Abstract
This study assessed and compared the efficacy of culturally tailored behavioral interventions to increase use and acceptability of sexual barrier products among HIV-positive women in Zambia. It also sought to evaluate cultural preferences as facilitators or impediments to potential use of vaginal chemical barriers for sexual risk reduction within the Zambian context. Women (N = 240), recruited from the University Teaching Hospital HIV Voluntary Counseling and Testing Center, were randomized into group or individual intervention arms. Participants attended a baseline assessment, three intervention sessions and follow up assessments at six and 12 months. All participants increased use and acceptability of female condoms and vaginal products and maintained male condom use at six and 12 months. Preliminary data indicated that group participants increased male condom use at six months and trial use and acceptability of female condoms and lubricants predicted their use in the group condition. Results support group interventions to increase sexual barrier use and acceptability in HIV-positive women within the Zambian context. From a public health standpoint, groups may represent a cost-effective and culturally congruent intervention.
Introduction
Of the 25.4 million persons infected with HIV in sub-Saharan Africa, 13.3 million (57%) are women (UNAIDS-WHO, 2004). Zambia, a country of 10.6 million, has adult (ages 15–49) infection rates approaching 25% (UNAIDS-WHO, 2002). Among women tested for HIV during pregnancy in Lusaka, 27% were HIV-positive in 1997 (Fylkesnes et al., 1997), 29% were HIV-positive in 2000 (UNAIDS-WHO, 2000) and as many as 50% in selected urban clinics were HIV-positive in 2002 (Central Statistical Office, Zambia (CSOZ), 2002). Life expectancy for Zambians has fallen from 54 to 43 years and is projected to drop to 34 by 2010 (UNAIDS, 2004). Those aged 15 have over a 50% risk of dying from AIDS before the age of 35 (CSOZ, 2002).
Women in Zambia are disproportionately affected by HIV due to genital vulnerability, the social context of gender-based power dynamics and sexual practices engaged in to satisfy husbands and prevent marital infidelity (e.g. dry sex, vaginal penetration with non-lubricated genital contact) (Chikumbi, 1999; CSOZ, 1999; 2002b). HIV prevention efforts have focused principally on encouraging the use of male condoms and voluntary counseling and testing (VCT) programs (Allen et al., 1992); VCT has proven most successful in reducing transmission among serodiscordant couples (Allen et al., 1999, 2003). While high in efficacy (93–95%; Kamb et al., 1998), male condoms’ impact on disease prevention has been limited, due in part to low acceptability and culture-specific sexual preferences (Buseh et al., 2002; Lagarde et al., 2001). In Zambia, HIV intervention strategies include limiting sexual partners, promoting use and availability of condoms, controlling STDs and encouraging VCT (CSOZ, 1999).
Our pilot research in Zambia found that a group intervention significantly increased sexual barrier use and acceptability among HIV-positive and -negative women in comparison with the standard of care (VCT) and an individual format six months later (Jones et al., 2004). The current study utilized preliminary data from the New Interventions for Women project in Zambia. The study compared two multi-session, culturally tailored sexual-behavior interventions in individual and group formats over a period of 12 months. We assessed the acceptability and use of sexual barriers and placebos for vaginal chemical barriers (male and female condoms, vaginal lubricants) among HIV-positive Zambian women, the role of cultural preferences and intervention efficacy to increase use. Endpoints included acceptability and use and sexual risk behaviors.
Methods
Recruitment and eligibility
Institutional Review Board (US) and Research Ethics Committee (Zambia) approvals were obtained prior to study onset. Candidates were recruited from the VCT sites at the University Teaching Hospital, KARA Counseling Center, community clinics and the Network of Zambian People Living Positive. Participants (n=240) were sexually active HIV-positive women of 18 years or older living in Lusaka. Due to potential distress, candidates diagnosed HIV-positive within the previous two weeks were temporarily excluded.
Candidates were screened for eligibility, provided an informed consent and were administered a baseline assessment. Ineligibility was primarily due to lack of sexual activity. Recruiters, assessors and interventionists were multilingual and translated into participant language (e.g. Bemba, Nyanja, Nsenga) any information that required clarification. At the request of participants, assessments were primarily conducted in English. Interventions were conducted using a combination of Bemba, Nyanja and English, due to the mixture of audience language (73 local and three primary regional languages).
Participants were randomized into one of two arms, ‘group’ or ‘individual’ and completed three monthly sessions. Due to ethical concerns related to the transmission of HIV by participants, no control group or ‘usual care’ arm was included. Pilot data (Jones et al., 2004) indicated that even ‘enhanced usual care’ VCT clients significantly decreased their use of sexual barrier products over time. To respond to cultural mores, participants were able to invite male partners to attend a single session to inform them about the intervention and study products.
All participants were followed over a twelve-month period (baseline assessment, three sessions, brief assessments at months four and five and a six- and twelve-month post-baseline assessment). Participants were screened for STDs and vaginal infections and provided with appropriate treatment prior to receiving study products. All participants received compensation for their time and travel expenses. Assessors and facilitators were blind to study arm assignment.
Intervention content
Group arm
The intervention was manualized and developed with feedback from previous pilot projects (Jones et al., 2001; 2004) and focus groups were conducted in the US and Zambia. Facilitators were registered and licensed practical nurses and healthcare staff trained in intervention administration.
Groups, limited to ten women, employed a closed, structured, behavioural-change intervention. Each of the two-hour sessions emphasized participation, practice, experimentation and feedback on sexual barrier products and risk reduction strategies. Group cohesion and skill building was fostered through activities such as role playing and real life examples and problem solving strategies. Group content utilized the conceptual model of the Theory of Reasoned Action and Planned Behaviour (Albarracin et al., 2001). The intervention and accompanying African videos were in English and translated into local language as required during viewing. Videos addressed barrier use, common questions and sexual negotiation strategies. Participants were provided with a one-month supply of male and female condoms and vaginal lubricants (gels and suppositories) at each visit and were strongly encouraged to use condoms in conjunction with the lubricants.
Session one
HIV/STDs, safer sex, barrier use, reproductive choice, HIV re-infection, transmission and infection with other STDs and hierarchical methods of sexual barrier use were reviewed. Male and female condoms were introduced with videos and practice with models. Cognitive/behavioral (CB) skill training, a technique designed to relate participants’ thinking patterns (cognitions) as they relate to their behaviors, was applied to sexual behavior. CB techniques were applied to interpersonal negotiating skills and cognitive reframing, changing perceived positive or negative value or interpretation of situations, interactions and individuals, as well as to increasing participants’ awareness of their potentially negative attitudes or opinions related to barrier use.
Reproductive choice addressed those not using any sexual protection while seeking to become pregnant. Participants charted their menstrual cycle to determine the most likely time to conceive and were encouraged to use sexual barriers during the time when pregnancy was unlikely, providing protection during the majority of the cycle.
Session two
Vaginal lubricants, gels and suppositories, were introduced and participants were asked to discuss their preferences. Products were clearly identified as lubricants and as having no spermicidal or microbicidal protection. Women were instructed in application and provided with each of the products. CB skill building focused on sexual problem solving techniques.
Session three
Participants discussed lubricants as potential microbicidal sexual barriers and identified their favorites. Women addressed their experiences with barrier products, partners’ reactions and problems. CB skill training and role-plays continued to focus on problem solving. Cognitive restructuring, reviewing and revising unproductive thinking as limiting new behaviors, was applied to practicing safer sex, e.g. use of sexual barriers and communication with sexual partners.
Individual arm
Participants were provided with information in a traditional health education individual format. Sessions included identical information on HIV/STD transmission hierarchical counseling and skill training to facilitate product use. Videos, written materials on use and supplies of male and female condoms and vaginal lubricants were provided.
Outcome measures
Sexual activities questionnaire
This 55-item scale was adapted from the Sexual Risk Behavior Assessment Schedule (Meyer-Bahlberg et al., 1990). Responses include frequency of heterosexual sexual intercourse (vaginal, oral, anal) in the past month with primary (most frequent) and non-primary (other male) partners, barrier use, partner HIV status and sexual practices and alcohol or drug use during sex. The measure utilizes a Likert scale, ‘all the time’ or ‘nine times out of ten’ = 5, ‘most times’ or ‘seven times out of ten’ = 4, ‘half of the time’ or ‘five times out of ten’ = 3, ‘sometimes’ or ‘three times out of ten’ = 2, ‘never’ = 1.
Barrier questionnaire
Adapted from the University of California at San Francisco Center for AIDS Prevention Studies Barrier Questionnaire, this measure assesses current, previous and future willingness to use sexual barriers using a Likert scale (like to use; ‘like very much’ = 5, ‘like somewhat’ = 4, ‘neutral’ = 3, ‘dislike somewhat’ = 2, ‘strongly dislike’ = 1; willingness to use: ‘not at all willing to use’ = 1, ‘slightly willing’ = 2, ‘moderately willing’ = 3, ‘very willing’ = 4). Stem prompts were adapted to state willingness to use products based on specific characteristics.
Acceptability measures
These 25-item scales were developed using US and Zambian pilot-testing feedback and assessment of product preference, ease of use, comfort, fun, sexual pleasure, control, communication, confidence and secrecy. Scales include rating and comparison between products using combined Likert scales of 1–7 (‘definitely yes’ = 1 to ‘definitely no’ =7), partner reactions to products and ranking of attributes.
Demographic questionnaire
This questionnaire assessed age, religion, nationality, ethnicity, educational level, employment status, residential status, date of HIV infection (if known), drug or alcohol use, marital/partner status, living situation, number of children and children’s serostatus (if known).
Statistical analyses
This study used a repeated measures design with experimental arm (group, individual) as the between-subjects factor and time (baseline, post-intervention) as the within-subjects factor. Correlations are reported as Pearson’s r statistics, repeated measures between arms are reported as F statistics and effects of time on the overall sample are reported as t-tests, alpha (2-tailed) is 0.05.
Results
Participants
Participants’ (n=240) mean age was 29; most women (79%) were unemployed. Ethnic groups included Bemba (30%), Nsenga/Ngoni/Tumbuka (26%), Tonga (8%), Lozi (6%), Mambwe/Namwanga (10%) and other (20%). Average level of educational attainment was six years, ranging from no formal education (2%) to primary education (58%), secondary education (39%) and university (1%). Most (82%) were married with children (88%; mean number of children =4) and lived in another’s home (64%). Twenty-one percent of participants had seropositive children, while 12% were pregnant and 22% planned to have more children. There were no significant demographic differences between arms.
Baseline sexual behaviour and product ratings
Most women (77%) were sexually active in the last month (see Table I). Male condom use was correlated with partner serodiscordance (r = 0.19, p = 0.03) and partner attendance at an information session (r = 0.21, p =0.008). There were no differences in sexual behavior between arms at baseline.
Table I.
Sexual behavior: Entire Sample.
| Domain | Baseline -% | 6 Months -% | 12 Months -% |
|---|---|---|---|
| Consistent condom use | 54 use all the time | 47 use all the time | 33 use all the time |
| Male condom use | 30 use less than half the time | 29 use less than half the time | 39 use less than half the time |
| Female condom use | 8 previous use
100 never used |
16 use at least half the time
100 never used |
9 use at least half the time
100 never used |
| Vaginal chemical barriers with Condoms | 1 previous use
100 never used |
8 use at least half the time | 23 use at least half the time |
| Dry sex practice | 14 | 9 | 5 |
| Oral sex | 9 | 4 | 0.04 |
| Anal sex | 1 | 1 | 1 |
| Knowledge of partner’s HIV status | HIV-positive 37 | HIV-positive 61 | HIV-positive 61 |
| HIV-negative 15 | HIV-negative 12 | HIV-negative 12 | |
| Don’t know 48 | don’t know 27 | don’t know 27 | |
| Other sexual partners | 2 | 0.04 | 0.04 |
| Primary partner has other sexual partners | 24 | 24 | 24 |
| Willingness ratings | |||
| Not willing … very willing (1 … 4) | |||
| Willingness to use male condoms | X = 3.73 somewhat/very willing to use | somewhat/very willing to use | very willing to use |
| Willingness to use female condoms | X = 3.07 somewhat willing | somewhat/very willing | somewhat/very willing |
| Willingness to use vaginal gels | X =2.90 slightly willing | very willing to use | very willing to use |
| Willingness to use creams | X = 2.98 slightly willing | slightly willing | slightly willing |
| Willingness to use suppositories | X =2.84 moderately willing | moderately/very willing | moderately/very willing |
Sexual behaviour six and twelve months post-baseline
Among women who were sexually active at six months (see Table I), 29% reported less than 50% adherence to condom use. Use of female condoms increased from 8% to 80% reporting trial use and from 1% to 77% reporting trial use of lubricants with condoms, while male condom use was sustained. Using a repeated measures analysis of variance (ANOVA, sex × time × group; controlling for serodiscordance and partner participation), those sexually active at baseline and at six-months in the group arm used sexual barriers (F1,82 = 4.6, p<0.05) and male condoms (F1,67=13.5, p < 0.001) p < 0.001) more often than those in the individual arm, increasing from ‘some of the time’ to ‘most of the time’. There were no differences between arms in levels of female condom use (F1,66 = 0.03, p = 0.86), lubricant use (F1,66 = 0.01, p = 0.91) or use of lubricants with condoms (F1,65 = 3.43, p = 0.07). All participants increased use of female condoms (t1,87 = −8.88, p <0.001), lubricants in with condoms (t 1,86 =−5.15, p <0.001) and lubricants alone (t 1,87 = −11.77, p <0.001) from ‘never’ to ‘some of the time’.
Use of male and female condoms and lubricants with condoms was sustained at 12 months; 15% were currently using female condoms and 69% were using lubricants with condoms. There were no differences between arms in barrier use (F1,113 = 0.5, p = 0.5), use of male condoms (F1,65 = 0.24, p = 0.62), female condoms (F1,65 = 2.8, p = 1), lubricants (F1,65 = 0.97, p = 0.07) or lubricants in combination with condoms (F1,65 = 0.94, p = 0.34). All participants increased their use of female condoms (t1,83 = −5.81, p <0.001), vaginal lubricants (t1,83 = −7.72, p<0.001) and vaginal lubricants with condoms (t1,83 = − 7.7, p<0.001) to ‘some/half of the time’ at 12 months.
Participant retention did not differ between arms at six months (97%) and twelve months (69%), due primarily to employment, illness, hospitalization and death (5%).
Product ratings
Ratings of lubricants and female condoms improved at six and 12 months, male condoms improved at 12 months. Ratings did not differ between arms over time. Among all participants at six months, ratings of male condoms did not improve, while ratings of female condoms (t1,177 = −6.14, p <0.001), gels (t1,177 = −4.69, p <0.001) and suppositories (t1,178 = −3.08, p <0.001) increased. At twelve months, ratings of male condoms (t1,163 = −3.56, p <0.001), female condoms (t1,163 = − 6.33, p <0.001), gels (t1,163 = −6.15, p <0.001) and suppositories (currently being marketed; t1,153 = −4.69, p <0.001) improved.
Product acceptability
Following trial use, participants identified ease of use, comfort, ability to talk about sex and control of barrier-use as the most important characteristics of barrier products and potential to use a product secretly as least important. The most preferred lubricant was the suppository. Acceptability of male and female condoms predicted use of female condoms for the group (F8,66 = 5.37, p <00.001) but not the individual arm (F8,71 = 0.56, p = .81). Vaginal lubricant acceptability predicted its use in the group (F8,66 = 3.21, p = 0.004) but not the individual arm (F8,66 = 0.71, p = 0.70). Finally, trial use of female condoms and lubricants predicted sustained use of both in the group (F8,66 = 3.21, p = 0.004) but not the individual arm (F8,66) = 0.60, p = 0.78).
Discussion
Overall response to this sexual barrier intervention for HIV-positive Zambian women was quite favorable. Group participants increased their use of male condoms over six months, trial use of sexual barriers favorably influenced overall acceptability of products and acceptability predicted their use. Among the entire sample, use of female condoms and vaginal lubricants in combination with condoms significantly increased and was sustained over 12 months without condom drift.
This study highlights the need for longer-term interventions to sustain condom use and suggests that group interventions may be adjuncts to prevention for HIV-positive women in addition to the traditional individual health education. Groups may be acceptable in the Zambian traditional cultural framework of group information dissemination more so than the single-session individual or couples counseling of existing VCT techniques. From a public health standpoint, groups represent a cost effective use of resources, reaching larger numbers of women with lower numbers of staff.
In contrast to studies of shorter duration, participants reported sustained increases in sexual barrier use for up to twelve months. Anecdotal reports suggested that participants even endeavored to regulate their lubricant dosages over 12 months to extend their supplies as long as possible. A small percentage (5%) purchased male condoms. Male and female condoms are available at a discount through social marketing and at no cost at clinics and HIV agencies; lubricants are unavailable.
The necessity for an effective and acceptable vaginal chemical barrier emphasizes the lack of information regarding potential acceptability among diverse populations. In our previous research, Zambian women preferred less lubricated sex Jones et al., 2004). However, this study demonstrated that cultural preferences for dry sex were influenced by interventions introducing lubricants. Such findings could guide development of culturally sensitive sexual-behavior interventions relevant to the introduction of microbicides. Anecdotally, women also used the introduction of lubricants as an opportunity to initiate sexual communication.
The primary study limitation remains its sample size, given the multicultural composition of at least five distinct cultural groups, which precluded analyses by cultural group. In addition, approximately one third of participants were not sexually active at all time points, which reduced the analysis of barrier use and the reliance on self-report, which may limit accuracy. However, given randomization, inaccuracies should be randomly distributed between conditions. Finally, sexual behaviours of HIV-positive women may differ from those of HIV-negative women and the role of male partners was unexplored.
Female-controlled vaginal barriers potentially allow women a more prominent role in risk reduction while ensuring their own protection. However, sexual behaviour does not occur in a vacuum. The role of Zambian men as the culturally defined decision makers must also be included. As methods of HIV prevention develop, acceptability and sexual barrier use research must include both men and women’s preferences within the context of both their sexual and cultural relationships.
Figure 1.
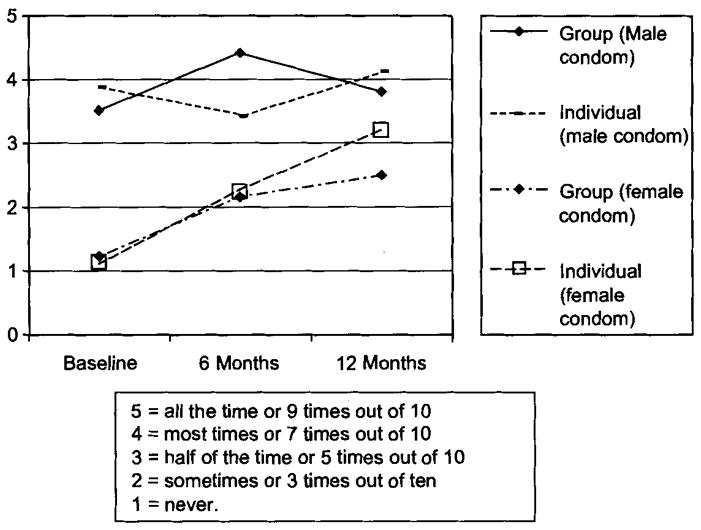
Frequency of male and female condom use.
Figure 2.
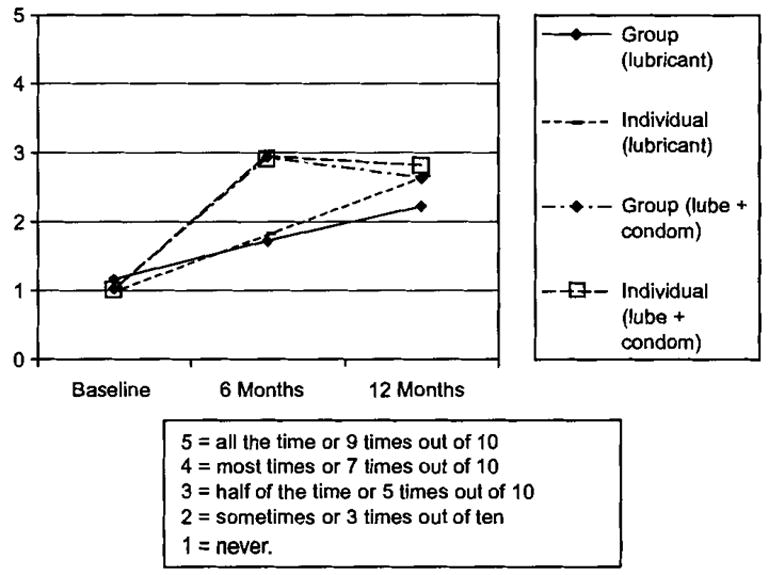
Frequency of lubricant use with and without condoms.
Acknowledgments
We would like to dedicate this manuscript to Dr. Ganapati J. Bhat, who passed away in March 2005, without whom this research would not have been possible. We would also like to acknowledge all those in our research team at the University Teaching Hospital in Lusaka, community clinics providing referrals, KARA Counselling, the National Association for Zambian People Positive and, most importantly, the women participating in this research. This research was support by a grant from the National Institute of Mental Health RO1MH63630.
References
- Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin. 2001;727:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen S, Bogaerts J, Van De Perre P, Nsengumuremyi F, Lindan C, Carael M, et al. Confidential HIV testing and condom promotion in Africa: Impact on HIV and gonorrhea rates. Journal of the American Medical Association. 1992;268:3338–3343. [PubMed] [Google Scholar]
- Allen SA, Karita E, N’gandu N, Tichacek A. The evolution of Voluntary Testing and Counseling as an HIV prevention strategy. In: Gibney, et al., editors. Preventing HIV in developing countries: Biomedical and behavioral approaches. New York: Plenum Press; 1999. [Google Scholar]
- Allen S, Meinzen-Derr J, Kautzman M, et al. Sexual behavior of HIV-discordant couples after HIV counseling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- Buseh AG, Glass LK, McElmurry BJ. Cultural and gender issues related to HIV/AIDS prevention in rural Swaziland: A focus group analysis. Health Care for Women International. 2002;23(2):173–184. doi: 10.1080/073993302753429040. [DOI] [PubMed] [Google Scholar]
- Central Statistical Office, Zambia. Zambia Sexual Behavior Survey 1998 with selected findings from the quality of STD Services Assessment. 1999. [Google Scholar]
- Central Statistical Office, Zambia. ANC Sentinel Surveillance of HIV/Syphilis Trends in Zambia 1994–2002. 2002. [Google Scholar]
- Central Statistical Office, Zambia. Zambia Demographic and Health Survey. Central Statistical Office; Zambia: 2002b. [Google Scholar]
- Chikumbi B. Dry sex potentiates HIV and STD spread. The Eleventh International conference on AIDS and STDs in Africa (ICASA); Lusaka, Zambia. 1999. [Google Scholar]
- UNAIDS/WHO. Epidemiological Fact Sheet on HIV/AIDS and sexually transmitted infections; 2000 update. 2000. [Google Scholar]
- Fylkesnes K, Musonda RM, Kasumba K, et al. The HIV epidemic in Zambia: Socio-demographic prevalence patterns and indications of trends among childbearing women. AIDS. 1997;11:339–345. doi: 10.1097/00002030-199703110-00012. [DOI] [PubMed] [Google Scholar]
- JOINT UNITED NATIONS PROGRAMME ON HIV/AIDS UNAIDS. Zambia: Epidemiological Fact Sheet on HIV/AIDS and Sexually Transmitted Infections. 2004. [Google Scholar]
- Jones DL, Weiss SM, Malow R, Ishii M, Devieux J, Stanley H, et al. A brief sexual barrier intervention for women living with AIDS: Acceptability, use and ethnicity. Journal of Urban Health. 2001;12:593–604. doi: 10.1093/jurban/78.4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DL, Weiss SM, Bhat GJ, Feldman DA, Bwalya V, Budash D. A sexual barrier intervention for HIV-positive/negative Zambian women: Acceptability and use of vaginal chemical barriers. Journal of Multicultural Nursing and Health. 2004;10:21–31. [PMC free article] [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas JM, Rhodes K, Rogers J, Bolan G, et al. The study group on the heterogeneity of HIV epidemics in African cities. AIDS. 1998;15:1399–1408. [Google Scholar]
- Lagarde E, Auvert B, Chege J, et al. Condom use and its association with HIV/sexually transmitted diseases in four urban communities of sub-Saharan Africa. AIDS. 2001;4:571–578. doi: 10.1097/00002030-200108004-00008. [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlberg HFL, Ehrhardt AA, Exner TM, Gruen RS. Sexual risk behavior assessment schedule: Adult (SERBAS-A-DF-4) Manual 1992 [Google Scholar]
- UNAIDS/WHO. Epidemiological Fact Sheet on HIV/AIDS and sexually transmitted infections; 2000 update. 2000. [Google Scholar]
- UNAIDS/WHO. Report on the Global AIDS Epidemic: 2004 Executive Summary. 2004 Available at: http://www.unaids.org/bangkok2004/GAR2004>html/ExecSummar.
- UNAIDS/WHO Working Group on Global HIV/AIDS and STD Surveillance. Epidemiological Fact Sheet on HIV/AIDS and sexually transmitted diseases. 2002 Available at: http://www.sho.ch/emc/diseases/hiv.
- UNAIDS-WHO Joint United National Programme on HIV/AIDS. AIDS Epidemic Update. World Health Organization; Geneva, Switzerland: 2002. [Google Scholar]
- UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance. Zambia Epidemiological Fact Sheet on HIV/AIDS and sexual transmitted infections. 2000 Update; Geneva, Switzerland. 2000. [Google Scholar]


