Abstract
Individuals undergoing treatment for alcohol use disorders smoke at rates that exceed those reported in the general population, and most patients will continue to smoke after treatment completion. A growing body of research indicates that quitting smoking is associated with better alcoholism treatment outcomes. Studies that dichotomize participants into smokers and nonsmokers, however, may be overlooking the possibility that even decreases in cigarette consumption over time among continuing smokers may also be related to improved alcohol use outcomes.
The purpose of this article was to examine the relationship between cigarette consumption and alcohol use outcomes using data from Project MATCH. Smokers were divided into three groups according to whether their cigarette consumption decreased, increased, or remained constant from baseline to the 15-month follow-up. Results showed that smokers whose cigarette consumption decreased were significantly less likely to relapse to alcohol use than those whose consumption increased or remained unchanged. These findings suggest that even reductions in tobacco use may be associated with better drinking outcomes in alcoholism treatment.
Keywords: Smoking, Cigarette consumption, Cessation, Alcohol, Relapse, Abstinence, Treatment
1. Introduction
Individuals undergoing treatment for alcohol and drug use disorders tend to smoke at rates as high as 70–95%, as compared with the 23.3% rate reported for the general population (Batel, Pessione, Maitre, & Rueff, 1995; Bobo, McIlvain, Lando, Walker, & Leed-Kelly, 1998; Burling & Ziff, 1988; Centers for Disease Control and Prevention, 2002; Substance Abuse and Mental Health Services Administration, 2002; Zimmerman, Warheit, Ulbrich, & Auth, 1990). Moreover, these individuals are likely to continue smoking during and after substance abuse treatment, thereby increasing their risk of acquiring tobacco-related illnesses (Bobo et al., 1998; Myers & Brown, 1994).
Discrepant results have been reported regarding the impact of smoking cessation on alcohol use outcomes. Most studies in which tobacco dependence was a focus of treatment have reported that quitting smoking did not hurt and, in some cases, actually helped with alcohol abstinence efforts (Abrams, Monti, Niaura, Rohsenow, & Colby, 1996; Hughes, Novy, Hatsukami, Jensen, & Callas, 2003; Hurt et al., 1994; Toneatto, Sobell, Sobell, & Kozlowski, 1995). In contrast, discrepant results have been reported by investigations in which smoking was not a treatment focus, with some research showing that smoking cessation resulted in better substance use outcomes (Friend & Pagano, 2005; Lemon, Friedmann, & Stein, 2002) and other studies reporting the opposite (Schmidt & Smolka, 2001; Stotts, Schmitz, & Grabowski, 2003). Community investigations in which there was no intervention for alcohol and drug use have also found that smoking cessation was associated with increased substance use (Carmelli, Swan, & Robinette, 1993).
Although most individuals undergoing treatment for substance use disorders maintain their same smoking status throughout treatment duration, a small percentage increase or decrease their cigarette use. With the use of data from Project MATCH (N = 1,726), Friend and Pagano (2004, 2005) reported a quit rate of 12% among baseline smokers and a smoking initiation rate of 15% among baseline nonsmokers undergoing treatment for alcohol use disorders. In examining 749 HMO patients in California, Kohn, Tsoh, and Weisner (2003) found similar rates of 13% and 12%, respectively. In a community sample of 254 polydrug users studied over 3 years, McCarthy, Zhou, and Hser (2001) reported that the probability of retaining the same smoking status across any two consecutive assessments was 0.77 for nonsmokers and was 0.82 for everyday smokers.
Because most smokers do not change their smoking status, most investigations have examined differences in alcohol use between smokers and nonsmokers or between smokers and quitters. There is a paucity of research that have looked into associations between changes in cigarette consumption levels over time and drinking outcomes. Gulliver et al. (2000) reported that, in a sample of alcoholic smokers for whom smoking was not a targeted intervention, 6-month alcohol relapse was not significantly associated with 6-month reductions in cigarette consumption (from a mean of 27.5 ± 12.8 cigarettes/day to that of 23.3 ± 11.6 cigarettes/day) in 45% of 116 inpatients who decreased their cigarette use. Likewise, in a sample of 155 alcohol abusers undergoing treatment for their alcohol use only, Toneatto et al. (1995) found that posttreatment change in smoking status (increase or decrease) was not significantly related to 7- to 12-month drinking outcomes, including days abstinent, morning drinking days, and heavy drinking days.
These two studies suggest that changes in cigarette consumption may not be related to posttreatment drinking outcomes, but further research is warranted. The purpose of this article was to examine associations between cigarette consumption, measured by number of cigarettes smoked daily, and drinking outcomes. We used data from Project MATCH, the largest multisite randomized clinical trial on behavioral treatment of alcohol abuse and alcoholism to date. Our study offers a unique contribution to the literature for several reasons. Project MATCH represents the largest data set of its kind, with a sample size of 1,726. It used prospective assessments, with follow-ups every 90 days, as compared with every 6 months in the two investigations described previously. We also used the advanced analytic method of survival analysis, which allows for more accurate conclusions from complex, longitudinal data.
We chose to base our hypotheses on our prior work, although its findings are discrepant from those reported by Gulliver et al. (2000) and Toneatto et al. (1995), using data from Project MATCH that demonstrated that smokers who quit smoking showed better drinking outcomes (Friend & Pagano, 2004). Thus, we hypothesized that continuing smokers who reduced their cigarette consumption would have better drinking outcomes, as assessed by percentage of days abstinent from alcohol use, than those who did not reduce or who increased their cigarette consumption. This study represents a continuing line of research that seeks to understand better associations between smoking and drinking during and after treatment for alcohol use disorders, including the cases of nonsmokers who initiated smoking during Project MATCH (Friend & Pagano, 2004) and who quit smoking during the year following treatment (Friend & Pagano, 2005).
2. Method
We used data from Project MATCH, a longitudinal investigation of the efficacies of three behavioral interventions for alcohol abuse and dependence that were each delivered over the course of 12 weeks (U.S. Department of Health and Human Services [USDHHS], 2001). Patients did not receive treatment for their cigarette use.
One thousand seven hundred twenty-six patients with alcohol abuse and dependence disorders participated in Project MATCH. There were two study arms: outpatient and aftercare. Outpatients were recruited directly from communities or outpatient centers. Patients in aftercare were recruited from intensive inpatient or day-hospital treatments. Inclusion criteria included having either a current (for the outpatient arm) or a 3-months-prior-to-treatment (for the aftercare arm) DSM-III-R diagnosis of alcohol abuse or dependence. Exclusion criteria included meeting a current DSM-III-R diagnosis of dependence for sedative/hypnotic drugs, stimulants, cocaine, or opiates; having taken these drugs intravenously during the previous 6 months; being currently dangerous to themselves or others; exhibiting symptoms of acute psychosis; and/or having severe organic impairment. Participants provided informed consent and the procedures used were in accordance with the standards of the Committee on Human Experimentation with the Helsinki Declaration of 1975 (Project MATCH Research Group, 1993).
For the current investigation, only participants who smoked continuously throughout the 15-month investigation and who had complete data at intake and at each of the follow-up intervals were included, resulting in a final sample of 955 patients. Nicotine and alcohol use measures were administered at baseline and at 3-, 6-, 9-, 12-, and 15-month follow-ups.
2.1. Measures
2.1.1. Nicotine use
Nicotine (cigarette) use was assessed at intake and at all follow-ups using the Form I-90, which was developed specifically for Project MATCH (National Institute of Alcohol Abuse and Alcoholism [NIAAA], 1996). This instrument measured nicotine use during the “current period,” corresponding to the preceding 90 days approximately. Questions regarding nicotine (cigarette) use included the following: (a) ever used tobacco (yes/no), (b) number of lifetime weeks of use, and (c) number of cigarettes per day in the preceding 90 days (NIAAA, 1996). “Cigarettes per day in the current period” was used to determine whether a participant was a current smoker. A participant who reported smoking 0 cigarettes/day in a given follow-up period was designated as a nonsmoker, whereas a participant who reported smoking ≥1 cigarettes/day in a given follow-up period was classified as a smoker.
2.1.2. Smoker classifications
Smokers were categorized into three groups: (a) light smokers (those who consumed 1–15 cigarettes/day); (b) moderate smokers (those who consumed 16–24 cigarettes/day); and (c) heavy smokers (those who consumed ≥25 cigarettes/day). These classifications were roughly based on those used by Cummings, Hyland, Ockene, Hymowitz, and Manley (1997) in their analysis of nicotine patch use among participants in the COMMIT Study.
2.1.3. Change in cigarette consumption classifications
“Change in cigarette consumption” classification groups were determined by comparing differences in cigarette consumption at baseline with those at the final 15-month follow-up. Changes in cigarette consumption were categorized into three groups: (a) participants whose consumption patterns remained constant throughout the study (light smoker at baseline/light smoker at 15 months, moderate smoker at baseline/moderate smoker at 15 months, heavy smoker at baseline/heavy smoker at 15 months); (b) participants who increased their cigarette consumption (light smoker at baseline/heavy smoker at 15 months, moderate smoker at baseline/heavy smoker at 15 months, light smoker at baseline/moderate smoker at 15 months); and (c) participants who decreased their cigarette consumption (moderate smoker at baseline/light smoker at 15 months, heavy smoker at baseline/moderate smoker at 15 months, heavy smoker at baseline/light smoker at 15 months).
One concern was that a participant whose cigarette consumption changed from, for example, 15 to 16 cigarettes/day would be classified in the same group (i.e., “increased consumption”) as would a participant whose consumption changed from 5 to 20 cigarettes/day. Based on the assumption that minimal change in consumption should not be represented as having changed consumption levels, we decided that someone whose cigarette consumption level changed by ≤5 cigarettes/day would be classified in the “constant consumption” group. Based on this criterion, eight participants whose consumption did change but by <6 cigarettes/day received this classification. The remaining members of the constant consumption group smoked the same number of cigarettes daily at baseline and at 15 months.
2.1.4. Alcohol use
Alcohol consumption was assessed using percentage of days abstinent from alcohol use and drinks per drinking day as measured by timeline follow-back (TLFB; Sobell & Sobell, 1992; Sobell, Sobell, Klajner, Pavan, & Basian, 1986). The TLFB is a calendar-assisted daily drinking estimation method that provides a comprehensive assessment of a person's drinking over a designated period. It has demonstrated adequate psychometric properties in a variety of patient samples (USDHHS, 1995). The TLFB tends to provide greater estimates of drinking frequency than quantity–frequency measures (Grant, Tonigan, & Miller, 1995; Lemmens, Tan, & Knibbe, 1992; Sobell, Sobell, Leo, & Cancilla, 1988), although these differences do not appear to be clinically relevant (USDHHS, 1995). Because the data were heavily skewed owing to floor and ceiling effects, log-transformed variables were used (Project MATCH Research Group, 1993). Alcohol relapse was defined as consuming any drink during a given follow-up period.
2.2. Data analysis
Statistical analyses were conducted with SAS Version 8.0 (SAS Institute Inc., 1999), using PROC FREQ, PROC ANOVA, PROC REG, and PROC LIFETEST. Depending on the type of variables (continuous or discrete), analysis of variance or χ2 analysis was performed to evaluate demographic and clinical differences between groups. Kaplan–Meier survival estimates were used to calculate probabilities of time to alcohol relapse.
3. Results
3.1. Sample demographic and baseline clinical characteristics
Most of the sample patients were male (n = 729; 76%) and Caucasian (n =748; 78%), see Table 1. On average, participants were 39 years old and had 13 years of education. They had been smoking for an average of 1,131.7 weeks (SD = 571.8 weeks) over their lifetime. At baseline, participants smoked a mean of 24.9 cigarettes/day (SD = 14.6 cigarettes/day).
Table 1.
Demographic and clinical characteristics by smoker consumption levels
| Intake variable | Light smokers (1–15 cigarettes/day; n = 241; 25%) |
Moderate smokers (16–24 cigarettes/day; n = 302; 32%) |
Heavy smokers (≥25 cigarettes/day; n = 412; 43%) |
Total (N = 955; 100%) |
|---|---|---|---|---|
| Sex [n (%)] | ||||
| Male | 181 (25) | 226 (31) | 322 (44) | 729 (76) |
| Female | 60 (27) | 76 (34) | 90 (40) | 226 (24) |
| Race [n (%)] | ||||
| White | 179 (24) | 247 (33) | 322 (43) | 748 (78) |
| African American | 26 (25) | 24 (23) | 54 (52) | 104 (11) |
| Hispanic | 29 (33) | 27 (31) | 31 (35) | 87 (9) |
| Other | 7 (43) | 4 (25) | 5 (31) | 16 (2) |
| Age in years [M (SD)]** | 36.8 (10.6) | 37.8 (9.4) | 41.9 (10.5) | 39.3 (10.4) |
| Years of education [M (SD)] | 12.9 (2.1) | 13.0 (1.9) | 12.9 (2.1) | 12.9 (2.1) |
| Lifetime weeks of use [M (SD)]** | 878.2 (580.8) | 1,084.4 (494.9) | 1,314.6 (556.6) | 1,131.7 (571.8) |
| Percentage of days abstinent from alcohol [M (SD)]* | 59.6 (39.2) | 53.4 (39.5) | 48.9 (41.6) | 53.4 (40.0) |
| Drinks per drinking day [M (SD)]* | 3.9 (1.2) | 4.0 (1.1) | 4.2 (1.3) | 4.0 (1.2) |
p < .01.
p < .001.
We compared light, moderate, and heavy smokers on baseline demographic and substance use characteristics. Light smokers smoked an average of 9.2 cigarettes/day (SD = 4.4 cigarettes/day); moderate smokers, an average of 19.9 cigarettes/day (SD = 0.9 cigarettes/day); and, heavy smokers, an average of 37.9 cigarettes/day (SD = 12.4 cigarettes/day). Light smokers were significantly younger (p < .0001), reported fewer lifetime weeks of tobacco use (p<.001), had more baseline percentage of days abstinent from alcohol use (p<.01), and consumed fewer drinks per drinking day (p<.01) than members of the other two groups. There was no significant difference between smoker groups in sex, education, and race/ethnicity.
3.2. Changes in cigarette consumption and demographic and clinical characteristics
Next, we examined whether there was any significant demographic difference between participants who remained constant in their cigarette consumption, those who decreased their cigarette consumption, and those who increased their cigarette consumption. Most smokers (n = 673; 71%) did not change their average number of cigarettes smoked daily; 99 participants (10%) decreased their consumption and 183 participants (19%) increased theirs.
We examined the mean levels of cigarette consumption for each change classification group at each follow-up interval to examine if change in classification group reflected overall patterns throughout the study period. As shown in Fig. 1, smokers whose consumption decreased showed the greatest declines in the first 3 months of the study (i.e., during treatment). Consumption levels continued to decline over the next 12 months. Participants whose cigarette consumption was constant at baseline and at 15 months also showed a constant smoking pattern throughout the study period. In contrast, participants whose cigarette consumption increased demonstrated consumption levels that gradually increased over 9 months and then plateaud during the remaining 6 months of the study.
Fig. 1.
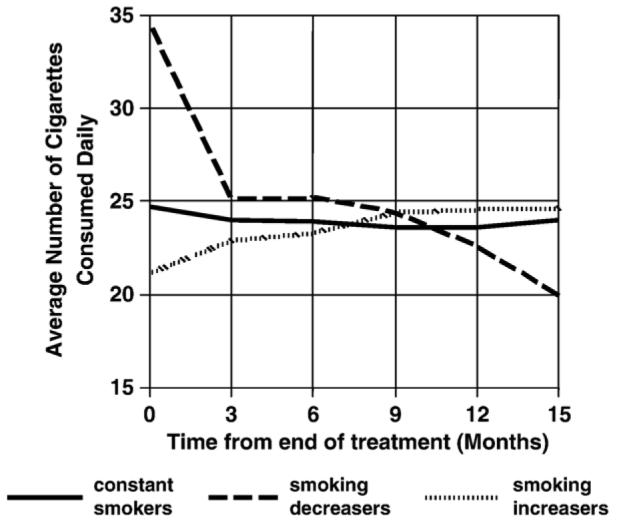
Average number of cigarettes at each follow-up by change in smoking classification group.
Demographic and clinical characteristics among the changes in cigarette consumption classification groups were also examined (see Table 2). Participants whose consumption decreased were significantly older (p<.01) and showed greater lifetime weeks of tobacco use (p<.01) than those whose cigarette consumption remained constant or increased. Participants whose cigarette consumption decreased smoked significantly more cigarettes per day at baseline compared with those whose consumption remained constant or increased (p<.0001). There was no significant difference among the groups in sex, education, race/ethnicity, percentage of days abstinent from alcohol use at baseline, and drinks per drinking day at baseline.
Table 2.
Demographic and clinical characteristics of smokers who showed constant, increased, and decreased cigarette consumption from baseline to 15-month follow-up
| Intake variable | No change (n = 673; 71%) |
Increased (n = 183; 19%) |
Decreased (n = 99; 10%) |
Total (n = 955; 100%) |
|---|---|---|---|---|
| Sex [n (%)] | ||||
| Male | 517 (71) | 143 (20) | 69 (9) | 729 (76) |
| Female | 156 (69) | 40 (18) | 30 (13) | 226 (24) |
| Race [n (%)] | ||||
| White | 526 (70) | 142 (19) | 80 (11) | 748 (78) |
| African American | 73 (70) | 21 (20) | 10 (10) | 104 (11) |
| Hispanic | 62 (71) | 19 (22) | 6 (7) | 87 (9) |
| Other | 12 (75) | 1 (6) | 3 (19) | 16 (2) |
| Age in years [M (SD)]* | 39.3 (10.3) | 38.1 (10.1) | 42.1 (11.1) | 39.4 (10.4) |
| Years of education [M (SD)] | 13.0 (2.1) | 12.9 (1.9) | 12.8 (1.9) | 13.0 (2.0) |
| Lifetime weeks of use [M (SD)]* | 1,132.9 (570.9) | 1,036.8 (554.3) | 1,298.7 (576.6) | 1,131.7 (571.8) |
| Cigarettes/day [M (SD)]** | 24.7 (14.8) | 21.7 (12.9) | 34.5 (12.1) | 24.9 (14.6) |
| Percentage of days abstinent from alcohol [M (SD)] | 51.7 (40.8) | 56.5 (39.0) | 52.9 (39.7) | 53.4 (40.0) |
| Drinks per drinking day [M (SD)] | 4.0 (1.2) | 4.2 (1.2) | 4.2 (1.4) | 4.0 (1.2) |
p < .01.
p < .001.
3.3. Probabilities of alcohol relapse by change in cigarette consumption
We then examined whether change in cigarette consumption was associated with drinking outcomes. Fig. 2 shows survival curves representing the proportion of participants who avoided taking a drink as a function of time from the end of active treatment (i.e., at approximately Day 90). The time axis of Fig. 1 represents the number of days after Day 90. Approximately 78% of the study sample relapsed in the 12 months following treatment, which is similar to the rate found in the original Project MATCH sample.
Fig. 2.
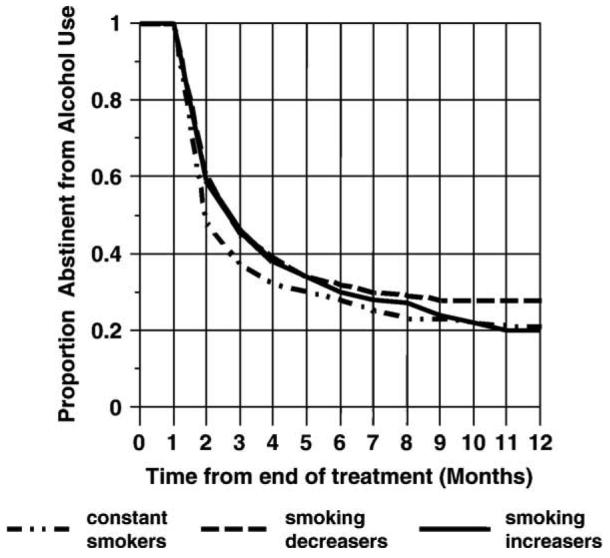
Survival curves of time to first drink by change in smoking classification group.
In comparing the survival curves between cigarette consumption change classification groups, we found that alcohol relapse rates were highest in all three groups immediately after treatment, as indicated by the steep drop in the survival curves. Over time, the rate of new relapses decreased and the curves tended to flatten. With the use of Kaplan–Meier survival estimates, participants who decreased their cigarette consumption were significantly less likely to relapse in the 12 months following treatment than those whose cigarette consumption levels remained constant or increased (Wilcoxon χ2 = 7.5, p = .02). More specifically, 28% of participants who decreased their consumption did not drink in the first year following treatment, as compared with 21% of those whose cigarette consumption remained constant and 20% of those who increased their cigarette consumption.
We also conducted regression analyses to determine if our categorical smoking outcomes were associated with alcohol consumption, measured as a continuous variable. With control for the baseline demographic characteristics of age, sex, education, and race, results showed that percentage of days abstinent from drinking did not predict changes in cigarette consumption (p = .11), although this relationship approached significance. We did find, however, that drinks per drinking day were a significant predictor of changes in cigarette consumption (p = .03), whereby a unit's increase in alcohol consumption resulted in an average increase of 6 cigarettes/month.
4. Discussion
The purpose of this study was to investigate if change in cigarette consumption during and after treatment for alcohol use disorders was associated with alcohol use outcomes among continuing smokers. Our data were derived from Project MATCH, a 15-month study of the efficacy of three behavioral treatments for alcohol abuse and dependence.
Our hypothesis was confirmed. Smokers who decreased their daily cigarette consumption during and after treatment for alcoholism were significantly less likely to relapse to alcohol use than smokers who remained constant or increased their cigarette consumption.
Our results are inconsistent with those of Gulliver et al. (2000) and Toneatto et al. (1995), who found that 6- to 12-month posttreatment cigarette consumption was not associated with drinking outcomes. Participants in the Gulliver et al. (2000) smoked, on average, fewer cigarettes per day at baseline, and the decline in consumption was substantially less than that of the participants in the current investigation (∼4 vs. 15 cigarettes/day). The greater drop in cigarette consumption among our participants raises the possibility that this sample was more ready to make lifestyle changes and thus to maintain alcohol abstinence. Moreover, subjects in the Gulliver et al. (2000) investigation were inpatients and likely had more severe alcohol use disorders than those in Project MATCH. Subjects in the Toneatto et al. (1995) investigation were outpatients, but the researchers' measure of cigarette consumption was based on the degree of nicotine dependence, as assessed by time to first cigarette of the day instead of number of cigarettes smoked daily; thus, the findings of the two studies are not exactly comparable. Although differences in study samples, methodologies, and substance abuse clinical characteristics may have accounted in part for the discrepancies in results, our findings are important because of the large sample size and analyses used. Further research on the impact of changes in cigarette consumption and drinking outcomes is merited.
We also found that smokers whose cigarette consumption stayed the same or increased showed no difference in alcohol use outcomes. These findings suggest that, whereas quitting smoking or reducing the number of cigarettes smoked daily during alcoholism treatment might be associated with motivation toward general lifestyle change, steady or increased tobacco consumption may have no such correlation. Additional studies are warranted to empirically verify this hypothesis and to tease apart further ways in which changes in tobacco consumption may be related to alcohol consumption outcomes during and after alcoholism treatment. We think so.
We conducted regression analyses to predict changes in cigarette consumption based on percentage of days abstinent from drinking and on drinks per drinking day. Results showed that percentage of days abstinent did not predict changes in cigarette consumption. Changes in alcohol consumption levels, as measured by drinks per drinking day, only modestly predicted changes in the number of cigarettes smoked daily. There are several factors that may help account for these results. First, because smoking cessation was not included as part of the treatment in this study, many smokers decreased their drinking consumption but did not alter their smoking patterns. Second, this finding is consistent with the synergy, discussed previously, between alcohol and tobacco use. Additional studies are needed to understand how smoking and drinking outcomes might be related. Such information may have important clinical implications in terms of whether the goal of dual substance abstinence or reductions in daily use should be proactively encouraged.
Regardless of the direction of the association between cigarette and alcohol consumption, reductions in one substance may result in decreased use of the other because of the synergistic effect of the two. Both animal and human studies suggest that common genes may influence the prevalence of cross-addictions between alcohol and tobacco (Heath et al., 2002; Tritto, Marley, Bastisas, Stitzel, & Collins, 2001; True et al., 1999). Nicotine and other substances also appear to share common physiological reinforcing mechanisms and show additive effects on tolerance and sensitization (Collins, Romm, Selvaag, Turner, & Marks, 1993; Soderpalm, Ericson, Olausson, Blomqvist, & Engel, 2000).
Genetic and physiological factors alone, however, appear inadequate to completely explain shared vulnerability to dependence on alcohol/drugs and nicotine; environmental and behavioral factors also merit attention (Tsuang, Bar, Harley, & Lyons, 2001). Use of multiple substances commonly occurs at bars, parties, and other social arenas in which smoking is deemed socially acceptable (Burling, Ramsey, Seidner, & Kondo, 1997). Smoking may act to attenuate some of the physiological or cognitive effects resulting from alcohol or drug abuse (Leigh, Tong, & Campbell, 1977; Lyon, Tong, Leigh, & Claire, 1975; Perkins, 1996; Tong, Knott, McGraw, & Leigh, 1974). Acute behavioral effects of alcohol/drug and nicotine use, such as stress and negative mood reduction, may also help account for their combined use (Perkins, 1996). Nicotine use may reduce the neuropathology associated with alcohol withdrawal (Prendergast, Harris, Mayer, & Littleton, 2000). In summary, these results suggest that the high rate of tobacco use among substance abusers is related to a constellation of factors that work synergistically. Therefore, one might hypothesize that reductions in the use of one could result in reductions in use of the other. Further studies are needed to empirically validate this prediction.
In our investigation, smoking was not a targeted intervention. Because research in which cigarette use is a focus of treatment have shown that stopping smoking was associated with better alcohol outcomes than continuing smoking, it is possible that our drinking outcomes may have been even more dramatic if participants had been treated for their tobacco dependence. It should be noted, however, that treatment for tobacco dependence could substantially change the composition of the groups if more individuals stopped smoking entirely.
Although research have suggested that individuals with alcohol and drug use disorders tend to be heavier smokers than individuals in the general population, we found that nearly similar proportions of participants were light, moderate, and heavy smokers. This finding suggests that smokers in alcohol and drug use treatment may represent a more heterogeneous group than is typically recognized and may help explain discrepancies in study outcomes (Bobo et al., 1998; Burling & Ziff, 1988; Collins & Marks, 1995; Zimmerman et al., 1990). Future research should attempt to account for these possible variations in cigarette consumption rates and how these differences might influence alcoholism treatment outcomes.
Studies are needed to determine at which point patients undergoing treatment or aftercare clients change their smoking habits without formal smoking cessation interventions. This information may help clinicians capitalize on using specific time frames when clients are likely to be more ready to change. Related to this issue, some research have examined at what point in treatment it is better to help patients quit smoking. Results, however, have been mixed and inconclusive, likely because patients fall into different groups in terms of when they are motivated to address both alcohol and tobacco use (Sobell, Sobell, & Agrawal, 2002). Some studies support initiating tobacco dependence treatment at the beginning of alcohol or drug abuse treatment. It may be easier to encourage patients to quit smoking at treatment admission. Campbell, Wander, Stark, and Holbert (1995) reported greater success for a smoking cessation intervention delivered early in substance abuse treatment but also found that even the delayed condition yielded higher quit rates than a control condition. Generally, studies appear to indicate that smoking cessation outcomes are similar regardless of the timing of tobacco dependence treatment (Joseph, Willenbring, Nelson, & Nugent, 2002; Kalman et al., 2001; Sees & Clark, 1993). Patients' illness severity, however, may contribute to when tobacco treatment should be started, with those more heavily addicted less willing to address both issues concurrently (Ellingstad, Sobell, Sobell, Cleland, & Agrawal, 1997). Length of alcohol abstinence prior to smoking cessation may mediate both readiness to consider smoking cessation and cessation outcomes (Hitman et al., 2002; Kalman et al., 2001; but see Martin et al., 1997 for discrepant findings), suggesting that sequential, rather than concurrent, alcohol and smoking treatments may be warranted, at least for some patients.
We considered assessing correlations between cigarette consumption and other alcohol outcomes, such as time to heavy drinking days. We recognized, however, that it would be difficult to define “heavy drinking days” because the definition may vary according to sex, body weight, and other factors (USDHHS, 2001). Because of the novelty of this research and the complexity of the analyses and interpretations, we chose to evaluate only alcohol abstinence in this article. In future work, we intend to address changes in alcohol consumption and other important alcohol-related outcomes.
There are several study limitations that should be noted. The participants who decreased their cigarette consumption began the study consuming significantly more cigarettes per day, on average, than those from the other smoker change classification groups and thus had a greater range of movement among cigarette consumption categories. Future studies that use a greater number of smoker change classification groups or consider continuous cigarette consumption measures to determine if a more flattened distribution yields different results should be conducted. Moreover, our assessments relied only on self-reports to assess alcohol and cigarette use, without biochemical verification, other than a breathalyzer test for acute alcohol consumption, or collateral corroboration.
These limitations withstanding, our findings suggest that even reductions in cigarette consumption are associated with better drinking outcomes and raise the possibility that tobacco treatment may be a worthwhile addition to substance abuse treatment programs. This study represents an ongoing line of research we are developing that examines associations between smoking and drinking during and after alcoholism treatment (Friend & Pagano, 2004, 2005). Our study results may have clinical relevance in helping determine if and when smoking cessation might be addressed in alcohol and drug treatment and which clients might be interested in such an intervention.
Research that attempts to determine whether motivation to quit smoking, rather than reductions in cigarette consumption per se, is associated with better alcohol use outcomes is warranted. Studies that determine how best to address smoking within the context of clinical, rather than research, settings are also needed to maximize the generalizability of research findings.
Acknowledgments
We would like to thank Dr. Robert L. Stout for his suggestions and comments regarding the interpretation of findings in this study.
The data used in this study were provided by Project MATCH, a collaborative clinical trial sponsored by the National Institute on Alcohol Abuse and Alcoholism (Bethesda, Maryland). Analyses and manuscript preparation were made possible through the generous support of the Department of Psychiatry of the Brown University (Providence, Rhode Island) and the Decisions Sciences Institute (Providence, Rhode Island).
The authors acknowledge that the reported results are, in whole or in part, based on the analyses of the Project MATCH Public Data Set. These data were collected as part of a multisite clinical trial of alcoholism treatments that were supported by a series of grants from the National Institute on Alcohol Abuse and Alcoholism and made available to the authors by the Project MATCH Research Group. This article was not reviewed or endorsed by the Project MATCH Research Group and does not necessarily represent the opinions of its members, who are not responsible for the contents.
References
- Abrams DB, Monti P, Niaura R, Rohsenow DJ, Colby SM. Interventions for alcoholics who smoke. Alcohol Health and Research World. 1996;2092:111–117. [PMC free article] [PubMed] [Google Scholar]
- Batel P, Pessione F, Maitre C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90:977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: Findings from a randomized community intervention trial. Addiction. 1998;93:877–887. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- Burling TA, Ramsey TG, Seidner AL, Kondo CS. Issues related to smoking cessation among substance abusers. Journal of Substance Abuse. 1997;9:27–40. doi: 10.1016/s0899-3289(97)90004-3. [DOI] [PubMed] [Google Scholar]
- Burling TA, Ziff DC. Tobacco smoking: A comparison between alcohol and drug abuse inpatients. Addictive Behaviors. 1988;13:185–190. doi: 10.1016/0306-4603(88)90010-x. [DOI] [PubMed] [Google Scholar]
- Campbell BK, Wander N, Stark MJ, Holbert T. Treating cigarette smoking in drug-abusing clients. Journal of Substance Abuse Treatment. 1995;12:89–94. doi: 10.1016/0740-5472(95)00002-m. [DOI] [PubMed] [Google Scholar]
- Carmelli D, Swan GE, Robinette D. The relationship between quitting smoking and changes in drinking in World War II veteran twins. Journal of Substance Abuse. 1993;5:103–116. doi: 10.1016/0899-3289(93)90055-g. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Cigarette smoking among adults—United States, 2000. Morbidity and Mortality Weekly Report. 2002 July 26;51:642–645. [PubMed] [Google Scholar]
- Collins AC, Marks MJ. Animal models of alcohol–nicotine interactions. In: Ferttig JB, Allen JP, editors. Alcohol and tobacco: From basic science to clinical practice. Supt. of Docs U.S. Govt. Print. Office; Washington, DC: 1995. pp. 129–144. [Google Scholar]
- Collins AC, Romm E, Selvaag S, Turner S, Marks MJ. A comparison of the effects of chronic nicotine infusion on tolerance to nicotine and cross-tolerance to ethanol in long- and short-sleep mice. Journal of Pharmacology and Experimental Therapeutics. 1993;266:1390–1397. [PubMed] [Google Scholar]
- Cummings KM, Hyland A, Ockene JK, Hymowitz N, Manley M. Use of the nicotine skin patch by smokers in 20 communities in the United States, 1992–1993. Tobacco Control. 1997;6(Suppl 2):S63–S70. doi: 10.1136/tc.6.suppl_2.s63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellingstad TP, Sobell LC, Sobell MB, Cleland PA, Agrawal S. Alcohol abusers who want to quit smoking: Implications for clinical treatment. Drug and Alcohol Dependence. 1997;54:259–264. doi: 10.1016/s0376-8716(98)00180-x. [DOI] [PubMed] [Google Scholar]
- Friend KB, Pagano M. Smoking initiation among alcoholics in treatment. Journal of Substance Abuse Treatment. 2004;26:219–224. doi: 10.1016/S0740-5472(04)00003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friend KB, Pagano M. Smoking cessation and alcohol consumption in individuals in treatment for alcohol use disorders. Journal of Addictive Diseases. 2005 April;24(2) doi: 10.1300/J069v24n02_06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant KA, Tonigan JS, Miller WR. Comparison of three alcohol consumption measures: A concurrent validity study. Journal of Studies on Alcohol. 1995;56:168–172. doi: 10.15288/jsa.1995.56.168. [DOI] [PubMed] [Google Scholar]
- Gulliver SB, Kalman D, Rohsenow DJ, Colby SM, Eaton CA, Monti PM. Smoking and drinking among alcoholics in treatment: Cross-sectional and longitudinal relationships. Journal of Studies on Alcohol. 2000;61:157–163. doi: 10.15288/jsa.2000.61.157. [DOI] [PubMed] [Google Scholar]
- Heath AC, Todorov AA, Nelson EC, Madden PA, Bucholz KK, Martin NG. Gene–environment interaction effects on behavioral variation and risk of complex disorders: The example of alcoholism and other psychiatric disorders. Twin Research. 2002;5:30–37. doi: 10.1375/1369052022875. [DOI] [PubMed] [Google Scholar]
- Hitman B, Abrams DB, Shadel WG, Niaura R, Borrelli B, Emmons KM, et al. Depressive symptoms and readiness to quit smoking among cigarette smokers in outpatient alcohol treatment. Psychology of Addictive Behaviors. 2002;16:264–268. [PubMed] [Google Scholar]
- Hughes JR, Novy P, Hatsukami DK, Jensen J, Callas PW. Efficacy of nicotine patch in smokers with a history of alcoholism. Alcoholism, Clinical and Experimental Research. 2003;27:946–954. doi: 10.1097/01.ALC.0000071742.86555.4D. [DOI] [PubMed] [Google Scholar]
- Hurt RD, Eberman KM, Croghan IT, Offord KP, Davis LJ, Morse RM, et al. Nicotine dependence treatment during inpatient treatment for other addictions: A prospective intervention trial. Alcoholism, Clinical and Experimental Research. 1994;18:867–872. doi: 10.1111/j.1530-0277.1994.tb00052.x. [DOI] [PubMed] [Google Scholar]
- Joseph AM, Willenbring ML, Nelson D, Nugent SM. Timing of alcohol and smoking cessation study. Alcoholism, Clinical and Experimental Research. 2002;26:1945–1946. doi: 10.1097/01.ALC.0000041004.10869.E0. [DOI] [PubMed] [Google Scholar]
- Kalman K, Hayes K, Colby SM, Eaton CA, Rohsenow DJ, Monti PM. Concurrent versus delayed smoking cessation treatment for persons in early alcohol recovery: A pilot study. Journal of Substance Abuse Treatment. 2001;20:233–238. doi: 10.1016/s0740-5472(00)00174-4. [DOI] [PubMed] [Google Scholar]
- Kohn CS, Tsoh JY, Weisner CM. Changes in smoking status among substance abusers: Baseline characteristics and abstinence from alcohol and drugs at 12-month follow-up. Drug and Alcohol Dependence. 2003;69:61–71. doi: 10.1016/s0376-8716(02)00256-9. [DOI] [PubMed] [Google Scholar]
- Leigh G, Tong JE, Campbell JA. Effects of ethanol and tobacco on divided attention. Journal of Studies on Alcohol. 1977;38:1233–1239. doi: 10.15288/jsa.1977.38.1233. [DOI] [PubMed] [Google Scholar]
- Lemmens P, Tan ES, Knibbe RA. Measuring quantity and frequency of drinking in a general population survey: A comparison of 5 indices. Journal of Studies on Alcohol. 1992;53:476–486. doi: 10.15288/jsa.1992.53.476. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Friedmann PD, Stein MD. The impact of smoking cessation on drug abuse treatment outcome. Addictive Behaviors. 2002;884:1–9. doi: 10.1016/s0306-4603(02)00259-9. [DOI] [PubMed] [Google Scholar]
- Lyon RJ, Tong JE, Leigh G, Claire G. The influence of alcohol and tobacco on the components of choice reaction time. Journal of Studies on Alcohol. 1975;36:587–596. doi: 10.15288/jsa.1975.36.587. [DOI] [PubMed] [Google Scholar]
- Martin JE, Calfas KJ, Patten CA, Polarek M, Hofstetter CR, Noto J, et al. Prospective evaluations of three smoking interventions in 205 recovering alcoholics: One-year results of Project SCRAP-Tobacco. Journal of Consulting and Clinical Psychology. 1997;65:190–194. doi: 10.1037//0022-006x.65.1.190. [DOI] [PubMed] [Google Scholar]
- McCarthy WJ, Zhou Y, Hser Y. Individual change amid stable smoking patterns in polydrug users over 3 years. Addictive Behaviors. 2001;26:143–149. doi: 10.1016/s0306-4603(00)00083-6. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. Smoking and health in substance abusing adolescents: A two-year follow-up. Pediatrics. 1994;93:561–566. [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. National Institutes of Health Volume 5–Form 90: A structured assessment interview for drinking and related behaviors test manual NIH Publication No. 96-4004. 1996 Retrieved from www.niaaa.nih.gov/publications/match-test.htm [on May 16, 2002]
- Perkins KA. Sex differences in nicotine vs. nonnicotine reinforcement as determinants of tobacco smoking. Experimental and Clinical Psychopharmacology. 1996;4:166–177. [Google Scholar]
- Prendergast MA, Harris BR, Mayer S, Littleton JM. Chronic, but not acute, nicotine exposure attenuates ethanol withdrawal-induced hippocampal damage in vitro. Alcoholism, Clinical and Experimental Research. 2000;24:1583–1592. [PubMed] [Google Scholar]
- Project MATCH Research Group Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism, Clinical and Experimental Research. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT user's guide [Version 8] SAS Institute Inc; Cary, NC: 1999. p. 3884. [Google Scholar]
- Schmidt LG, Smolka M. Relapse prevention in alcoholics by cigarette smoking? Involvement of nicotinic–dopaminergic mechanisms. Alcohol. 2001;24:111–115. doi: 10.1016/s0741-8329(01)00129-x. [DOI] [PubMed] [Google Scholar]
- Sees KL, Clark HW. When to begin smoking cessation in substance abusers. Journal of Substance Abuse Treatment. 1993;10:189–195. doi: 10.1016/0740-5472(93)90044-3. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. The Humana Press Inc; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB, Agrawal S. Self-change and dual recoveries among individuals with alcohol and tobacco problems: Current knowledge and future directions. Alcoholism, Clinical and Experimental Research. 2002;26:1936–1938. doi: 10.1097/01.ALC.0000041001.11773.49. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. British Journal of the Addictions. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students' recent drinking history: Utility for alcohol research. Addictive Behaviors. 1986;11:149–162. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Soderpalm B, Ericson M, Olausson P, Blomqvist O, Engel JA. Nicotinic mechanisms involved in the dopamine activating and reinforcing properties of ethanol. Behavioural Brain Research. 2000;113:85–96. doi: 10.1016/s0166-4328(00)00203-5. [DOI] [PubMed] [Google Scholar]
- Stotts AL, Schmitz JM, Grabowski J. Concurrent treatment for alcohol and tobacco dependence: Are patients ready to quit both? Drug and Alcohol Dependence. 2003;69:1–7. doi: 10.1016/s0376-8716(02)00227-2. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Office of Applied Statistics 2001 National Household Survey on Drug Abuse (NHSDA): Alcohol or tobacco use tables. 2002 September 3; Retrieved January 21, 2003 from http://www.samhsa.gov/oas/NHSDA/2k1NHSDA/vol2/appendixh_2.htm.
- Toneatto A, Sobell LC, Sobell MB, Kozlowski LT. Effect of cigarette smoking on alcohol treatment outcome. Journal of Substance Abuse. 1995;7:245–252. doi: 10.1016/0899-3289(95)90008-x. [DOI] [PubMed] [Google Scholar]
- Tong JE, Knott VJ, McGraw DJ, Leigh G. Alcohol, visual discrimination and heart rate: Effects of dose, activation and tobacco. Quarterly Journal of Studies on Alcohol. 1974;35:1003–1022. [PubMed] [Google Scholar]
- Tritto T, Marley RJ, Bastisas D, Stitzel JA, Collins AC. Potential regulation of nicotine and ethanol actions by alpha4-containing nicotinic receptors. Alcohol. 2001;24:69–78. doi: 10.1016/s0741-8329(01)00135-5. [DOI] [PubMed] [Google Scholar]
- True WR, Heath AC, Scherrer JF, Xian H, Lin N, Eisen SA, et al. Interrelationship of genetic and environmental influences on conduct disorder and alcohol and marijuana dependence symptoms. American Journal of Medical Genetics. 1999;88:391–397. doi: 10.1002/(sici)1096-8628(19990820)88:4<391::aid-ajmg17>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, Bar JL, Harley RM, Lyons MJ. The Harvard Twin Study of Substance Abuse: What we have learned. Harvard Review of Psychiatry. 2001;9:267–279. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. National Institute for Alcohol Abuse and Alcoholism . Assessing alcohol problems: A guide for clinicians and researchers. In: Allen JP, Columbus M, editors. NIH Publication No. 95-3745. National Institute of Alcohol Abuse and Alcoholism; Bethesda, MD: 1995. pp. 55–73. [Google Scholar]
- U.S. Department of Health and Human Services. Public Health Service. National Institutes of Health, National Institute of Alcohol Abuse and Alcoholism . Project MATCH Monograph Series. [NIH Publication No. 01-4238] National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. Project MATCH hypotheses: Results and causal chain analysis. [Google Scholar]
- Zimmerman RS, Warheit GJ, Ulbrich PM, Auth JB. The relationship between alcohol use and attempts and success at smoking cessation. Addictive Behaviors. 1990;15:197–207. doi: 10.1016/0306-4603(90)90063-4. [DOI] [PubMed] [Google Scholar]


