed kinetic chain. Studies were included if they were (1) conducted in vivo or in vitro and directly examined ACL loading (ie, ACL tensile force or strain) as a result of muscle forces and other combined knee loadings, including knee muscle force, force on the tibia, or moment to the knee joint, (2) conducted in vivo or in vitro and directly examined ACL loading during functional weight-bearing tasks, and 3) computer simulations that estimated ACL loading patterns during weight-bearing functional tasks. We limited our review to these studies for our second purpose, as our review of described mechanisms of noncontact ACL injuries revealed they are more likely to be multiplane loading in nature and to happen during weight-bearing activities. We chose not to include studies that examined sex differences in biomechanical factors during “at-risk” motions for the ACL, as they did not directly assess ACL loading patterns. Additional citations that were not identified in the initial literature search were obtained via recommendations from experts and references from the articles retrieved.
To clarify, we defined the knee motions described in this review as follows: (1) knee internal (external) rotation as tibial internal (external) rotation relative to the femur in the transverse plane and (2) knee valgus (varus) as tibial abduction (adduction) relative to the femur in the frontal plane. Results from these studies are summarized and compared to identify the current state of knowledge regarding possible noncontact ACL injury mechanisms.
Results
For our first purpose, we initially retrieved a total of 608 articles through MEDLINE. From these articles, we identified 7 articles that met our inclusion criteria. The findings of these studies are summarized in Table 1. For our second objective, 847 citations were initially retrieved. From these citations, 33 articles (7 in vivo, 18 in vitro, and 8 computer simulation studies) were identified that met our inclusion criteria. The summary findings for these studies are categorized by knee muscle forces, multiplane knee loadings, weight-bearing functional activities in vivo and in vitro, and computer simulation models. These results are presented in Tables 2 through 7.
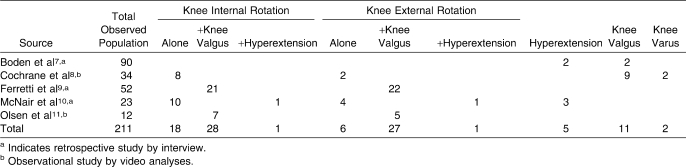
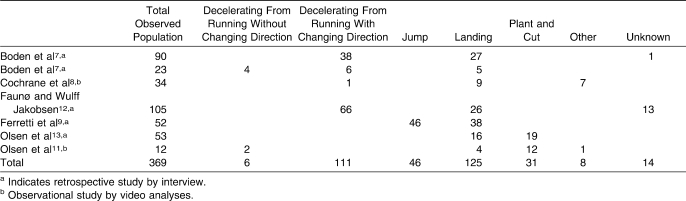
Table 1a.
Mechanisms of Anterior Cruciate Ligament Injuries Described by Previous Authors
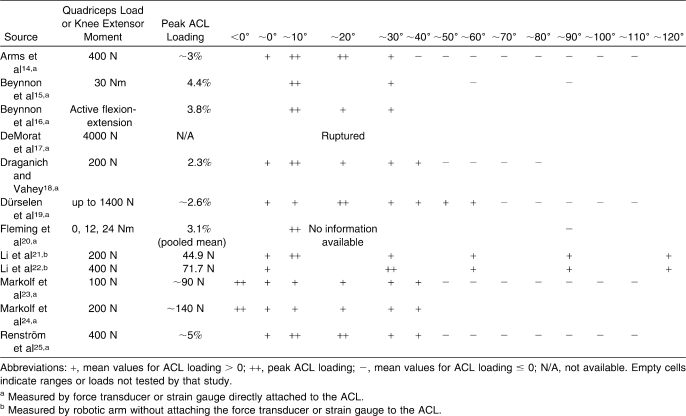
Table 2.
Anterior Cruciate Ligament (ACL) Loading Responses Due to Quadriceps Muscle Force or Produced Knee Extensor Moment at Different Knee Flexion Angles in Previous In Vivo and In Vitro Studies
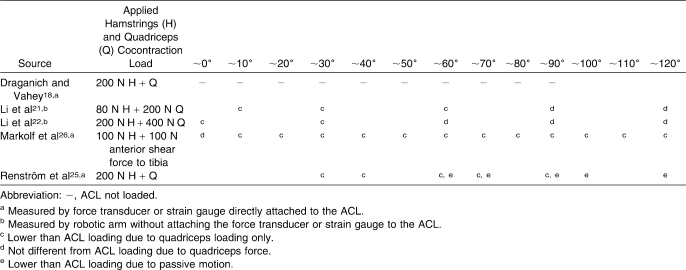
Table 3.
The Effects of Hamstrings Muscle Cocontraction Forces (H) With Quadriceps Muscle Force (Q) or Anterior Shear Force to the Tibia on Anterior Cruciate Ligament (ACL) Loading Responses at Different Knee Flexion Angles in Previous In Vivo and In Vitro Studiesa
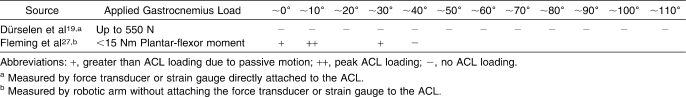
Table 4.
Anterior Cruciate Ligament (ACL) Loading Responses Due to Gastrocnemius Muscle Force at Different Knee Flexion Angles in Previous In Vivo and In Vitro Studies
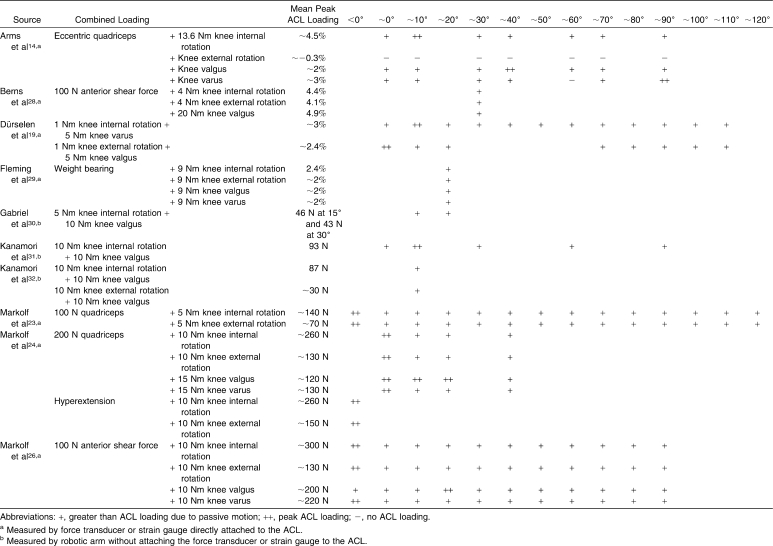
Table 5.
Anterior Cruciate Ligament (ACL) Loading Responses Due to Combined Knee Loading in Previous In Vivo and In Vitro Studies
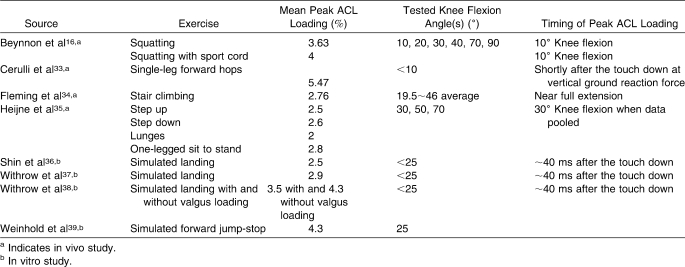
Table 6.
Anterior Cruciate Ligament (ACL) Loading Responses Due to Closed Kinetic Chain Exercise in Previous In Vivo and In Vitro Studies
Discussion
Our primary finding was that the mechanisms of noncontact ACL injuries appeared to be multiplane knee loadings. The ACL may be loaded excessively if vigorous quadriceps forces are combined with frontal-plane and/or transverse-plane knee loadings with insufficient hamstrings muscle cocontraction forces, especially when the knee is at near-extension or hyperextension. We will discuss the results from retrospective and observational studies first in order to examine the motions observed at the time of noncontact ACL injuries. In the following sections, we will discuss the effects of knee muscle forces, multiplane knee loadings, and weight-bearing activities in vivo and in vitro on ACL loading patterns and, finally, we will present results from computer simulation models that examined ACL loading patterns during functional tasks.
Retrospective Interviewing Studies
Mechanisms of ACL injury have been retrospectively investigated by interviewing those who have sustained an ACL injury (Table 1).7,9,10,12,13 Most of the injuries are reported to occur with noncontact mechanisms, such as those involving landing from a jump and sudden deceleration of the body while running, with or without a change in direction.7,9,10,12,13 A common characteristic in these retrospective studies is that ACL-injured individuals often report that the knee moves in multiple planes of motion.9,10,13 For example, in many cases patients reported that the knee went into valgus with either internal or external rotation while the knee was hyperextended or in a shallow knee flexion angle (eg, 20°).9,10 Another important characteristic appears to be the knee flexion angle at the time of injury. Although one group10 reported that the ACL injury occurred when the knee was at or near full extension, knee hyperextension is also often reported as part of the mechanism.7,10 Also, the majority of noncontact ACL injuries were reported to happen during weight-bearing conditions,7,9,10,12,13 a finding supported by Faunø and Wulff Jakobsen,12 who noted that 104 of 105 ACL-injured patients stated that the injury happened when the injured foot was in contact with the ground.
Some limitations are inherent when using these retrospective methods to identify the injury mechanism. All the information gained about the mechanism of ACL injury depends on the patient's recall and senses to describe the positions of each lower extremity segment at the time of the injury. Boden et al7 reported that the time of interview was, on average, 3.4 years after the injury (range = 1 day–30.3 years). With this range between injury and interview, it is questionable whether all patients accurately recalled the exact mechanisms or the position of their body at the time of injury. This may be true especially for small motions, such as knee internal-external rotation. For these reasons, descriptions of the ACL injury mechanism are often vague.7,9,10 Moreover, the internal-external forces and moments applied to the tibia at the time of injury cannot be determined from these studies.
Even with these limitations, important information regarding the mechanisms of ACL injury has been gained. From these reports, noncontact injury may be more likely to occur when the knee is in a shallow flexion angle10 or a hyperextended position,7,10 and the often-observed combined motions in both frontal and transverse planes during sudden deceleration motions indicate that ACL injury likely results from multiplane knee loading.7,9,10,12,13
Observational Analyses
Qualitative (observational) analyses using video7,8,11 are consistent with retrospective interviews noting that ACL injuries happened during weight-bearing activities at a shallow knee flexion angle (eg, 5° to approximately 20°), often with combined knee motions (Table 1). In particular, valgus motions were frequently observed with transverse-plane knee rotation motions.7,8,11 Boden et al7 and Olsen et al11 described other important features that ACL-injured patients demonstrated at the time of the injury. Boden et al7 observed that the injured leg was often placed in front of the body with the upper body leaning backward, whereas Olsen et al11 observed that players were often perturbed by other opponents just before landing.
Although these expert observations shed further light on the mechanisms of ACL injury, a primary limitation of these observational studies is that the time point at which ACL injury actually occurs cannot accurately be determined. The authors provided no explanation for how they determined the moment of injury,7,8,11 and it is difficult to decipher if the joint angles and motions observed occurred before or after injury. For example, Ireland47 coined the term position of no return to describe the combined motions of hip adduction and internal rotation, external rotation of the tibia relative to the femur, internal rotation of the tibia on the foot, and forefoot pronation. However, it is possible that the observed position of no return is a result of the ACL injury, not the mechanism leading to the ACL injury itself. Further, exact movements of bony segments cannot be precisely determined by these visual techniques. However, given the consensus of these reports with the retrospective studies previously described, observational studies continue to support the typical occurrence of ACL injuries as a result of combined motion patterns,7,8,11 especially with weight bearing7,8,11 and the knee near full extension.8,11
Based on the findings from these retrospective and observational studies, we then examined the literature relative to the effects of isolated and combined muscle forces about the knee on ACL loading; these muscle forces include the quadriceps, hamstrings (as a hip extensor), and gastrocnemius muscles. We then examined studies that investigated the effects of combined knee loading, such as combined frontal-plane and transverse-plane knee loadings and knee muscle forces with hyperextension and transverse-plane or frontal-plane knee loadings in vivo and in vitro. Finally, we examined studies that examined the effects of functional weight-bearing tasks on ACL loading patterns in vivo, in vitro, and in computer simulations. Results from these studies are discussed in order to examine how motions observed at the time of ACL injury correspond with actual ACL loadings.
Anterior Cruciate Ligament Loading in Vivo and in Vitro
Anterior cruciate ligament loading patterns have been examined by applying external loads (eg, moment, force) to the knee both in vivo and in vitro. In vivo study denotes an investigation with a living organism, whereas in vitro study describes an investigation performed in the laboratory, usually using isolated tissue, organ, or cell preparations (eg, cadaver knees).48 Although the authors of these studies did not directly examine mechanisms of ACL injuries, they provide further evidence regarding external loads that may possibly stress and damage the ACL.
Generally speaking, 2 measurement methods have been used to assess ACL tensile forces or strain during the application of various external loads to the knee.49 One method is to use a small force transducer or strain gauge attached to the origin or insertion of the ACL to directly measure the amount of ACL tensile force or strain.* Another method, which does not directly attach a force transducer or strain gauge to the ACL, has been introduced by Woo et al.49 Using a robotic arm with a 6–degrees-of-freedom force transducer, various loads are applied to cadaver knees with most of the passive structures present. The robotic arm records the force during the application of loads to the knee. Then the ACL is cut, and the robotic arm loads the knee in the same path of movement as before. The force obtained by subtracting the force with the ACL absent from the force of the intact ACL is considered to be the force developed in the ACL. The force transducer method can only obtain the magnitude of ACL tensile force, but the latter robotic arm method can obtain not only the magnitude of the force vector but also the direction and origin of the force vector.49
Strain is measured using a small gauge implanted on the ACL, usually on the anteromedial bundle.15,16,20,29,34 Because the strain gauge is small, ACL strain has been obtained from both living humans and cadavers.† Strain represents the change in length of the ACL from its initial length and is expressed as a percentage of its initial length. In contrast to force measurement, a lack of change in ACL strain does not necessarily mean that the ACL is not loaded. Rather, it simply means that the force did not result in a change of length of the ACL from its initial length in the section where the strain gauge is attached. Also, because the strain gauge is attached to only a small part of the ACL (usually the anteromedial bundle), the strain measured at the implanted site may not represent strain across the ACL as a whole.
One of the advantages of using cadaveric knees (ie, in vitro studies) to assess ACL loading behavior is that it is easier to control knee joint kinematics and kinetics (ie, the force or moment applied to the knee). However, because the patterns of ACL loading due to various types of external loading may depend on how intact the knee specimen is,14 ACL loading patterns demonstrated by cadaveric knees may not represent ACL loading patterns in the living human. Although in vivo studies may overcome such limitations of these in vitro studies, it is difficult to control and assess external and internal forces or moments acting on the intact knee joint, making it difficult to determine the forces and moments responsible for ACL loading. Although in vivo and in vitro studies each have their strengths and limitations, together they provide valuable information regarding ACL loading patterns with different knee loads. In the following sections, we will summarize the results from biomechanical studies using these methods to examine ACL loading patterns.
Knee Muscle Forces
The ACL is loaded when an anterior directed force is applied to the tibia, and the ACL serves as the primary restraint to anterior tibiofemoral shear forces.49–51 In recent studies49,50 using a robotic arm with a 6–degrees-of-freedom force transducer, the authors measured ACL tensile force during application of an anterior shear force to the tibia at various knee flexion angles. When the knee was near full extension (less than 30°), ACL tensile forces were of similar magnitude as the applied anterior shear force.49,50 However, when the knee was flexed more than 60°, ACL tensile forces due to the applied anterior shear force were smaller than those measured when the knee was flexed less than 30°.49,50 For example, Sakane et al50 reported ACL tensile force when 110 N of anterior shear force was applied to the tibia at various knee flexion angles. More than 90 N of ACL tensile force was observed at knee flexion angles of less than 30°, whereas only 70 N and 59 N of ACL tensile force were observed at 60° and 90° of knee flexion angle, respectively. These results are in agreement with those of Butler et al,51 who showed that the ACL is the major restraint against anterior shear forces applied to the tibia relative to the femur, especially with shallow knee flexion angles, indicating that the ACL is more vulnerable to excessive anterior loads near full knee extension.50 Because the anterior force on the tibia is influenced by knee muscle forces such as quadriceps, hamstrings, and gastrocnemius muscle contractions, the following section will discuss the effects of these muscles on ACL loading.
Quadriceps Muscle Force
Table 2 provides a summary of in vivo and in vitro findings regarding ACL loading responses due to quadriceps muscle force or produced knee extensor moment at different knee flexion angles. Quadriceps muscle contraction has been considered to be one of the major forces producing anterior-directed forces on the tibia.52,53 An increase in ACL tensile force during quadriceps contractions with the knee in a shallow flexion angle can be explained by the direction of the infrapatellar tendon force vector in the sagittal plane. Nunley et al54 reported that the angle between the infrapatellar tendon and the longitudinal axis of the tibia is largest during shallow knee flexion angles. These results were in agreement with those of Isaac et al.53 Therefore, the anterior shear force component becomes larger near full knee extension compared with deeper knee flexion angles (ie, more than 70°), in which the direction of the shear force actually moves posteriorly. Thus, vigorous, unopposed quadriceps contractions near full knee extension can theoretically increase ACL tensile forces and may be harmful to the ACL.
Table 1b.
Activities Observed or Reported at the Time of Noncontact Anterior Cruciate Ligament Injuries
This theory is supported by authors of in vitro studies, who found that isolated quadriceps contractions increased ACL strain or tensile force during shallow knee flexion angles (ie, less than 40° to approximately 60° of knee flexion) and reduced ACL strain or tensile force when the knee was flexed to more than 45° to 60°.14,18,19,21–25 These findings are also consistent with those of in vivo studies by authors examining ACL strain during open kinetic chain knee extension exercises.15,16,20 During isometric quadriceps contractions and the eccentric phase of knee extension exercise, Beynnon et al15,16 and Fleming et al20 found that ACL strain increased during shallow knee flexion angles but not at knee flexion angles of greater than 40° to approximately 60° or at 90°.
Although these results indicate that excessive quadriceps force may increase the risk of ACL injuries, the authors did not directly examine ACL injury. We found only 1 group that directly examined this possibility. DeMorat et al17 examined the effect of a 4500-N quadriceps contraction force on the ACL in cadavers and observed that 6 of the 11 knee specimens experienced partial or complete ACL ruptures. However, DeMorat et al17 observed not only anterior tibial displacement but also knee internal rotation and knee valgus motions with application of the quadriceps load. Hence, quadriceps contractions appeared to produce some degree of knee internal rotation and valgus moment to the tibia in addition to anterior tibial translation, thus affecting ACL loading in more than one plane of motion.
Hamstrings Muscle Force
Table 3 provides a summary of in vivo and in vitro findings regarding the effects of hamstrings muscle cocontraction forces with quadriceps muscle force or anterior shear force to the tibia on ACL loading responses at different knee flexion angles. Hamstrings contractions are thought to produce posterior shear forces and, along with the quadriceps, compressive forces at the tibiofemoral joint, thereby increasing knee stability.55,56 Anterior cruciate ligament tensile force due to quadriceps contractions decreased with hamstrings cocontractions.18,21–23,25 The amount of reduction in ACL tensile force was especially notable as the knee flexion angle increased.18,21–23,25 From these results, we can determine that the protective function of the hamstrings muscle with regard to the ACL may decrease at extended knee angles. Thus, the notion that the application of excessive quadriceps contraction forces or anterior shear forces to the tibia near full knee extension places the ACL at greater vulnerability for strain and tension is further supported.
Gastrocnemius Muscle Force
Table 4 describes in vivo and in vitro ACL loading responses due to gastrocnemius muscle force at different knee flexion angles. Gastrocnemius muscle force has been hypothesized to create an anterior shear force on the tibia, resulting in an increase in ACL loading using a computer simulation model.57 This hypothesis was tested by 2 groups that examined the effects of gastrocnemius muscle force on ACL strain in vivo27 and in vitro,19 and the results were contradictory.
Dürselen et al19 inserted 2 screws in the posterior aspects of the lateral and medial femoral epicondyles. They attached a wire to the screws and pulled to simulate gastrocnemius contraction force (actual force not specified). The gastrocnemius forces had no effect on the ACL strain at any knee flexion angle (full extension to 110°) compared with ACL strain values due to passive knee flexion. Conversely, Fleming et al27 showed that gastrocnemius forces increased ACL strain in vivo. They electrically stimulated the gastrocnemius muscle to produce at least a 15-Nm ankle plantar-flexion moment and assessed the amount of ACL strain. The ACL was strained with gastrocnemius contractions as compared with no muscle contraction between 5° and 30° of knee flexion. However, the amount of ACL strain due to the gastrocnemius depended on knee flexion angle, as the ACL strain value reached about 4% at 15° of knee flexion and was close to zero or unstrained at above 30° of knee flexion.
Methodologic differences may explain these contradictory results (eg, using a wire to simulate the muscle force in vitro19 versus stimulating the gastrocnemius muscle in vivo33). When the authors46 of a computer simulation study assessed the effects of gastrocnemius force during a drop landing, they found it had minimal effect on ACL loading, as it produced only a small amount of anterior shear force to the tibia. Hence, the available data are insufficient to conclusively determine whether a gastrocnemius force is important for ACL loading and injury. More studies are needed to critically answer these questions.
In summary, excessive quadriceps contraction forces near full knee extension may increase ACL loading and possibly the risk of ACL injury. This factor may be of particular concern during deceleration maneuvers, when the weight is back on the heel. Athletes who sustain an ACL injury have often reported that the involved leg was positioned in front of the upper body, with the upper body leaning backward during a sudden deceleration motion from forward running.7 In this position, the individual must produce a substantial quadriceps force to decelerate the limb. Further, the hip is extended (secondary to the body leaning backward), which places the hamstrings in a shortened position and, therefore, presumably lends little stability to the knee during this sudden deceleration motion. As a result, high anterior tibial shear forces may be experienced, increasing ACL tensile force and injury risk. Given evidence that the quadriceps contraction force may also produce moments in the frontal and transverse planes (ie, knee internal rotation and valgus rotation moments),17,21,58 we need to examine ACL loading in multiple planes.
Combined Knee Loading-Hyperextension Loading
Table 5 provides a summary of in vivo and in vitro findings regarding the effects of ACL loading responses due to combined knee loading. Hyperextension may be the most obvious mechanism of noncontact ACL injury, as the motion primarily occurs in the sagittal plane and has been observed in such injuries.7,10 Previous authors who measured ACL tensile force agreed that hyperextension of the knee loads the ACL. Markolf et al24 showed that even during passive knee flexion-extension motions, ACL tensile forces increase as the knee approaches full extension and peak with knee hyperextension. When knee hyperextension was combined with knee internal or external rotation moments, ACL tensile forces were more than double the forces recorded for knee internal or external rotation moments with the knee flexed to 20° or more.23,24 Because hyperextension with or without transverse plane loading dramatically increases ACL tensile force, it may be said that excessive hyperextension loading increases the risk of damaging the ACL.
Frontal-Plane and Transverse-Plane Loading
Most ACL injuries happen in weight bearing during deceleration motions that are assumed to be accompanied by a quadriceps contraction.7–13 Therefore, ACL loading patterns with the application of external loads in the frontal and transverse planes were primarily considered when combined with quadriceps force or weight-bearing loads. The effects of combined anterior shear force and frontal-plane or transverse-plane loadings were also considered, because anterior shear force is closely associated with quadriceps force, as stated above. Further, ACL loading patterns due to combined frontal-plane (ie, valgus-varus) and transverse-plane (knee internal-external rotation) loads were also considered, as they are also frequently observed motions during noncontact ACL injuries.7–9,11,12
Based on the results of in vivo and in vitro studies, applying a knee internal rotation moment increases ACL loading more than an applied knee external rotation moment when combined with a quadriceps force14,23,29 or anterior shear force.26,28 Approximately twice the ACL tensile forces have been observed in cadaveric knees with a combined quadriceps force and knee internal rotation moment compared with a combined quadriceps force with and without a knee external rotation moment.23 Although ACL strain was highest during a combined quadriceps force and knee internal rotation moment (up to approximately 2% higher than the strain values with the application of only quadriceps force), ACL strain actually reduced during a combined quadriceps force and knee external rotation moment.14 In both cases, higher ACL strain and tensile forces were observed near full knee extension (0° and 15°).14,23 Similarly, authors of an in vivo study29 demonstrated larger ACL strain values during weight bearing at 20° of knee flexion angle with the application of 9 Nm of knee internal and external rotation moments as compared with the strain values due to weight bearing alone. Although no statistical analysis was conducted, the incremental increase in ACL strain due to the application of a knee internal rotation moment appeared to be appreciably higher than that due to an external rotation moment during weight bearing.29 These results imply that when the knee experiences an excessive knee internal rotation moment along with excessive quadriceps force during weight bearing, substantial strain or tensile forces may be imposed on the ACL, potentially increasing ACL injury risk.
Applications of a valgus or varus moment with a quadriceps contraction, weight bearing, or anterior shear force have also been reported to increase ACL strain in vivo and in vitro.14,26,28,29 In a cadaver study, ACL strain values were higher when a quadriceps force was combined with a 15-Nm valgus or varus moment during knee flexion angles greater than approximately 40°.14 However, with knee flexion angles of less than 40°, ACL strain due to these combined loading patterns was slightly lower (approximately 1%) than the strain due to quadriceps force alone. Further, during weight bearing in vivo, the application of 10-Nm valgus-varus moments did not change the strain value when compared with the strain due to weight bearing alone.29 These studies indicate that during weight-bearing activities, when quadriceps muscle activity becomes dominant, a valgus or varus moment may not dramatically influence ACL strain.
However, Berns et al28 and Markolf et al26 showed that when frontal-plane knee loadings were combined with anterior shear force, ACL tensile force was greater than that due to anterior shear force alone. At this point, the reason for such a discrepancy in the effects of frontal-plane knee loading with quadriceps, weight bearing, or anterior shear force is unknown. Nevertheless, these studies showed a possible increase in ACL loading if knee valgus or varus loading is combined with anterior shear force to the tibia, for example, due to quadriceps contractions.
Although high valgus loading has been shown to damage or load the ACL secondary to medial collateral ligament injury,59,60 varus-valgus loading rarely occurs in isolation, and it is possible that ACL loading patterns may be quite different when varus-valgus knee loads are combined with transverse-plane knee loads.
A limited number of groups have examined the effect of combined frontal-plane and transverse-plane knee loading on ACL tensile forces.19,30–32 Such studies are relevant because these motions are often observed together at the time of injury.9,11,61 Authors who used a robotic arm to examine ACL tensile forces showed that combined loading of valgus with either a knee internal rotation or external rotation moment increased ACL tensile force.30–32 However, ACL tensile force was almost 2 times greater with combined valgus and knee internal rotation loads than with combined valgus and knee external rotation loads at 15° of knee flexion and was greater than an isolated valgus load at 30° of knee flexion.31 Dürselen et al19 agreed with these results in that combined knee loading of knee valgus and knee external rotation motion did not increase ACL strain as compared with passive knee flexion. These studies provide evidence that when excessive valgus and knee internal rotation loads are combined near full knee extension, the ACL may be at greater risk for strain and injury. This risk appears to be greater when these moments are experienced in weight bearing augmented by excessive quadriceps contraction.
Based on the collective findings of these studies, Ireland's47 description of ACL injury as one that is frequently due to combined excessive valgus and knee external rotation is somewhat unclear. However, knee external rotation cannot be ruled out as a mechanism for ACL injury because of the potential for ACL impingement against the femoral intercondylar notch.62 Fung and Zhang62 assessed ACL strain behavior using a 3-dimensional simulation model. Two human knee specimens with obvious ACL impingement were chosen for the experiment. The ACL and the bony surfaces of the tibia and femur were digitized, and the ACL was partitioned into anteromedial, posterolateral, and intermediate bands. They then simulated combination knee motions of either external rotation and valgus or internal rotation and varus. The combination of 8° of valgus and 5° of knee external rotation stretched all 3 bands of the ACL as a result of impingement against the intercondylar notch. Further increases in knee external rotation (12°) resulted in more ACL strain (approximately 2% in the anteromedial band and 1% in the intermediate and posterolateral bands). Conversely, the ACL never contacted the intercondylar notch with combined knee internal rotation and varus loading. Because ACL strain values due to the combined knee loading (knee internal rotation and varus) were not reported in this study, which combined knee loadings created the greatest ACL strain is unknown. Also, because they did not report strain values due to the combination of knee internal rotation and valgus loading, comparing their strain values with those of other studies is difficult. Nonetheless, Fung and Zhang62 stated that knee external rotation and valgus may also increase the risk of ACL injury due to impingement.
As we can see from these results, the combination of valgus with both knee internal rotation and external rotation may offer one of the more compelling causes of ACL injury. Although valgus and knee external rotation motion is commonly believed to be an ACL injury mechanism based on retrospective reports,9–11 biomechanical studies demonstrate the importance of also examining knee internal rotation motion during dynamic tasks.14,17,21,23,29–32,63,64 Speer et al64 found that 93% of patients with ACL ruptures (50 out of 54) showed evidence of posterolateral injuries to the proximal tibia and, in particular, injuries to the posterior horn of the lateral meniscus. The authors concluded that this finding reflected a violent anterior subluxation of the lateral tibial plateau as the ACL was ruptured in knee flexion, and they hypothesized the mechanism of injury to be an “index pivot shift event.”
Closed Kinetic Chain Exercises
Anterior cruciate ligament injuries typically occur when the foot makes contact with the ground, such as during sudden deceleration, landing, or jumping.7–10 Although few authors have examined ACL loading during closed kinetic chain exercise, these investigations are particularly relevant because these activities share movement and muscle activation patterns in weight bearing. Therefore, examining ACL loading patterns during weight-bearing activities provides additional insights into the mechanisms of ACL injury (Table 6).
Anterior cruciate ligament strain patterns during a sudden deceleration task have been assessed in only 1 case study,33 whereas the authors of 4 in vitro studies examined ACL loading patterns during landing using cadaveric knees by simulating the muscle and impact forces during landing.36–39 Cerulli et al33 examined ACL strain in vivo during a forward hop and landing task. A small strain gauge was implanted on the anteromedial part of the ACL in the left leg, and the participant performed 3 trials of single-leg forward hop (jump with right leg and land with only left leg). The peak strain values were recorded immediately after the foot contact, at approximately the same time that peak ground reaction forces occurred. Average strain values were 2% during a Lachman test and 5.5% during the jump-stop task. Thus, the ACL may experience larger loads during a sudden deceleration task, especially immediately after foot contact. The findings from in vitro studies simulating knee loading during landing were similar to those of Cerulli et al33 in that the ACL was strained during landing,36–39 with peak strain occurring shortly (approximately 40 milliseconds) after touchdown.36–38 Further, Withrow et al38 demonstrated that ACL strain during landing increased with valgus loading during landing impact as compared with no valgus loading.
The amount of ACL strain during exercises that are often used for ACL reconstruction rehabilitation has also been examined. Three groups16,34,35 examined the ACL strain patterns during several closed kinetic chain exercises. Heijne et al35 investigated the ACL strain pattern during step-up and step-down motions, lunges, and 1-legged sit to stand and observed average peak strain values of 1.8% to 2.8%, with no difference in strain values between exercises. The ACL strain values at 30° of knee flexion were larger than those at 50° and 70° of knee flexion. Similarly, Beynnon et al16 reported that ACL strain values (approximately 4%) were the largest at 10° of knee flexion during squatting, with and without an applied resistance to the motion (created by a rubber tube). The ACL strain values decreased as knee flexion angle increased, with ACL strain near zero at 60° of knee flexion. Fleming et al34 also agreed with these results in observing higher ACL strain in near-full extension during a stair-climbing task.
These studies of nonballistic closed chain exercises once again demonstrate that ACL strain values were higher during shallow knee flexion angles, further validating retrospective observational studies that ACL injuries tend to happen near full knee extension.7,8,10,11 Comparing the mean strain values reported by Beynnon et al16 and Cerulli et al33 indicates that the amount of strain may be higher during more ballistic types of exercise, such as sudden deceleration motions. This comparison may be appropriate because the strain values observed during a Lachman test were similar in both studies (approximately 2% of ACL strain).16,33 Further, during such ballistic deceleration tasks, receiving large valgus loading may further increase ACL loading,38 supporting valgus loading as part of noncontact ACL injury mechanisms.7,8,9,11
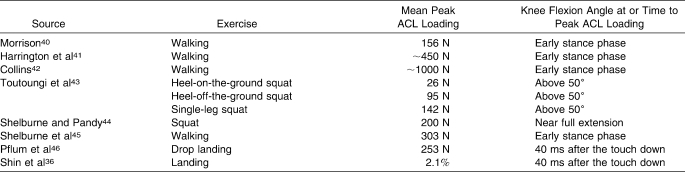
Anterior Cruciate Ligament Loading Estimated by Computer Simulations
Computer simulations have also been used to predict ACL loading during closed kinetic motions (Table 7).36,40–45,54 The authors of the studies referenced in Table 7 directly calculated the amount of ACL tensile force based on predicted kinetic and kinematic variables accounting for such factors as individual muscle forces, anthropometric properties, and other soft tissue supports. Although this approach is useful to predict the amount of ACL tensile force during actual dynamic motions, the extent to which the calculated values (eg, muscle force, ligamentous force) from these studies reflect actual values during corresponding dynamic human motions is unknown. However, these findings add information in our effort to understand the patterns of ACL loading behavior due to dynamic motion and muscle contractions.
Table 7.
Anterior Cruciate Ligament (ACL) Loading Responses Due to Closed Kinetic Chain Exercise in Computer Simulation Models
A strength of computer simulation studies is that they make it possible to test the function of individual structures while controlling for all other structures.65 For example, it is difficult to control the activation of involved muscles in vivo, but computer simulations can demonstrate the effects of different muscle activations on ACL loading patterns during exercise. Thus, computer simulations allow us to test various loading conditions.
The ACL loading patterns estimated by computer simulations were generally in agreement with those noted in the previously mentioned in vivo studies (Table 6).16,34,35 Shelburne and Pandy44 demonstrated that the ACL was loaded only from full extension to 10° of knee flexion. The findings of simulation studies examining ACL loading patterns during walking also agreed with these results in that peak ACL strain occurred in early stance phase after the heel strike.36,40–42,45,54 These results were also in agreement with those of the previously discussed in vivo studies examining ACL loading during closed kinetic chain exercises.16,34,35 Further, Shelburne and Pandy44 showed the importance of hamstrings activation in reducing ACL loading during nonballistic squatting motions, further emphasizing hamstrings cocontraction during weight bearing. Although the study examined static position in 2 dimensions, more complex factors should be considered in more ballistic dynamic motions. During such dynamic motions, ACL loading results from multiple factors, including ground reaction forces, joint reaction forces, muscle forces, and external moments in multiple planes.54
Pflum et al46 and Shin et al36 examined ACL loading patterns during landing based on data from 1 participant46 and a cadaveric knee. Their models showed a net posterior shear force at the proximal tibia shortly after landing because of the large, posteriorly directed ground reaction force at the very beginning of the landing. Because both models experienced net posteriorly directed shear force at the proximal tibia at the start of deceleration, the ACL was unstrained. Although ACL loading was not directly calculated, the computer simulation study by McLean et al66 also demonstrated that net sagittal-plane force at the proximal tibia was directed posteriorly in the beginning of the stance phase of a sidestep crossover maneuver as a result of the large, posteriorly directed ground reaction force. Thus, even with a quadriceps muscle force, the authors stated that the net anterior shear force at the proximal tibia would never be large enough to rupture the ACL. Rather, because they observed enough external knee internal rotation and valgus knee loading to damage the ACL in their perturbation simulations, they concluded that these transverse-plane and frontal-plane loadings would be more important for ACL injury.66
These results highlight a controversy in the literature as to whether a posteriorly directed ground reaction force actually pushes the tibia back, resulting in the ACL being unloaded,67 or increases the knee extensor (ie, quadriceps) contraction demand, thereby increasing the anterior shear force at the proximal tibia and loading the ACL during such deceleration tasks.68 An inconsistency in the results of ACL loading patterns during closed kinetic chain exercise has been noted. For example, although authors33 of an in vivo study showed that the ACL was constantly strained during rapid deceleration after a forward jump that should cause a posteriorly directed ground reaction force, no strain on the ACL was observed immediately after the touch down in simulated landing studies.36–38,46 Whether the amount of anterior shear force due to the quadriceps muscle force would become large enough to injure the ACL during such deceleration activities is not clear at this point because of the limited number of available research models.61,67–70 Further studies with a variety of research models are needed to clarify this issue.
These computer simulation studies, however, highlight the concept that the sum of all the forces acting on the knee determines the ACL loading during dynamic motions. In other words, ACL loading cannot be explained by only the quadriceps force or joint reaction force from inverse dynamics. Mathematical models such as those described are not perfect, as it is not possible to obtain perfect data about all the tissue properties, muscle activation patterns, and forces produced by individual muscles. Thus, the extent to which results from these computer simulation models reflect the real human ACL is unknown. However, the results from these models reinforce that ACL loading patterns during dynamic motions change depending on the involvement of many factors. Although a controversy still exists, in general it appears that quadriceps and hamstrings muscle contractions significantly influence the amount of ACL loading, as shown in in vivo and in vitro biomechanical studies.*
Conclusions
Anterior cruciate ligament injuries often happen when an individual attempts to decelerate the body from a jump or forward running while the knee is in a shallow flexion angle.7,9–11,13 At the time of injury, combined motions such as knee valgus and knee internal-external rotation are often noted.7,9–11 From these observations, we can expect that the knee is loaded in multiple planes of motion.
The ACL has been widely known to be loaded with anterior tibial shear forces.49,50 Unopposed quadriceps muscle forces produce anterior shear forces,53,54 possibly damaging the ACL, especially near full extension.17 On the other hand, hamstrings cocontraction forces are protective to the ACL, increasing knee stability while the quadriceps are contracting.18,21–23,25 An ACL injury often occurs when the body is positioned with the weight back on the heel, which may increase the quadriceps contraction force and reduce the efficacy of the hamstrings. Thus, controlling body position and thigh muscle activations during sudden deceleration and landing motions appears to be an important ACL prevention strategy.
Applying moments to the knee in the frontal and transverse planes may also strain the ACL, particularly when they are accompanied by a quadriceps contraction or weight bearing.14,23,29 The results of both in vivo and in vitro studies showed that the application of knee internal rotation moments increased ACL loading more than the application of knee external rotation moments when combined with a quadriceps force or weight bearing.14,23,29 Combined valgus and knee internal rotation moments also produced higher ACL tensile forces than did combined valgus and knee external rotation moments.31 Although knee external rotation is often described in the mechanisms for ACL injuries, the literature indicates that knee internal rotation may be an equally, if not more important, motion to protect the ACL. Further, the application of knee valgus loading during a sudden decelerating, weight-bearing task, such as landing, may also increase ACL loading.38 Hence, excessive knee internal rotation or valgus loading during sudden deceleration motion at a shallow knee flexion angle, especially with excessive quadriceps force, appears to be particularly problematic for the ACL; this subject deserves further study relative to the mechanisms that may injure the ACL.
Because a combination of knee external rotation and valgus motions may impinge the ACL against the femoral intercondylar notch62 and because these motions have been often observed during noncontact ACL injury, knee external rotation remains an important consideration for ACL injury.9,11 However, many of the authors whose work is discussed in this review question the belief that the combined motions of knee external rotation and valgus, as described by the position of no return, are always the cause of ACL injury. Moreover, the motion characterized by position of no return may actually result from ACL failure. At this point, it is not possible to definitively conclude which motions are more problematic for ACL injuries. Yet the results of studies to date demonstrate the importance of focusing not only on the combination of knee valgus and external rotation motion but also on knee internal rotation motion during dynamic motion.
Information regarding combined knee loading patterns during a sudden deceleration task remains scant. Still, our knowledge to date supports the notion that increasing the knee flexion angle during deceleration and acceleration tasks and preventing excessive quadriceps contraction while increasing hamstrings muscle cocontractions, especially at near-full knee extension, may protect the ACL. Also important is the need to protect against excessive frontal-plane and transverse-plane loads to the knee in weight bearing, particularly valgus and internal rotation loads. Information gained from this review may assist clinicians and researchers in our continued efforts to design effective injury prevention programs to reduce the risk of ACL injury.
Footnotes
Yohei Shimokochi, PhD, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Sandra J. Shultz, PhD, ATC, FNATA, FACSM, contributed to conception and design and critical revision and final approval of the article.
References
- 1.Griffin L.Y, Agel J, Albohm M.J, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Lohmander L.S, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 3.Daniel D.M, Stone M.L, Dobson B.E, Fithian D.C, Rossman D.J, Kaufman K.R. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 4.Mayr H.O, Weig T.G, Plitz W. Arthrofibrosis following ACL reconstruction: reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518–522. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 5.Hewett T.E, Lindenfeld T.N, Riccobene J.V, Noyes F.R. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 6.Mandelbaum B.R, Silvers H.J, Watanabe D.S, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 7.Boden B.P, Dean G.S, Feagin J.A, Jr, Garrett W.E., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):537–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 8.Cochrane J.L, Lloyd D.G, Buttfield A, Seward H, McGivern J. Characteristics of anterior cruciate ligament injuries in Australian football. J Sci Med Sport. 2007;10(2):96–104. doi: 10.1016/j.jsams.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Ferretti A, Papandrea P, Conteduca F, Mariani P.P. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20(2):203–207. doi: 10.1177/036354659202000219. [DOI] [PubMed] [Google Scholar]
- 10.McNair P.J, Marshall R.N, Matheson J.A. Important features associated with acute anterior cruciate ligament injury. N Z Med J. 1990;103(901):537–539. [PubMed] [Google Scholar]
- 11.Olsen O.E, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 12.Faunø P, Wulff Jakobsen B. Mechanism of anterior cruciate ligament injuries in soccer. Int J Sports Med. 2006;27(1):75–79. doi: 10.1055/s-2005-837485. [DOI] [PubMed] [Google Scholar]
- 13.Olsen O.E, Myklebust G, Engebretsen L, Holme I, Bahr R. Relationship between floor type and risk of ACL injury in team handball. Scand J Med Sci Sports. 2003;13(5):299–304. doi: 10.1034/j.1600-0838.2003.00329.x. [DOI] [PubMed] [Google Scholar]
- 14.Arms S.W, Pope M.H, Johnson R.J, Fischer R.A, Arvidsson I, Eriksson E. The biomechanics of anterior cruciate ligament rehabilitation and reconstruction. Am J Sports Med. 1984;12(1):8–18. doi: 10.1177/036354658401200102. [DOI] [PubMed] [Google Scholar]
- 15.Beynnon B.D, Fleming B.C, Johnson R.J, Nichols C.E, Renstrom P.A, Pope M.H. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23(1):24–34. doi: 10.1177/036354659502300105. [DOI] [PubMed] [Google Scholar]
- 16.Beynnon B.D, Johnson R.J, Fleming B.C, Stankewich C.J, Renstrom P.A, Nichols C.E. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension: a comparison of an open and a closed kinetic chain exercise. Am J Sports Med. 1997;25(6):823–829. doi: 10.1177/036354659702500616. [DOI] [PubMed] [Google Scholar]
- 17.DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32(2):477–483. doi: 10.1177/0363546503258928. [DOI] [PubMed] [Google Scholar]
- 18.Draganich L.F, Vahey J.W. An in vitro study of anterior cruciate ligament strain induced by quadriceps and hamstring forces. J Orthop Res. 1990;8(1):57–63. doi: 10.1002/jor.1100080107. [DOI] [PubMed] [Google Scholar]
- 19.Dürselen L, Claes L, Kiefer H. The influence of muscle forces and external loads on cruciate ligament strain. Am J Sports Med. 1995;23(1):129–136. doi: 10.1177/036354659502300122. [DOI] [PubMed] [Google Scholar]
- 20.Fleming B.C, Ohlen G, Renstrom P.A, Peura G.D, Beynnon B.D, Badger G.J. The effects of compressive load and knee joint torque on peak anterior cruciate ligament strains. Am J Sports Med. 2003;31(5):701–707. doi: 10.1177/03635465030310051101. [DOI] [PubMed] [Google Scholar]
- 21.Li G, Rudy T.W, Sakane M, Kanamori A, Ma C.B, Woo S.L. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32(4):395–400. doi: 10.1016/s0021-9290(98)00181-x. [DOI] [PubMed] [Google Scholar]
- 22.Li G, Zayontz S, Most E, DeFrate L.E, Suggs J.F, Rubash H.E. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22(2):293–297. doi: 10.1016/S0736-0266(03)00179-7. [DOI] [PubMed] [Google Scholar]
- 23.Markolf K.L, O'Neil G, Jackson S.R, McAllister D.R. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32(5):1144–1149. doi: 10.1177/0363546503262198. [DOI] [PubMed] [Google Scholar]
- 24.Markolf K.L, Gorek J.F, Kabo J.M, Shapiro M.S. Direct measurement of resultant forces in the anterior cruciate ligament: an in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–567. [PubMed] [Google Scholar]
- 25.Renstrom P.A, Arms S.W, Stanwyck T.S, Johnson R.J, Pope M.H. Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med. 1986;14(1):83–87. doi: 10.1177/036354658601400114. [DOI] [PubMed] [Google Scholar]
- 26.Markolf K.L, Burchfield D.M, Shapiro M.M, Shepard M.F, Finerman G.A, Slauterbeck J.L. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 27.Fleming B.C, Renstrom P.A, Ohlen G, et al. The gastrocnemius muscle is an antagonist of the anterior cruciate ligament. J Orthop Res. 2001;19(6):1178–1184. doi: 10.1016/S0736-0266(01)00057-2. [DOI] [PubMed] [Google Scholar]
- 28.Berns G.S, Hull M.L, Patterson H.A. Strain in the anteromedial bundle of the anterior cruciate ligament under combination loading. J Orthop Res. 1992;10(2):167–176. doi: 10.1002/jor.1100100203. [DOI] [PubMed] [Google Scholar]
- 29.Fleming B.C, Renstrom P.A, Beynnon B.D, et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34(2):163–170. doi: 10.1016/s0021-9290(00)00154-8. [DOI] [PubMed] [Google Scholar]
- 30.Gabriel M.T, Wong E.K, Woo S.L, Yagi M, Debski R.E. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 31.Kanamori A, Woo S.L, Ma C.B, et al. The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadaveric study using robotic technology. Arthroscopy. 2000;16(6):633–639. doi: 10.1053/jars.2000.7682. [DOI] [PubMed] [Google Scholar]
- 32.Kanamori A, Zeminski J, Rudy T.W, Li G, Fu F.H, Woo S.L. The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy. 2002;18(4):394–398. doi: 10.1053/jars.2002.30638. [DOI] [PubMed] [Google Scholar]
- 33.Cerulli G, Benoit D.L, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):307–311. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 34.Fleming B.C, Beynnon B.D, Renstrom P.A, et al. The strain behavior of the anterior cruciate ligament during stair climbing: an in vivo study. Arthroscopy. 1999;15(2):185–191. doi: 10.1053/ar.1999.v15.015018. [DOI] [PubMed] [Google Scholar]
- 35.Heijne A, Fleming B.C, Renstrom P.A, Peura G.D, Beynnon B.D, Werner S. Strain on the anterior cruciate ligament during closed kinetic chain exercises. Med Sci Sports Exerc. 2004;36(6):935–941. doi: 10.1249/01.mss.0000128185.55587.a3. [DOI] [PubMed] [Google Scholar]
- 36.Shin C.S, Chaudhari A.M, Andriacchi T.P. The influence of deceleration forces on ACL strain during single-leg landing: a simulation study. J Biomech. 2007;40(5):1145–1152. doi: 10.1016/j.jbiomech.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Withrow T.J, Huston L.J, Wojtys E.M, Ashton-Miller J.A. The relationship between quadriceps muscle force, knee flexion, and anterior cruciate ligament strain in an in vitro simulated jump landing. Am J Sports Med. 2006;34(2):269–274. doi: 10.1177/0363546505280906. [DOI] [PubMed] [Google Scholar]
- 38.Withrow T.J, Huston L.J, Wojtys E.M, Ashton-Miller J.A. The effect of an impulsive knee valgus moment on in vitro relative ACL strain during a simulated jump landing. Clin Biomech (Bristol, Avon) 2006;21(9):977–983. doi: 10.1016/j.clinbiomech.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Weinhold P.S, Stewart J.D, Liu H.Y, Lin C.F, Garrett W.E, Yu B. The influence of gender-specific loading patterns of the stop-jump task on anterior cruciate ligament strain. Injury. 2007;38(8):973–978. doi: 10.1016/j.injury.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 40.Morrison J.B. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3(1):51–61. doi: 10.1016/0021-9290(70)90050-3. [DOI] [PubMed] [Google Scholar]
- 41.Harrington I.J. A bioengineering analysis of force actions at the knee in normal and pathological gait. Biomed Eng. 1976;11(5):167–172. [PubMed] [Google Scholar]
- 42.Collins J.J. The redundant nature of locomotor optimization laws. J Biomech. 1995;28(3):251–267. doi: 10.1016/0021-9290(94)00072-c. [DOI] [PubMed] [Google Scholar]
- 43.Toutoungi D.E, Lu T.W, Leardini A, Catani F, O'Connor J.J. Cruciate ligament forces in the human knee during rehabilitation exercises. Clin Biomech (Bristol, Avon) 2000;15(3):176–187. doi: 10.1016/s0268-0033(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 44.Shelburne K.B, Pandy M.G. Determinants of cruciate-ligament loading during rehabilitation exercise. Clin Biomech (Bristol, Avon) 1998;13(6):403–413. doi: 10.1016/s0268-0033(98)00094-1. [DOI] [PubMed] [Google Scholar]
- 45.Shelburne K.B, Torry M.R, Pandy M.G. Muscle, ligament, and joint-contact forces at the knee during walking. Med Sci Sports Exerc. 2005;37(11):1948–1956. doi: 10.1249/01.mss.0000180404.86078.ff. [DOI] [PubMed] [Google Scholar]
- 46.Pflum M.A, Shelburne K.B, Torry M.R, Decker M.J, Pandy M.G. Model prediction of anterior cruciate ligament force during drop-landings. Med Sci Sports Exerc. 2004;36(11):1949–1958. doi: 10.1249/01.mss.0000145467.79916.46. [DOI] [PubMed] [Google Scholar]
- 47.Ireland M.L. Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train. 1999;34(2):150–154. [PMC free article] [PubMed] [Google Scholar]
- 48.Venes D, editor. Tabler's Cyclopedic Medical Dictionary. 19th ed. Philadelphia, PA: FA Davis; 2001. [Google Scholar]
- 49.Woo S.L, Fox R.J, Sakane M, Livesay G.A, Rudy T.W, Fu F.H. Biomechanics of the ACL: measurements of in situ force in the ACL and knee kinematics. Knee. 1998;5(4):267–288. [Google Scholar]
- 50.Sakane M, Livesay G.A, Fox R.J, Rudy T.W, Runco T.J, Woo S.L. Relative contribution of the ACL, MCL, and bony contact to the anterior stability of the knee. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):93–97. doi: 10.1007/s001670050128. [DOI] [PubMed] [Google Scholar]
- 51.Butler D.L, Noyes F.R, Grood E.S. Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–270. [PubMed] [Google Scholar]
- 52.Pandy M.G, Shelburne K.B. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30(10):1015–1024. doi: 10.1016/s0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 53.Isaac D.L, Beard D.J, Price A.J, Rees J, Murray D.W, Dodd C.A. In-vivo sagittal plane knee kinematics: ACL intact, deficient and reconstructed knees. Knee. 2005;12(1):25–31. doi: 10.1016/j.knee.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 54.Nunley R.M, Wright D, Renner J.B, Yu B, Garrett W.E., Jr Gender comparison of patella tendon tibial shaft angle with weight bearing. Res Sports Med. 2003;11(3):173–185. [Google Scholar]
- 55.Baratta R, Solomonow M, Zhou B.H, Letson D, Chuinard R, D'Ambrosia R. Muscle coactivation: the role of the antagonist musculature in maintaining knee stability. Am J Sports Med. 1988;16(2):113–122. doi: 10.1177/036354658801600205. [DOI] [PubMed] [Google Scholar]
- 56.Solomonow M, Baratta R, Zhou B.H, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. Am J Sports Med. 1987;15(3):207–213. doi: 10.1177/036354658701500302. [DOI] [PubMed] [Google Scholar]
- 57.O'Connor J.J. Can muscle co-contraction protect knee ligaments after injury or repair. J Bone Joint Surg Br. 1993;75(1):41–48. doi: 10.1302/0301-620X.75B1.8421032. [DOI] [PubMed] [Google Scholar]
- 58.Hirokawa S, Solomonow M, Lu Y, Lou Z.P, D'Ambrosia R. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20(3):299–306. doi: 10.1177/036354659202000311. [DOI] [PubMed] [Google Scholar]
- 59.Mazzocca A.D, Nissen C.W, Geary M, Adams D.J. Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg. 2003;16(3):148–151. [PubMed] [Google Scholar]
- 60.Bendjaballah M.Z, Shirazi-Adl A, Zukor D.J. Finite element analysis of human knee joint in varus-valgus. Clin Biomech (Bristol, Avon) 1997;12(3):139–148. doi: 10.1016/s0268-0033(97)00072-7. [DOI] [PubMed] [Google Scholar]
- 61.Chaudhari A.M, Andriacchi T.P. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks [letter] Am J Sports Med. 2006;34(2):312. doi: 10.1177/0363546505283274. [DOI] [PubMed] [Google Scholar]
- 62.Fung D.T, Zhang L.Q. Modeling of ACL impingement against the intercondylar notch. Clin Biomech (Bristol, Avon) 2003;18(10):933–941. doi: 10.1016/s0268-0033(03)00174-8. [DOI] [PubMed] [Google Scholar]
- 63.Fukuda Y, Woo S.L, Loh J.C, et al. A quantitative analysis of valgus torque on the ACL: a human cadaveric study. J Orthop Res. 2003;21(6):1107–1112. doi: 10.1016/S0736-0266(03)00084-6. [DOI] [PubMed] [Google Scholar]
- 64.Speer K.P, Spritzer C.E, Bassett FH I.I.I, Feagin J.A, Jr, Garrett W.E., Jr Osseous injury associated with acute tears of the anterior cruciate ligament. Am J Sports Med. 1992;20(4):382–389. doi: 10.1177/036354659202000403. [DOI] [PubMed] [Google Scholar]
- 65.Gerritsen K.G, van den Bogert A.J, Nigg B.M. Direct dynamics simulation of the impact phase in heel-toe running. J Biomech. 1995;28(6):661–668. doi: 10.1016/0021-9290(94)00127-p. [DOI] [PubMed] [Google Scholar]
- 66.McLean S.G, Huang X, Su A, van den Bogert A.J. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon) 2004;19(8):828–838. doi: 10.1016/j.clinbiomech.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 67.van den Bogert A.J, McLean S.G. Effect of fatigue on knee kinetics and kinematics in stop jump tasks [letter] Am J Sports Med. 2006;34(2):312–313. doi: 10.1177/0363546505283276. [DOI] [PubMed] [Google Scholar]
- 68.Yu B, Chappell J.J, Garrett W.E., Jr Effect of fatigue on knee kinetics and kinematics in stop-jump tasks [letter] Am J Sports Med. 2006;34(2):313–315. [Google Scholar]
- 69.McLean S.G, Andrish J.T, van den Bogert A.J. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury [letter] Am J Sports Med. 2005;33(7):1106. doi: 10.1177/0363546505278247. [DOI] [PubMed] [Google Scholar]
- 70.Garrett W.E, Jr, Yu B. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury [letter] Am J Sports Med. 2005;33(7):1106–1107. doi: 10.1177/0363546505278247. [DOI] [PubMed] [Google Scholar]