Abstract
The purpose of this study was to test the hypothesis of whether the center of rotation (COR) in the transverse plane of the knee is in the medial side during normal walking in a manner similar to that previously described during non-ambulatory activities. The kinematics for normal knees was obtained from 46 knees during normal walking using the point cluster technique. The center of rotation of the medial-lateral axis of the femur relative to the tibia was determined during the stance phase of walking. The hypothesis that the COR is in the medial side during stance was not supported by this study. The average center of rotation during the stance phase of walking was in the lateral compartment for all 46 knees. In addition, the instantaneous COR occurred on the medial side on average less than 25% of the time during the stance phase. Thus, while the COR is predominantly on the lateral side of the knee during walking, the normal function of the knee during walking is associated with both lateral and medial pivoting. These results also demonstrate the importance of describing knee kinematics in the context of a specific activity or the constraints of the test conditions.
Keywords: Knee kinematics, Center of rotation, Lateral pivoting, Medial pivoting, Natural knee movement, Knee prosthesis
INTRODUCTION
The normal function of the knee requires a subtle balance between stability and mobility that depends on the interaction between the ligaments, joint surfaces and muscles spanning the joint. While the joint provides a high degree of mobility for large flexion motion, there is a range of laxity (Markolf, 1978) in other degrees of freedom that is required for normal function during certain activities. For example, there is a unique combination of flexion, anterior-posterior (AP) translation and internal-external (IE) rotation that occur during walking (Dyrby, 2004) that is different than what would occur during deep squatting or a passive flexion/extension motion. The direction and phasing of these relationships between the primary (flexion) and secondary movements (AP and IE) will determine the location of the center of rotation (COR) of the knee in the transverse plane (Banks, 2004).
The location of the transverse plane COR represents the motion of the medial and lateral condyles of the femur relative to the proximal tibia during a specific activity and is an important factor in attempting to restore normal function after reconstructive surgery such as total knee replacement (TKR) and anterior cruciate ligament (ACL) reconstruction.
Asymmetry in the motions in the medial and lateral compartments depends on the internal-external rotation and can be influenced by internal structures in the joint. For example, the anatomy of the knee suggests that the medial compartment has a more conforming contact than the lateral compartment (Kapandji, 1987). In addition, the lateral meniscus is more mobile than the medial meniscus (Kapandji, 1987, McMahon, 2006) suggesting that the COR of the knee is in the medial compartment. In addition, an in vivo study of knee kinematics during deep knee bending and chair rising (Komistek, 2003) as well as in vitro studies of flexion/extension motion (Blaha, 2003, Freeman, 2005, Iwaki, 2000) reported that the tibiofemoral contact points had larger AP movement in the lateral than medial compartments. While the above studies of non-ambulatory activities suggest that the knee predominantly translates on the lateral side and thus the COR is in the medial side of the knee, it remains to be seen whether these observations can be extrapolated to walking. In fact, studies of ambulatory activities (Andriacchi, 2003, Dyrby, 2004, Lafortune, 1992) demonstrate that knee kinematics are uniquely dependent on the specific activity and suggest that the AP motion of the knee is not predominantly in the lateral compartment during ambulation.
Given that walking is the most frequent activity of daily living and understanding the relative movement between the femur and tibia during walking can influence the success or failure of various reconstructive procedures of the knee, it is important to quantitatively assess the location of the COR which represents the relative movement between the femur and tibia in the medial and lateral compartments during walking.
The purpose of this study was to test the hypothesis that the transverse plane COR is in the medial side of the knee, which represents greater tibiofemoral AP movement in the lateral than medial compartments during normal walking as suggested in previous studies of non-ambulatory activities.
METHODS
This study measured knee kinematics during walking to determine the movement of the axes of the femur with respect to the tibia. The average location of the transverse plane COR was determined during stance phase, from heel strike to toe off, using a previously described method (Banks, 2004). The percentage of time that the instantaneous COR was medial to the center of the tibia or lateral to the center of the tibia was tested to determine the frequency of time the knee pivoted medially or laterally during the stance phase of walking.
Twenty three healthy subjects (14 males and 9 females, age 37±12 (s.d.) years, body mass index 23.6±2.4 (s.d.) kg/m2) without knee pain or injury histories were recruited for the study. The study was approved by the IRB and an informed consent was obtained from each subject before the test.
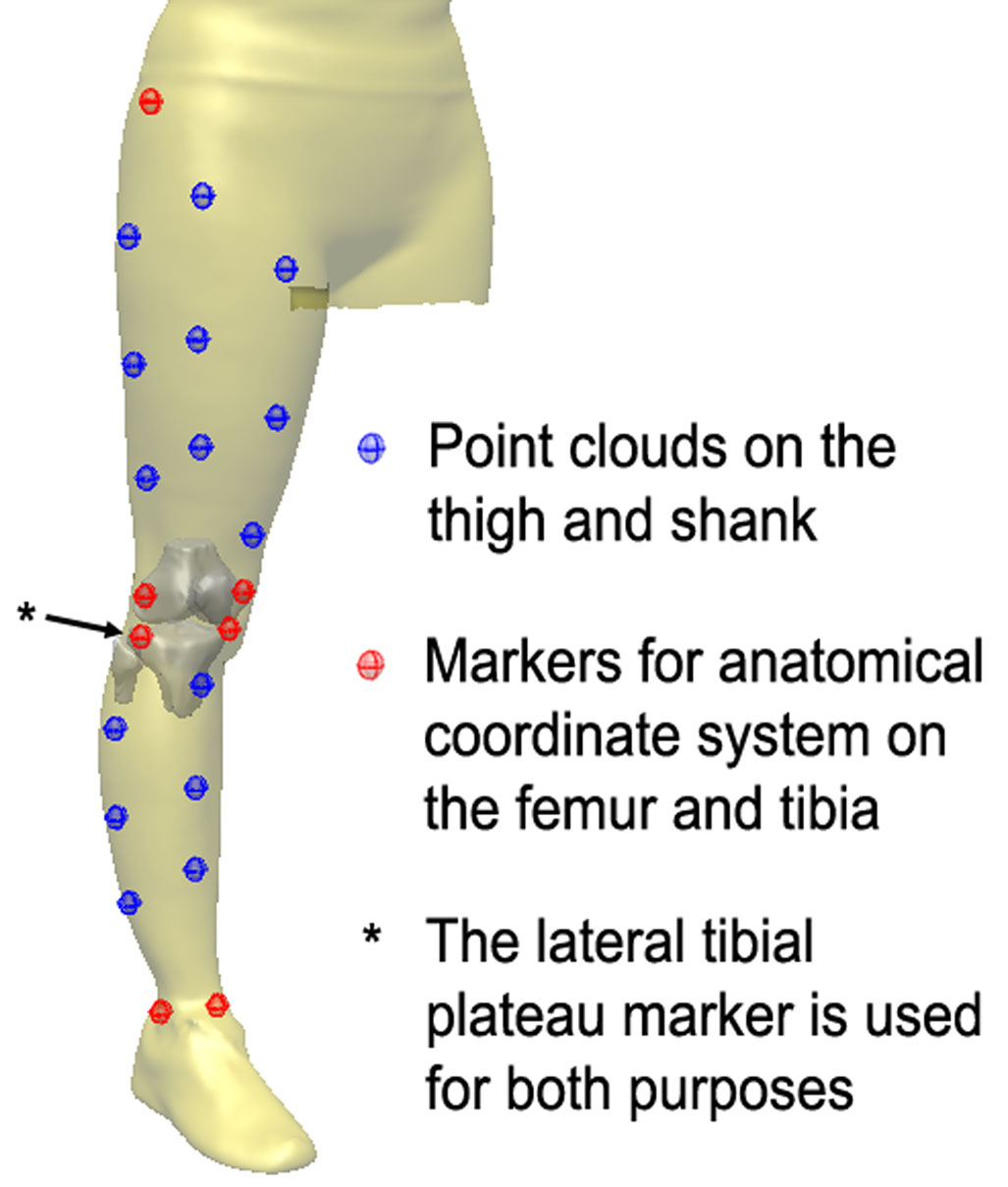
The subjects were tested bilaterally at a self-selected normal walking speed and six degrees of freedom knee joint kinematics were measured using the point cluster technique (PCT) (Andriacchi, 1998). With the PCT, clusters of nine and seven reflective markers were distributed on the thigh and shank, respectively, to predict the movements of the underlying femur and tibia (Figure 1). Cluster coordinate systems were calculated for the marker clusters on the thigh and shank separately by calculating principal axes assuming a unit weight for each marker. During a static reference trial, markers placed on bony landmarks in addition to the clusters of markers were used to establish the femoral and tibial anatomic coordinate systems. The details of the coordinate systems have been previously described (Andriacchi, 1998, Dyrby, 2004). The relative position between the marker clusters and the anatomical coordinate systems were calculated from the marker locations in the reference run for the thigh and shank, separately. At each time frame of normal walking, locations of the marker clusters were tracked in three-dimensional space and the cluster coordinate systems of thigh and shank were calculated. Using the information about the relative locations of the anatomic coordinate systems to cluster coordinate systems obtained in the static reference trial, the locations of the femur and tibia were calculated.
Figure 1.
Point cluster technique is used to measure the kinematics of the femur and tibia. Clouds of skin markers (blue markers) were used to track the motions of the thigh and shank which were translated as the motion of femur and tibia through the markers on bony landmarks (red markers) on the femur and tibia.
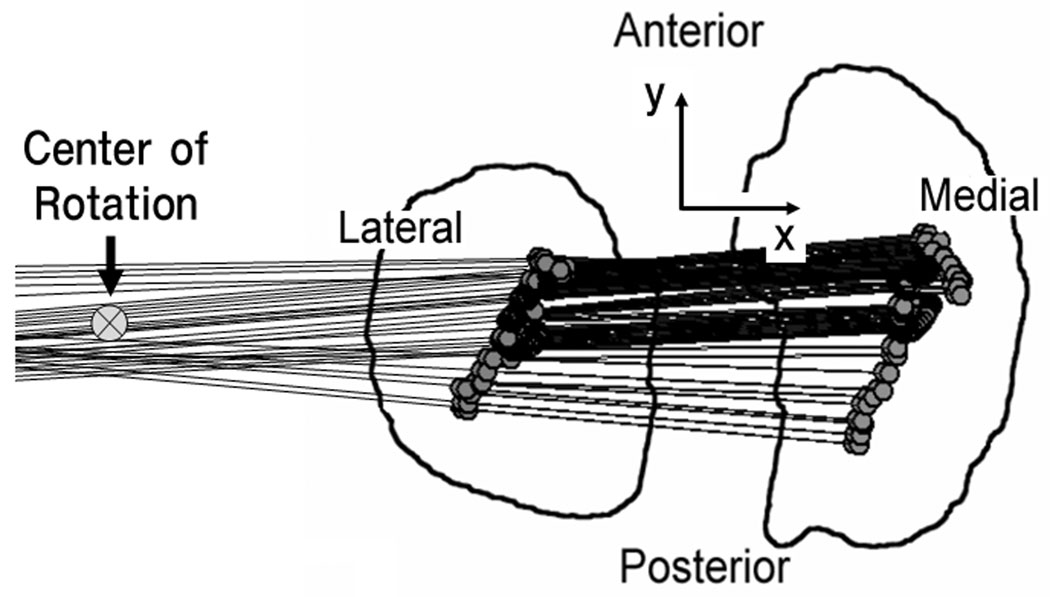
An equation for the line representing the medial-lateral axis of the femur projected on to the transverse plane of the tibial coordinate system was calculated from the AP translation and IE rotation of the femur relative to the tibia obtained from the PCT. The equation of the medial-lateral axis at frame i was written as
| (1) |
where x and y represent the medial-lateral and AP directions, respectively, as shown in Figure 2.
Figure 2.
Medial-lateral axis of the femur projected on the fixed tibial coordinate system is shown at each instance during the stance phase of walking. COR was calculated from the lines in a least square sense.
The average COR of the medial-lateral axis of the femur (Figure 2) was calculated by solving the least-squares system of equations of the lines (Banks, 2004) defining the medial-lateral axis projected on the transverse plane of the tibial axis during the stance phase of walking.
| (2) |
The system of equations (2) describes the medial-lateral axes for time i =1 through n samples. Thus, the average COR (xc, yc) for the entire stance phase (n samples) is
| (3) |
The instantaneous CORs between two consecutive time frames were calculated as shown above and the percentage of time (frequencies) when the COR was medial to the center of the tibia during the stance phase of walking was obtained.
For statistical analysis, a one-sample Z-test was used considering the correlation between the measurements from left and right knees of each subject in calculating variance. The xc value of the average COR (Equation 3) was tested to determine if it was medial or lateral to the center of the tibia. We also tested whether the COR was in the medial side for more than 50% of the time during the stance phase of walking.
Since skin movement can affect the calculation of the average COR from PCT, its robustness was tested by adding Gaussian random noise in the AP translation and IE rotation for each frame. This process was repeated 1000 times to calculate the empirical 95% confidence interval of the average COR for each gait trial. During this process, the standard deviation of the Gaussian random noise was set to 1, 2 and 3 mm for AP translation and 1, 2 and 3 degrees for IE rotation to calculate the robustness at different levels of noise.
RESULTS
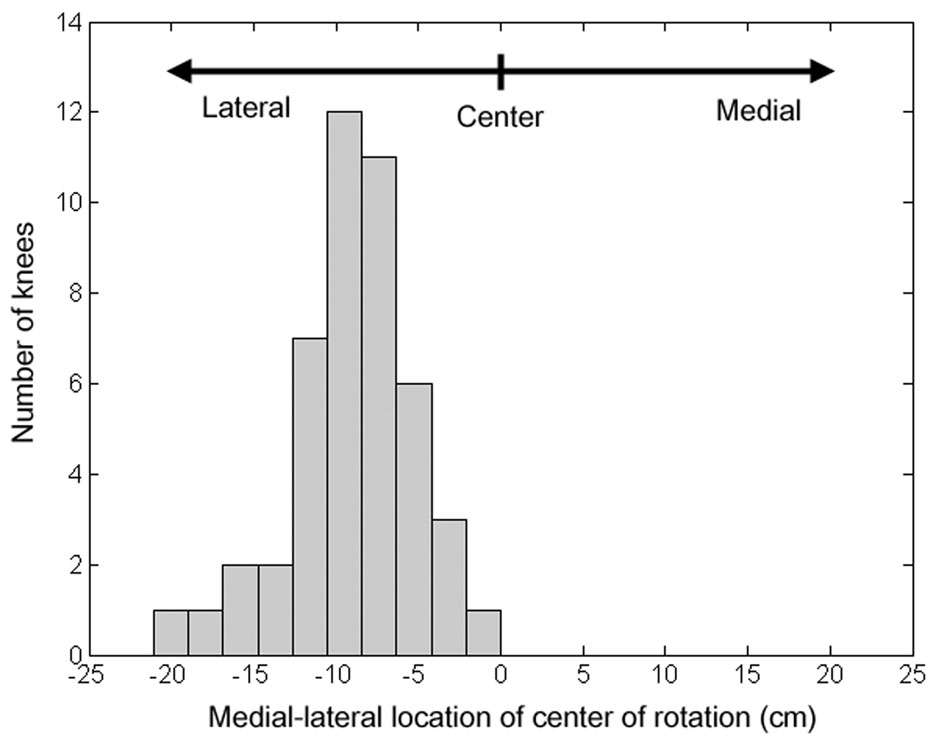
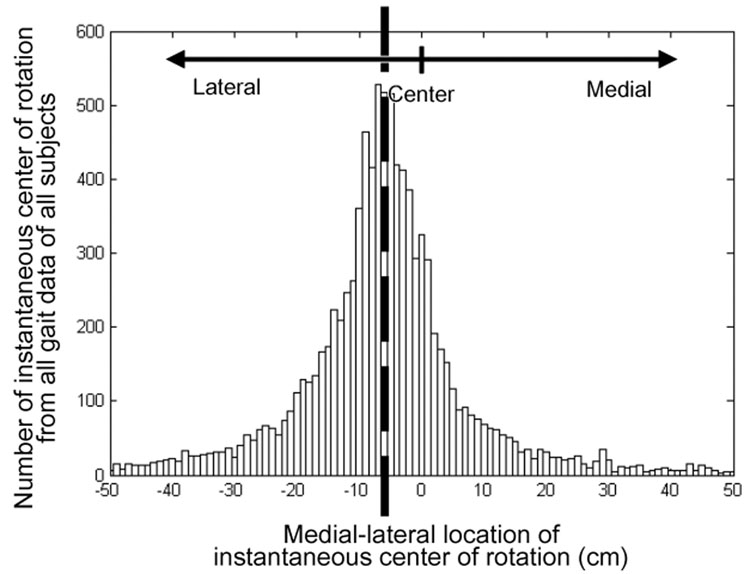
The hypothesis that the transverse plane COR of the knee is in the medial side during stance was not supported by this study. The average COR calculated during the stance phase of normal walking was in the lateral compartment for all 46 knees (p<0.01) (Figure 3). The average (9.0±3.7 (s.d.) cm) and median (8.7 cm) locations of the average COR were lateral (extra articular) to the center of the tibial surface. The subjects walked at an average speed of 1.41±0.18 (s.d.) m/s.
Figure 3.
Histogram of the locations of the transverse plane COR for 46 knees: In the x-axis, zero represents the middle of the tibial surface in the medial-lateral direction and negative values represent the lateral side of the knee. For all tested knees, the COR was on the lateral side of the center of the tibia.
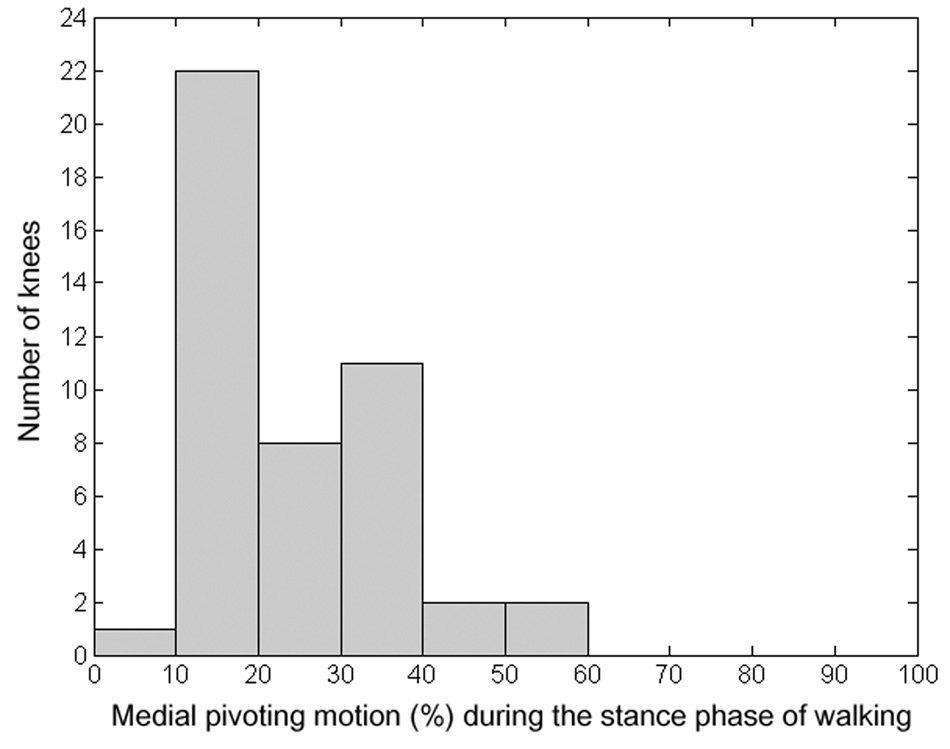
In addition, both the average (24.9±11.6 (s.d.) %) and median (20.5%) percentage of time when the instantaneous COR was in the medial side during stance were significantly (p<0.01) less than 50% indicating that the knee spent a significantly greater amount of time pivoting laterally during walking. The average time when the instantaneous COR was in the medial side was less than 50 percent during the stance phase of walking for 44 knees out of the 46 knees (Figure 4), suggesting that the instantaneous COR was predominantly lateral to the center of the tibia during the stance phase of walking.
Figure 4.
Histogram of the percentage of the medial pivoting motion during the stance phase of walking for 46 knees: Majority of knees had less than 50% of medial pivoting motion during the stance phase.
When all the instantaneous CORs during stance phase for each subject’s gait trial were pooled, the median of the total instantaneous CORs was 6.2 cm lateral to the center of the tibia and 74.8% of the instantaneous CORs were in the lateral side of the knee.
The robustness of the calculation of the average COR was tested for 9 different levels of Gaussian random noise in the AP translation and IE rotation as shown in Table 1. Even when the standard deviations were 3 mm and 3 degrees for the Gaussian noise for AP translation and IE rotation, respectively, the average COR was significantly in the lateral side for 40 knees (87%). None of the knees had an average COR significantly in the medial side for any level of noise.
Table 1.
The robustness of the calculation of the average COR was tested for different levels of Gaussian random noise in the AP translation and IE rotation.
| Gaussian noise for AP translation | Gaussian noise for IE rotation | COR significantly in the lateral side | COR significantly in the medial side |
|---|---|---|---|
| Mean=0, sd=0 mm | Mean=0, sd=0 degree | 46 | 0 |
| Mean=0, sd=1 mm | Mean=0, sd=1 degree | 45 | 0 |
| Mean=0, sd=1 mm | Mean=0, sd=2 degrees | 44 | 0 |
| Mean=0, sd=1 mm | Mean=0, sd=3 degrees | 41 | 0 |
| Mean=0, sd=2 mm | Mean=0, sd=1 degrees | 45 | 0 |
| Mean=0, sd=2 mm | Mean=0, sd=2 degrees | 44 | 0 |
| Mean=0, sd=2 mm | Mean=0, sd=3 degrees | 41 | 0 |
| Mean=0, sd=3 mm | Mean=0, sd=1 degrees | 44 | 0 |
| Mean=0, sd=3 mm | Mean=0, sd=2 degrees | 44 | 0 |
| Mean=0, sd=3 mm | Mean=0, sd=3 degrees | 40 | 0 |
DISCUSSION
The results of this study did not support the hypothesis that the transverse plane COR of the knee was predominantly on the medial side during walking. Rather, the average COR was in the lateral (extra articular) side of the knee. While the instantaneous COR does move to the medial side during a portion of stance the vast majority (44 of 46) spent, on average, more than 70% of time with a COR in the lateral side.
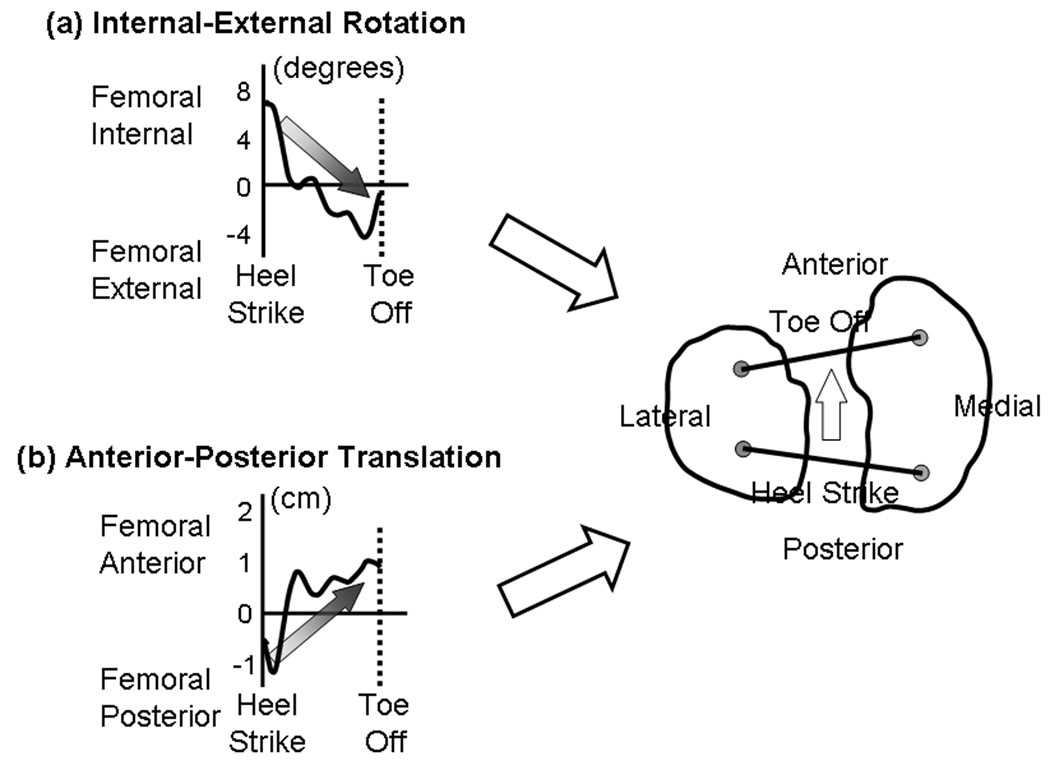
These results are consistent with previous kinematic studies of walking (Andriacchi, 2004 Lafortune, 1992) that report AP and IE motions. These studies show that at heel strike the femur is rotated internally and translated posteriorly relative to the tibia (Figure 6 (a) and (b)). Throughout the stance phase of walking, the femur rotates externally and translates anteriorly relative to the tibia. The combination of the translation and rotation during the stance phase of normal walking suggests that the COR of the knee is on the lateral side for most of the time during the stance phase of normal walking.
Figure 6.
Typical patterns of (a) internal-external rotation and (b) anterior-posterior translation of the femur relative to the tibia during the stance phase of normal walking are shown. (c) The lines represent the locations of the medial-lateral axis of the femur projected on the tibial surface at the beginning and end of the stance phase of walking. These patterns would result in the lateral pivoting in the knee.
Studies of patients with ACL deficient knees (Andriacchi, 2005) showed a pattern of AP and IE motions that are consistent with the patterns found in healthy knees in this study suggesting that the COR of the knee is predominantly in the lateral side in both healthy and ACL deficient knees. These results are consistent with studies of patients with certain types of TKR (Banks, 2004) that show the average COR is in the lateral side of the knee.
While the majority of the instantaneous CORs were distributed close to the center or just lateral of the center of the tibia (Figure 5), there were extreme values on both the medial and lateral sides. An extreme COR value indicates that there is almost pure AP translation occurring during this instant in the stance phase of normal walking.
Figure 5.
Histogram of all instantaneous CORs from the stance phase of all subjects’ trials
The point cluster technique uses skin markers to predict the motion of the underlying bones, so the accuracy in detecting bone motions can be affected by skin movement (Alexander, 2001). Thus, the robustness of the calculation of the average COR was tested by adding Gaussian random noise in measuring AP translation and IE rotation. Even after considering the uncertainties in the measurements, the majority of knees (87%) had lateral pivoting patterns.
A simple flexion/extension motion of cadaver knees showed that the lateral compartment has a larger AP range of movement than the medial compartment (Blaha, 2003, Freeman, 2005, Iwaki, 2000) suggesting that the COR of the knee is in the medial compartment during passive knee motions. The COR of the knee also has been shown to exist in the medial compartment during in vivo open chain activites but it has not been shown during normal walking. Based on the studies of on-ambulatory activities it has also been suggested that designs of TKR should incorporate articular surface shapes that guide medial pivot movement (Blaha, 2004, Schmidt, 2003). Though a previous study reported that the COR of the knee is in the medial compartment during walking for healthy subjects (Komistek, 2003), the tests were conducted at an unrealistically slow speeds; 0.28–0.56 m/s while normal speed is ~1.24 m/s in healthy subjects (Mundermann, 2004).
The results of this study indicate that knee kinematics during walking are different than kinematics measured during non-ambulatory activities (Blaha, 2003, Dennis, 2005, Freeman, 2005, Iwaki, 2000, Komistek, 2003, Li, 2006, Mahfouz, 2004) or observations of passive knee anatomy (Kapandji, 1987) that report that the COR of the knee is in the medial compartment. Taken together with the findings of other studies the results support the conclusions that knee joint kinematics are highly dependent on the specific activity (Andriacchi, 2004, Dyrby, 2004) and knee kinematics should be described in the context of the activity.
While the COR is predominantly on the lateral side of the knee during walking, the instantaneous COR does occur on the medial side about 25% of the stance. Thus, the normal knee function is associated with pivoting in both the medial and lateral sides of the knee. The results of this study indicate that TKR designs should permit lateral pivoting motions during normal walking (the most frequent activity of daily living) while permitting the capacity for medial pivoting motions during non-ambulatory activities such as squatting. The results also suggest the importance of describing knee kinematics in the context of a specific activity or the constraints of the test conditions. Thus, it is not possible to extrapolate knee kinematics from non-ambulatory activities to ambulatory kinematics.
ACKNOWLEDGEMENTS
This study was funded by NIH R01 AR049792. We thank Chris Dyrby for providing the gait data and for his consultation on the marker positions of the point cluster technique.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Alexander EJ, Andriacchi TP. Correcting for deformation in skin-based marker systems. Journal of Biomechanics. 2001;34:355–361. doi: 10.1016/s0021-9290(00)00192-5. [DOI] [PubMed] [Google Scholar]
- Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. Journal of Biomechanical Engineering. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- Andriacchi TP, Dyrby CO, Johnson TS. The use of functional analysis in evaluating knee kinematics. Clinical Orthopaedics and Related Research. 2003;410:44–53. doi: 10.1097/01.blo.0000062383.79828.f5. [DOI] [PubMed] [Google Scholar]
- Andriacchi TP, Johnson TS, Hurwitz DE, Natarajan R. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Huiskes R, editors. Basic Orthopaedic Biomechanics and Mechano-Biology. 3rd ed. Lippincott Williams & Wilkins; 2004. [Google Scholar]
- Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. Journal of Biomechanics. 2005;38:293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Banks SA, Hodge WA. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. Journal of Arthroplasty. 2004;19:809–816. doi: 10.1016/j.arth.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Blaha JD. The rationale for a total knee implant that confers anteroposterior stability throughout range of motion. Journal of Arthroplasty. 2004;19 Suppl. 1:22–26. doi: 10.1016/j.arth.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Blaha JD, Mancinelli CA, Simons WH, Kish VL, Thyagarajan G. Kinematics of the human knee using an open chain cadaver model. Clinical Orthopaedics and Related Research. 2003;410:25–34. doi: 10.1097/01.blo.0000063564.90853.ed. [DOI] [PubMed] [Google Scholar]
- Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. Journal of Biomechanics. 2005;38:241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. Journal of Orthopaedic Research. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Freeman MAR, Pinskerova V. The movement of the normal tibio-femoral joint. Journal of Biomechanics. 2005;38:197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. Journal of Bone and Joint Surgery (Br) 2000;82:1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- Kapandji IA. The Physiology of the Joints: Lower Limb, Volume 2 (Lower Limb) 5th ed. Churchill Livingstone: 1987. [Google Scholar]
- Komistek RD, Dennis DA, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clinical Orthopaedics and Related Research. 2003;410:69–81. doi: 10.1097/01.blo.0000062384.79828.3b. [DOI] [PubMed] [Google Scholar]
- Lafortune MA, Cavanagh PR, Sommer HJ, 3rd, Kalenak A. Three-dimensional kinematics of the human knee during walking. Journal of Biomechanics. 1992;25:347–357. doi: 10.1016/0021-9290(92)90254-x. [DOI] [PubMed] [Google Scholar]
- Li G, Suggs J, Hanson G, Durbhakula S, Johnson T, Freiberg A. Three dimensional tibiofemoral articular contact kinematics of a cruciate-retaining total knee arthroplasty. Journal of Bone and Joint Surgery (Am) 2006;88:395–402. doi: 10.2106/JBJS.D.03028. [DOI] [PubMed] [Google Scholar]
- Mahfouz MR, Komistek RD, Dennis DA, Hoff WA. In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. Journal of Bone and Joint Surgery (Am) 2004;86-A Suppl 2:56–61. doi: 10.2106/00004623-200412002-00009. [DOI] [PubMed] [Google Scholar]
- Markolf KL, Mensch JS, Amstutz HC. Stiffness and laxity of the knee-the contributions of the supporting structures. A quantitative in vitro study. Journal of Bone and Joint Surgery (Am) 1976;58:583–594. [PubMed] [Google Scholar]
- McMahon PJ, Kaplan LD. Sports Medicine. In: Skinner HB, editor. Current diagnosis & treatment in orthopedics. 4th ed. McGraw-Hill Medical; 2006. [Google Scholar]
- Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis and Rheumatism. 2004;50:1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee plants. Clinical Orthopaedics and Related Research. 2003;410:139–147. doi: 10.1097/01.blo.0000063565.90853.a4. [DOI] [PubMed] [Google Scholar]