Abstract
Most individuals with alcohol use disorders are dependent on both alcohol and nicotine, and combined use of both substances is more damaging to health than use of either alone. Although research indicates that alcoholics can quit smoking, discrepant results have been reported regarding whether smoking cessation is associated with increased risk of alcohol relapse. The purpose of this paper was to examine the relationship between smoking cessation and alcohol consumption using data from Project MATCH. Of the 1,307 participants who smoked at any point during the study, 160 (12%) quit. Quitters consumed less alcohol than those who continued smoking. In addition, quitters demonstrated a significant reduction in alcohol consumption at the time of smoking cessation, which was sustained for six months post-cessation. These findings suggest that individuals in treatment for alcohol use disorders who are motivated to stop smoking can safely be encouraged to do so without jeopardizing their sobriety.
Keywords: Smoking, cessation, alcohol, relapse, abstinence, treatment
ARE INDIVIDUALS IN TREATMENT FOR ALCOHOL USE DISORDERS WHO QUIT SMOKING MORE LIKELY TO RELAPSE?
Introduction
Most individuals with alcohol and drug use disorders are also dependent on nicotine, with rates of current smoking ranging from 60-95%.1-9 They also tend to be heavy smokers.10,11 High smoking rates are likely to continue after substance abuse treatment,12,13 and use of both alcohol/drugs and tobacco appears to be more deleterious to health than use of only a single substance.14-17
Several studies indicate that tobacco treatment, including pharmacotherapy and behavioral interventions, are efficacious for individuals in treatment for substance use disorders.12,16,18-24 One-year post-treatment quit rates, however, are typically lower than those reported for the general population, ranging from 1-13%.12,18,20-26 Despite the dangers of continued smoking and the fact that patients in recovery can stop, substance abuse treatment clinicians are often reluctant to advise their patients to quit smoking.27,28
In terms of alcohol-related outcomes, some research has suggested that continued cigarette use during and after treatment may help to facilitate alcohol consumption, and perhaps relapse, for several reasons. For example, use of one substance may trigger use of the other through conditioning mechanisms (i.e., cross-cue reactivity) because of repeated usage of alcohol/drugs when smoking.29-34 Smoking may have made the shift from moderate to heavy drinking more likely by decreasing the effects of alcohol intoxication, suggesting that smoking may help alcohol consumption continue if relapse occurs.35 In a laboratory study, Cooney et al.36 reported that non-nicotine deprived smokers responded to alcohol cues with increased alcohol and cigarette cravings, whereas nicotine-deprived alcoholics exposed to alcohol cues showed only increased smoking urges but no increased urge to drink.
In contrast however, some research suggests that smoking might actually help those in treatment remain abstinent from alcohol use. Prendergast et al.37,38 found that nicotine decreased the effects of ethanol withdrawal, thereby making at least the initial part of alcoholism treatment more tolerable. Palfai et al.33 reported opposite findings from those of Cooney et al.,36 although their study examined hazardous, and not dependent, drinkers. Expectancies regarding the belief that smoking will help to suppress drinking urges might also play a role cigarettes' role in alcohol abstinence. Colby et al.39 found that alcoholics from a detoxification unit who reported using smoking to cope with urges to drink were less likely to relapse to alcohol use than individuals who rarely or never smoked for this purpose.
Most clinical research studies of patients in treatment for alcohol use disorders in which smoking cessation was a targeted outcome have typically found that smoking cessation enhanced alcohol abstinence, or at least did not hurt sobriety.9,21,40-45 Some research in which patients' smoking was not a focus of treatment have also reported similar results. Lemon et al.43 reported that, among 2,316 smokers in the Drug Abuse Treatment Outcome Study, smoking cessation was related to improved drug abstinence rates (p = .04).
In contrast, Stotts et al.46 examined patients in a dual substance dependency treatment program and found that patients with higher motivation to stop drinking and lower motivation to quit smoking were more likely to remain in treatment. In a clinical trial of an anticraving drug for alcoholics in which cigarette use was not a focus of treatment, Schmidt and Smolka47 reported that smokers showed a trend of maintaining their sobriety longer than continuing nonsmokers (173 vs. 114 days; p = .092). Community studies in which there was no substance use intervention have also found that smoking cessation was associated with increased substance use (e.g., Carmelli et al.48).
In summary, these inconsistencies in the literature suggest that additional research is warranted to test whether smoking cessation is associated with the maintenance of sobriety or with relapse. The purpose of this paper is to examine associations between smoking cessation and alcohol consumption, using data derived from Project MATCH, the largest multi-site randomized clinical trial on alcoholism to date. Our study offers a unique contribution to the literature for several reasons. The reviewed treatment investigations had sample sizes ranging from 155-749 participants, whereas Project MATCH included a far larger sample (N = 1,726). The studies cited above collected follow-up assessments annually or biannually, whereas Project MATCH used prospective data collection methods that assessed participants every 90 days. Moreover, we utilized statistical methods that allow for more accurate conclusions to be drawn from complex, longitudinal data. Developments in statistical methods to study outcome event patterns over time, such as latent growth analysis, have only recently begun to find application in alcohol treatment studies.49 This study is the first application in which time-varying covariates are used to examine the association over time between smoking cessation and drinking.
Because the majority of alcohol treatment studies in which smoking is not a targeted intervention link smoking cessation with increased substance use, we hypothesized that participants who quit smoking will show worse alcohol outcomes, as assessed by percent days abstinent from alcohol use and drinks per drinking day, than continuing smokers. Moreover, we also predicted that smokers who quit smoking during the 15-month investigation will show increased alcohol use after they quit than prior to smoking cessation.
METHODS
Our study was based on Project MATCH, a longitudinal investigation of the effects of three different behavioral interventions for alcohol abuse and dependence that were each delivered over the course of 12 weeks.50 Patients did not receive treatment for their cigarette use.
One thousand seven hundred and twenty-six patients with alcohol abuse and dependence disorders participated in the study. There were two study arms: outpatient and aftercare. Patients in the former were recruited directly from the community or outpatient centers; in the latter, from intensive inpatient or day-hospital treatments. Inclusion criteria included either current (for the outpatient arm) or three months prior to treatment (for the aftercare arm) DSM-III-R diagnosis of alcohol abuse or dependence. Exclusion criteria included if patients met current DSM-III-R diagnosis of dependence for sedative/hypnotic drugs, stimulants, cocaine, or opiates; had taken these drugs intravenously during the previous six months; were currently dangerous to themselves or others; exhibited symptoms of acute psychosis; and/or had severe organic impairment. Participants provided informed consent and the procedures used were in accordance with the standards of the Committee on Human Experimentation with the Helsinki Declaration of 1975.51
For the current investigation, only participants who smoked at some point during the study and who did not have missing smoking data at baseline were included, reducing the final sample to 1,307. Results regarding nonsmokers who initiated smoking during the course of Project MATCH can be found elsewhere.52 Nicotine and alcohol use measures were administered at baseline and 3-, 6-, 9-, 12-, and 15-month follow-up.
Measures
Nicotine use
Nicotine (cigarette) use was assessed at intake and all follow-ups using the Form I-90, developed specifically for Project MATCH.53 This instrument measured nicotine use during the “current period,” corresponding to the preceding 90 days, roughly. Questions regarding nicotine (cigarette) use included (a) ever tobacco use (yes/no), (b) number of lifetime weeks of use, and (c) number of cigarettes per day in the preceding 90.53 Cigarettes per day in the current period was used to determine whether a participant was a current smoker. A participant who reported smoking zero cigarettes per day in a given follow-up period was designated as a nonsmoker, whereas a participant who reported smoking one or more cigarettes was classified as a smoker for that follow-up period.
Alcohol use
Alcohol use was assessed utilizing percent of days abstinent from alcohol use and drinks per drinking day, as measured using the Timeline Follow-Back54 (TLFB), at baseline. The TLFB is a calendar-assisted daily drinking estimation method that provides a comprehensive assessment of a person's drinking over a designated period of time. It has demonstrated adequate psychometric properties in a variety of patient samples.55 The TLFB tends to provide greater estimates of drinking frequency than quantity-frequency measures,56-59 although these differences do not appear to be clinically relevant.55
Data Analysis
Statistical analyses were conducted using SAS version 8(1), using PROC FREQ, PROC ANOVA, and PROC MIXED. To examine differences between quitters and continuing smokers at baseline, nominal data were cross-tabulated and examined for independence by using chi-square tests. Fisher's exact test was used when expected cell frequencies were small. Ordinal data were examined with Wilcoxon tests.
To test the hypothesis that continuing smokers will show greater percent of days abstinent from alcohol use and fewer drinks per drinking day than quitters, we performed random effect regression analyses to examine the relationship between smoking status (smoking vs. quit smoking) and drinking scores during follow-up, with age, education, and baseline percent of days abstinent from alcohol use or drinks per drinking day scores as covariates.
To test the hypothesis that quitters will demonstrate increased alcohol consumption following smoking cessation, we employed latent growth analysis methods to test an interrupted timeseries model for drinking around the time of quitting smoking. Using our prospective methodology, we first identified the month in which a smoker quit smoking, and then examined the drinking scores in the months preceding and following this event. We tested for a step-change in drinking, beginning in the month of quitting smoking and continuing after. Preliminary analyses suggested that a linear timeseries model, allowing for a change in slope and intercept at the time of the event, was adequate. The analysis, relying on the least restrictive assumption available, assumed that the correlations among the time points were unstructured.
Graphing the course of functioning before and after life event
To compliment and extend the latent growth analyses, we graphed the time course of drinking six months prior to and following the time of the event of quitting smoking. We designated the beginning month of the follow-up interval during which a smoker reported no longer smoking as month 0. Percent of days abstinent from alcohol use and drinks per drinking day were then calculated and plotted relative to that time point, up to six months prior to the life event and six months after the event.
RESULTS
Sample Demographic and Baseline Clinical Characteristics
The majority of the sample was male (76%) and Caucasian (89%; see Table 1). Participants were, on average, 39 years old, with 13 years of education. At baseline, approximately 95% of participants were current smokers (N = 1,245), with an average daily consumption of 23.40 cigarettes (SD = 15.00). One hundred and sixty participants (12%) quit smoking over the course of the study. Of baseline smokers who quit within the first six months of our study, approximately 46% were still not smoking at least six months after they stopped.
Table 1.
Patient Demographic and Clinical Characteristics
| Variable | Chronic Smokers (N = 1,147) (88%) |
Quitters (N = 160) (12%) |
Total (N = 1,307) (100%) |
|
|---|---|---|---|---|
| Gender | ||||
| Male | 873 (76) | 120 (24) | 993 (76%) | |
| Female | 274 (75) | 40 (25) | 314 (24%) | |
| Race | ||||
| White | 932 (87%) | 140 (13%) | 1,072 (89%) | |
| African-American | 119 (91%) | 12 (9%) | 131 (10%) | |
| Other | 96 (92%) | 8 (8%) | 104 (8%) | |
| Age (M, SD)* | 39.4 (10.4) | 37.6 (9.5) | 39.2 (10.3) | |
| Years of education (M, SD)* | 13.0 (2.0) | 13.4 (2.0) | 13.1 (2.0) | |
| Lifetime weeks of use (M, SD)** | 1,118.3 (585.4) | 648.3 (600.9) | 1,060.8 (606.9) | |
| Baseline % days abstinent (M, SD)* | 0.31 (0.30) | 0.37 (0.31) | 0.32 (0.30) | |
| Baseline drinks per drinking day (M, SD) | 17.6 (11.1) | 16.2 (10.9) | 17.5 (11.1) | |
Significant difference between chronic smokers and quitters; p < .05
Significant difference between chronic smokers and quitters; p < .0001
We compared smokers who quit smoking (“quitters”) to smokers who continued smoking (“continuing smokers”) on baseline demographic and substance use characteristics. At baseline, quitters were significantly younger and better educated (p < .05), reported greater number of lifetime weeks of tobacco use (p < .0001), smoked fewer cigarettes per day in the past 90 days (p < .0001), and had more baseline percent of days abstinent from alcohol use than continuing smokers (p < .05). There were no significant differences between quitters and continuing smokers on gender, race, or baseline drinks per drinking day.
Between Group Comparisons: Alcohol Consumption in Quitters vs. Continuing Smokers
Cross-sectional rates of smoking were also generally consistent over the course of the study: 95% of the sample was smoking at 3 months, 94% at 6 months, and 93% at 9 months, and 91% at 12 and 15 months. Although most smokers who quit smoking did so within the first six months of the study (i.e., during or immediately after treatment), quit rates remained relatively stable over the course of the investigation. Of the 160 participants who quit smoking, 39 (24%) quit at 3 months, 44 (28%) at 6 months, 23 (14%) at 9 months, 34 (21%) at 12 months, and 20 (12%) at 15 months.
Random effects analyses showed that quitters had greater percent of days abstinent from alcohol use than continuing smokers (p < .001) (see Table 2). On average across all follow-up periods, quitters had 84% days abstinent from alcohol consumption, compared to continuing smokers' 79% days abstinent. Quitters also reported significantly fewer drinks per drinking day than continuing smokers (1.20 vs. 1.47;p < .01). A time effect in both models indicated a significant decrease in alcohol consumption patterns from baseline to 3 months, the months in which treatment occurred. There was no significant difference, however, in the rate of decrease in alcohol consumption between quitters and continuing smokers.
Table 2.
Random Effects by Alcohol Outcome Measure
| Alcohol Outcome Measure | ||||
|---|---|---|---|---|
| Percent of days abstinent | Drinks per drinking day | |||
| F | p | F | p | |
| Smoker status | 8.45 | .0037 | 10.80 | .0010 |
| Time | 14.67 | .0001 | 7.42 | .0001 |
| Smoker status × time | 0.28 | .8887 | 0.73 | .5692 |
Within Group Comparisons: Alcohol Consumption in Quitters
Controlling for the overall time trend of a reduction in alcohol consumption, latent growth analyses showed a statistically significant increase in mean level of percent of days abstinent from drinking and reduction in drinks per drinking day at the time of smoking cessation. Contrary to our hypothesis, however, quitters reported an average increase of 8% days abstinent from alcohol use (p < .05) and an average reduction of 0.5 drinks per drinking day (p < .05) when they stopped smoking. Figure 1 shows the time course of drinking scores six months prior to and following the event of quitting smoking. Decreases in alcohol consumption appeared to begin prior to quitting smoking in the initial treatment months of the study. At the time of quitting smoking, even greater reductions in drinks per drinking day were noted. This decline in alcohol consumption was sustained for at least six months post-cessation.
FIGURE 1.
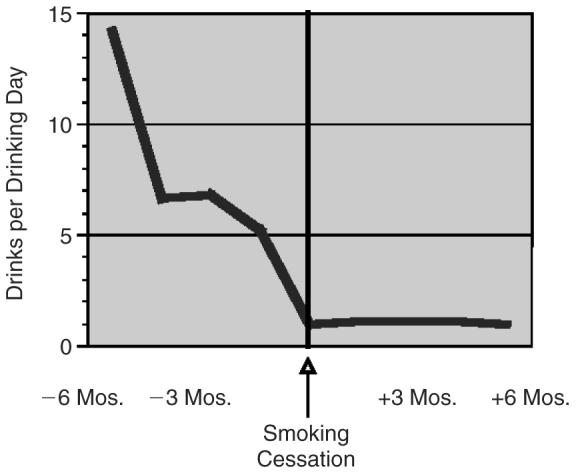
Drinks per Drinking Day Before and After Smoking Cessation
DISCUSSION
The purpose of this study was to investigate whether alcohol outcomes were negatively impacted by smoking cessation among smokers in treatment for alcohol abuse and dependence. Our data were based on Project MATCH, a 15-month study of the efficacy of three behavioral treatments for alcohol abuse and dependence. Both of our hypotheses were disconfirmed.
Smokers who quit smoking during the 15-month investigation reported, on average, lower rates of alcohol consumption, as assessed by percent of days abstinent from alcohol use and drinks per drinking day, than smokers who continued to smoke throughout the duration of the investigation. Moreover, quitters showed significantly greater percent of days abstinent from alcohol use and reduced drinks per drinking day at the time of smoking cessation, which was sustained six months post-quit.
In our investigation, smoking was not a targeted intervention. Since research in which cigarette use is a focus of treatment has shown that stopping smoking may be associated with better alcohol outcomes than continuing smoking, we might assume that our results could have been even more dramatic had smoking been a targeted intervention.
Among those investigations that did not encourage participants to quit smoking, our results are consistent with those of Lemon et al.,43 who found better drug outcomes among quitters, but at odds with those of Schmidt and Smolka.47 These discrepancies suggest that additional studies are merited to determine under what circumstances and in which populations quitting smoking would not be hazardous to drinking outcomes.
Of smokers who stopped smoking within the first six months of the study, approximately 46% retained their nonsmoking status over six months or longer. This quit rate surpasses not only that of untreated smokers in the general population, but and even that of smokers who use intensive pharmacotherapies and/or behavioral treatments.60-62 It is possible that the cessation rate in our study was higher because participants may have been motivated to change habits, such as smoking, that they associated with drinking.63
Our data suggest that, although the motivation to reduce drinking is likely to precede the motivation to quit smoking, quitting smoking does not stop the momentum for continual improvement in alcohol consumption patterns. It is not clear if some aspect of alcoholism treatment and/ or the environment may have provided an opportunity for patients to attempt to quit smoking. Our 12.5% six-month quit rate among smokers not being treated for their tobacco dependence suggests that something about the process of achieving abstinence may have helped motivate participants to stop smoking and stay quit. Future research should examine motivation to address smoking cessation during substance abuse treatment and factors that facilitate or inhibit quit attempts.
This study has several limitations that merit attention. First, inadequate sample size of quitters who were initially nonsmokers prior to treatment did not allow us to examine their patterns of alcohol consumption compared to those who smoked prior to treatment. Second, we used a conservative approach in determining quitter status (no cigarettes vs. one or more cigarettes) in order to identify an event of quitting smoking. Future research might capture changes in smoking consumption patterns, particularly among continuing smokers, by using a continuous measure of cigarette use. Third, our assessments relied only on self-report, without biochemical verification (other than a breathalyzer test for acute alcohol consumption) or collateral corroboration.
These limitations withstanding, our findings suggest that smoking cessation may be related to better drinking outcomes, particularly for less heavy smokers, and provides support for smoking interventions in conjunction with alcohol treatment approaches. Future studies are needed to examine if our results are also applicable for heavy smokers, since the quitters in our study smoked significantly fewer cigarettes per day than continuing smokers. Investigations are needed that examine which individual and environmental factors (e.g., smoking restrictions) were related to the high six-month cessation rate seen in our sample. Research is warranted that attempts to determine whether there is something about the motivation to quit smoking, rather than smoking cessation itself, that is associated with better alcohol use outcomes. Studies that determine how best to address smoking within the context of clinical, rather than research, settings are needed to help bridge the gap in translating study findings from research to practice.
Acknowledgments
The authors would like to thank Benjamin Rodriguez for his helpful comments regarding this manuscript.
The authors acknowledge that the reported results are, in whole or in part, based on analyses of the Project MATCH Public Data Set. These data were collected as part of a multisite clinical trial of alcoholism treatments, which were supported by a series of grants from the National Institute on Alcohol Abuse and Alcoholism and made available to the authors by the Project MATCH Research Group. This paper was not reviewed or endorsed by the Project MATCH Research Group and does not necessarily represent the opinions of its members, who are not responsible for the contents.
This research was funded through NIAAA Grant 2 T32AA07459-16 (Alcohol Intervention/Treatment Outcome Research Training) awarded to Brown University's Center for Alcohol and Addiction Studies.
Footnotes
Publisher's Disclaimer: Copyright of Journal of Addictive Diseases is the property of Haworth Press and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Contributor Information
Karen B. Friend, Karen B. Friend is affiliated with the Pacific Institute for Research and Evaluation, Decision Sciences Institute, and Brown University, Department of Psychiatry and Human Behavior..
Maria E. Pagano, Maria E. Pagano is affiliated with Brown University, Department of Psychiatry and Human Behavior..
REFERENCES
- 1.Batel P, Pessione F, Maitre C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90(7):977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- 2.Burling TA, Ziff DC. Tobacco smoking: a comparison between alcohol and drug abuse inpatients. Addict Behav. 1988;13(2):185–190. doi: 10.1016/0306-4603(88)90010-x. [DOI] [PubMed] [Google Scholar]
- 3.Degenhardt L, Hall W. The relationship between tobacco use, substance-use disorders and mental health: Results from the National Survey of Mental Health and Well-Being. Nicotine and Tobacco Research. 2001;3(3):225–234. doi: 10.1080/14622200110050457. [DOI] [PubMed] [Google Scholar]
- 4.Fiore MC, Bailey WC, Cohen CJ, Dorfman SF, Goldstein MG, Gritz ER, Heyman RB, Jaen CR, Kottke TE, Lando HA, Mecklenburg RE, Mullen PD, Nett LM, Robinson L, Stitzer ML, Tommasello AC, Villejo L, Wewers ME. Clinical practice guideline. U.S. Department of Health and Human Services, Public Health Service; Rockville, Maryland: 2000. Treating tobacco use and dependence. [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Office of Applied Studies 1999 National Household Survey of Drug Abuse, National estimates of substance use. 2000a Retrieved from http://www.health.org/govstudy/bkd376/Chapter2.htm on May 21, 2002.
- 6.Substance Abuse and Mental Health Services Administration. Office of Applied Studies 2000 National Household Survey of Drug Abuse, Illicit drug use. 2001 Retrieved from http://www.samhsa.gov/oas/nhsda/2knhsda/chapter2.htm on May 21, 2002.
- 7.Substance Abuse and Mental Health Services Administration. Office of Applied Statistics 2001 National Household Survey on Drug Abuse (NHSDA): Alcohol or Tobacco Use tables. 2002 September 3; Retrieved from http://www.samhsa.gov/oas/NHSDA/2k1NHSDA/vol2/appendixh_2.htm January 21, 2003.
- 8.Sobell LC, Sobell MB, Brown J, Cleland PA. A randomized trial comparing group versus individual guided self-change treatment for alcohol and drug abusers; the 29th Annual Meeting of the Association for Advancement of Behavior Therapy; Washington, DC. 1995. Presented at. [Google Scholar]
- 9.Toneatto A, Sobell LC, Sobell MB. Effect of cigarette smoking on alcohol treatment outcome. J Subst Abuse. 1995;7(2):245–252. doi: 10.1016/0899-3289(95)90008-x. [DOI] [PubMed] [Google Scholar]
- 10.Collins AC, Marks MJ. Animal models of alcohol-nicotine interactions. In: Fertig JB, Allen JP, editors. Alcohol and tobacco: From basic science to clinical practice. Supt. of Docs., U.S. Govt. Print. Off.; Washington, DC: 1995. pp. 129–144. NIAAA Research Monograph No. 30. NIH Pub. No. 95-3931. [Google Scholar]
- 11.Marks JL, Hill EM, Pomerleau CS, Mudd SA, Blow FC. Nicotine dependence and withdrawal in alcoholic and nonalcoholic ever-smokers. J Subst Abuse Treat. 1997;14(6):512–527. doi: 10.1016/s0740-5472(97)00049-4. [DOI] [PubMed] [Google Scholar]
- 12.Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: Findings from a randomized community intervention trial. Addiction. 1998;93(6):877–887. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- 13.Myers MG, Brown SA. Smoking and health in substance abusing adolescents: A two-year follow-up. Pediatrics. 1994;93:561–566. [PubMed] [Google Scholar]
- 14.Burling TA, Salvio M-A, Seidner AL, Ramsey TG. Cigarette smoking in alcohol and cocaine abusers. J Subst Abuse. 1996;8(4):445–452. doi: 10.1016/s0899-3289(96)90005-x. [DOI] [PubMed] [Google Scholar]
- 15.Elwood JM, Pearson JC, Skippen DH, Jackson SM. Alcohol, smoking, social and occupational factors in the etiology of cancer of the oral cavity, pharynx and larynx. Int J Cancer. 1984;34:603–612. doi: 10.1002/ijc.2910340504. [DOI] [PubMed] [Google Scholar]
- 16.Hurt RD, Offord KL, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, Melton J., III Mortality following inpatient addictions treatment: Role of tobacco use in a community-based cohort. JAMA. 1996;275(14):1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services . The health consequences of smoking: cancer: A report of the Surgeon General. U.S. Government Printing Office; Washington, DC: 1982. [Google Scholar]
- 18.Burling TA, Burling AS, Latini D. A controlled smoking cessation trial for substance-dependent inpatients. Journal of Counseling and Clinical Psychology. 2001;69(2):295–304. doi: 10.1037//0022-006x.69.2.295. [DOI] [PubMed] [Google Scholar]
- 19.Campbell BK, Wander N, Stark MJ, Holbert T. Treating cigarette smoking in drug-abusing clients. J Subst Abuse Treat. 1995;12(2):89–94. doi: 10.1016/0740-5472(95)00002-m. [DOI] [PubMed] [Google Scholar]
- 20.Hughes J. Do smokers with current or past alcoholism need different or more intensive treatment? Alc Clin Exp Res. 2002 December;26:1934–1936. doi: 10.1097/01.ALC.0000041282.57396.30. [DOI] [PubMed] [Google Scholar]
- 21.Hurt RD, Eberman KM, Croghan IT, Offord KP, Davis LJ, Morse RM, Palmen MA, Bruce BK. Nicotine dependence treatment during inpatient treatment for other addictions: A prospective intervention trial. Alc Clin Exp Res. 1994;18:867–872. doi: 10.1111/j.1530-0277.1994.tb00052.x. [DOI] [PubMed] [Google Scholar]
- 22.Irving LM, Seidner AL, Burling TA, Thomas RG, Brenner GF. Drug and alcohol inpatients' attitudes about smoking cessation. J Subst Abuse. 1994;6(3):267–278. doi: 10.1016/s0899-3289(94)90458-8. [DOI] [PubMed] [Google Scholar]
- 23.Joseph AM, Nichol KL, Anderson H. Effect of treatment for nicotine dependence on alcohol and drug treatment outcomes. Addict Behav. 1993;18:635–644. doi: 10.1016/0306-4603(93)90017-4. [DOI] [PubMed] [Google Scholar]
- 24.Rohsenow DJ, Monti P, Colby S, Martin R, Abrams D, Sirota A. Brief interventions for smoking cessation in alcoholic smokers. Alc Clin Exp Res. 2002 December;26(12):1950–1951. doi: 10.1097/01.ALC.0000041006.59547.9A. [DOI] [PubMed] [Google Scholar]
- 25.Burling TA, Marshall GD, Seidner AL. Smoking cessation for substance abuse inpatients. J Subst Abuse. 1991;3:269–276. doi: 10.1016/s0899-3289(10)80011-2. [DOI] [PubMed] [Google Scholar]
- 26.Gariti P, Alterman A, Mulvaney F, Mechanic K, Dhopesh V, Yu E, Chychula N, Sacks D. Nicotine intervention during detoxification and treatment for other substance use. Am J Drug Alcohol Abuse. 2002;28(4):671–679. doi: 10.1081/ada-120015875. [DOI] [PubMed] [Google Scholar]
- 27.Gil BS, Bennett DC. Addiction professionals' attitudes regarding treatment of nicotine dependence. J Subst Abuse Treat. 2000;19(4):317–318. doi: 10.1016/s0740-5472(00)00106-9. [DOI] [PubMed] [Google Scholar]
- 28.Hahn EJ, Warnick TA, Plemmons S. Smoking cessation in drug treatment programs. J Addict Dis. 1999;18(4):89–101. doi: 10.1300/J069v18n04_08. [DOI] [PubMed] [Google Scholar]
- 29.Drobes DJ. Cue reactivity in alcohol and tobacco dependence. Alc Clin Exp Res. 2002 December;26(12):1928–1929. doi: 10.1097/01.ALC.0000040983.23182.3A. [DOI] [PubMed] [Google Scholar]
- 30.Ellingstad TP, Sobell LC, Sobell MB, Cleland PA, Agrawal S. Alcohol abusers who want to quit smoking: Implications for clinical treatment. Drug Alcohol Depend. 1999;54:259–264. doi: 10.1016/s0376-8716(98)00180-x. [DOI] [PubMed] [Google Scholar]
- 31.Gulliver SB, Rohsenow DJ, Colby SM, Dey AN, Abrams DB, Niaura RS, Monti PM. Interrelationship of smoking and alcohol dependence, use and urges to use. J Stud Alcohol. 1995;56:202–206. doi: 10.15288/jsa.1995.56.202. [DOI] [PubMed] [Google Scholar]
- 32.Gulliver SB, Kalman D, Rohsenow DJ, Colby SM, Eaton CA, Monti PM. Smoking and drinking among alcoholics in treatment: Cross-sectional and longitudinal relationships. J Stud Alcohol. 2000;61(1):157–163. doi: 10.15288/jsa.2000.61.157. [DOI] [PubMed] [Google Scholar]
- 33.Palfai TP, Monti PM, Ostafin B, Hutchison K. Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. J Abnorm Psychol. 2000;109(1):96–105. doi: 10.1037//0021-843x.109.1.96. [DOI] [PubMed] [Google Scholar]
- 34.Sayette M. The effects of alcohol on cigarette craving. Alc Clin Exp Res. 2002 December;26(12):1925–1927. doi: 10.1097/01.ALC.0000040961.08770.AD. [DOI] [PubMed] [Google Scholar]
- 35.Madden PA, Heath AC, Starmer GA, Whitfield JB, Martin NG. Alcohol sensitivity and smoking history in men and women. Alc Clin Exp Res. 1995;2003;19(5):1111–1120. doi: 10.1111/j.1530-0277.1995.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 36.Cooney JL, Cooney NL, Pilkey DT, Kranzler HR, Oncken CA. Effects of nicotine deprivation on urges to drink and smoke in alcoholic smokers. Addiction. 2003;98(7):913–921. doi: 10.1046/j.1360-0443.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 37.Prendergast MA, Harris BR, Mayer S, Blanchard JA, Gibson DA, Littleton JM. In vitro effects of ethanol withdrawal and spermidine on viability of hippocampus from male and female rat. Alc Clin Exp Res. 2000;24:1855–1861. [PubMed] [Google Scholar]
- 38.Prendergast MA, Togers DT, Barron S, Bardo MT, Littleton JM. Ethanol and nicotine: A pharmacologic balancing act? Alc Clin Exp Res. 2002 December;26(12):1917–1918. doi: 10.1097/01.ALC.0000040846.27378.80. [DOI] [PubMed] [Google Scholar]
- 39.Colby SM, Rohsenow DJ, Sirota AD, Abrams DB, Niaura RS, Monti PM. Alcoholics' beliefs about quitting smoking during alcohol treatment: Do they make a difference?. In: Monti PM, Abrams DB, editors. Alcohol and nicotine dependence: Biobehavioral mechanisms, treatment, and policy implications; Maui, HI. 1994. Symposium presented at the annual meeting for the Research Society on Alcoholism. [Google Scholar]
- 40.Abrams DB, Monti P, Niaura R, Rohsenow DJ, Colby SM. Interventions for alcoholics who smoke. Alcohol Health and Research World. 1996;2092:111–117. [PMC free article] [PubMed] [Google Scholar]
- 41.Hughes JR, Novy P, Hatsukami DK, Jensen J, Callas PW. Efficacy of nicotine patch in smokers with a history of alcoholism. Alc Clin Exp Res. 2003;27(6):946–954. doi: 10.1097/01.ALC.0000071742.86555.4D. [DOI] [PubMed] [Google Scholar]
- 42.Joseph AM. Nicotine treatment at the drug dependency program of the Minneapolis VA Medical Center. J Subst Abuse Treat. 1993;85:147–152. doi: 10.1016/0740-5472(93)90039-5. [DOI] [PubMed] [Google Scholar]
- 43.Lemon SC, Friedmann PD, Stein MD. The impact of smoking cessation on drug abuse treatment outcome. Addict Behav. 2002;884:1–9. doi: 10.1016/s0306-4603(02)00259-9. [DOI] [PubMed] [Google Scholar]
- 44.Martin JE, Calfas KJ, Patten CA, Polarek M, Hofstetter CR, Noto J, Beach D. Prospective evaluation of three smoking interventions in 205 recovering alcoholics: One-year results of Project SCRAP-Tobacco. Journal of Consulting and Clinical Psychology. 1997;65(1):190–194. doi: 10.1037//0022-006x.65.1.190. [DOI] [PubMed] [Google Scholar]
- 45.Sullivan MA, Covey LS. Current perspectives on smoking cessation among substance abusers. Curr Psychiatry Rep. 2002;4(5):388–396. doi: 10.1007/s11920-002-0087-5. [DOI] [PubMed] [Google Scholar]
- 46.Stotts AL, Schmitz JM, Grabowski J. Concurrent treatment for alcohol and tobacco dependence: Are patients ready to quit both? Drug Alcohol Depend. 2003;69:1–7. doi: 10.1016/s0376-8716(02)00227-2. [DOI] [PubMed] [Google Scholar]
- 47.Schmidt LG, Smolka M. Relapse prevention in alcoholics by cigarette smoking? Involvement of nicotinic-dopaminergic mechanisms. Alcohol. 2001;24(2):111–115. doi: 10.1016/s0741-8329(01)00129-x. [DOI] [PubMed] [Google Scholar]
- 48.Carmelli D, Swan GE, Robinette D. The relationship between quitting smoking and changes in drinking in World War II veteran twins. J Subst Abuse. 1993;5:103–116. doi: 10.1016/0899-3289(93)90055-g. [DOI] [PubMed] [Google Scholar]
- 49.Stout RL. Methodological and statistical considerations in measuring alcohol treatment effects Alcoholism: Clinical and Experimental Research. 2003;27(10):1–6. doi: 10.1097/01.ALC.0000091225.43296.8A. [DOI] [PubMed] [Google Scholar]
- 50.U.S. Department of Health and Human Services. Public Health Service. National Institutes of Health. National Institute of Alcohol Abuse and Alcoholism (Project MATCH Monograph Series. NIH Publication No. 01-4238).Project MATCH hypotheses: Results and causal chain analysis. 2001 [Google Scholar]
- 51.Project MATCH Research Group Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alc Clin Exp Res. 1993;17(6):1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 52.Friend KB, Pagano M. Smoking initiation among alcoholics in treatment. J Subst Abuse Treat. 26(3):219–224. doi: 10.1016/S0740-5472(04)00003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.National Institute of Alcohol Abuse and Alcoholism. National Institutes of Health (NIH Publication No. 96-4004).Volume 5-Form 90: A Structured Assessment Interview for Drinking and Related Behaviors Test Manual. 1996 1996; Retrieved from www.niaaa.nih.gov/publications/match-test.htm on May 16, 2002.
- 54.Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring alcohol consumption. The Humana Press, Inc.; 1992. [Google Scholar]
- 55.U.S. Department of Health and Human Services. National Institute for Alcohol Abuse and Alcoholism . In: Assessing alcohol problems: A guide for clinicians and researchers. Allen JP, Columbus M, editors. National Institute of Alcohol Abuse and Alcoholism; Bethesda, Maryland: 1995. (NIH Publication No. 95-3745). [Google Scholar]
- 56.Grant KA, Tonigan JS, Miller WR. Comparison of three alcohol consumption measures: A concurrent validity study. Journal of Studies on Alcohol. 1995;56(2):168–172. doi: 10.15288/jsa.1995.56.168. [DOI] [PubMed] [Google Scholar]
- 57.Lemmens P, Tan ES, Knibbe RA. Measuring quantity and frequency of drinking in a general population survey: A comparison of 5 indices. Journal of Studies on Alcohol. 1992;53:476–486. doi: 10.15288/jsa.1992.53.476. [DOI] [PubMed] [Google Scholar]
- 58.Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students' recent drinking history: Utility for alcohol research. Addict Behav. 1986;11:149–162. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- 59.Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. British Journal of the Addictions. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 60.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, Heyman RB, Jaen CR, Kottke TE, Lando HA, Mecklenburg RE, Mullen PD, Nett LM, Robinson L, Stitzer ML, Tommasello AC, Villejo L, Wewers ME. Treating tobacco use and dependence. Clinical practice guideline. U.S. Department of Health and Human Services, Public Health Service; Rockville, Maryland: 2000. [Google Scholar]
- 61.Stead LF, Lancaster T. The Cochrane Library. 1. John Wiley & Sons, Ltd.; Chichester, UK: 2004. Individual behavioural counseling for smoking cessation (Cochrane Review) [Google Scholar]
- 62.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. The Cochrane Library. 1. John Wiley & Sons, Ltd.; Chichester, UK: 2004. Nicotine replacement therapy for smoking cessation (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 63.Bobo JK, Husten C. Sociocultural influences on smoking and drinking. Alcohol Research and Health. 2000;24(4):225–232. [PMC free article] [PubMed] [Google Scholar]


