Abstract
Objective To estimate the one year prognosis and identify prognostic factors in cases of recent onset low back pain managed in primary care.
Design Cohort study with one year follow-up.
Setting Primary care clinics in Sydney, Australia.
Participants An inception cohort of 973 consecutive primary care patients (mean age 43.3, 54.8% men) with non-specific low back pain of less than two weeks’ duration recruited from the clinics of 170 general practitioners, physiotherapists, and chiropractors.
Main outcome measures Participants completed a baseline questionnaire and were contacted six weeks, three months, and 12 months after the initial consultation. Recovery was assessed in terms of return to work, return to function, and resolution of pain. The association between potential prognostic factors and time to recovery was modelled with Cox regression.
Results The follow-up rate over the 12 months was more than 97%. Half of those who reduced their work status at baseline had returned to previous work status within 14 days (95% confidence interval 11 to 17 days) and 83% had returned to previous work status by three months. Disability (median recovery time 31 days, 25 to 37 days) and pain (median 58 days, 52 to 63 days) took much longer to resolve. Only 72% of participants had completely recovered 12 months after the baseline consultation. Older age, compensation cases, higher pain intensity, longer duration of low back pain before consultation, more days of reduced activity because of lower back pain before consultation, feelings of depression, and a perceived risk of persistence were each associated with a longer time to recovery.
Conclusions In this cohort of patients with acute low back pain in primary care, prognosis was not as favourable as claimed in clinical practice guidelines. Recovery was slow for most patients. Nearly a third of patients did not recover from the presenting episode within a year.
Introduction
On any given day 12-33% of people report low back pain.1 The costs of treatment are enormous: in Australia, a country of 21 million people, the treatments costs are about $A1bn (£0.5bn, €0.6bn, $0.9bn) a year.2
There is evidence that the type of advice given to patients can alter the course of an episode of low back pain.3 4 For this reason, most management guidelines recommend that patients should be reassured that they have a favourable prognosis. This recommendation is commonly supported with the statement that 90% of patients recover within six weeks.5 6 Such statements, however, might be too optimistic. While patients typically improve rapidly, the risk of developing chronic low back pain (that is, pain persisting for more than three months) is uncertain.7 8 9 Estimates of this risk vary from 2%10 to 56%.11
To provide individualised advice, it is also necessary to consider prognostic factors. All guidelines for low back pain recommend identification of adverse prognostic factors, commonly described as “yellow flags.” Examples of yellow flags include fear of re-injury, leg pain, or low job satisfaction. While all guidelines endorse screening for prognostic factors, there is considerable uncertainty regarding the choice of these factors and their predictive value.7 8 9
The lack of consensus regarding the prognosis and prognostic factors for recent onset low back pain has been attributed to methodological shortcomings of previous studies.8 9 12 The most common shortcomings are failure to recruit a representative sample of patients and healthcare providers,10 11 13 14 incomplete follow-up,13 14 and inadequate duration of follow-up.10 15 Our previous review9 found only 15 methodologically sound studies, and, of these, only two provided information on outcomes beyond three months. Without accurate data on prognosis and prognostic factors clinicians are unable to provide appropriate information and advice to their patients with acute low back pain.
We conducted a cohort study with the primary aim of determining the long term (one year) prognosis for people with recent onset low back pain presenting to primary care clinicians. Our secondary aim was to identify patients’ characteristics that could be readily assessed by a primary care clinician and were associated with poor prognosis.
Methods
The protocol for this study has been published previously.16 We recruited an inception cohort of 973 participants from a socioeconomically diverse region in the Sydney metropolitan area of Australia. Consecutive patients with recent onset low back pain who presented to primary care were invited to participate.
In many parts of the world, including Australia, the management of low back pain in primary care is usually provided by general practitioners, physiotherapists, and chiropractors.17 We invited all such clinicians practising within the study area to participate. Participating clinicians screened all patients with the primary complaint of low back pain who presented to their clinics from November 2003 to July 2005.
Low back pain was defined as pain in the area bounded superiorly by T12 and inferiorly by the buttock crease,18 lasting for more than 24 hours but less than two weeks, and preceded by a period of at least one month without back pain.19 To be eligible, participating patients had to be at least 14 years old, provide written consent to participate in the study, and be able to speak and read English. Participants were excluded if a serious pathology (such as cancer, spinal infection, spinal fracture, and inflammatory arthritis) had already been diagnosed as the cause of the current episode of low back pain when they visited the primary care clinician or if serious pathology was established during the course of the study. Participants with radiculopathy were also excluded. The clinicians were given a copy of the most recent clinical guidelines for low back pain20 and asked to follow the guidelines when appropriate.
Baseline data were collected at the first consultation with the primary care clinician. These data were used to describe the cohort and to evaluate putative predictors of outcome. The individual variables were grouped into seven factors: current history; past history; red flags (features associated with serious spinal pathology); sociodemographics; general health; psychological; and work.These seven factors have been suggested to be associated with a poor outcome, but there is little consensus regarding which are important.21 22 23 Low back pain and disability were also measured at baseline with adaptations of items 7 and 8 of the SF-3624: How much low back pain have you had in the past week? and During the past week, how much did low back pain interfere with your normal work (including both work outside the home and housework?). The original wording was changed from “bodily pain” to “low back pain” to reflect our specific interest in low back pain. To compensate clinicians for their time they were paid $A10 for each screened ineligible patient, $A50 for each enrolled patient, and $A100 for each verified case of serious pathology.
Researchers conducted follow-up assessments by telephone interview at six weeks, three months, and 12 months after the initial assessment. As there is no universally accepted single measure of recovery from low back pain, we sampled three dimensions of recovery—pain intensity, disability, and work status—which participants were asked to rate at each time point. Interviewers also established whether the patient had recovered on each of these dimensions and if so the date of recovery. When participants reported being pain-free, or without disability, or having returned to previous work status, and that was sustained for a whole month, they were considered “recovered” in that dimension at the beginning of that month.19 A fourth measure of recovery—“complete recovery”—required the patient to recover on all three dimensions. For this last measure, we ignored the return to work dimension for participants who were not seeking work.
Data analysis
We used the dates on which participants returned to pre-injury work status and/or had no disability and/or had no pain to construct survival curves. The survival curves were used to describe the prognosis of participants with non-specific low back pain presenting to primary care practitioners. Median survival time (days to recovery) was determined for each of the three recovery measures individually and for attainment of all three recovery measures.
We used Cox regression to identify the independent associations between the seven factors and the time to complete recovery from acute low back pain. Firstly, we carried out a univariate analysis to test for an association between each individual variable and time to recovery (see bmj.com). Variables with significant association (P<0.10) were retained as components of their seven factors. If any of the seven factors had no variables significantly associated with time to recovery, it was excluded from further analyses. Participants’ age, sex, intensity of low back pain, and level of interference with function at baseline were considered to be prognostic covariates and were forced into the multivariate analysis. A forward selection procedure was used to sequentially add factors to the model. At each step the factor with the greatest additional explanatory value was added to the model. Factors that did not add significantly to the model were excluded from further analyses. All analyses were performed with SPSS for Windows version 14.0 (SPSS, Chicago, IL).
Results
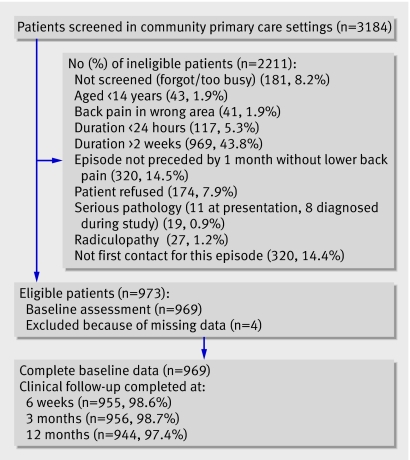
A total of 1254 clinicians in the study region were identified and contacted. Of these, 170 (73 general medical practitioners, 77 physiotherapists, and 20 chiropractors) worked in primary care, agreed to participate, and were trained in the study protocol. The trained clinicians screened 3184 consecutive patients with low back pain from November 2003 to July 2005. Of these, 973 patients (mean age 43.3, 54.8% men) had non-specific low back pain of less than two weeks’ duration and were thus eligible to participate (fig 1). Figure 1 also shows reasons for ineligibility. Data on individual items of the baseline questionnaire were missing for four participants (0.4%). As few data were missing, we excluded participants with missing baseline data from all analyses. The follow-up rate remained above 97% over the 12 month period. Participants for whom we did not have complete follow-up data and who had not reported recovery from their low back pain were censored at the time of their last follow-up.
Fig 1 Flowchart of participants through study
Table 1 shows baseline demographic and clinical features of participants. We used the participant’s postcode and data from the Australian census to judge socioeconomic disadvantage: 21.4% fell in the most disadvantaged quarter, 8.4% in the second quarter, 14.8% in the third quarter, and 55.1% in the fourth quarter.
Table 1.
Baseline characteristics of eligible participants. Figures are numbers (percentages) of patients unless stated otherwise
| Variable | Participants (n=969) |
|---|---|
| Mean (SD) age (years) | 43.3 (14.4) |
| Male | 527 (54.8) |
| Primary care clinician: | |
| General practitioner | 184 (19.0) |
| Physiotherapist | 755 (77.9) |
| Chiropractor | 30 (3.1) |
| Born in Australia | 680 (70.2) |
| Aboriginal/Torres Strait Islander | 8 (0.8) |
| Smoker | 188 (19.4) |
| Exercising regularly | 564 (58.2) |
| Self rated health: | |
| Poor | 3 (0.3) |
| Fair | 63 (6.5) |
| Good | 338 (34.9) |
| Very good | 397 (41.0) |
| Excellent | 168 (17.3) |
| Highest level of education diploma or higher* | 411 (42.4) |
| Details of lower back pain: | |
| Previous episode | 727 (75.0) |
| Previous sick leave | 381 (39.3) |
| Previous surgery | 26 (2.7) |
| Sudden onset | 797 (82.2) |
| Compensation case† | 189 (19.2) |
| Currently taking medication | 399 (41.20) |
| Mean (SD) duration (days) | 4.9 (3.3) |
| Mean (SD) days of forced reduction of usual activities | 3.1 (2.8) |
| Interference with function from lower back pain: | |
| Not at all | 59 (6.1) |
| Little bit | 133 (13.7) |
| Moderate | 215 (22.2) |
| Quite a bit | 373 (38.5) |
| Extreme | 189 (19.5) |
| Leg pain | 199 (20.5) |
| Intensity of lower back pain: | |
| Very mild | 22 (2.1) |
| Mild | 85 (8.8) |
| Moderate | 349 (36.0) |
| Severe | 426 (44.0) |
| Very severe | 87 (8.9) |
| Mean (SD) days off from work or school from lower back pain (n=814) | 1.5 (2.2) |
| Working before injury | 770 (79.5) |
| Changed work status as result (n=770) | 291 (38.0) |
*Post-school education.
†Worker’s compensation and third party motor vehicle insurance cases.
There were 770 (79.5%) participants who reported working before the onset of their episode of acute low back pain. Of these, 291 (37.8% of workers, 30.0% of the total cohort) reported changing their work status as a result of their low back pain. The median time to return to previous work hours and duties for these 291 participants was 14 days (95% confidence interval 11 to 17 days). Kaplan-Meier curves (see bmj.com) showed that the cumulative probability of returning to pre-back pain work hours and duties for those who reduced their work status at baseline because of low back pain was 74.6% at six weeks, 83.2% at 12 weeks, and 89.5% one year after consulting a primary care clinician for acute low back pain.
The median time to recovery in terms of disability was 31 days (25 to 37 days). By six weeks the cumulative probability of having no disability was 54.9%. This probability increased to 73.3% by 12 weeks, and 83.3% by one year. The median time to recovery in terms of pain after an episode of acute low back pain was 58 days (53 to 63 days). The cumulative probability of being pain-free was 39.9% by six weeks, 58.2% by 12 weeks, and 72.5% by one year. See bmj.com for further details.
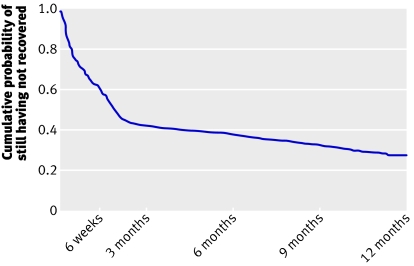
Complete recovery from recent onset low back pain, determined by recovery on all three dimensions (return to work, no disability, and no pain) took a median time of 59 days (53 to 65 days). Six weeks after presentation to primary care, the cumulative probability of recovery was 39.0%. By 12 weeks the probability was 57.4%, and this increased to 71.8% by one year (fig 2).
Fig 2 Kaplan-Meier estimate of time to complete recovery, determined by phone follow-up at six weeks, three months, and 12 months. Participants were interviewed to establish if they had recovered (no pain for one month AND no disability for one month AND returned to previous work status for one month). If they had recovered they were asked to nominate start date of one month period. This date was used to determine time to recovery. Curves are not smoothed but appear so because of large sample size
Table 2 shows pain, disability, and work status assessed at study entry and each follow-up. At six weeks, three months, and 12 months, 40%, 52%, and 57% of participants reported being pain-free; 60%, 71%, and 75% reported being disability-free. Immediately before the onset of the episode 77% were working full time and this reduced to 48% at baseline, rising to 69%, 72%, and 72% at six weeks, three months, and 12 months. At 12 months the participants’ responses to the question “If you had to live with the symptoms you have right now, how would you feel about it?” were generally positive, though 133 of the 969 participants reported feeling very dissatisfied and 106 somewhat dissatisfied.
Table 2.
Pain, disability, and work status of 969 participants immediately before onset of episode and at study entry, six weeks, three months, and 12 months. Figures are numbers (percentages) of participants
| Pre-episode | Study entry | 6 weeks | 3 months | 12 months | |
|---|---|---|---|---|---|
| Pain: | |||||
| None | * | 0 | 382 (39.5) | 499 (51.5) | 556 (57.4) |
| Very mild | * | 22 (2.3) | 195 (20.0) | 158 (16.3) | 100 (10.3) |
| Mild | * | 85 (8.7) | 213 (22.0) | 153 (15.8) | 132 (13.6) |
| Moderate | * | 349 (36.0) | 128 (13.3) | 120 (12.4) | 128 (13.2) |
| Severe | * | 426 (44.0) | 34 (3.5) | 26 (2.7) | 23 (2.4) |
| Very severe | * | 87 (9.0) | 3 (0.3) | 0 | 5 (0.5) |
| Disability: | |||||
| Not at all | * | 59 (6.0) | 584 (60.3) | 691 (71.4) | 725 (74.8) |
| Little bit | * | 133 (13.7) | 188 (19.4) | 135 (13.9) | 110 (11.4) |
| Moderate | * | 215 (22.2) | 115 (11.9) | 89 (9.2) | 84 (8.7) |
| Quite a bit | * | 373 (38.6) | 53 (5.5) | 37 (3.8) | 22 (2.3) |
| Extreme | * | 189 (19.5) | 15 (1.5) | 4 (0.4) | 3 (0.2) |
| Work status: | |||||
| Employed: | |||||
| Full duties | 742 (76.6) | 461 (47.6) | 670 (69.1) | 696 (71.8) | 699 (72.2) |
| Selected duties | 27 (2.8) | 145 (15.0) | 75 (7.7) | 59 (6.1) | 40 (4.1) |
| Sick leave | 7 (0.7) | 159 (16.4) | 17 (1.8) | 12 (1.2) | 12 (1.2) |
| Maternity or long service leave | 17 (1.8) | 19 (2.0) | 10 (1.0) | 8 (0.8) | 7 (0.7) |
| Unemployed | 30 (3.1) | 36 (3.7) | 35 (3.6) | 33 (3.4) | 33 (3.4) |
| Not seeking paid employment, such as retired | 142 (14.7) | 145 (15.0) | 143 (14.9) | 143 (14.9) | 148 (15.3) |
| Other | 4 (0.3) | 4 (0.3) | 5 (0.5) | 5 (0.5) | 5 (0.5) |
| Missing data | 0 | 0 | 14 (1.4) | 13 (1.3) | 25 (2.6) |
*Not formally measured but study inclusion was that current episode was preceded by period of at least one month without back pain.
Full results for the univariate Cox regression analyses are on bmj.com. Cultural variables were not significantly associated with time to recovery. After adjustment for age, sex, intensity of pain, and interference with function, psychological characteristics were most closely associated with time to recovery (χ2=81.51, P<0.001). Of the other factors, only factors related to current history further contributed significantly to the model (χ2=36.72, P≤0.001, table 3). Seven individual variables were independently associated with time to recovery: age, intensity of pain, feelings of depression, risk of persistence, low back pain in compensation cases, days of reduced activity, and duration of the episode.
Table 3.
Cox regression model for time to complete recovery from acute low back pain (LBP) with hazard ratios (HR) and 95% confidence intervals
| Variable | Crude (unadjusted) | Adjusted | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Age (years) | 1.00 (0.99 to 1.00) | 0.090 | 0.99 (0.99 to 1.00) | 0.004 | |
| Male | 1.05 (0.91 to 1.23) | 0.500 | 1.01 (0.86 to 1.18) | 0.900 | |
| Pain/disability (χ2=31.32, P<0.001) | |||||
| Pain intensity* | 0.79 (0.73 to 0.86) | <0.001 | 0.86 (0.77 to 0.96) | 0.009 | |
| Interference with function† | 0.85 (0.90 to 0.91) | <0.001 | 0.96 (0.88 to 1.05) | 0.339 | |
| Psychological (χ2=81.51, P<0.001) | |||||
| Pain control§ | 1.04 (1.01 to 1.07) | 0.010 | 1.02 (0.99 to 1.05) | 0.267 | |
| Tension/anxiety¶ | 0.94 (0.91 to 0.96) | <0.001 | 1.02 (0.99 to 1.06) | 0.208 | |
| Feelings of depression¶ | 0.91 (0.89 to 0.93) | <0.001 | 0.94 (0.91 to 0.97) | <0.001 | |
| Risk of persistence¶ | 0.89 (0.87 to 0.92) | <0.001 | 0.92 (0.89 to 0.95) | <0.001 | |
| Current history (χ2=36.72, P<0.001) | |||||
| Compensable LBP¶ | 0.56 (0.45 to 0.69) | <0.001 | 0.59 (0.47 to 0.74) | <0.001 | |
| Currently taking medication for LBP | 0.75 (0.65 to 0.88) | <0.001 | 0.96 (0.81 to 1.14) | 0.657 | |
| Days of reduced activity due to LBP¶ | 0.96 (0.93 to 0.99) | 0.005 | 1.04 (1.00 to 1.08) | 0.033 | |
| Leg pain¶ | 0.71 (0.59 to 0.86) | 0.001 | 0.90 (0.70 to 1.16) | 0.408 | |
| No of pain sites‡ | 0.83 (0.75 to 0.91) | <0.001 | 0.92 (0.81 to 1.03) | 0.147 | |
| Duration of episode | 0.97 (0.95 to 0.99) | 0.030 | 0.97 (0.94 to 1.0) | 0.033 | |
| Clinical red flags (not included in model) | |||||
| No of positive red flags | 0.95 (0.91 to 1.00) | 0.048 | — | ||
*Pain intensity scale: 1=none, 2=very mild, 3=mild, 4=moderate, 5=severe, 6=very severe.
†Disability scale: 1=not at all, 2=little bit, 3=moderate, 4=quite a bit, 5=extreme.
§Rated on scale from 0-10, with higher score indicating better ability to control pain.
¶Rated on scales from 0-10, with higher scores indicating more tension and anxiety, more feelings of depression, or higher risk of persistent pain.
‡One point for each pain site: neck, shoulder, upper back, lower back, and leg.
Discussion
In this study of 12 month prognosis in patients with recent onset low back pain, recovery was typically much slower than previously reported. Nearly a third of patients did not recover from the presenting episode within a year. Return to work and recovery from disability and pain did not occur synchronously. We identified seven readily assessed factors that were associated with speed of recovery and can be considered by clinicians when advising their patients about the prognosis for their episode of acute low back pain.
Strengths and weaknesses
The strengths of our study are that we enrolled an inception cohort from the three main primary care providers who manage low back pain and measured pain, disability, and work status over a 12 month period with high rates of follow-up. Our previous review of prognostic studies of low back pain found that few studies of acute low back pain have achieved these benchmarks.9 A limitation of the study is that socioeconomically disadvantaged people were under-represented in the cohort. There are many health conditions where socioeconomic disadvantage has been linked to poor outcome, and if this applies to low back pain it might be that we have produced an overly optimistic view of prognosis. Another limitation is that we did not record participants’ occupation so we were unable to assess whether this factor influenced the speed with which people returned to work.
Comparison with other research
There are only a few methodologically sound prognosis studies that have followed patients beyond three months.9 Schiottz-Christensen et al enrolled 524 patients from Danish primary care whose pain had lasted less than two weeks and found that recovery was slow and incomplete.11 Complete recovery was 41% by one month, 44% by six months, and 54% by 12 months; results quite similar to our six week, three month, and 12 month figures of 39%, 57%, and 72%. In contrast, Coste et al reported that recovery was rapid.10 They reported that 90% of their cohort had recovered by two weeks whereas in our study only 23% had recovered by two weeks and in the study of Schiottz-Christensen et al only 41% had recovered by four weeks (recovery data for two weeks are not reported). Coste et al enrolled 103 patients from French primary care and, unlike in our study and that of Schiottz-Christensen et al, used a cut-off of 72 hours to define an inception cohort.10 To test the effect of Coste et al’s stricter criterion, we repeated our survival analysis on the subset of participants (n=530) whose back pain had lasted for up to three days but found the recovery rate virtually unchanged at two weeks. Accordingly, we are unable to explain the marked difference in results.
There are difficulties comparing prognostic factors between our study and those of Coste et al10 and Schiottz-Christensen et al11 because there was not a common set of predictors, the studies used different approaches to building a prognostic model, and with 103,10 524,11 and 969 participants had quite different statistical power to detect prognostic associations. None the less, there are some common findings. All three studies report that low back pain in compensation cases and high disability at baseline were adverse prognostic factors, and our study and the study by Coste et al10 report that a previous episode of low back pain was an adverse prognostic factor. In common with our study, Schiottz-Christensen et al reported that perceived risk of persistence was an adverse prognostic factor,11 but in that study the clinician judged risk of persistence whereas in our study this judgment was made by the patient.
Implications for the guidelines
Our findings support the recommendations in clinical practice guidelines that clinicians should screen for adverse prognostic factors (yellow flags). We identified seven factors associated with poor prognosis that could be readily applied in primary care. These results also concur with the view that psychosocial factors are important factors predicting poor outcome. In contrast to most guidelines we found that recovery from low back pain is typically slow and incomplete. The slow and incomplete recovery occurred even though we trained all clinicians in the study to provide best practice care consistent with current clinical guidelines. At the moment it is unclear how better health outcomes can be achieved. Establishing whether it is the endorsed treatments or their implementation that is the problem could help to improve outcomes for acute low back pain.
Recovery did not occur synchronously in the three dimensions of return to work, interference with function, and pain status. Most patients who reduced their work status as a result of their low back pain resumed their pre-back pain work status quickly, but this was not indicative of recovery from an episode of low back pain. The return to pre-injury work hours and duties occurred more quickly and in more participants than recovery from pain or interference with function. Of the three dimensions used to measure recovery, pain took the longest to resolve. In fact the survival curves for recovery from pain and complete recovery were similar. This indicates that the primary impediment to complete recovery is ongoing pain. Nearly a third of the participants had not recovered from the initial episode by 12 months.
Despite widespread investigation, there has been little consensus regarding predictors of outcome from acute low back pain.12 25 Rather than testing the predictive value of large numbers of individual variables, as is common practice, we grouped potential predictive variables into discrete factors, controlling for demographic and pain related covariates. While the factors might not have been able to fully describe complex constructs such as culture and psychology, factor items were taken from validated questionnaires.17 25 26 Using this approach we identified seven variables that were independently associated with poor prognosis. Psychological characteristics (feelings of depression and perceived risk of persistence) were most closely associated with time to recovery, while characteristics of the current history (low back pain in compensation cases and duration of episode) were still significantly associated with time to recovery after we accounted for psychological characteristics.
The most obvious use of prognostic information is to provide patient specific estimates of prognosis to individual patients in primary care. The prognostic factors we identified are readily assessed in primary care. That treatment should be targeted towards factors that have an adverse effect on recovery,22 and our findings provide some insight into how this might be achieved in primary care. For example, as compensation status was the strongest predictor, it might be worth investigating the process of care for a cohort of patients in compensation cases to identify potential causes of delayed recovery. In addition, our findings suggest that effective strategies could be investigated for the assessment and management of symptoms of depression and catastrophising. Further studies are warranted to evaluate the validity of these predictors in other cohorts of patients with acute low back pain in primary care.
What is already known on this topic
Clinical practice guidelines suggest that recovery from an episode of recent onset low back pain is usually rapid and complete
Recent systematic reviews suggest that the risk of developing chronic low back pain is uncertain
What this study adds
In this cohort of patients, recovery from recent onset low back pain was much slower than has been reported and nearly a third did not recover within a year
Older age, back pain associated with compensation cases, higher pain intensity, longer duration of low back pain before consultation, more days of reduced activity because of low back pain before consultation, feelings of depression, and a perceived risk of persistence were all associated with poorer prognosis
Contributors: CGM, KMR, RDH, RGC, and JB were the chief investigators on the NHMRC project grant that funded the study. All authors contributed to the design of the study. NH, AD, JHMc, CGM, KMR, JB, and JY trained the recruiting clinicians. NH, AD, and JHMc conducted the follow-up assessments and entered and double checked the data. All authors contributed to the analysis and interpretation of the data and reviewed and approved the final version of the manuscript. CGM is guarantor.
Funding: National Health and Medical Research Council of Australia.
Competing interests: None declared.
Ethical approval: University of Sydney human research ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Cite this as: BMJ 2008;337:a171
References
- 1.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 2000;13:205-17. [DOI] [PubMed] [Google Scholar]
- 2.Walker B, Muller R, Grant W. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health 2003;15:79-87. [DOI] [PubMed] [Google Scholar]
- 3.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomised clinical trial. Spine 1995;20:473-7. [DOI] [PubMed] [Google Scholar]
- 4.Hagen E, Eriksen H, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine 2000;25:1973-6. [DOI] [PubMed] [Google Scholar]
- 5.Van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15:S169-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waddell G, Feder G, McIntosh A, Lewis M, Hutchinson A. Low back pain evidence review 1st ed. London: Royal College of General Practitioners, 1996
- 7.Abbott J, Mercer S. The natural history of acute low back pain. N Z J Physiother 2002;30:8-16. [Google Scholar]
- 8.Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J 2003;12:149-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pengel L, Herbert R, Maher C, Refshauge K. Acute low back pain: systematic review of its prognosis. BMJ 2003;327:323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coste J, Delecoeuillerie G, Cohen de Lara A, Le Parc JM, Paolaggi JB. Clinical course and prognostic factors in acute low back pain: an inception cohort study in primary care practice. BMJ 1994;308:577-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schiottz-Christensen B, Nielsen GL, Hansen VK, Schodt T, Sorensen HT, Olesen F. Long-term prognosis of acute low back pain in patients seen in general practice: a 1-year prospective follow-up study. Fam Pract 1999;16:223-32. [DOI] [PubMed] [Google Scholar]
- 12.McIntosh G, Frank J, Hogg-Johnson S, Hall H, Bombardier C. Low back pain prognosis: structured review of the literature. J Occ Rehabil 2000;10:101-15. [Google Scholar]
- 13.Klenerman L, Slade P, Stanley I, Pennie B, Reily J, Atchison L, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine 1995;20:478-84. [DOI] [PubMed] [Google Scholar]
- 14.Sieben J, Vlaeyen J, Tuerlinckx S, Portegijs P. Pain-related fear in acute low back pain: the first two weeks of a new episode. Eur J Pain 2002;6:229-37. [DOI] [PubMed] [Google Scholar]
- 15.Grotle M, Brox JI, Veierod MB, Glomsrod B, Lonn JH, Vollestad NK. Clinical course and prognostic factors in acute low back pain: patients consulting primary care for the first time. Spine 2005;30:976-82. [DOI] [PubMed] [Google Scholar]
- 16.Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prognosis of acute low back pain: design of a prospective inception cohort study. BMC Musculoskelet Disord 2006;7:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker B, Muller R, Grant W. Low back pain in Australian adults. Health provider utilization and care seeking. J Manipulative Physiol Ther 2004;27:327-35. [DOI] [PubMed] [Google Scholar]
- 18.Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DP, Silman AJ, et al. Low back pain in schoolchildren: the role of mechanical and psychosocial factors. Arch Dis Child 2003;88:12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de vet H, Heymans M, Dunn K, Pope D, van der Beek A, Macfarlane G, et al. Episodes of low back pain. A proposal for uniform definitions to be used in research. Spine 2002;27:2409-16. [DOI] [PubMed] [Google Scholar]
- 20.NHMRC. Evidence-based management of acute musculoskeletal pain Canberra: National Health and Medical Research Council, 2003 [DOI] [PubMed]
- 21.Bekkering GE, Hendriks HJ, van Tulder MW, Knol DL, Simmonds MJ, Oostendorp RA, et al. Prognostic factors for low back pain in patients referred for physiotherapy: comparing outcomes and varying modeling techniques. Spine 2005;30:1881-6. [DOI] [PubMed] [Google Scholar]
- 22.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002;27:e109-20. [DOI] [PubMed] [Google Scholar]
- 23.Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med 2005;62:851-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ware J, Sherbourne C. The MOS 36-item short-form health survey (SF-36). 1. Conceptual framework and item selection. Med Care 1992;30:473-83. [PubMed] [Google Scholar]
- 25.Kent PM, Keating JL. Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review. Man Ther 2008;13:12-28. [DOI] [PubMed] [Google Scholar]
- 26.Linton SJ, Hallden K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain 1998;14:209-15. [DOI] [PubMed] [Google Scholar]