Abstract
Objective:
To present the recommendations made by the Appropriate Medical Care for Secondary School-Aged Athletes Task Force and to summarize the subsequent monograph developed around 11 consensus points.
Data Sources:
The MEDLINE, CINAHL, and SportDiscus databases were searched for relevant literature regarding secondary school-aged athletes; health care administration; preparticipation physical examination; facilities; athletic equipment; emergency action planning; environmental conditions; recognition, evaluation, and treatment of injuries; rehabilitation and reconditioning; psychosocial consultation; nutrition; and prevention strategies.
Conclusions and Recommendations:
Organizations that sponsor athletic programs for secondary school-aged athletes should establish an athletic health care team to ensure that appropriate medical care is provided to all participants. The 11 consensus points provide a framework—one that is supported by the medical literature and case law—for the development of an athletic health care team and for assigning responsibilities to the team, administrators, and staff members of institutions sponsoring secondary school and club-level athletic programs.
Keywords: safety, high schools, adolescents, athletic injuries
Participation by secondary school-aged adolescents in sports, recreation, and exercise is widespread. In 2005, more than 7 000 000 high school students were participating in interscholastic athletics in the United States.1 Participation in co-curricular activities, including interscholastic athletics, benefits student-athletes by serving as an extension of a good education program, teaching valuable lessons for practical situations, and fostering success in later life.2 However, many of these activities involve the risk of injury. As a result, approximately 715 000 sport-related and recreation-related injuries occur in US school settings each year.3 Specific to the secondary school-aged athlete, Powell and Barber-Foss4 reported 23 566 reportable injuries over a 3-year study period in 10 interscholastic sports. These injuries resulted in approximately 6000 athletes sustaining an injury at least once each year, with 26.5% of the reportable injuries resulting in a time loss of greater than 7 days.4
Developing a comprehensive approach to injury control strategies for athletics is difficult. To begin to establish this direction, in 2002 the National Athletic Trainers' Association (NATA) created an interassociation task force (Appendix A) to develop recommendations and guidelines for appropriate medical care for adolescents competing in school and club-level sports. The Appropriate Medical Care for Secondary School-Aged Athletes Task Force (AMCSSAA) comprised experts from 17 school, health care, and medical associations who all shared the same goal: ensuring that young athletes receive consistent and adequate medical care while participating in practices and games. The committee included individuals representing certified athletic trainers, physicians, other health care professionals, administrators, and school principals.5 This effort addressed more than basic emergency care during sport participation; it involved virtually all aspects of prevention and activities of ongoing daily athletic health care. The recommendations are intended for use by the sponsoring organizations of athletic programs and the athletic health care teams (AHCTs) they establish, in consultation with administrators, coaches, parents, and participants. By approaching the issue of athletic injuries in a comprehensive way, we develop a better sense of where the problems lie and what can be done to eliminate or reduce them.
The group initially developed a consensus statement (Appendix B; http://www.nata.org/statements/consensus/Consensus20Statement_Final20Version_Sept02.pdf) that set minimum standards of health care for adolescent athletes. The AMCSSAA monograph5 (http://www.nata.org/statements/support/secondary_school_medcarecommunication.pdf) was written by a subgroup of the task force and is intended to help secondary schools and community organizations sponsoring athletic programs for this age group to justify the importance of providing appropriate medical care and establishing an AHCT. The purpose of this paper is to provide a summary of the key points contained within the monograph and to highlight important information with regard to appropriate medical coverage for secondary school-aged athletes. Potential strategies for the prevention of injury and illness as they relate to athletic participation by secondary school-aged individuals are described in detail in the 11 sections of the monograph. A brief overview of each consensus statement point is listed below, and the full set of recommendations for each consensus statement is available in the monograph.5
Consensus Statement Point 1: Develop and Implement a Comprehensive Athletic Health Care Administrative System
Organizations sponsoring athletic programs for secondary school-aged individuals should establish a comprehensive athletic health care administrative system that ensures that appropriate medical care is provided for all participants. To provide appropriate medical care, organizations must create an AHCT that must function in a coherent, coordinated, and efficient manner with coaches and administrators of sponsoring organizations and that must adhere to commonly accepted standards of good clinical practice.
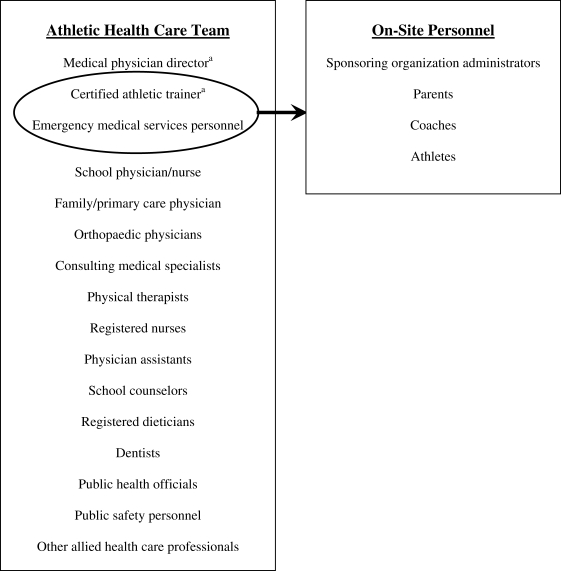
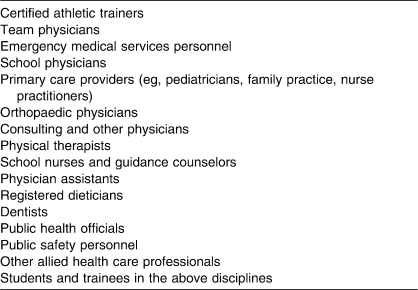
Medical and allied health professionals representing various disciplines are involved in the provision of athletic health care to adolescents and should be part of the AHCT. At the request of the American Academy of Pediatrics, the American Medical Association (AMA) has recommended that athletic medical units include a team physician and an athletic health coordinator, with preference in this role given to Board of Certification–certified athletic trainers (ATs).6 Furthermore, many jurisdictions require that ATs be supervised by licensed physicians, just as school nurses are supervised by school physicians and emergency medical technicians (EMTs) are supervised by emergency medical service (EMS) physicians. Therefore, the AT and team physician form the core of the AHCT, with the AT being the most appropriate on-site member of the AHCT and the official team physician being ultimately responsible for medical decisions made by the AHCT. A designated school official should act as a liaison to the AHCT when it is not possible to have an on-site member of the AHCT. The Figure depicts the various individuals who should be included as members of the AHCT and on-site personnel who are liaising with the AHCT. The list in the rectangle on the left denotes health care providers who should be considered in the formation of the AHCT. Of these, the AT and, in some cases, EMS personnel provide on-site medical coverage. The other members of the AHCT should be sought out by the AT as referral sources. In addition, on-site personnel such as administrators, coaches, parents, and athletes should work with the on-site members of the AHCT to ensure the implementation of the athletic health care administrative system. Other members of the team, along with the relationships among them, should be dictated by local needs and statutes (Table 1).
Figure. relationship between the athletic health care team and the on-site personnel. a Denotes core members of the athletic health care team.
Table 1.
Medical Professionals Who Should Be Members of the Athletic Health Care Team
A comprehensive athletic health care system should enhance the care of the athlete by allowing the strengths of individual members to complement each other and by preventing the unnecessary duplication of efforts. The roles and responsibilities of all medical team members should be clearly defined and available to all.
In addition, the sponsoring organization must create the appropriate policies and procedures to ensure all on-site athletic staff adhere to safe clinical practice guidelines for adequate medical care, designate appropriate physical space and equipment, document the activities of the AHCT, take part in injury surveillance, and commit to cycles of quality improvement so that appropriate medical care is available for all secondary school-aged athletes.
Consensus Statement Point 2: Determine the Individual's Readiness to Participate Through the Preparticipation Physical Examination
In 1992, 5 organizations (American Academy of Family Physicians, American Academy of Pediatrics, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sports Medicine) published a consensus report regarding the preparticipation physical examination (PPE),7 which was updated in 2005.8 This document clearly outlines the stated goals of the PPE along with guidelines for the organization and administration of the examination and, with the 1998 American Heart Association guidelines for cardiovascular screening of competitive athletes9,10 and the recommendations from the 36th Bethesda Conference,11 set the standard for the PPE.
Members of the AHCT may be the health care professionals who most often interact with adolescent athletes. The AMA has estimated that the athletic PPE serves as the only routine health maintenance for 80% to 90% of adolescents.12 The PPE is essential to identify athletes at risk for injury and to implement corrective actions before injuries occur. Yearly screening of these athletes is imperative, because health conditions may change from year to year and the development of subtle problems may be overlooked. The PPE is mandated for all participants in every scholastic sport and should be encouraged for those participating in community-based sports programs. The PPE should be performed by the athlete's primary care physician, school physician, or team physician. It is important that all pertinent information regarding the PPE be communicated to the AHCT if the PPE is performed by a family physician or a physician outside the AHCT.
The purpose of the PPE is not to exclude an individual from activity but instead to recognize individuals who may be at risk for developing injuries related to their activity and those who may be at risk for sudden death or catastrophic injuries as a result of underlying medical problems.8 The goal is to promote safe participation for the secondary school-aged athlete.
Although no time frame exists for performing the PPE, it has been suggested that the PPE be performed in advance of the sport season to allow optimum time to address any issues that may arise during the examination; 4 to 6 weeks before the start of a season seems to be the most appropriate time for the PPE. In scholastic sports played in the fall season, the PPE may be performed before the end of the preceding school year, so that any chronic injuries can be addressed and a treatment plan laid out for the student-athlete in the summer months. The AMCSSAA monograph5 describes the advantages and disadvantages of several methods of administering the PPE.
Many schools and states require yearly evaluations as a prerequisite for participation in sports. The AMA Group on Science and Technology endorsed the work of Risser et al13 and McKeag,14 who recommended that a PPE be performed at the beginning of any new level of competition, with a review before the start of each new season.15 Regardless of the time frames adapted, it is important to realize the need for routine screening for injury and illness recognition and prevention.
Consensus Statement Point 3: Promote Safe and Appropriate Practice, Competition, and Treatment Facilities
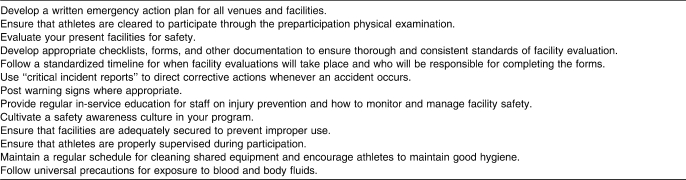
One of the goals of the AHCT is preventing athletic injuries. Prevention strategies should include having appropriate risk management strategies, such as the PPE and emergency action plan (EAP); using proper equipment; and having safe and well-maintained facilities available (Table 2).
Table 2.
Risk Management Strategies
Secondary school-aged athletes have a right to play in facilities that are safe and without the potential for unnecessary harm. When injuries do occur, these participants also have a right to be treated in a clean and appropriate environment that is dedicated to this purpose. Although the benefits young athletes gain from sports participation are immeasurable, the effects of accidental injuries and deaths to this age group cannot be ignored. Making sports facilities safe for young athletes is of paramount importance from a risk management standpoint. Providing safe facilities is an integral component of effective sports management and is governed by ethical, legal, and other administrative considerations. Safe facilities provide the opportunities for safe participation and a positive experience for the young athlete. The right to participate in safe and healthy environments is contained in The Bill of Rights for Young Athletes.16 Well-maintained facilities ensure that safety is a priority, and that priority is then carried to the public.
Sponsoring organizations that do not provide a safe environment expose themselves to unnecessary legal action and the athletes they are supposed to help to undue preventable injury. Facilities that are not routinely maintained also provide opportunity for undue accidental injury. Countless lawsuits have been filed and won by parties who have sustained injuries as a result of improper inspection and maintenance of facilities,17–19 hazards in and around facilities,20–23 unsafe grounds and external walkways,24–26 and improper facility signage.27–29 Such litigation depletes the financial resources of sponsoring institutions and reflects a negative image to the public about the specific institution and about sports in general.
In general, sports safety inspections should include all structures and surfaces used by the athletes. All parties involved with youth sports activities should regularly and thoroughly inspect their facilities: coaches, administrators, grounds and facilities staffs, and members of the AHCT. Some areas, such as fixed building structures, will require less-frequent inspections, whereas other areas, such as fields and floors, must be inspected frequently. Young athletes should be encouraged to be a part of this “injury prevention team” by immediately reporting any unsafe conditions to their adult sponsors.
Athletic facilities can vary greatly in size and complexity. Regardless of the size and purpose of a facility or the resources of its caretakers, entities that sponsor sports opportunities for secondary school-aged athletes should ensure that all facilities are safe. The AHCT can play a vital role in sports facility safety issues, specifically maintenance and sanitation, usage, and supervision.
Consensus Statement Point 4: Advise on the Selection, Fit, Function, and Maintenance of Athletic Equipment
Equipment essential to some sports (helmets, shoulder pads for football, sticks for field hockey) may be supplied by the sponsoring organization or the individual participant. If a sponsoring organization requires the participant to provide such equipment, it is incumbent upon the sponsoring entity to ensure that all equipment worn and used is in good condition, appropriate, and properly fitted. Sponsoring organizations that require the participant to provide his or her own equipment must ensure that personal equipment complies with requirements outlined by a sport regulatory agency. Entities that provide guidelines for approval of athletic equipment are the National Operating Committee on Standards in Athletic Equipment (NOCSAE) and the American Society for Testing and Materials (ASTM). The agency responsible for testing and certifying many types of helmets (including football, baseball, softball, lacrosse, and hockey helmets), soccer shin guards, and youth baseballs is NOCSAE,30 whereas standards for helmets for snow sports and eye protectors were developed by ASTM.31 Equipment that has not been approved by certifying bodies should not be used. A review of case law shows that equipment that is not well maintained or that is improperly fitted can contribute to, if not cause, injury to participants. In addition, the use of equipment that has not been approved by the appropriate certifying body exposes the athlete to injury and the sponsoring entity to liability and negligence.32–37
Ensuring that all athletes have properly fitting equipment is important to maintaining a safe athletic environment. Sponsoring agencies should ensure that qualified personnel (coach, AT, equipment manager) select, fit, and maintain equipment and that the athlete has appropriate equipment for participation. Many equipment manufacturers provide detailed instructions on the fitting of their equipment. These instructions should be followed when fitting participants or else the sponsoring agency could be found liable. In the case of Gerritty v Beatty,33 the school was found liable when an athlete reported poorly fitting equipment and the school did nothing about it.
Once equipment is properly fit to the athlete, sponsoring agencies and members of the AHCT must make sure the equipment is properly maintained and reconditioned. All athletic equipment should be examined periodically during the season and the fit maintained throughout the season (eg, if an athlete shaves his head, the helmet should be refit).38 In addition, school and team officials should closely inspect any equipment used by or around participants and know the risks involved in the use of such equipment. Case law has judged in favor of the plaintiffs when a latent defect in a pitching machine caused injury to the face of an athlete while the machine was unplugged39 and when a vaulting horse was altered and the holes for the pommels were exposed.37
Many manufacturers now recommend that equipment be reconditioned on a regular basis, so that flaws and defects can be identified and corrected. Most manufacturers state that they will not stand behind the product if the proper reconditioning and checks have not been made.40 In the case of Gerritty v Beatty,33 the school district was found negligent for refusing to furnish well-maintained equipment. Therefore, school districts should ensure that qualified personnel purchase, fit, and maintain appropriate athletic equipment and recondition existing equipment according to the manufacturers' recommendations. The qualified individual should have experience in fitting equipment and be familiar with manufacturers' manuals. The sponsoring organization and on-site members of the AHCT should be responsible for the oversight of proper fit and maintenance of equipment. In addition, the sponsoring organization should be cautioned not to accept used equipment passed down from higher-level organizations unless the equipment has been properly maintained and reconditioned.
Consensus Statement Point 5: Develop and Implement a Comprehensive Emergency Action Plan
Members of the AHCT, along with coaches and administrators, need to be prepared for emergency situations through the development and implementation of a comprehensive EAP. Participation in some athletic activities carries an inherent risk of serious injury. Sudden, serious illness can also afflict student-athletes and those involved with an athletic program. The sponsoring organization should have a comprehensive EAP in place to ensure that the appropriate care can be provided in a timely manner. The EAP should include planning for responses to medical emergencies involving spectators, coaches, and officials; crowd control; and evacuation in the event of severe weather, fire, and other natural or man-made disasters. In 2002, NATA41 issued a position statement regarding the need for established emergency plans in all athletic venues and suggested guidelines for developing and implementing the plans.
The need for an EAP has been well documented in the literature2,41–47 and is supported by case law.47 In Kleinknecht v Gettysburg College in 1993,48 it was decided that an institution owed a duty to each athlete to provide an emergency plan that was adequate for the risks involved in sport participation. This extends beyond the collegiate level and interscholastic athletic events, as seen in Barth by Barth v Board of Education in 1986,49 which showed the need for obtaining prompt medical treatment for students injured in physical education activities. In Jarreau v Orleans Parish School Board in 1992,50 a school board was found vicariously liable for the failure to promptly seek medical attention for an injured athlete. The implementation of an EAP addresses these needs and provides the most efficient opportunity for treatment for injury and illness.
The medical personnel who make up the AHCT often have experience in various areas of emergency athletic care and can contribute to the plan to ensure that it is comprehensive and appropriate for school-aged athletes and their events. The development of an EAP, however, requires the input of the AHCT, administrators of the sponsoring organization, coaches, and facility managers, along with parents and members of the local emergency response community. The EAP should be reviewed annually with all involved personnel and should have legal approval before it is implemented.
Consensus Statement Point 6: Establish Protocols Regarding Adverse Environmental Conditions
Secondary school-aged individuals participating in athletics are subject to injury and illness as a result of adverse environmental conditions. Adverse environmental conditions, including heat stress, cold stress, lightning, severe weather, air quality, insects, rodents, reptiles, fire, and possible allergic reaction–inducing conditions, pose various challenges to those participating in athletic events. The type of environmental conditions athletes face is based on geographic region and the influencing factors specific to that region. Each organization that sponsors an athletics program should establish protocols related to adverse environmental conditions specific to the region.51 The organizations should identify individuals responsible for ensuring the implementation of the protocols for the safety of adolescent athletes. This may include having the AHCT be responsible for the development and implementation of policies regarding adverse environmental conditions.
Several environmental considerations and threats can be included in an individual protocol depending on the venue and geographic region. Established policies regarding heat stress,52–56 cold stress,56,57 and lightning58,59 can be used as models for development. Other environmental condition protocols should be established with the members of the AHCT to ensure that all contingencies have been discussed in detail.
Consensus Statement Point 7: Provide for On-Site Recognition, Evaluation, and Immediate Treatment of Injury and Illness, with Appropriate Referrals
The initiation of prompt treatment is critical in the management of life-threatening or limb-threatening injuries or conditions. Early injury evaluation and treatment encourage proper healing and decrease the risk of reinjury.4,60–63 An immediate injury evaluation also permits the quick initiation of appropriate medical treatment, which is associated with proper healing and a reduced risk of reinjury.60,62 Immediate treatment can mean the difference between life and death. Heat stroke, for example, is one condition that can be fatal without prompt recognition and treatment.52 A suspected neck or cervical spine injury may lead to secondary injury or a worsening of the original injury.64
A thorough on-site initial evaluation is important to recognizing the nature and severity of the injury, to determining if more advanced treatment and care are required, and to limiting participation to protect the initial injury and prevent further harm. Adolescents who have sustained an injury should be evaluated immediately to determine the nature and extent of the injury, because its signs and symptoms may change relatively quickly.4,60–63 In addition, it is important to have qualified individuals who can make decisions about when and if an athlete can return to play or should be referred to the emergency room or for a medical evaluation by a physician. As described in Consensus Point 1, an AT is the recommended individual to provide on-site medical care for secondary school–aged athletes.
In some cases, the coach is the only person available on site during practices and games. The task force strongly recommends that all coaches be trained in first aid and cardiopulmonary resuscitation (CPR); however, the coach must adhere to his or her scope of practice, which would mean not making decisions regarding when it is appropriate for an athlete to return to play after an injury or illness. At a minimum, a coach or other individual who is with the team on a regular basis and who is trained in CPR (including use of an automated external defibrillator) and first aid should be available to tend to injuries that occur. In addition, protocols should be established, in advance, governing referrals and return-to-play decisions, especially when a sponsoring organization may have multiple simultaneous events going on at several sites.
Another viable option is the presence of an EMT/paramedic or a registered nurse at practices and games. These individuals would offer a higher level of care than an individual with first aid and CPR training; however, these individuals may be limited in their ability to render return-to-play decisions and to apply protective taping and padding after an injury.
Consensus Statement Point 8: Facilitate Rehabilitation and Reconditioning
For most athletes, a return to activity after the injury is expected. Although the evaluation and treatment provided immediately after the injury are critical, a rehabilitation and reconditioning program designed to safely return the individual to play is just as important. Rehabilitation and reconditioning programs reduce the likelihood of reinjury and promote a safe return to play. Organizations that sponsor athletic programs should establish an on-site member of the AHCT and identify this individual to manage the postinjury treatment plans of the athletes.
Programs designed to return an injured individual to a preinjury level of function can be described using a variety of terms, including injury treatment, rehabilitation program, and therapy. In general, these programs consist of exercise, therapeutic modalities, and functional activities specific to the individual and the injury.65–67 The goals of rehabilitation and reconditioning programs include preventing further injury and promoting a safe return to play.65 Adolescents who are injured during athletic performance should complete a rehabilitation and reconditioning program to promote a safe return to play.
The rehabilitation and reconditioning of athletic injuries represents a major component of a comprehensive injury prevention program and should be undertaken by a selected member of the AHCT. As described in Consensus Point 1, ATs are the best choice because they have the proper training and educational background to provide appropriate care for injured athletes and are able to make sound decisions regarding when an athlete can return to play.60,68 Although not all secondary schools or club sports organizations have the resources to hire an AT or implement a sophisticated sports medicine program, they can designate a qualified member of the coaching staff to work with a member of the AHCT to prevent injuries, provide medical care, and rehabilitate injured athletes.60 In addition, as members of the AHCT, physical therapists can provide rehabilitation services and communicate the athlete's progress and status to the on-site members of the AHCT, coaches, or administrators.
Consensus Statement Point 9: Provide for Psychosocial Consultation and Referral
Members of the AHCT should be capable of identifying potential psychosocial conditions and referring the athlete for appropriate diagnosis and management. Often this identification and referral occur through the PPE discussed earlier in this manuscript. Organizations that sponsor athletic programs must identify local experts who specialize in these areas and who can serve as referral sources for adolescent athletes in need of consultation.
Adolescents are at significant risk for morbidities associated with substance abuse, sexual activity, depression, eating disorders, suicidal tendencies, weapon use, violence, and vehicular recklessness. Adolescent athletes in particular may have an increased risk of depression associated with injury or athletic “burnout.” Furthermore, although adolescent athletes may have a decreased risk of cigarette smoking, some researchers have suggested increased use of smokeless tobacco, unsafe sexual activity, alcohol abuse, vehicular recklessness, and other risk-taking behaviors among certain adolescent athletes.
The health professionals best positioned and best suited to recognize psychosocial concerns in the athletic setting may be ATs, because they are more likely to be consistently available on site.69 Members of the AHCT may be well positioned but, because of their training, may not be well suited to identify emerging psychosocial problems. Implementation of this recommendation would therefore require some, if not all, of the following elements: As detailed in the PPE monograph,8 thorough psychosocial screening should be an important component of the PPE and should be conducted, ideally, by the athlete's primary care provider. If not conducted by the primary care provider, a thorough psychosocial screening could be conducted by another health care professional who is comfortable with adolescents and familiar with the basic tenets of confidential and sensitive interviewing. The issues that can be addressed in a thorough psychosocial screening can include questions regarding home life and family dynamics, education (school performance and relationships), activities (sports, jobs, and leisure enjoyment), diet, drug use, safety issues (violence, weapon use, vehicular recklessness), sexuality (contraception; type, number, and frequency of partners), depression, and suicidal tendencies. It is important to note that the on-site members of the AHCT often serve in a recognition and referral capacity.
Consensus Statement Point 10: Provide Scientifically Sound Nutritional Counseling and Education
Sports nutrition is a key factor in an athlete's growth, development, and performance. Adolescents have unique nutritional requirements that are further complicated by sport participation. The massive industry of supplements marketed to enhance sports performance and the lack of regulation with regard to the effectiveness and safety of such products pose an additional risk to secondary school–aged athletes. Athletes need guidance to make sound nutritional decisions in an age when fad diets and performance-enhancement products are prevalent.
Sponsoring organizations of athletic programs have a responsibility to provide a safe environment, including scientifically based information regarding nutrition and supplements. A solid knowledge of nutritional concepts is crucial to all AHCTs, especially those caring for secondary school–aged athletes. In addition to basic growth and development, competition puts an increased demand on daily nutritional requirements. Factors such as ethnicity, social and economic status, family history and environment, peer pressure, and inaccurate diet information can complicate the prescription for good nutrition. In addition, adolescents' tendencies to skip meals, snack on junk food, and feast at fast-food restaurants can add to poor eating habits.
A system for reviewing an athlete's nutritional status is the basis of providing appropriate information to athletes and parents regarding long-term nutritional health. Childhood obesity is on the rise in the United States and puts children at risk for heart disease, illness, and injury.70 A review of an athlete's nutritional status could alert the child and parents to a problem. If a child is found to have poor nutritional habits, an allied health care professional should help combat the problem by creating a plan to address the issues identified in the nutritional review.
Use of sports supplements and performance-enhancing drugs is fairly common among secondary school students.71,72 Most athletic governing bodies prohibit the use of supplements and drugs that are designed to enhance performance73; however, often no sanctions are imposed against athletes that might possibly deter them in the use of prohibited substances. Supplements marketed to enhance athletic performance often are touted as “herbal” or “natural,” which implies an element of safety. This, coupled with the massive marketing campaigns and the use of such products by professional athletes, provides for the “easy path to success” for the secondary school–aged athlete. Society's emphasis on winning and a child's desire to please parents and coaches make for a potentially deadly combination. Although young people may realize that supplements and performance-enhancing drugs are dangerous, few know the potential side effects.72,73
Members of the AHCT should be well versed in proper sports nutrition for the adolescent and have a basic knowledge of proper nutrition and eating habits. They should also have access to a professional nutritionist or dietician. Organizations should establish components of a comprehensive sports nutritional support system, based on current scientific facts, which should include (1) a system for reviewing an athlete's nutritional status, (2) policies to ensure the availability of hydration fluids in a clean, noninfectious environment at all sport settings, (3) a plan to encourage the ingestion of appropriate pre-exercise and postexercise food, (4) a system to identify athletes at risk for disordered eating and to treat those who have been identified, and (5) a plan that relies on scientifically supported literature when developing rules that restrict the use of performance-enhancing supplements, drugs, and substances as well as educational programs to inform coaches, athletes, and parents of the dangers of ergogenic aids.
Consensus Statement Point 11: Develop Injury and Illness Prevention Strategies
Injuries and illnesses may place a heavy burden on the well-being of secondary school-aged athletes. Thus, preventing these conditions should be a goal of the AHCT. Many interventions have proved effective in reducing the severity of athletic injuries.74–77 Still, many opportunities for prevention remain. The AMCSSAA monograph5 established recommendations for the prevention, care, and appropriate management of athletic-related injuries and illnesses specific to secondary school-aged athletes through a public health framework for developing effective interventions to reduce the burden of injuries.
A well-accepted scientific process exists for addressing a public health injury problem and, in this case, athletic injury among secondary school-aged athletes. This public health approach78–81 includes the following 5 mandates, which are described in greater detail in the AMCSSAA monograph5: (1) determine the existence and size of the problem (injury surveillance), (2) identify what may cause the problem (risk factors), (3) determine strategies and interventions that may prevent the problem, (4) implement prevention strategies, and (5) monitor and evaluate the effectiveness of prevention efforts.
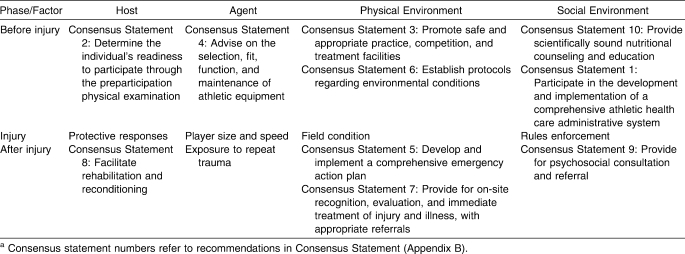
Once adequate surveillance studies have been completed and risk factors identified, one method for developing strategies for injury prevention is based on the approach introduced by William Haddon; this approach is known as the Haddon matrix.82 Prevention efforts can occur at 1 of 3 times: before the injury (when the energy becomes uncontrolled), during the injury (when the energy transferred to the body is more than can be safely absorbed), and after the injury (when the body attempts to heal the damage). In addition to the time axis, the Haddon matrix includes an axis of risk factors also found in the public health framework: the host (potentially injured person), the agent (the energy and the way in which it is transferred), and the environment (both physical and social). The resulting 12-cell matrix can be used as a brainstorming tool to devise interventions according to specific time phases and risk factors. An example of the use of the Haddon matrix applied to the problem of athletic injuries is found in Table 3. A strong prevention program incorporates interventions that span the time axis and address the different risk factors.
Table 3.
Haddon Matrix Applied to the Problem of Athletic Injuriesa
Ultimately, the goal is to determine whether the intervention worked and whether injuries have been reduced.83 The process returns full circle to the first step of surveillance for data that support or deny the effectiveness of the interventions that have been implemented. Although most of the interest lies in this primary question, other reasons, which are unrelated to the intervention and might explain why injuries were reduced, also must be considered. Another key issue is whether any unintended consequences (good or bad) were a direct result of the intervention. A bad unintended consequence may ruin any positive effect of the intervention, so whether fewer injuries occurred and whether the intervention had a positive effect on the athletes' overall well-being must be determined. Evaluation requires the conducting of well-designed randomized controlled effectiveness studies.
The potential strategies for the prevention of injury and illness in the secondary school-aged athlete have been presented in the individual sections of the AMCSSAA monograph.5 These interventions address various aspects of the framework previously described, including the athlete, energy transfer, and environment. They also relate to efforts that affect the safety and welfare of athletes before, during, and after the injury or illness. Finally, all members of the AHCT need to regularly review the effectiveness of a comprehensive program and monitor injuries and illnesses as part of an ongoing quality assurance program, as appropriate medical coverage for the secondary school-aged athlete is an active process, not one that is put in place and is then self-sustaining.
Conclusions
Appropriate medical care of the secondary school-aged individual involves more than basic emergency care during sport participation. It encompasses the provision of many other health care services. Although emergency medical care and event coverage are critical, appropriate medical care also includes activities of ongoing daily athletic health care. The AHCT comprises appropriate health care professionals in consultation with administrators, coaches, parents, and participants. Appropriate health care professionals can include ATs, team physicians, consulting physicians, school nurses, physical therapists, EMS personnel, dentists, and other allied health care professionals. Organizations sponsoring athletic programs for secondary school–aged individuals should establish an AHCT that functions to ensure that appropriate medical care is provided for all participants.
Appendix A. Special Thanks To The Following Members And Their Sponsoring Associations For Serving On The Appropriate Medical Care For Secondary School-Aged Athletes Task Force
American Academy of Family Physicians
Robert Pallay, MD
American Academy of Orthopaedic Surgeons
Clarence Shields, Jr, MD
American Academy of Pediatrics
Keith Loud, MD, FAAP
American Medical Society for Sports Medicine
Dave Jenkinson, DO
American Orthopaedic Society for Sports Medicine
Robert Hunter, MD
American Osteopathic Academy of Sports Medicine
Angela Cavanna, DO, FAOASM
Michele Gilsenan, DO, FAOASM
American Physical Therapy Association
Erin Barill, PT, ATC
American Public Health Association
Andrew Lincoln, ScD, MS
Emergency Medical Services
Robb Rehberg, PhD, ATC, NREMT
International Academy for Sports Dentistry
Leslie Rye, DDS
National Association of School Nurses
Elizabeth Mattey, MSN, RN, NCSN
National Association of Secondary School Principals
David Vodila
National Athletic Trainers' Association
Jon Almquist, ATC, Task Force Chair
Glenn Beachy, MS, ATC
Glen Cooper, ATC
Perry Denehy, MEd, ATC
Tony Fitzpatrick, MA, ATC
Lorrie Howe, ATC, CAA
Joe Iezzi, ATC
Roger Kalisiak, MS, ATC
Scott Linaker, MS, ATC
Bart Peterson, MSS, ATC
Craig Portwood, LAT, ATC
John Reynolds, MS, ATC
Brian Robinson, MS, ATC
Sandra J. Shultz, PhD, ATC, CSCS
Tamara Valovich McLeod, PhD, ATC
Thomas S. Woods, LAT, ATC
National Federation of State High School Associations
Jerry Diehl
National Interscholastic Athletic Administrators' Association
Alan Mallanda
National Safety Council
Barbara Caracci, MS
The President's Council on Physical Fitness and Sports
Christine G. Spain, MA
Disclaimer: The information contained within this document does not necessarily reflect endorsement from the individual organizations listed above.
Appendix B. Appropriate Medical Care For Secondary School-Aged Athletes Consensus Statement (revised April 2004)
Mission Statement
Establish recommendations for the prevention, care, and appropriate management of athletic-related injury and illnesses specific to the secondary school–aged individual.
Athletic Health Care Team
The athletic health care team (AHCT) may be composed of appropriate health care professionals in consultation with administrators, coaches, parents, and participants. Appropriate health care professionals could be certified athletic trainers, team physicians, consulting physicians, school nurses, physical therapists, emergency medical services personnel, dentists, and other allied health care professionals.
Recommendations for Appropriate Medical Care
Appropriate medical care of the secondary school–aged individual involves more than basic emergency care during sport participation. It encompasses the provision of many other health care services. Although emergency medical care and event coverage are critical, appropriate medical care also includes activities of ongoing daily athletic health care.
Organizations sponsoring athletic programs for secondary school–aged individuals should establish an AHCT that functions to ensure that appropriate medical care is provided for all participants.
The AHCT should have a designated athletic health care provider(s) who is educated and qualified to
Participate in the development and implementation of a comprehensive athletic health care administrative system (eg, personal health information, policies and procedures, insurance, referrals).
Determine the individual's readiness to participate.
Promote safe and appropriate practice, competition, and treatment facilities.
Advise on the selection, fit, function, and maintenance of athletic equipment.
Develop and implement a comprehensive emergency action plan.
Establish protocols regarding environmental conditions.
Provide for on-site recognition, evaluation, and immediate treatment of injury and illness, with appropriate referrals.
Facilitate rehabilitation and reconditioning.
Provide for psychosocial consultation and referral.
Provide scientifically sound nutritional counseling and education.
Develop injury and illness prevention strategies.
Education
Designated athletic health care providers shall maintain expertise through continuing education and professional development.
All coaches should be trained in first aid, cardiopulmonary resuscitation (CPR), and automated external defibrillator (AED) use, utilization of AHCT professionals, injury prevention, and modification of training in response to injury and illness.
Definitions
Certified Athletic Trainer: An allied health care professional who, on graduation from an accredited college or university, and after successfully passing the Board of Certification examination, is qualified and appropriately credentialed according to state regulations to work with individuals engaged in physical activity in the prevention of injuries and illnesses; the recognition, evaluation, and immediate care of injuries and illnesses; the rehabilitation and reconditioning of injuries and illnesses; and the administration of this health care system. This individual must have current certification in CPR and be qualified in first aid and blood-borne pathogens. Other health care professionals with equivalent certification and/or licensure would also meet this standard.
Team Physician: The team physician must have an unrestricted medical license and be an MD or a DO who is responsible for treating and coordinating the medical care of athletic team members. The principal responsibility of the team physician is to provide for the well-being of individual athletes, enabling each to realize his or her full potential. The team physician should possess special proficiency in the care of musculoskeletal injuries and medical conditions encountered in sports. The team physician also must actively integrate medical expertise with that of other health care providers, including medical specialists, athletic trainers, and allied health professionals. The team physician must ultimately assume responsibility within the team structure for making medical decisions that affect the athlete's safe participation.
(Reference: Team Physician Consensus Statement. http://www.acsm.org/Content/NavigationMenu/News/Pronouncements_Statements/TeamPhysicianConsensusStatements/Consensus_Statements.htm. Accessed December 14, 2007.)
Appendix C. Statements of Support
The “Summary Statement: Appropriate Medical Care for Secondary School-Aged Athletes” (SSAMCSSAA) has been endorsed by the American Academy of Pediatrics. The document has been approved by the American Academy of Family Physicians.
The American Orthopaedic Society for Sports Medicine
Participated in and endorsed the SSAMCSSAA for providing appropriate medical care for secondary school-aged athletes;
Supports the National Athletic Trainers' Association SSAMCSSAA document as a comprehensive resource for fulfilling the different important components of medical care for secondary school-aged athletes;
Encourages secondary school athletics programs to follow the guidelines elaborated in the document wherever practical. In those instances where it may not be feasible to follow the guidelines, secondary schools should take acceptable alternative measures to ensure that medical care is consistent with the SSAMCSSAA.
The National Federation of State High School Associations participated in the development of the SSAMCSSAA and advocates appropriate medical care for all secondary school-aged athletes. The National Federation of State High School Associations Sports Medicine Advisory Committee is committed to the well-being of the 7 000 000 student athletes in its more than 18 000 high schools. The National Athletic Trainers' Association is well positioned to assist member state associations with this goal.
Footnotes
Jon Almquist, ATC; Tamara C. Valovich McLeod, PhD, ATC, CSCS; Angela Cavanna, DO, FAOASM; Dave Jenkinson, DO; Andrew E. Lincoln, ScD, MS; Keith Loud, MD, FAAP; Bart C. Peterson, MSS, ATC; Craig Portwood, LAT, ATC; John Reynolds, MS, ATC; and Thomas S. Woods, LAT, ATC, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
References
- 1.National Federation of State High School Associations. 2004-05 NFHS High School Athletics Participation Survey. Indianapolis, IN: National Federation of State High School Associations; 2005. [Google Scholar]
- 2.Washington R.L, Bernhardt D.T, Gomez J, et al. Organized sports for children and preadolescents. Pediatrics. 2001;107(6):1459–1462. doi: 10.1542/peds.107.6.1459. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention and Control. CDC Injury Research Agenda. Atlanta, GA: Centers for Disease Control and Prevention; 2002. [Google Scholar]
- 4.Powell J.W, Barber-Foss K.D. Injury patterns in selected high school sports: a review of the 1995–1997 seasons. J Athl Train. 1999;34(3):277–284. [PMC free article] [PubMed] [Google Scholar]
- 5.Almquist J.L, Valovich McLeod T, Cavanna A, et al. Appropriate medical care for the secondary school–age athlete communication. http://www.nata.org/statements/support/secondary_school_medcarecommunication.pdf. Accessed July 7, 2007. [DOI] [PMC free article] [PubMed]
- 6. American Medical Association Resolution H-470.995 Athletic (Sports) Medicine (1998).
- 7.Smith D.M, Kovan J.R, Rich B.S.E, Tanner S.M. Preparticipation Physical Evaluation. 2nd ed. New York, NY: McGraw-Hill; 1997. [Google Scholar]
- 8.Preparticipation Physical Evaluation Working Group. Preparticipation Physical Evaluation. Minneapolis, MN: McGraw-Hill; 2005. [Google Scholar]
- 9.Maron B.J, Thompson P.D, Puffer J.C, et al. Cardiovascular preparticipation screening of competitive athletes: a statement for health professionals from the Sudden Death Committee (Clinical Cardiology) and Congenital Cardiac Defects Committee (Cardiovascular Disease in the Young), American Heart Association. Circulation. 1996;94(4):850–856. doi: 10.1161/01.cir.94.4.850. [DOI] [PubMed] [Google Scholar]
- 10.Maron B.J, Thompson P.D, Puffer J.C, et al. Cardiovascular preparticipation screening of competitive athletes: an addendum. An addendum to a statement for health professionals from the Sudden Death Committee (Council on Clinical Cardiology) and the Congenital Cardiac Defects Committee (Council on Cardiovascular Disease in the Young), American Heart Association. Circulation. 1998;97(22):2294. doi: 10.1161/01.cir.97.22.2294. [DOI] [PubMed] [Google Scholar]
- 11.Maron B.J, Chaitman B.R, Ackerman M.J, et al. Working Groups of the American Heart Association Committee on Exercise, Cardiac Rehabilitation and Prevention, Councils on Clinical Cardiology and Cardiovascular Disease in the Young. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109(22):2807–2816. doi: 10.1161/01.CIR.0000128363.85581.E1. [DOI] [PubMed] [Google Scholar]
- 12.Athletic preparticipation examinations for adolescents: Report of the Board of Trustees. Group on Science and Technology, American Medical Association. Arch Pediatr Adolesc Med. 1994;148(1):93–98. [PubMed] [Google Scholar]
- 13.Risser W.L, Hoffman H.M, Bellah G.G., Jr Frequency of preparticipation sports examinations in secondary school athletes: are the University Interscholastic League guidelines appropriate. Tex Med. 1985;81(7):35–39. [PubMed] [Google Scholar]
- 14.McKeag D.B. Preseason physical examination for the prevention of sports injuries. Sports Med. 1985;2(6):413–431. doi: 10.2165/00007256-198502060-00003. [DOI] [PubMed] [Google Scholar]
- 15.Rifat S.F, Ruffin M.T, IV, Gorenflo D.W. Disqualifying criteria in preparticipation sports evaluations. J Fam Pract. 1995;41(1):42–50. [PubMed] [Google Scholar]
- 16.National Association for Sport and Physical Education. The bill of rights for young athletes. In: Martens R, Sefeldt V, editors. Guidelines in Children's Sports. Reston, VA: National Association for Sport and Physical Education; 1979. [Google Scholar]
- 17. Bush v Parents Without Partners, 21 CR2d 178 (1993).
- 18. Short v Griffiths, 255 SE2d 479 (Va 1979).
- 19. Ardoin v Evangeline Parish School Board, 376 So2d 372 (La 1979).
- 20. Domino v Murcurio, 193 NE2d 893 (NY 1963).
- 21. Dawson v Rhode Island Auditorium, Inc, 242 A2d 407 (RI 1968).
- 22. Pedersen v Joilet Park District, 483 NE2d 21 (Ill 1983).
- 23. Singer v School District of Philadelphia, 513 A2d 1108 (Pa 1986).
- 24. Flournoy v McCoumas, 488 P2d 1104 (1971).
- 25. Taylor v Oakland Scavenger Company, 17 C2d 594 (1941).
- 26. Horynak v The Pomfret School, 783 F2d 284 (1st Cir 1986).
- 27. First Overseas Investment Corporation v Cotton, 491 So2d 293 (Fla Dist Ct of App 1986).
- 28. Markowitz v Arizona Park Board, 706 P2d 364 (146 Ariz 352 1985).
- 29. Jacobs v Commonwealth Highland Theatres, Inc, 738 P2d 6 (Col Ct of App 1986).
- 30.Standard documents and laboratory guides. National Operating Committee on Standards for Athletic Equipment. http://www.nocsae.org/standards/documents.html. Accessed July 7, 2007. [PubMed]
- 31.American Society for Testing and Materials. http://www.astm.org. Accessed July 7, 2007.
- 32. Everett v Bucky Warren, Inc, 380 NE (2d).
- 33. Gerritty v Beatty, 71 Ill 2d 47 (373 NE2d 1323).
- 34. O'Brien v Township High School District, 392 (NE).
- 35. Stineman v Fontbonne College, 664 (F2d).
- 36. Berman v Philadelphia Board of Education, 456A (2d).
- 37. Tiemann v Independent School District #740, 331 (NW2d).
- 38.Michigan Governor's Council on Physical Fitness, Health and Sports. Position statement: the prevention of injuries in amateur football. 2003. http://www.mdch.state.mi.us/pha/vipf2/football.htm. Accessed January 2003.
- 39. Dudley Sports Co, Inc v Lawrence Robert Schmitt b/n/f/ Joseph Schmitt, 151 Ind App 217 (279 NE2d).
- 40.Schutt Sports. Schutt football FAQ. http://www.schuttsports.com/aspx/FAQ/FAQ.aspxid1. Accessed May 31, 2003.
- 41.Andersen J.C, Courson R.W, Kleiner D.M, McLoda T.A. National Athletic Trainers' Association position statement: emergency planning in athletics. J Athl Train. 2002;37(1):99–104. [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Nonfatal sports- and recreation-related injuries treated in emergency departments—United States, July 2000–June 2001. MMWR Morb Mortal Wkly Rep. 2002;51(33):736–740. [PubMed] [Google Scholar]
- 43.Walsh K. Thinking proactively: the emergency action plan. Athl Ther Today. 2001;6(5):57–63. [Google Scholar]
- 44.American Academy of Pediatrics. Committee on School Health. Guidelines for emergency medical care in school. Pediatrics. 2001;107(2):435–436. doi: 10.1542/peds.107.2.435. [DOI] [PubMed] [Google Scholar]
- 45.Physical fitness and activity in schools: policy statement. American Academy of Pediatrics. Pediatrics. 2002;105(5):1156–1157. doi: 10.1542/peds.105.5.1156. [DOI] [PubMed] [Google Scholar]
- 46.National Collegiate Athletic Association. NCAA Sports Medicine Handbook. 15th ed. Indianapolis, IN: National Collegiate Athletic Association; 2002. NCAA guideline 1f, emergency care and coverage; pp. 16–17. [Google Scholar]
- 47.Wilde J, Cotton D. Sport Law for Sport Managers. Dubuque, IA: Kendall/Hunt; 1997. [Google Scholar]
- 48. Kleinknecht v Gettysburg College, 786 F Supp 449 (3rd Cir 1993).
- 49. Barth by Barth v Board of Education, 490 NE2d 77 (Ill App 1 Dist 1986).
- 50. Jarreau v Orleans Parish School Board, 600 So2d 1389 (La 1992).
- 51.American Orthopaedic Society for Sports Medicine. Sideline Preparedness for the Team Physician: A Consensus Statement. Rosemont, IL: American Orthopaedic Society for Sports Medicine; 2002. [Google Scholar]
- 52.Binkley H.M, Beckett J, Casa D.J, Kleiner D.M, Plummer P.E. National Athletic Trainers' Association position statement: exertional heat illness. J Athl Train. 2002;37(3):329–343. [PMC free article] [PubMed] [Google Scholar]
- 53.Convertino V.A, Armstrong L.E, Coyle E.F, et al. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 1996;28(1):i–vii. doi: 10.1097/00005768-199610000-00045. [DOI] [PubMed] [Google Scholar]
- 54.Inter-Association Task Force. Inter-Association Task Force on Exertional Heat Illnesses Consensus Statement. National Athletic Trainers' Association. http://www.nata.org/statements/consensus/heatillness.pdf. Accessed 2003.
- 55.National Collegiate Athletic Association. NCAA Sports Medicine Handbook. Indianapolis, IN: National Collegiate Athletic Association; 2002. NCAA guideline 2c, prevention of heat illness; pp. 22–24. [Google Scholar]
- 56.Armstrong L.E, Epstein Y, Greenleaf J.E, et al. American College of Sports Medicine position stand: heat and cold illnesses during distance running. Med Sci Sports Exerc. 1996;28(12):i–x. [PubMed] [Google Scholar]
- 57.National Collegiate Athletic Association. NCAA Sports Medicine Handbook. Indianapolis, IN: National Collegiate Athletic Association; 2002. NCAA guideline 2m, cold stress; pp. 48–50. [Google Scholar]
- 58.Walsh K.M, Bennett B, Cooper M.A, Holle R.L, Kithil R, Lopez R.E. National Athletic Trainers' Association position statement: lightning safety for athletics and recreation. J Athl Train. 2000;35(4):471–477. [PMC free article] [PubMed] [Google Scholar]
- 59.National Collegiate Athletic Association. NCAA Sports Medicine Handbook. Indianapolis, IN: National Collegiate Athletic Association; 2002. NCAA guideline 1d, lightning safety; pp. 12–14. [Google Scholar]
- 60.Lyznicki J.M, Riggs J.A, Champion H.C. Certified athletic trainers in secondary schools: report of the Council on Scientific Affairs, American Medical Association. J Athl Train. 1999;34(3):272–276. [PMC free article] [PubMed] [Google Scholar]
- 61.National Athletic Trainers' Association. Minimizing the risk of injury in high school athletics. http://www.nata.org/publications/brochures/minimizingtherisks.htm. Accessed February 19, 2003.
- 62.Shimon J.M. Youth sports injury: prevention is key. Strategies. 2002;15(5):27–30. [Google Scholar]
- 63.Weaver N.L, Marshall S.W, Miller M.D. Preventing sports injuries: opportunities for intervention in youth athletics. Patient Educ Counsel. 2002;46(3):199–204. doi: 10.1016/s0738-3991(01)00213-0. [DOI] [PubMed] [Google Scholar]
- 64.Kleiner D.M, Almquist J.L, Bailes J, et al. Prehospital Care of the Spine-Injured Athlete: A Document from the Inter-Association Task Force for Appropriate Care of the Spine-Injured Athlete. Dallas, TX: National Athletic Trainers' Association; 2001. [Google Scholar]
- 65.Prentice W.E. Rehabilitation Techniques in Sports Medicine. 2nd ed. St. Louis, MO: Mosby; 1994. [Google Scholar]
- 66.Harris G.R, Susman J.L. Managing musculoskeletal complaints with rehabilitation therapy: summary of the Philadelphia Panel evidence-based clinical practice guidelines on musculoskeletal rehabilitation interventions. J Fam Pract. 2002;15(12):1042–1046. [PubMed] [Google Scholar]
- 67.Hurwitz E.L, Morgenstern H, Harber P, Kominski G.F, Belin T.R, Adams A.H. University of California–Los Angeles. A randomized trial of medical care with and without physical therapy and chiropractic care with and without physical modalities for patients with low back pain: 6-month follow up outcomes from the UCLA low back pain study. Spine. 2002;27(20):2193–2204. doi: 10.1097/00007632-200210150-00002. [DOI] [PubMed] [Google Scholar]
- 68.American Medical Association. Report 5 of the Council on Scientific Affairs (A-98): certified athletic trainers in secondary schools. http://www.ama-assn.org/ama/pub/article/2036-2373.html. Accessed May 25, 2003. [PMC free article] [PubMed]
- 69.Board of Certification. Role Delineation Study for the Entry-Level Certified Athletic Trainer. 5th ed. Omaha, NE: Board of Certification; 2004. p. 12. [Google Scholar]
- 70.Ogden C.L, Flegal K.M, Carroll M.D, Johnson C.L. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 71.Dodge T.L, Jaccard J.J. The effect of high school sports participation on the use of performance-enhancing substances in young adulthood. J Adolesc Health. 2006;39(3):367–373. doi: 10.1016/j.jadohealth.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 72.Castillo E.M, Comstock R.D. Prevalence of use of performance-enhancing substances among United States adolescents. Pediatr Clin North Am. 2007;54(4):663–675. doi: 10.1016/j.pcl.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 73.Shultz S.J, Valovich T.C, Zinder S.M. Sports Medicine Handbook. Indianapolis, IN: National Federation of State High School Associations; 2002. [Google Scholar]
- 74.Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer: a prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol. 1996;4(1):19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 75.Junge A, Rosch D, Peterson L, Graf-Baumann T, Dvorak J. Prevention of soccer injuries: a prospective intervention study in youth amateur players. Am J Sports Med. 2002;30(5):652–659. doi: 10.1177/03635465020300050401. [DOI] [PubMed] [Google Scholar]
- 76.Perna F.M, Antoni M.H, Baum A, Gordon P, Schneiderman N. Cognitive behavioral stress management effects on injury and illness among competitive athletes: a randomized clinical trial. Ann Behav Med. 2003;25(1):66–73. doi: 10.1207/S15324796ABM2501_09. [DOI] [PubMed] [Google Scholar]
- 77.Tyler T.F, Nicholas S.J, Campbell R.J, Donellan S, McHugh M.P. The effectiveness of a preseason exercise program to prevent adductor muscle strains in professional ice hockey players. Am J Sports Med. 2002;30(5):680–683. doi: 10.1177/03635465020300050801. [DOI] [PubMed] [Google Scholar]
- 78.Jones B.H, Hansen B.C. An Armed Forces epidemiological board evaluation of injuries in the military. Am J Prev Med. 2000;18(suppl 3):14–25. doi: 10.1016/s0749-3797(99)00170-1. [DOI] [PubMed] [Google Scholar]
- 79.Jones B.H, Knapik J.J. Physical training and exercise-related injuries: surveillance, research and injury prevention in military populations. Sports Med. 1999;27(2):111–125. doi: 10.2165/00007256-199927020-00004. [DOI] [PubMed] [Google Scholar]
- 80.Mercy J.A, Rosenburg M.L, Powell K.E, Broome C.V, Roper W.L. Public health policy for preventing violence. Health Aff (Millwood) 1993;12(4):7–29. doi: 10.1377/hlthaff.12.4.7. [DOI] [PubMed] [Google Scholar]
- 81.Robertson L.S. Injury Epidemiology. New York, NY: Oxford Press; 1992. [Google Scholar]
- 82.Haddon W. Options for the prevention of motor vehicle crash injury. Isr J Med Sci. 1980;16(1):45–65. [PubMed] [Google Scholar]
- 83.Sleet D, Bonzo S, Branche C. An overview of the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention. Injury Prev. 1998;4(4):308–312. doi: 10.1136/ip.4.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]