Abstract
TRAIL/Apo-2L has shown promise as an anti-glioma drug, based on investigations of TRAIL sensitivity in established glioma cell lines, but it is not known how accurately TRAIL signalling pathways of glioma cells in vivo are reproduced in these cell lines in vitro. To replicate as closely as possible the in vivo behaviour of malignant glioma cells, 17 early passage glioma cell lines and 5 freshly resected gliomas were exposed to TRAIL-based agents and/or chemotherapeutic drugs. Normal human hepatocytes and astrocytes and established glioma cell lines were also tested. Cross-linked TRAIL, but not soluble TRAIL, killed both normal cell types and cells from three tumours. Cells from only one glioma were killed by soluble TRAIL, although only inefficiently. High concentrations of cisplatin were lethal to glioma cells, hepatocytes and astrocytes. Isolated combinations of TRAIL and chemotherapy drugs were more toxic to particular gliomas than normal cells, but no combination was generally selective for glioma cells. This study highlights the widespread resistance of glioma cells to TRAIL-based agents, but suggests that a minority of high-grade glioma patients may benefit from particular combinations of TRAIL and chemotherapy drugs. In vitro sensitivity assays may help identify effective drug combinations for individual glioma patients.
Keywords: glioma, astrocytoma, glioblastoma, Apo-2L, apoptosis
The vast majority of malignant glioma patients die within 2 years of diagnosis, regardless of treatment (Group, 2002; Stupp et al, 2005). More effective treatments are therefore urgently required. Chemotherapy and irradiation trigger apoptosis of sensitive cells by provoking the ‘intrinsic’ apoptosis pathway (Norbury and Zhivotovsky, 2004). This involves the detection of DNA damage and instigation of a self-destruction program, which is regulated by the Bcl-2 family and executed by a molecular machinery including cytochrome c, Apaf-1 and the apoptotic proteases caspase-9 and caspase-3. Defects in the intrinsic pathway can contribute to resistance to chemotherapy and radiotherapy (Longley and Johnston, 2005). In contrast, ‘death ligands’, members of the TNF-α superfamily including FasL/CD95 and TRAIL/Apo2L, stimulate apoptosis through the ‘extrinsic’ pathway (Thorburn, 2004). Ligation of death receptors (such as Fas, DR4/TRAIL-R1 and DR5/TRAIL-R2) promotes recruitment of an adaptor molecule, FADD, caspase-8 and/or caspase-10 to form a complex known as the death-inducing signalling complex (DISC) (Kischkel et al, 1995). The initiator caspases are activated within the DISC, and acquire the ability to proteolytically activate effector caspases (such as caspase-3), either directly or indirectly (Scaffidi et al, 1998). The downstream caspases then destroy the cell by digesting numerous cellular proteins.
Because this extrinsic apoptosis pathway uses distinct components from that triggered by conventional anti-cancer treatments, there has been substantial research interest in exploiting its potential for treating tumour types that are unresponsive to currently available therapies. TRAIL and agonistic anti-TRAIL receptor antibodies are currently being evaluated in early-phase clinical trials. Initial reports portrayed TRAIL as an exemplary anti-cancer agent, as it induced apoptosis in many types of tumour cells but, unlike FasL, did not kill normal cells. Subsequent studies tempered that initial optimism somewhat. Although the extracellular portion of human TRAIL (amino acids 114–281, henceforth referred to as soluble TRAIL) was generally tolerated by normal human cells (Ashkenazi et al, 1999), other formulations were found to be toxic to particular normal cell types (Leverkus et al, 2000; Nitsch et al, 2000; Pettersen et al, 2002). Freshly isolated human hepatocytes displayed substantial sensitivity to His-tagged TRAIL, cross-linked TRAIL formulations and agonistic anti-DR4 and DR5 antibodies (Jo et al, 2000; Mori et al, 2004; Ganten et al, 2006), but survived incubation with soluble TRAIL (Ashkenazi et al, 1999; Lawrence et al, 2001; Ganten et al, 2006). The TRAIL sensitivity of normal brain cells is particularly relevant for the development of TRAIL-based anti-glioma therapies. Human astrocytes were relatively resistant to soluble untagged TRAIL in vitro (Ashkenazi et al, 1999; Song et al, 2006). Cell death was detected in brain slices incubated with FLAG-tagged TRAIL that had been cross-linked with an anti-FLAG antibody (Nesterov et al, 2002). Immunofluorescent assays suggested that the cells killed in these experiments included isolated neurons, oligodendrocytes, astrocytes and microglial cells (Nesterov et al, 2002).
Established glioma cell lines vary considerably in their responsiveness to TRAIL receptor ligation (reviewed in Hawkins, 2004). It is presently unknown how faithfully the death ligand signalling pathways of glioma cells in vivo are mimicked by established glioma cell lines, but it is has been shown that glioma cells do undergo substantial phenotypic changes in vitro (Anderson et al, 2002; Lee et al, 2006). TRAIL sensitivity of freshly resected uncultured glioma cells has not been reported to date. A few papers have documented the TRAIL responsiveness of minimally cultured gliomas, most of which were resistant to TRAIL as a sole agent (Roa et al, 2003; Song et al, 2003; Jeremias et al, 2004; Eramo et al, 2005; Li et al, 2006; Koschny et al, 2007). TRAIL can cooperate with other agents, including currently used chemotherapy drugs, to kill established glioma cells that survive exposure to TRAIL alone. It was recently published that the proteosome inhibitor bortezomib dramatically sensitised minimally passaged glioma cells to isoleucine-zipper-tagged TRAIL (Koschny et al, 2007). Importantly, however, the sensitivity of normal astrocytes to this co-treatment has not been reported.
Numerous mechanisms of glioma cell resistance to TRAIL have been suggested. Some resistant glioma cell lines could be sensitised by the treatment with the translation inhibitor cycloheximide, implicating a labile inhibitor of TRAIL signalling in the resistance of those cell lines (Rieger et al, 1998; Wu et al, 2000; Hao et al, 2001; Rohn et al, 2001; Fulda et al, 2002a). Lack of surface expression of TRAIL death receptors was reported in one glioma cell line (Arizono et al, 2003). Co-treatment of some resistant lines with chemotherapy drugs, which raised TRAIL receptor levels, enhanced TRAIL sensitivity (Nagane et al, 2000; Rohn et al, 2001; Shinohara et al, 2001; Arizono et al, 2003). Expression of inhibitors such as PKCε (Shinohara et al, 2001), cFLIP (Hao et al, 2001; Xiao et al, 2002) or PEA-15 (Hao et al, 2001; Xiao et al, 2002) was associated with resistance in a small number of glioma cell lines, but causal relationships were not conclusively demonstrated. The ability of bortezomib to sensitise early passage glioma cells to TRAIL (Koschny et al, 2007) implies that proteosomal degradation of critical TRAIL pathway components could contribute to resistance in those cells. Inhibition of IAP activity in type II glioma cells sensitised them to TRAIL (Fulda et al, 2002b), indicating that IAP activity contributed to the TRAIL resistance of those lines. Low levels of caspase-8 may also contribute to TRAIL resistance (Knight et al, 2001; Ashley et al, 2005; Eramo et al, 2005).
A tenet underlying modern approaches to cancer treatment is that combination therapies can provide better selectivity and efficacy than single-agent treatments. To explore the possible clinical utility of combination TRAIL/chemotherapy treatment for malignant glioma, this study examined the responses of glioma cells, astrocytes and hepatocytes to TRAIL-based agents and/or chemotherapy drugs. Four TRAIL-related agents were tested: two forms of cross-linked TRAIL (F-LZ-TRAIL and ‘Superkiller’), the extracellular portion of TRAIL (‘soluble TRAIL’) and an agonistic anti-DR5 antibody. Seven chemotherapy drugs used for glioma therapy were also employed: cisplatin, carboplatin, CCNU, temozolomide, etoposide, vincristine and procarbazine. The drug combinations were tested on freshly resected gliomas and early passage glioma cell lines, to mimic as closely as possible the in vivo behaviour of malignant glioma cells.
Materials and Methods
Glioma samples and normal cells
Table 1 provides details about the patients whose tumours were assayed in this study. Gliomas RMH018-023 were resected at the Royal Melbourne Hospital, Australia. Informed consent was obtained from the patients, and approval for this study was obtained from the ethics committees of the Royal Children's Hospital, Royal Melbourne Hospital and La Trobe University. To generate a single cell suspension, tumour pieces were minced with a scalpel, then incubated with Accumax (Sigma, St Louis, MO, USA) and filtered through a tea stainer and 100 μM filter. Viable cells were isolated by Ficoll density centrifugation.
Table 1. Patient and cell line features.
| Tumour/ cell line | Sex, age (years) | Tumour grade (WHO) | Passage number | p53 genotypea | Treatment before sample obtained | Treatment after sample obtained | Progression free survival | Patient status |
|---|---|---|---|---|---|---|---|---|
| D2234 | M, 52 | IV | 10 | M | Radiotherapy, temozolomide | BCNU wafer, O6BG, cloretazine, AP23573 | 2 months | Died 7 months post-resection |
| D2235 | F, 20 | III | 9 | M | Nil | Radiotherapy, temozolomide, CCNU, tamoxifen | 35+months | Stable 35 months post-resection |
| D2238 | F, 31 | III | 7 | W | Nil | Radiotherapy, temozolomide, CCNU, tamoxifen | 34+months | Stable 34 months post-diagnosis |
| D2239 | M, 56 | IV | 7 | W | Nil | Radiotherapy, temozolomide, hydroxyurea, imatinib mesylate | 3 months | Died 4 months post-resection |
| D2245 | M, 44 | III | 9 | W | Temozolomide | Radiotherapy, CCNU, tamoxifen, imatinib mesylate, hydroxyurea, CCNU, bevacizumab, CPT-11 | 18 months | Stable 32 months post-resection |
| D2247 | M, 51 | IV | 8 | W | Radiotherapy, temozolomide | BCNU wafer, O6BG, CPT-11, imatinib mesylate, hydroxyurea | 4 months | Died 9 months post-resection |
| D2248 | M, 44 | III | 6 | W | Nil | Unknown | Data not available | Data not available |
| D2259 | M, 27 | III | 7 | W | Nil | Radiotherapy, temozolomide, CCNU | 31+months | Stable 31 months post-resection |
| D2261 | M, 52 | III | 5 | W | Nil | Radiotherapy, temozolomide, CCNU, cloretazine | 7 months | Died 10 months post-resection |
| D2262 | F, 40 | III | 5 | W | Nil | Radiotherapy, temozolomide | 3 months | Unknown |
| D2264 | F, 45 | IV | 4 | ND | Nil | Radiotherapy, temozolomide, CCNU, CPT-11, tamoxifen | 30+months | Stable 30 months post-resection |
| D2268 | M, 59 | IV | 6 | M1 | Nil | Radiotherapy, temozolomide, CCNU, CPT-11, imatinib mesylate, hydroxyurea/PTK787, bevacizumab, carboplatin | 7 months | Stable 26 months post-resection |
| D2301 | M, 51 | IV | 1 | M2 | Nil | BCNU wafer, radiotherapy, temozolomide, cilengitide, CCNU, imatinib mesylate, hydroxyurea, PTK787 | 3 months | Stable 13 months post-resection |
| D2302 | M, 40 | IV | 3 | ND | Nil | Radiotherapy, temozolomide, etoposide, re-resection | 24+months | Stable 24 months post-resection |
| LM-G-2 | M, 54 | IV | 4 | ND | Nil | Sub-total resection then radiotherapy | 4+months | Alive 4 months post-resection |
| LM-G-4 | M, 69 | IV | 3 | M | Nil | Gross total resection then radiotherapy | 12 months | Died 20 months post-resection |
| LM-G-8 | M, 74 | IV | 3 | M | Nil | Radiotherapy | 2 months | Died 5 months post-resection |
| RMH | ||||||||
| 018 | M, 54 | III | ex vivo | ND | Nil | Recurrence, resection | data not available | Alive 6 months post-resection |
| RMH | ||||||||
| 019 | M, 62 | IV | ex vivo | ND | Nil | Radiotherapy and temozolomide | data not available | Alive 6 months post-resection |
| RMH | ||||||||
| 020 | F, 52 | IV | ex vivo | ND | Resections, radiotherapy, temozolomide | Chemotherapy, radiotherapy | data not available | Alive 6 months post-resection |
| RMH | ||||||||
| 021 | M, 66 | IV | ex vivo | ND | Nil | Radiotherapy and temozolomide | data not available | Alive 4 months post-resection |
| RMH | ||||||||
| 022 | F, 54 | IV | ex vivo | ND | Nil | Radiotherapy | data not available | Died 3 months post-resection |
| RMH | ||||||||
| 023 | M, 58 | IV | ex vivo | ND | Nil | Radiotherapy and temozolomide | data not available | Alive 4 months post-resection but recurrence |
HRM=high-resolution melt; M=mutation possibly affecting p53 function; ND=not done; WT=wild type; M1=silent mutation; M2=mutation predicted by HRM analysis but not identified by sequencing. For details see Supplementary Figure 1.
p53 genotype, as determined by HRM analysis and sequencing.
The ‘D’ series of early passage lines was derived from specimens obtained from patients who had undergone tumour resection at Duke University Hospital (Durham, NC, USA). Informed consent was obtained from each patient prior to surgery in accordance with Duke Internal Review Board stipulations. The tumour material was collected in DMEM, 10% foetal bovine serum (FBS), 0.05 mg ml−1 gentamycin. Tumour samples were drained, placed in a 100 mm tissue culture dish and minced with sterile scissors. Warm sterile-filtered 0.4% collagenase solution (0.4% collagenase, 0.05 mg ml−1 gentamycin in zinc option-MEM, ZO-MEM) (Invitrogen, Carlsbad, CA, USA) was added to the minced tissue and incubated at 37°C for 1 h. Collagenase solution was inactivated by the addition of ZO-MEM, 10% FBS, 0.05 mg ml−1 gentamycin. Minced tissue was titurated to further homogenise sample and then centrifuged (1000 r.p.m., 5 min). Collagenase and media were removed, cells were re-suspended in fresh media and transferred to a 60-mm tissue culture dish and incubated at 37°C, 5% CO2. Cell cultures with a large RBC fraction were treated with haemolysis solution (0.83% ammonium chloride) as follows: cells were trypsinized and centrifuged (1000 r.p.m., 7 min), supernatant was discarded and cells were re-suspended in 2 ml FBC. Haemolysis solution was added at a ratio of 1 : 5 to 1 : 10. Haemolysis mixture was incubated at 4°C for 10 min, additional FBS was then added to bathe cells. Solution was centrifuged (1000 r.p.m., 7 min), following which the supernatant was discarded and the remaining cells were re-suspended in ZO-MEM, supplemented as described earlier. Tumour cultures were serially passaged using 0.25% trypsin-EDTA and collected in freezing medium (12.5% DMSO, 50% FBS and 37.5% ZO-MEM).
The early passage lines LM-G-2, LM-G-4 and LM-G-8 were made from tumours resected at the Austin Hospital (Heidelberg, VIC, Australia). Patients with known or suspected glioblastoma multiforme (GBM) were prospectively entered into a clinical trial after written informed consent was obtained. Ethics approval was granted by the Austin Hospital Human Research Ethics Committee. After intra-operative confirmation of a diagnosis of GBM, fresh tissue samples were obtained by biopsy or resection of tumour. Samples were mechanically disaggregated using the Medimachine (DAKO Diagnostika GmbH, Hamburg, Germany) (Brockhoff et al, 1999) and introduced into pre-warmed DMEM (Life Technologies, Grand Island, NY, USA) containing 10% FBS (CSL, Melbourne, VIC, Australia), 2 mM glutamine (Sigma Chemical Co, St Louis, MO, USA) and 50Uml−1 penicillin/ 50μgml−1 streptomycin, respectively (Life Technologies). After 24 h, any non-adherent cells and material were discarded and the media replenished. Media were replenished twice weekly or more frequently if required. When cells appeared to have reached 50% confluence or maximal confluency in a T25 flask for that cell line, they were expanded into a T75 flask (passage 2). Cells were also expanded into a T75 (passage 3) flask when they reached 50% confluence or maximal confluency for that cell line. Thereafter, cells were expanded into T175 flask (passage 4) for cryostorage, experimentation or propagation as required.
Normal human hepatocytes and astrocytes were purchased from Cambrex (East Rutherford, NJ, USA). The established glioma cell lines D270 and U373 have been characterized previously (Knight et al, 2001, 2004). LN18 cells were purchased from the ATCC (Manassas, VA, USA).
Drug treatments
We endeavoured to use physiologically relevant drug concentrations in this study. Cells were exposed to doses corresponding to 100% and 10% of peak plasma or tumour concentrations (Table 2). Data regarding the pharmacokinetics of the various TRAIL formulations in humans have not yet been published. We used soluble TRAIL (Peprotech, Rocky Hill, CT, USA) at concentrations commonly employed in vitro (1 μg ml−1 and 100 ng ml−1). We arbitrarily chose to use F-LZ-TRAIL (Knight et al, 2001) at 10-fold lower doses than soluble TRAIL (100 and 10 ng ml−1), because our previous in vitro analyses showed that it is more potent than the untagged formulation (data not shown). Superkiller TRAIL (Alexis Biochemicals, Lausen, Switzerland) was used at 100 ng ml−1.
Table 2. Chemotherapy drugs and doses used in this study.
| Drug | Concentrations used in this study | Published human peak intratumour or plasma concentrations |
|---|---|---|
| Soluble TRAIL | 1 μg ml−1 100 ng ml−1 | Not reported |
| F-LZ-TRAIL | 100 ng ml−1 10 ng ml−1 | Not reported |
| Superkiller TRAIL | 100 ng ml−1 | Not reported |
| Anti-DR5 | 3 μg ml−1 0.3 μg ml−1 | Not reported |
| Cisplatin | 54 μg ml−1 5.4 μg ml−1 | Peak tumour concentration after embolisation was 54 μg ml−1, after perfusion was 11.4 μg ml−1 (Tegeder et al, 2003). Peak plasma concentrations ranged from 1.5 μg ml−1 (Riva et al, 2000; Urien et al, 2005) to around 4 μg ml−1 (Siegel-Lakhai et al, 2005; Watanabe et al, 2003) |
| Carboplatin | 44 μg ml−1 4.4 μg ml−1 | Peak glioma concentration was 13 μg ml−1, peak plasma concentration was 44 μg ml−1 (Whittle et al, 1999) |
| CCNU | 9 μg ml−1 900 ng ml−1 90 ng ml−1 | Peak plasma concentration of active metabolites was reported to be 9 μg ml−1 (Lee et al, 1985) or 1–2 μg ml−1 (Kastrissios et al, 1996) |
| Temozolomide | 13.7 μg ml−1 1.37 μg ml−1 | Peak plasma concentration was 13.7 μg ml−1 (Brada et al, 1999) |
| Etoposide | 10.5 μg ml−1 1.05 μg ml−1 | Peak tumour concentration was 1.04–4.80 μg g−1. Peak plasma concentration was 7–10.5 μg ml−1 (Kiya et al, 1992) |
| Vincristine | 40.4 ng ml−1 4 ng ml−1 | Peak plasma concentration was 40.5 ng ml−1 but rapidly decreased to 5 ng ml−1 (Groninger et al, 2005) |
| Procarbazine | 540 ng ml−1 54 ng ml−1 | Peak plasma concentration was 540 ng ml−1 (He et al, 2004) |
Cell death/survival assays
During the experiments performed for this study, all cells were cultured in ZO-MEM supplemented with 10% FBS (SAFC Biosciences, Sydney, NSW, Australia). Cells were incubated with drugs for 48 h. The CellTiter-Glo kit (Promega, Madison, WI, USA) was used to quantitate survival, according to the manufacturer's instructions. Five hundred cells were used per treatment. Fifty thousand cells were used per condition for propidium exclusion assays (Knight et al, 2001), which were analysed using an LSRII (BD Biosciences, San Jose, CA, USA).
Caspase activity assay
Ten thousand cells were incubated with normal media or TRAIL-based drugs in 96-well plates for 6 h, then caspase (DEVDase) activity was detected using the Caspase-Glo 3/7 kit (Promega), according to the manufacturer's instructions. Cell-specific luminescence signals were obtained by subtracting the signal generated from plates containing media or drugs but no cells from the signal obtained from wells containing cells and drugs.
Immunoblotting
One hundred thousand cells were lysed, subjected to SDS–PAGE, immunoblotted and signals quantitated using previously published protocols (Ashley et al, 2005). The following antibodies were used: rabbit anti-DR4 and anti-DR5 from ProSci (San Diego, CA, USA) (no. 1139 and no. 2019, respectively), mouse anti-caspase-8 and anti-cFLIP from Alexis (Lausen, Switzerland) (clones 12F5 and NF6, respectively), mouse anti-FADD from BD Transduction Laboratories (San Jose, CA, USA) (clone 1/FADD), mouse anti-XIAP from MBL (Woburn, MA, USA) (clone 2F1), mouse anti-GAPDH from Chemicon (North Ryde, NSW, Australia) (clone 6C5), rabbit anti-p53 from Cell Signaling (Danvers, MA, USA) (no. 9282), goat anti-mouse-HRP (Sigma, no. A2304) and goat anti-rabbit-HRP (BD Biosciences no. 554021). Control lysates from 293T cells transiently transfected with plasmids directing the expression of caspase-8, FADD, cFLIPL were generated as previously reported (Ashley et al, 2005). Similar control lysates were made using expression plasmids encoding XIAP, DR4 (kindly provided by Paul Ekert) and DR5. pIRES-PL-XIAP was synthesised as follows. Oligonucleotides 1 and 2 were annealed and ligated into pIRES-Neo (Clontech, Mountain View, CA, USA) cut with BamHI and NotI, to yield pIRES-PL. The coding region of XIAP was amplified with primers 3 and 4, cut with EcoRI and NotI and ligated into EcoRI/NotI cut pIRES-PL, generating pIRES-PL-XIAP. pIRES-Neo-DR5 was made by amplifying the DR5 coding region with primers 5 and 6, cutting with EcoRI and BamHI and ligating into pIRES-Neo (Clontech).
Oligonucleotides:
- 1:
5′-GGCCGAATTCGCGGGATCCGCGCGCTAGCAGCTGCGGCCGCAGGCCT-3′;
- 2:
5′-GATCAGGCCTGCGGCCGCAGCTGCTAGCGCGCGGATCCCGCGAATTC-3′;
- 3:
5′-GGAATTCCGCCATGACTTTTAACAGTTTTGAAGG-3′;
- 4:
5′-CCCCCGCGGCCGCTTAAGACATAAAAATTTTTTGCTTG-3′;
- 5:
5′-GGAATTCCGCCATGGAACAACGGGGACAG-3′; and
- 6:
5′-GCGGATCCTTAGGACATGGCAGAGTC-3′.
p53 genotyping
Genomic DNA was extracted from frozen cell pellets (D2234MG, D2235MG, D2238MG, D2245MG, D2247MG, LM-G-4 and LM-G-8) or frozen cell suspensions (D2239MG, D2248MG, D2259MG, D2261MG, D2262MG and D2268MG, D2301MG) using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. PCR cycling and high-resolution melt (HRM) analysis were performed on the Rotor-Gene 6000 (Corbett Research, Sydney, NSW, Australia). Each sample was analysed in triplicate. High-resolution melt analysis of exons 5–8 was performed as described previously (Krypuy et al, 2007). The amplicon of exon 4 (176 bp) covers the DNA binding domain and was generated using the primers TP53-Exon4-DBD-F, 5′-CCCCTGCACCAGCAGCTCCTA-3′ and TP53-Exon4-DBD-R, 5′-CAGCCCCTCAGGGCAACTGA-3′. The amplified region corresponds to GenBank accession number AC087388, nucleotides 78962–79137. PCR was performed in a 100 μl PCR tube (Corbett Research) with a final volume of 20 μl, containing 200 nmol l−1 of the forward primer, 300 nmol l−1 of the reverse primer, 200 μmol l−1 of each dNTP, 0.5 U of HotStarTaq DNA Polymerase (Qiagen) in the supplied PCR buffer containing 2.0 mmol l−1 MgCl2, 5 μmol l−1 SYTO9 (Invitrogen) and 2.5 ng of genomic DNA as template. The initial denaturation (95°C, 15 min) was followed by 11 cycles of 15 s at 95°C, 15 s at 65–60°C touchdown (0.5°C per cycle), 20 s at 72°C and 39 cycles of 15 s at 95°C, 15 s at 60°C, 20 s at 72°C; one cycle of 1 min at 95°C, 72°C for 1.5 min and a HRM step from 72 to 95°C rising at 0.2°C per second, and holding for 1 s after each stepwise increment. To confirm the mutation positive HRM results, PCR products of the entire exon 5 (exons 5a and 5b) and the HRM products of exons 6 and 8 were purified, directly sequenced in both directions and analysed as described previously (Krypuy et al, 2007).
Results
TRAIL sensitivity
Cells from freshly resected gliomas, minimally passaged glioma cell lines, established glioma cell lines, normal astrocytes and hepatocytes were exposed to three formulations of TRAIL or an agonistic antibody, alone or in combination with seven chemotherapy drugs. Table 1 provides details of the glioma cells used and the patients from whom they were obtained. The normal cells tolerated exposure to ‘hepatosafe’ soluble TRAIL, the anti-DR5 antibody and the lower dose of cross-linked TRAIL (Figure 1A). Higher concentrations of cross-linked TRAIL and superkiller TRAIL were lethal to both types of normal cells, with hepatocytes being especially sensitive. As sole agents, the TRAIL formulations and anti-receptor antibody induced negligible cell death in most of the glioma samples tested. Only one of the early passage lines, D2247, was efficiently killed by the two cross-linked formulations of TRAIL and the anti-DR5 antibody. This line also displayed intermediate sensitivity to soluble TRAIL. Two other lines, D2234 and D2245, were somewhat sensitive to the cross-linked TRAIL formulations and the agonistic antibody, but not to soluble TRAIL. None of the ex vivo samples was substantially sensitive to any of the TRAIL-based treatments. As reported previously, LN18 and D270 were TRAIL-sensitive, but U373 was TRAIL-resistant (Hawkins, 2004). Consistent with the notion that apoptosis was responsible for the reductions in ATP levels observed in some drug-treated cells, caspase activity in D2247 cells but not in D2302 cells increased following exposure to TRAIL or anti-DR5 (Figure 1B).
Figure 1.
In vitro responses of glioma cells, astrocytes and hepatocytes to TRAIL. (A) Cells from the indicated early passage or established glioma cell lines, ex vivo gliomas, normal astrocytes or normal hepatocytes were incubated in vitro with TRAIL or with anti-DR5 antibody. Black triangles indicate high and low drug concentrations, when applicable (see Table 2 and the Materials and Methods section). Survival was assayed using the CellTiter Glo kit and depicted using ‘bubble’ graphs. The areas of the circles denote net survival following each treatment, relative to untreated cells (set at 100%, left column). Small circles indicate efficient killing, large circles reflect survival and/or proliferation, as illustrated in the graphical legend. Glioma assays were performed in duplicate (data are represented by circles). Four replicates were performed for hepatocytes and eight replicates for astrocytes. For astrocyte and hepatocyte data, grey circles depicting average survival are overlaid upon black circles indicating average survival plus standard error. (B) DEVDase activity in D2247 and D2302 cells was monitored 6 h following treatment with the specified TRAIL formulations, anti-DR5 antibody or normal media.
Cooperation between TRAIL and chemotherapy drugs
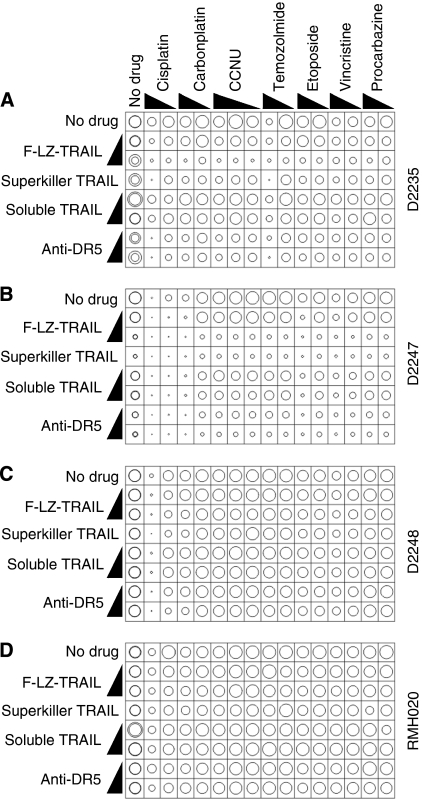
Previous studies have shown that co-treatment with traditional anti-cancer agents can sensitise some cells to TRAIL, in vitro and in vivo. We tested the ability of the various TRAIL formulations to kill glioma cells in conjunction with a number of chemotherapy drugs used in glioma therapy (Table 2). Figure 2 illustrates the effect of these combination treatments on D2247 (the most TRAIL-sensitive line), D2235 and D2248 (two of the TRAIL resistant lines) and RMH020 (one of the uncultured tumours). Average responses across all early passage lines and ex vivo tumours are shown in Figure 3. Many samples were killed by high-dose cisplatin, however a 10-fold lower concentration was much less effective. The higher dose of vincristine was weakly toxic to many of the glioma samples. Only the D2235 cells were markedly sensitive to temozolomide. The other drugs were ineffective as sole agents. All chemotherapy drugs tested further sensitised D2247 to F-LZ-TRAIL and anti-DR5 (Figure 2), but only additive toxicity was observed when TRAIL-resistant cells were exposed to the combination treatments (Figures 2 and 3 and data not shown). The possibility that prior treatment with chemotherapy drugs may enhance sensitivity to TRAIL was also explored. Cells from a TRAIL-resistant early passage line, D2302, were incubated with chemotherapy drugs only for 24 h, then TRAIL or anti-DR5 antibody was added for an additional 48 h period. These treatments had similar effects on cellular ATP levels to co-incubations with TRAIL plus chemotherapy drugs for either 48 or 72 h (Supplementary Figure 1), indicating that prior exposure to chemotherapy drugs did not sensitise D2302 cells to TRAIL. Propidium iodide uptake assays were performed on many of the samples, using selected drug combinations. This method, which gives a direct measure of the proportion of cells killed, yielded similar data to the CellTiter-Glo assay, which quantifies cellular ATP (Figure 4).
Figure 2.
In vitro sensitivity of three early passage glioma cell lines and one ex vivo tumour to TRAIL in combination with chemotherapy drugs. Cells from the early passage lines D2235 (A), D2247 (B) and D2248 (C) and the freshly resected glioma RMH020 (D) were incubated in vitro with the stated formulations of TRAIL or anti-DR5 antibody, alone or together with the listed chemotherapy drugs as described in the Materials and Methods section and Table 2. The resulting survival was assayed and graphed as described in the legend to Figure 1.
Figure 3.
In vitro sensitivity of glioma cells to TRAIL in combination with chemotherapy drugs. Cells from 17 early passage glioma cell lines (A) and 5 uncultured gliomas (B) were incubated in vitro with the stated formulations of TRAIL or anti-DR5 antibody, alone or together with the listed chemotherapy drugs. The resulting survival was assayed and graphed as described in the legend to Figure 1. Grey circles depicting average survival are overlaid upon black circles indicating average survival plus standard error.
Figure 4.
Propidium iodide uptake assay of glioma cell sensitivity to combination treatments. Cells from the indicated early passage glioma cell lines or ex vivo gliomas were incubated in vitro with soluble TRAIL at 100 ng ml−1 (+) or 1000 ng ml−1 (++) alone or together with temozolomide (13.7 μg ml−1) or cisplatin (54 μg ml−1) for 48 h. Flow cytometry measurement of propidium iodide exclusion was used to quantitate the proportion of surviving cells. The areas of the circles denote survival following each treatment. Small circles indicate efficient killing, large circles reflect survival.
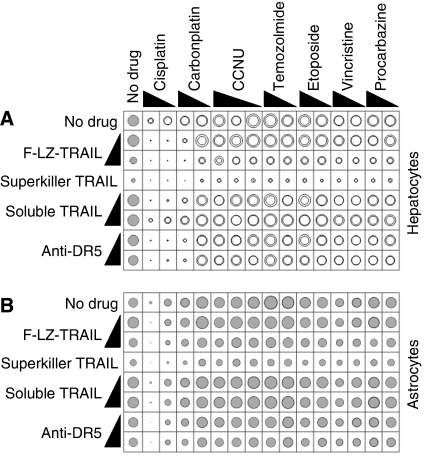
Normal cells
As previously published (Ashkenazi et al, 1999; Jo et al, 2000; Lawrence et al, 2001; Mori et al, 2004; Ganten et al, 2006), normal human hepatocytes were sensitive to cross-linked TRAIL formulations, but not to soluble untagged TRAIL (Figure 1). Hepatocytes were also efficiently killed by cisplatin and carboplatin (Figure 5). In general, chemotherapy drugs did not further sensitise hepatocytes to TRAIL, although treating hepatocytes with high-dose F-LZ-TRAIL and the chemotherapy drugs elicited a slightly superadditive effect (Figure 5). Normal human astrocytes were also sensitive to cross-linked TRAIL, cisplatin and carboplatin, but not to the same extent as hepatocytes. No significant cooperation in astrocyte lethality was noted between TRAIL and the chemotherapy drugs (Figure 5).
Figure 5.
In vitro sensitivity of astrocytes and hepatocytes to TRAIL in combination with chemotherapy drugs. Normal human hepatocytes (A) and astrocytes (B) were incubated in vitro with the stated formulations of TRAIL or anti-DR5 antibody, alone or together with the listed chemotherapy drugs. The resulting survival was assayed and graphed as described in the legend to Figure 1. (A) Quadruplicate assays were performed to examine hepatocyte survival following incubation with each TRAIL formulation alone. Grey circles depicting average survival are overlaid upon black circles indicating average survival plus standard error. Responses to combination treatment were assayed in duplicate; circles depict each result. (B) Eight replicates were performed to investigate astrocyte survival following incubation with each TRAIL formulation alone. Combination treatments were tested in quadruplicate. Grey circles depicting average survival are overlaid upon black circles indicating average survival plus standard error.
On average, the minimally cultured and uncultured glioma cells were as sensitive or less sensitive than the normal cells to TRAIL-based drugs, alone or in combination with chemotherapeutic agents. However, isolated examples of selective toxicity to glioma cells relative to normal cells were observed (Figure 6). TRAIL formulations combined with platinum-based drugs killed cells from a few gliomas (D2234, D2247, LM-G-8 and LM-G-2) at least 10 times more efficiently than normal astrocytes and hepatocytes. Temozolomide cooperated with TRAIL to kill D2235 cells more efficiently than the normal cells. Some selectivity of TRAIL/etoposide and TRAIL/vincristine combinations was observed for D2247 relative to normal cells.
Figure 6.
Treatments selectively toxic in vitro to glioma cells relative to normal cells. Coloured circles indicate gliomas killed in vitro by each treatment at least 3 times (A, C) or 10 times (B, D) more efficiently than the most sensitive astrocyte replicate (A, B) or hepatocyte replicate (C, D).
Pathway analyses
To explore potential mechanisms underlying the resistance of most of the gliomas to TRAIL-induced apoptosis, we surveyed minimally passaged gliomas for the expression of the TRAIL pathway components DR4 (TRAIL-R1), DR5 (TRAIL-R2), FADD and caspase-8, along with potential modulators of TRAIL signalling (cFLIP and XIAP) (Figure 7A–7D). None of the lines expressed detectable DR4 (data not shown) or cFLIPS (Figure 7E). Expression of the other components varied widely between samples. Four of the early passage lines that were TRAIL-resistant (D2259, D2261, D2262 and D2264) did not express detectable FADD. The TRAIL-sensitive line D2247 expressed relatively high levels of DR5 and XIAP and detectable, if relatively low, levels of FADD, caspase-8 and cFLIPL. D2235 and D2301 also expressed low levels of cFLIPL. The p53 status of the majority of lines was also examined. Mutations that may affect function were identified in four of the lines (D2234, D2235, LM-G-4 and LM-G-8) (Supplementary data). D2247 was the only line of those tested to express sufficient p53 to detect by immunoblotting (Figure 7E).
Figure 7.
Immunoblot analyses of candidate TRAIL signalling regulators. Immunoblotting was performed on lysates from the indicated glioma early passage cell lines or 293T cells transiently transfected with expression plasmids encoding the various apoptotic pathway components. (A–D) Anti-DR5 (A), anti-caspase-8 (B), anti-FADD (C) and anti-XIAP (D) signals were quantitated using a chemidoc instrument and plotted relative to the 293T transfectant lysates (set at 100%). A nonspecific band detected by the anti-DR5 antibody is indicated by an asterisk. Long exposures using autoradiograph film revealed some signals too weak to be detected by chemidoc (+). Illustrative immunoblots are inset within each graph. (E) Autoradiography was used to assay cFLIPL and p53 expressions in early passage lines and 293T cells transfected with the cFLIPL expression plasmid (cFLIPL, GAPDH immunoblots) or empty vector (p53 immunoblot). Irrelevant lanes separating the 293T transfectant signals from those of the early passage lines have been removed.
Discussion
Two conditions would have to be met for TRAIL to be clinically effective for treating malignant glioma: (a) a route of administration must be used that delivers concentrations of TRAIL that are lethal to the patient's glioma cells in vivo and (b) the glioma cells must be markedly more sensitive to TRAIL than normal cells exposed via that mode of delivery. Any treatment for brain tumours must transverse or bypass the blood–brain barrier. This means that any future TRAIL-based therapies for glioma would probably be administered intracranially. Intracranial delivery may also lessen hepatocyte exposure and thus reduce hepatotoxicity. Multiple intracranial delivery systems are being developed. The post-resection tumour cavity can be lined with drug-impregnated wafers (Westphal et al, 2006). Convection-enhanced delivery is a promising new technique in which drugs are infused at the tumour site under pressure, thus improving distribution into the mass of the tumour (Lopez et al, 2006). Mice bearing intracranial glioma xenografts were successfully treated with TRAIL administered using this approach (Saito et al, 2004).
Numerous studies have concluded that TRAIL is a promising anti-glioma drug based on the investigation of TRAIL sensitivity and signalling in established glioma cell lines. However, it has been reported that melanoma cells exhibited enhanced TRAIL sensitivity following in vitro culture (Nguyen et al, 2001). To minimise the potential for in vitro culturing artefacts, in this study we tested the TRAIL sensitivity of minimally cultured and freshly resected gliomas. Our analyses imply that minimally passaged and uncultured gliomas respond similarly to TRAIL. It is, however, possible that prolonged in vitro culturing, as with the commonly studied established glioma lines, may significantly affect TRAIL sensitivity.
Minimally cultured and uncultured glioma cells were generally resistant to the TRAIL formulations tested. None of the tumours tested was efficiently killed by the ‘hepatosafe’ formulation of TRAIL currently being evaluated in early-phase clinical trials. Three of the gliomas were sensitive to cross-linked formulations of TRAIL: D2234, D2245 and D2247. Intriguingly, the patients from whose tumours those lines were derived had all received chemotherapy before surgery. In contrast, only one patient whose tumour was TRAIL-resistant received treatment prior to resection (RMH020). Unfortunately, normal astrocytes and hepatocytes were also sensitive to cross-linked TRAIL. Only one glioma (D2247) was killed by cross-linked TRAIL more efficiently than normal astrocytes.
Four of the early passage lines lacked detectable FADD, possibly accounting for their TRAIL resistance. The TRAIL-sensitive line D2247 bore only low levels of FADD and caspase-8, arguing that low concentrations of these pathway components can be sufficient for TRAIL-induced apoptotic signalling. D2247 was one of a number of lines lacking mutations in p53, and the only line tested to express p53 levels detectable by immunoblotting. Consistent with this observation, D2247 also expressed high levels of DR5, a known p53-inducible protein (Wu et al, 1997). LM-G-4, a TRAIL resistant line, expressed higher levels of DR5, caspase-8 and FADD than D2247, arguing that factors other than the levels of these proteins influence TRAIL sensitivity in glioma cells. The expression of the potential TRAIL inhibitors XIAP and cFLIP was higher in the TRAIL-sensitive D2247 cells than the resistant lines, arguing against overexpression of these proteins as a mechanism of resistance in gliomas that survived incubation with TRAIL. Definition of the molecular mechanisms contributing to the resistance of the majority of the gliomas to TRAIL will require additional investigation, but it seems unlikely that a single resistance mechanism, perhaps amenable to therapeutic manipulation, will be found to account for the widespread survival of glioma cells following exposure to TRAIL.
Better therapies are urgently needed for malignant glioma. In vitro sensitivity assays could be used for preclinical evaluation of the anti-glioma potential of new drugs. In the future, such assays could also assist in the selection of the most effective drug combinations for individual patients. Our data imply that few glioma patients would benefit from TRAIL-based therapies; perhaps in vitro sensitivity testing could help identify the minority of patients most likely to respond. The luminescence assay used in this study is rapid, high-throughput and requires fewer cells than the commonly employed MTT and flow cytometric assays, thus allowing more drug doses and combinations to be tested per sample. The accuracy with which in vitro sensitivity testing predicts in vivo responses may be influenced by the mechanism of action of the particular drug as well as the degree to which cellular environment influences the toxicity of each agent to glioma cells. For example, glioma cell interactions with surrounding cells and the extracellular matrix could modulate the apoptosis-inducing capacity of anti-cancer drugs in vivo. For these reasons, it is also important to examine orthotopic models of cancer. Notwithstanding these considerations, in vitro apoptosis data do tend to correlate with patient responses in cancer types for which truly effective drugs exist (Nagourney, 2006). The dearth of effective drugs for treating glioma has limited assessment of the predictive value of in vitro sensitivity testing for this tumour type. Nevertheless, available evidence does argue that in vitro sensitivity testing can assist in selecting treatments for glioblastoma patients (Iwadate et al, 2003).
Currently, the majority of glioblastoma patients receive surgical resection, radiotherapy and temozolomide. Although temozolomide may benefit some patients, it is well recognised that the majority of patients do not respond to this drug. Temozolomide administration only extended median survival of glioblastoma patients from 12.1 to 14.6 months post-diagnosis, boosting 2-year survival from 10.4 to 26.5% (Stupp et al, 2005). Given this subtle effect in vivo, it is perhaps not surprising that only one of the tumours tested in this study (D2235) was efficiently killed by temozolomide in vitro. Cisplatin was the most effective of the drugs tested in vitro, however strong toxicity was triggered only by the higher of the doses employed, which corresponded to the peak intratumoral cisplatin level following embolisation (Tegeder et al, 2003). Only partial sensitivity was observed using a 10-fold lower concentration, which resembles peak tumour and plasma levels achieved following systemic cisplatin administration (Riva et al, 2000; Tegeder et al, 2003; Watanabe et al, 2003; Siegel-Lakhai et al, 2005). A few gliomas were more sensitive than normal cells to co-treatments with TRAIL and chemotherapy drugs.
In conclusion, our data indicate that TRAIL-based therapies would be unlikely to benefit the majority of glioma patients. This study does, however, suggest that particular patients may respond to specific combinations of TRAIL and chemotherapy drugs. In vitro sensitivity assays may prove useful in identifying such patients and predicting effective drug combinations.
Acknowledgments
We are very grateful to Stan Stylli for help with tumour acquisition, to Sarah Roberts for technical assistance and to John Silke and Don Phillips for providing reagents. This study was funded by grants from the Cancer Council Victoria (to CJH, DMA and HSF), Cure-for-Life Foundation (to CJH) and ANZ Trustees (to CJH).
Footnotes
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary Material
References
- Anderson RC, Elder JB, Brown MD, Mandigo CE, Parsa AT, Kim PD, Senatus P, Anderson DE, Bruce JN (2002) Changes in the immunologic phenotype of human malignant glioma cells after passaging in vitro. Clin Immunol 102: 84–95 [DOI] [PubMed] [Google Scholar]
- Arizono Y, Yoshikawa H, Naganuma H, Hamada Y, Nakajima Y, Tasaka K (2003) A mechanism of resistance to TRAIL/Apo2L-induced apoptosis of newly established glioma cell line and sensitisation to TRAIL by genotoxic agents. Br J Cancer 88: 298–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashkenazi A, Pai RC, Fong S, Leung S, Lawrence DA, Marsters SA, Blackie C, Chang L, McMurtrey AE, Hebert A, DeForge L, Koumenis IL, Lewis D, Harris L, Bussiere J, Koeppen H, Shahrokh Z, Schwall RH (1999) Safety and antitumor activity of recombinant soluble Apo2 ligand. J Clin Invest 104: 155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashley DM, Riffkin CD, Muscat AM, Knight MJ, Kaye AH, Novak U, Hawkins CJ (2005) Caspase-8 is absent or low in many ex vivo gliomas. Cancer 104: 1487–1496 [DOI] [PubMed] [Google Scholar]
- Brada M, Judson I, Beale P, Moore S, Reidenberg P, Statkevich P, Dugan M, Batra V, Cutler D (1999) Phase I dose-escalation and pharmacokinetic study of temozolomide (SCH 52365) for refractory or relapsing malignancies. Br J Cancer 81: 1022–1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockhoff G, Fleischmann S, Meier A, Wachs FP, Hofstaedter F, Knuechel R (1999) Use of a mechanical dissociation device to improve standardization of flow cytometric cytokeratin DNA measurements of colon carcinomas. Cytometry 38: 184–191 [DOI] [PubMed] [Google Scholar]
- Eramo A, Pallini R, Lotti F, Sette G, Patti M, Bartucci M, Ricci-Vitiani L, Signore M, Stassi G, Larocca LM, Crino L, Peschle C, De Maria R (2005) Inhibition of DNA methylation sensitizes glioblastoma for tumor necrosis factor-related apoptosis-inducing ligand-mediated destruction. Cancer Res 65: 11469–11477 [DOI] [PubMed] [Google Scholar]
- Fulda S, Meyer E, Debatin KM (2002a) Inhibition of TRAIL-induced apoptosis by Bcl-2 overexpression. Oncogene 21: 2283–2294 [DOI] [PubMed] [Google Scholar]
- Fulda S, Wick W, Weller M, Debatin KM (2002b) Smac agonists sensitize for Apo2L/TRAIL- or anticancer drug-induced apoptosis and induce regression of malignant glioma in vivo. Nat Med 8: 808–815 [DOI] [PubMed] [Google Scholar]
- Ganten TM, Koschny R, Sykora J, Schulze-Bergkamen H, Buchler P, Haas TL, Schader MB, Untergasser A, Stremmel W, Walczak H (2006) Preclinical differentiation between apparently safe and potentially hepatotoxic applications of TRAIL either alone or in combination with chemotherapeutic drugs. Clin Cancer Res 12: 2640–2646 [DOI] [PubMed] [Google Scholar]
- Glioma Meta-analysis Trialists Group (2002) Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 359: 1011–1018 [DOI] [PubMed] [Google Scholar]
- Groninger E, Meeuwsen-de Boer T, Koopmans P, Uges D, Sluiter W, Veerman A, Kamps W, de Graaf S (2005) Vincristine pharmacokinetics and response to vincristine monotherapy in an up-front window study of the Dutch Childhood Leukaemia Study Group (DCLSG). Eur J Cancer 41: 98–103 [DOI] [PubMed] [Google Scholar]
- Hao C, Beguinot F, Condorelli G, Trencia A, Van Meir EG, Yong VW, Parney IF, Roa WH, Petruk KC (2001) Induction and intracellular regulation of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) mediated apoptosis in human malignant glioma cells. Cancer Res 61: 1162–1170 [PubMed] [Google Scholar]
- Hawkins CJ (2004) TRAIL and malignant glioma. Vitamins and Hormones 67: 427–452 [DOI] [PubMed] [Google Scholar]
- He X, Batchelor TT, Grossman S, Supko JG (2004) Determination of procarbazine in human plasma by liquid chromatography with electrospray ionization mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 799: 281–291 [DOI] [PubMed] [Google Scholar]
- Iwadate Y, Fujimoto S, Namba H, Yamaura A (2003) Promising survival for patients with glioblastoma multiforme treated with individualised chemotherapy based on in vitro drug sensitivity testing. Br J Cancer 89: 1896–1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeremias I, Steiner HH, Benner A, Debatin KM, Herold-Mende C (2004) Cell death induction by betulinic acid, ceramide and TRAIL in primary glioblastoma multiforme cells. Acta Neurochir (Wien) 146: 721–729 [DOI] [PubMed] [Google Scholar]
- Jo M, Kim TH, Seol DW, Esplen JE, Dorko K, Billiar TR, Strom SC (2000) Apoptosis induced in normal human hepatocytes by tumor necrosis factor-related apoptosis-inducing ligand. Nat Med 6: 564–567 [DOI] [PubMed] [Google Scholar]
- Kastrissios H, Chao NJ, Blaschke TF (1996) Pharmacokinetics of high-dose oral CCNU in bone marrow transplant patients. Cancer Chemother Pharmacol 38: 425–430 [DOI] [PubMed] [Google Scholar]
- Kischkel FC, Hellbardt S, Behrmann I, Germer M, Pawlita M, Krammer PH, Peter ME (1995) Cytotoxicity-dependent APO-1 (Fas/CD95)-associated proteins form a death-inducing signaling complex (DISC) with the receptor. Embo Journal 14: 5579–5588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiya K, Uozumi T, Ogasawara H, Sugiyama K, Hotta T, Mikami T, Kurisu K (1992) Penetration of etoposide into human malignant brain tumors after intravenous and oral administration. Cancer Chemother Pharmacol 29: 339–342 [DOI] [PubMed] [Google Scholar]
- Knight ME, Riffkin CD, Ekert PG, Ashley DM, Hawkins CJ (2004) Caspase-8 levels affect necessity for mitochondrial amplification in death ligand-induced glioma cell apoptosis. Mol Carcinog 39: 173–182 [DOI] [PubMed] [Google Scholar]
- Knight MJ, Riffkin CD, Muscat AM, Ashley DM, Hawkins CJ (2001) Analysis of FasL and TRAIL induced apoptosis pathways in glioma cells. Oncogene 20: 5789–5798 [DOI] [PubMed] [Google Scholar]
- Koschny R, Holland H, Sykora J, Haas TL, Sprick MR, Ganten TM, Krupp W, Bauer M, Ahnert P, Meixensberger J, Walczak H (2007) Bortezomib sensitizes primary human astrocytoma cells of WHO Grades I–IV for tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis. Clin Cancer Res 13: 3403–3412 [DOI] [PubMed] [Google Scholar]
- Krypuy M, Ahmed AA, Etemadmoghadam D, Hyland SJ, DeFazio A, Fox SB, Brenton JD, Bowtell DD, Dobrovic A (2007) High resolution melting for mutation scanning of TP53 exons 5-8. BMC Cancer 7: 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D, Shahrokh Z, Marsters S, Achilles K, Shih D, Mounho B, Hillan K, Totpal K, DeForge L, Schow P, Hooley J, Sherwood S, Pai R, Leung S, Khan L, Gliniak B, Bussiere J, Smith CA, Strom SS, Kelley S, Fox JA, Thomas D, Ashkenazi A (2001) Differential hepatocyte toxicity of recombinant Apo2L/TRAIL versions. Nat Med 7: 383–385 [DOI] [PubMed] [Google Scholar]
- Lee FY, Workman P, Roberts JT, Bleehen NM (1985) Clinical pharmacokinetics of oral CCNU (lomustine). Cancer Chemother Pharmacol 14: 125–131 [DOI] [PubMed] [Google Scholar]
- Lee J, Kotliarova S, Kotliarov Y, Li A, Su Q, Donin NM, Pastorino S, Purow BW, Christopher N, Zhang W, Park JK, Fine HA (2006) Tumor stem cells derived from glioblastomas cultured in bFGF and EGF more closely mirror the phenotype and genotype of primary tumors than do serum-cultured cell lines. Cancer Cell 9: 391–403 [DOI] [PubMed] [Google Scholar]
- Leverkus M, Neumann M, Mengling T, Rauch CT, Brocker EB, Krammer PH, Walczak H (2000) Regulation of tumor necrosis factor-related apoptosis-inducing ligand sensitivity in primary and transformed human keratinocytes. Cancer Res 60: 553–559 [PubMed] [Google Scholar]
- Li YC, Tzeng CC, Song JH, Tsia FJ, Hsieh LJ, Liao SJ, Tsai CH, Van Meir EG, Hao C, Lin CC (2006) Genomic alterations in human malignant glioma cells associate with the cell resistance to the combination treatment with tumor necrosis factor-related apoptosis-inducing ligand and chemotherapy. Clin Cancer Res 12: 2716–2729 [DOI] [PubMed] [Google Scholar]
- Longley DB, Johnston PG (2005) Molecular mechanisms of drug resistance. J Pathol 205: 275–292 [DOI] [PubMed] [Google Scholar]
- Lopez KA, Waziri AE, Canoll PD, Bruce JN (2006) Convection-enhanced delivery in the treatment of malignant glioma. Neurol Res 28: 542–548 [DOI] [PubMed] [Google Scholar]
- Mori E, Thomas M, Motoki K, Nakazawa K, Tahara T, Tomizuka K, Ishida I, Kataoka S (2004) Human normal hepatocytes are susceptible to apoptosis signal mediated by both TRAIL-R1 and TRAIL-R2. Cell Death Differ 11: 203–207 [DOI] [PubMed] [Google Scholar]
- Nagane M, Pan G, Weddle JJ, Dixit VM, Cavenee WK, Huang HJ (2000) Increased death receptor 5 expression by chemotherapeutic agents in human gliomas causes synergistic cytotoxicity with tumor necrosis factor-related apoptosis-inducing ligand in vitro and in vivo. Cancer Res 60: 847–853 [PubMed] [Google Scholar]
- Nagourney RA (2006) Ex vivo programmed cell death and the prediction of response to chemotherapy. Curr Treat Options Oncol 7: 103–110 [DOI] [PubMed] [Google Scholar]
- Nesterov A, Ivashchenko Y, Kraft AS (2002) Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) triggers apoptosis in normal prostate epithelial cells. Oncogene 21: 1135–1140 [DOI] [PubMed] [Google Scholar]
- Nguyen T, Zhang XD, Hersey P (2001) Relative resistance of fresh isolates of melanoma to tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis. Clin Cancer Res 7: 966s–9973 , s [PubMed] [Google Scholar]
- Nitsch R, Bechmann I, Deisz RA, Haas D, Lehmann TN, Wendling U, Zipp F (2000) Human brain-cell death induced by tumour-necrosis-factor-related apoptosis-inducing ligand (TRAIL). Lancet 356: 827–828 [DOI] [PubMed] [Google Scholar]
- Norbury CJ, Zhivotovsky B (2004) DNA damage-induced apoptosis. Oncogene 23: 2797–2808 [DOI] [PubMed] [Google Scholar]
- Pettersen I, Figenschau Y, Olsen E, Bakkelund W, Smedsrod B, Sveinbjornsson B (2002) Tumor necrosis factor-related apoptosis-inducing ligand induces apoptosis in human articular chondrocytes in vitro. Biochem Biophys Res Commun 296: 671–676 [DOI] [PubMed] [Google Scholar]
- Rieger J, Naumann U, Glaser T, Ashkenazi A, Weller M (1998) APO2 ligand: a novel lethal weapon against malignant glioma? FEBS Lett 427: 124–128 [DOI] [PubMed] [Google Scholar]
- Riva C, Lavieille JP, Schmerber S, Cuisnie O, Reyt E (2000) Phase II trial of cisplatin, 5-fluorouracil and folinic acid using a weekly 24-h infusion schedule for locally advanced head and neck cancer: a pharmacokinetic and clinical survey. Int J Oncol 17: 543–549 [DOI] [PubMed] [Google Scholar]
- Roa WH, Chen H, Fulton D, Gulavita S, Shaw A, Th’ng J, Farr-Jones M, Moore R, Petruk K (2003) X-linked inhibitor regulating TRAIL-induced apoptosis in chemoresistant human primary glioblastoma cells. Clin Invest Med 26: 231–242 [PubMed] [Google Scholar]
- Rohn TA, Wagenknecht B, Roth W, Naumann U, Gulbins E, Krammer PH, Walczak H, Weller M (2001) CCNU-dependent potentiation of TRAIL/Apo2L-induced apoptosis in human glioma cells is p53-independent but may involve enhanced cytochrome c release. Oncogene 20: 4128–4137 [DOI] [PubMed] [Google Scholar]
- Saito R, Bringas JR, Panner A, Tamas M, Pieper RO, Berger MS, Bankiewicz KS (2004) Convection-enhanced delivery of tumor necrosis factor-related apoptosis-inducing ligand with systemic administration of temozolomide prolongs survival in an intracranial glioblastoma xenograft model. Cancer Res 64: 6858–6862 [DOI] [PubMed] [Google Scholar]
- Scaffidi C, Fulda S, Srinivasan A, Friesen C, Li F, Tomaselli KJ, Debatin KM, Krammer PH, Peter ME (1998) Two CD95 (APO-1/Fas) signaling pathways. EMBO J 17: 1675–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinohara H, Kayagaki N, Yagita H, Oyaizu N, Ohba M, Kuroki T, Ikawa Y (2001) A protective role of PKCepsilon against TNF-related apoptosis-inducing ligand (TRAIL)-induced apoptosis in glioma cells. Biochem Biophys Res Commun 284: 1162–1167 [DOI] [PubMed] [Google Scholar]
- Siegel-Lakhai WS, Crul M, Zhang S, Sparidans RW, Pluim D, Howes A, Solanki B, Beijnen JH, Schellens JH (2005) Phase I and pharmacological study of the farnesyltransferase inhibitor tipifarnib (Zarnestra, R115777) in combination with gemcitabine and cisplatin in patients with advanced solid tumours. Br J Cancer 93: 1222–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song JH, Bellail A, Tse MC, Yong VW, Hao C (2006) Human astrocytes are resistant to Fas ligand and tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis. J Neurosci 26: 3299–3308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song JH, Song DK, Pyrzynska B, Petruk KC, Van Meir EG, Hao C (2003) TRAIL triggers apoptosis in human malignant glioma cells through extrinsic and intrinsic pathways. Brain Pathol 13: 539–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352: 987–996 [DOI] [PubMed] [Google Scholar]
- Tegeder I, Brautigam L, Seegel M, Al-Dam A, Turowski B, Geisslinger G, Kovacs AF (2003) Cisplatin tumor concentrations after intra-arterial cisplatin infusion or embolization in patients with oral cancer. Clin Pharmacol Ther 73: 417–426 [DOI] [PubMed] [Google Scholar]
- Thorburn A (2004) Death receptor-induced cell killing. Cell Signal 16: 139–144 [DOI] [PubMed] [Google Scholar]
- Urien S, Brain E, Bugat R, Pivot X, Lochon I, Van ML, Vauzelle F, Lokiec F (2005) Pharmacokinetics of platinum after oral or intravenous cisplatin: a phase 1 study in 32 adult patients. Cancer Chemother Pharmacol 55: 55–60 [DOI] [PubMed] [Google Scholar]
- Watanabe R, Takiguchi Y, Moriya T, Oda S, Kurosu K, Tanabe N, Tatsumi K, Nagao K, Kuriyama T (2003) Feasibility of combination chemotherapy with cisplatin and etoposide for haemodialysis patients with lung cancer. Br J Cancer 88: 25–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal M, Ram Z, Riddle V, Hilt D, Bortey E (2006) Gliadel wafer in initial surgery for malignant glioma: long-term follow-up of a multicenter controlled trial. Acta Neurochir (Wien) 148: 269–275 [DOI] [PubMed] [Google Scholar]
- Whittle IR, Malcolm G, Jodrell DI, Reid M (1999) Platinum distribution in malignant glioma following intraoperative intravenous infusion of carboplatin. Br J Neurosurg 13: 132–137 [DOI] [PubMed] [Google Scholar]
- Wu GS, Burns TF, McDonald III ER, Jiang W, Meng R, Krantz ID, Kao G, Gan DD, Zhou JY, Muschel R, Hamilton SR, Spinner NB, Markowitz S, Wu G, el-Deiry WS (1997) KILLER/DR5 is a DNA damage-inducible p53-regulated death receptor gene. Nat Genet 17: 141–143 [DOI] [PubMed] [Google Scholar]
- Wu M, Das A, Tan Y, Zhu C, Cui T, Wong MC (2000) Induction of apoptosis in glioma cell lines by TRAIL/Apo-2L. J Neurosci Res 61: 464–470 [DOI] [PubMed] [Google Scholar]
- Xiao C, Yang BF, Asadi N, Beguinot F, Hao C (2002) Tumor necrosis factor-related apoptosis-inducing ligand-induced death-inducing signaling complex and its modulation by c-FLIP and PED/PEA-15 in glioma cells. J Biol Chem 277: 25020–25025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.